Salvage Hip Arthroplasty in Nail Failure: A Systematic Review
Abstract
:1. Introduction
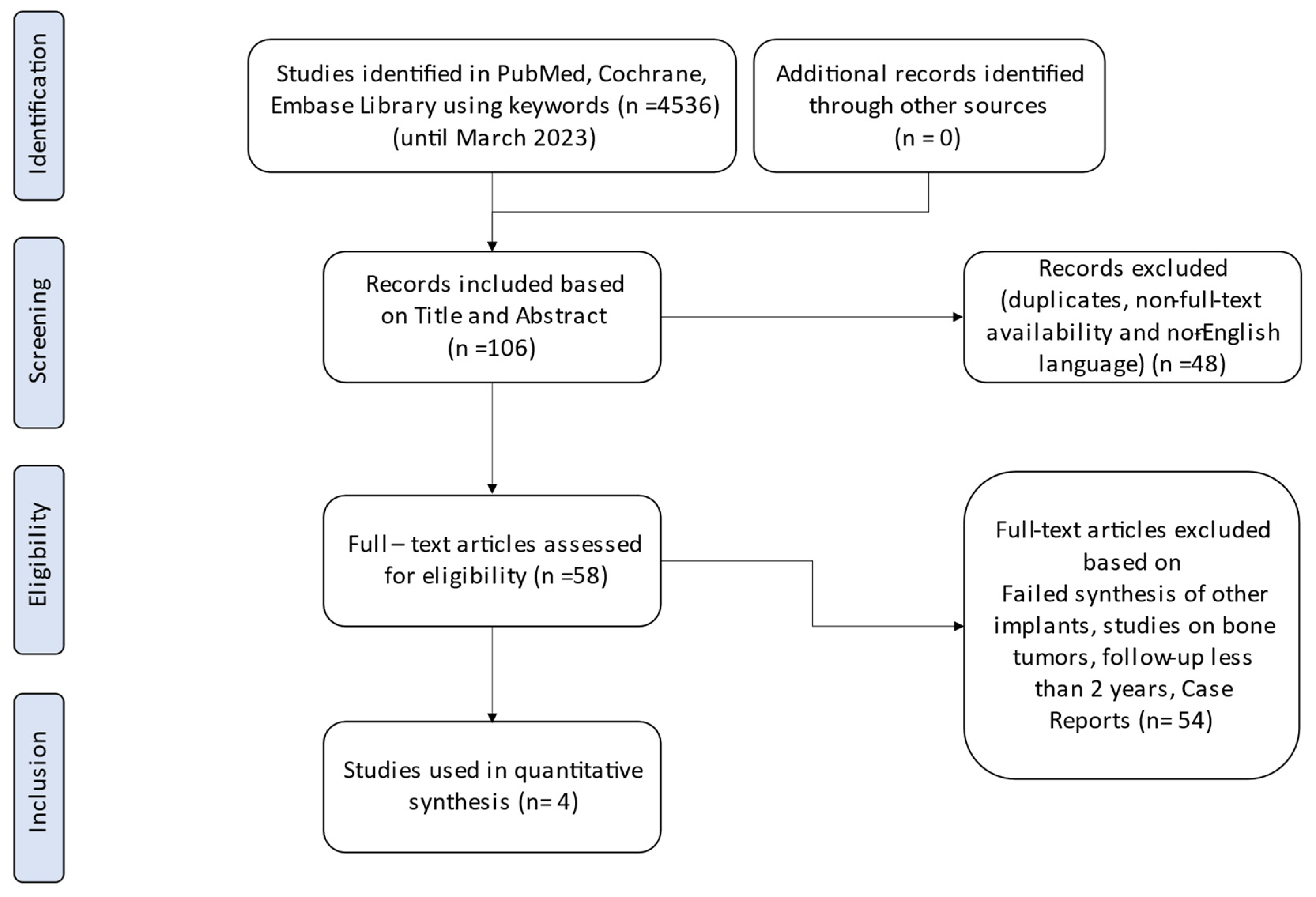
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Literature Appraisal
2.4. Data Extraction
3. Results
3.1. Search Results
3.2. Characteristics of the Included Studies
3.3. Clinical Results
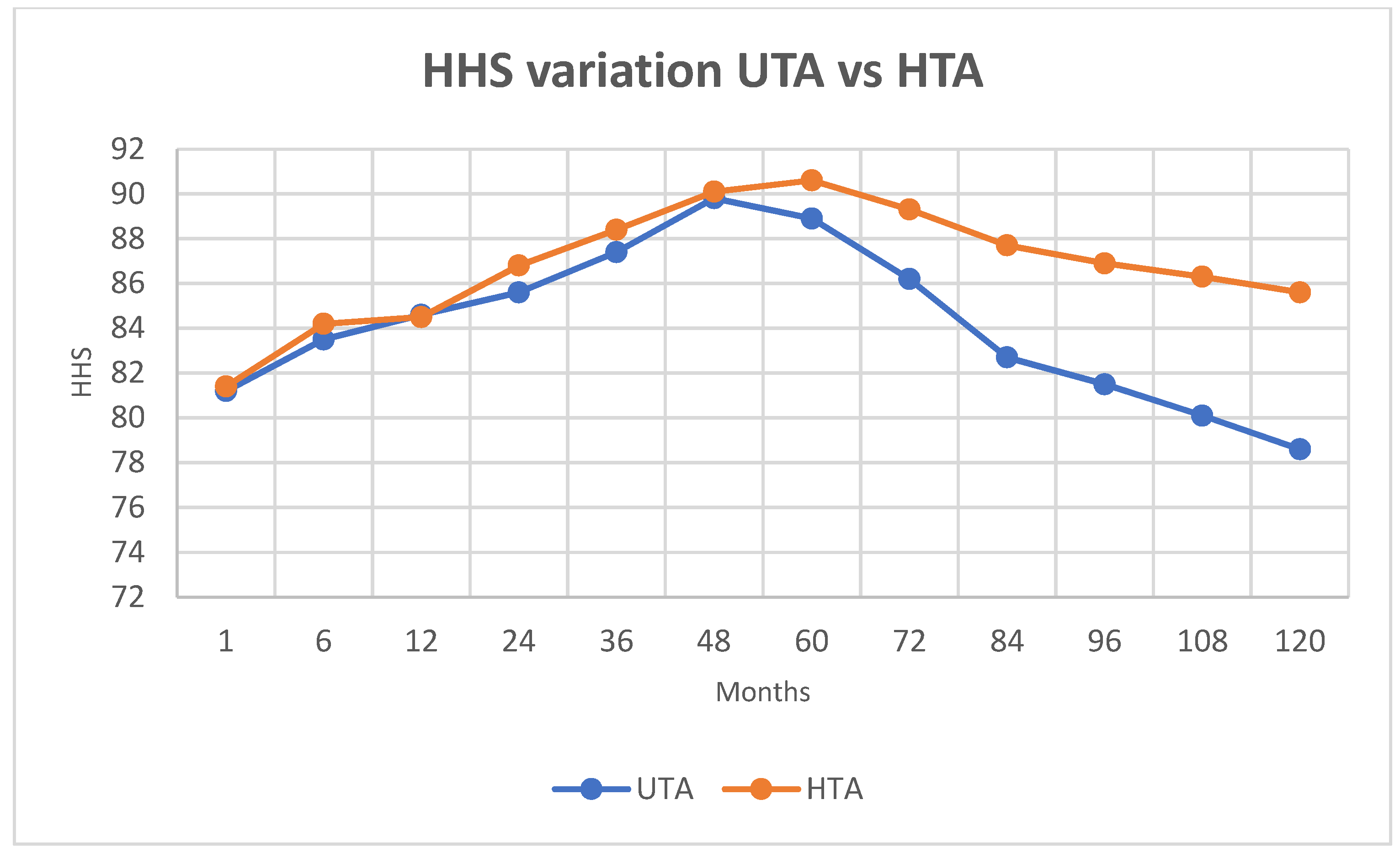
3.3.1. Functional Outcomes
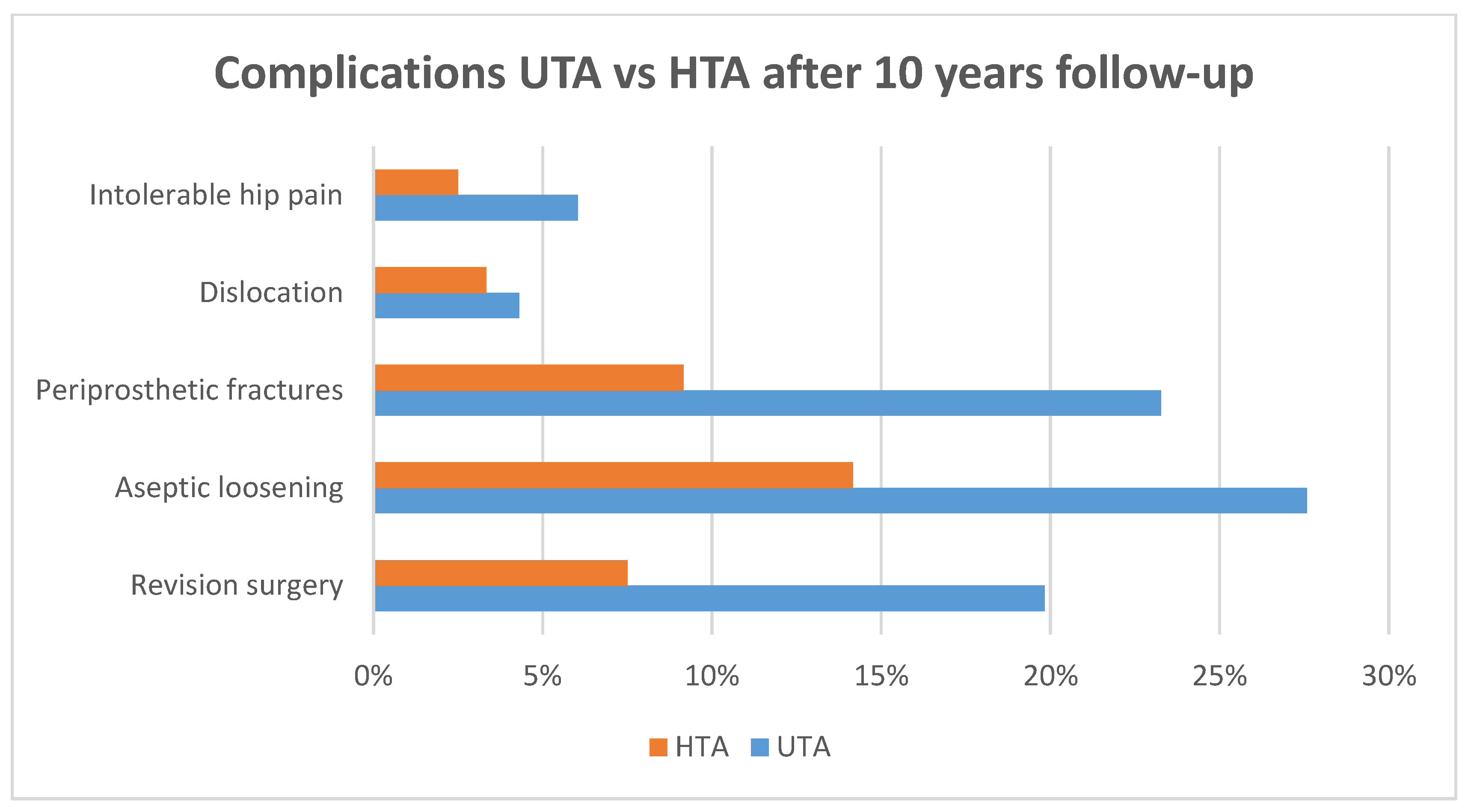
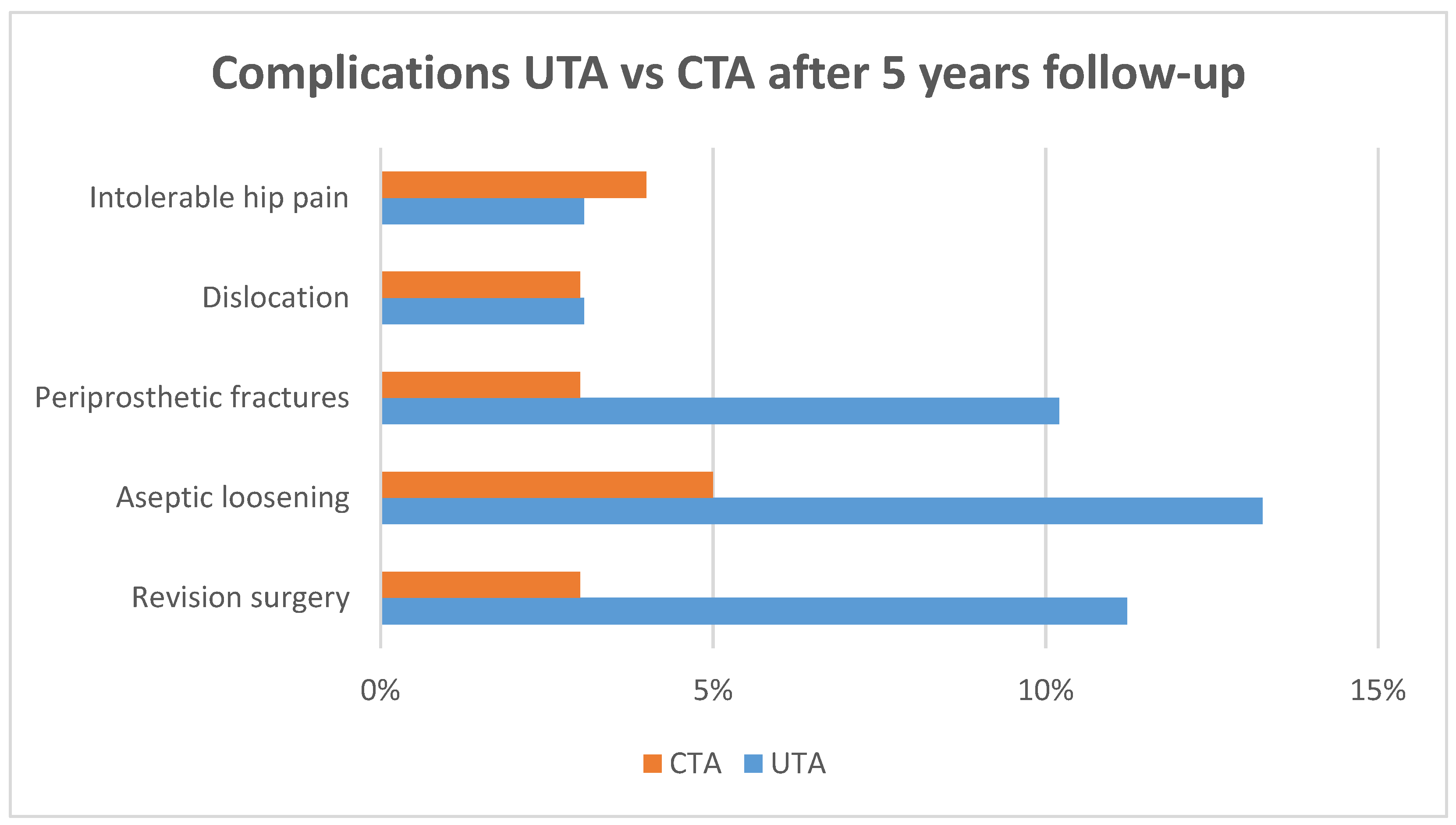
3.3.2. Complications
3.3.3. Survivorship
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ettinger, B.; Black, D.M.; Dawson-Hughes, B.; Pressman, A.R.; Melton, L.J. Updated Fracture Incidence Rates for the US Version of FRAX®. Osteoporos. Int. 2010, 21, 25–33. [Google Scholar] [CrossRef]
- Burge, R.; Dawson-Hughes, B.; Solomon, D.H.; Wong, J.B.; King, A.; Tosteson, A. Incidence and Economic Burden of Osteoporosis-Related Fractures in the United States, 2005–2025. J. Bone Miner. Res. 2007, 22, 465–475. [Google Scholar] [CrossRef]
- Lorich, D.G.; Geller, D.S.; Nielson, J.H. Osteoporotic Pertrochanteric Hip Fractures: Management and Current Controversies. Instr. Course Lect. 2004, 53, 441–454. [Google Scholar] [CrossRef] [PubMed]
- Cumming, R.G.; Nevitt, M.C.; Cummings, S.R. Epidemiology of Hip Fractures. Epidemiol. Rev. 1997, 19, 244–257. [Google Scholar] [CrossRef]
- Evaniew, N.; Bhandari, M. Cochrane in CORR ®: Intramedullary Nails for Extracapsular Hip Fractures in Adults (Review). Clin. Orthop. Relat. Res. 2015, 473, 767–774. [Google Scholar] [CrossRef]
- Socci, A.R.; Casemyr, N.E.; Leslie, M.P.; Baumgaertner, M.R. Implant Options for the Treatment of Intertrochanteric Fractures of the Hip: Rationale, Evidence, and Recommendations. Bone Jt. J. 2017, 99, 128–133. [Google Scholar] [CrossRef] [PubMed]
- Anglen, J.O.; Baumgaertner, M.R.; Smith, W.R.; Tornetta Iii, P.; Ziran, B.H. Technical Tips in Fracture Care: Fractures of the Hip. Instr. Course Lect. 2008, 57, 17–24. [Google Scholar]
- Wahlsten, L.R.; Palm, H.; Gislason, G.H.; Brorson, S. Sex Differences in Incidence Rate, and Temporal Changes in Surgical Management and Adverse Events after Hip Fracture Surgery in Denmark 1997–2017: A Register-Based Study of 153,058 Hip Fracture Patients. Acta Orthop. 2021, 92, 424–430. [Google Scholar] [CrossRef]
- Kim, B.-S.; Lim, J.-Y.; Ha, Y.-C. Recent Epidemiology of Hip Fractures in South Korea. Hip. Pelvis. 2020, 32, 119. [Google Scholar] [CrossRef]
- Rosenblum, S.; Zuckerman, J.; Kummer, F.; Tam, B. A Biomechanical Evaluation of the Gamma Nail. J. Bone Jt. Surg. Br. Vol. 1992, 74, 352–357. [Google Scholar] [CrossRef]
- Davis, T.; Sher, J.; Horsman, A.; Simpson, M.; Porter, B.; Checketts, R. Intertrochanteric Femoral Fractures. Mechanical Failure after Internal Fixation. J. Bone Jt. Surg. Br. Vol. 1990, 72, 26–31. [Google Scholar] [CrossRef] [PubMed]
- Utrilla, A.L.; Reig, J.S.; Muñoz, F.M.; Tufanisco, C.B. Trochanteric Gamma Nail and Compression Hip Screw for Trochanteric Fractures: A Randomized, Prospective, Comparative Study in 210 Elderly Patients with a New Design of the Gamma Nail. J. Orthop. Trauma 2005, 19, 229–233. [Google Scholar] [CrossRef]
- Alvarez, D.B.; Aparicio, J.P.; Fernández, E.L.-A.; Múgica, I.G.-B.; Batalla, D.N.; Jiménez, J.P. Implant Breakage, a Rare Complication with the Gamma Nail. A Review of 843 Fractures of the Proximal Femur Treated with a Gamma Nail. Acta Orthop. Belg. 2004, 70, 435–443. [Google Scholar] [PubMed]
- Parker, M. Cutting-out of the Dynamic Hip Screw Related to Its Position. J. Bone Jt. Surg. Br. Vol. 1992, 74, 625. [Google Scholar] [CrossRef]
- Kashigar, A.; Vincent, A.; Gunton, M.J.; Backstein, D.; Safir, O.; Kuzyk, P.R.T. Predictors of Failure for Cephalomedullary Nailing of Proximal Femoral Fractures. Bone Jt. J. 2014, 96, 1029–1034. [Google Scholar] [CrossRef]
- Hao, Y.; Zhang, Z.; Zhou, F.; Ji, H.; Tian, Y.; Guo, Y.; Lv, Y.; Yang, Z.; Hou, G. Risk Factors for Implant Failure in Reverse Oblique and Transverse Intertrochanteric Fractures Treated with Proximal Femoral Nail Antirotation (PFNA). J. Orthop. Surg. Res. 2019, 14, 350. [Google Scholar] [CrossRef] [PubMed]
- Mavrogenis, A.F.; Panagopoulos, G.N.; Megaloikonomos, P.D.; Igoumenou, V.G.; Galanopoulos, I.; Vottis, C.T.; Karabinas, P.; Koulouvaris, P.; Kontogeorgakos, V.A.; Vlamis, J.; et al. Complications After Hip Nailing for Fractures. Orthopedics 2016, 39, e108–e116. [Google Scholar] [CrossRef]
- Foster, A.L.; Moriarty, T.F.; Zalavras, C.; Morgenstern, M.; Jaiprakash, A.; Crawford, R.; Burch, M.-A.; Boot, W.; Tetsworth, K.; Miclau, T.; et al. The Influence of Biomechanical Stability on Bone Healing and Fracture-Related Infection: The Legacy of Stephan Perren. Injury 2021, 52, 43–52. [Google Scholar] [CrossRef]
- Steinmetz, S.; Wernly, D.; Moerenhout, K.; Trampuz, A.; Borens, O. Infection after Fracture Fixation. EFORT Open Rev. 2019, 4, 468–475. [Google Scholar] [CrossRef]
- Tomás-Hernández, J.; Núñez-Camarena, J.; Teixidor-Serra, J.; Guerra-Farfan, E.; Selga, J.; Antonio Porcel, J.; Andrés-Peiró, J.V.; Molero, V. Salvage for Intramedullary Nailing Breakage after Operative Treatment of Trochanteric Fractures. Injury 2018, 49, S44–S50. [Google Scholar] [CrossRef]
- Min, B.-W.; Lee, K.-J.; Oh, J.-K.; Cho, C.-H.; Cho, J.-W.; Kim, B.-S. Salvage Treatment of Failed Internal Fixation of Intertrochanteric Fractures: What Factors Determine the Failure of Treatment? Injury 2020, 51, 367–371. [Google Scholar] [CrossRef]
- Brunner, A.; Büttler, M.; Lehmann, U.; Frei, H.C.; Kratter, R.; Di Lazzaro, M.; Scola, A.; Sermon, A.; Attal, R. What Is the Optimal Salvage Procedure for Cut-out after Surgical Fixation of Trochanteric Fractures with the PFNA or TFN? Injury 2016, 47, 432–438. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. J. Clin. Epidemiol. 2021, 134, 178–189. [Google Scholar] [CrossRef] [PubMed]
- Innocenti, M.; Guido, D.; Cozzi Lepri, A.; Maritato, E.; Carulli, C.; Matassi, F.; Civinini, R. Proximal Femoral Replacement: A Salvage Treatment of Cephalomedullary Nails’ Mechanical Failures in the Elderly Population. Injury 2021, 52, 1868–1874. [Google Scholar] [CrossRef] [PubMed]
- Shi, W.; Zhang, Y.; Xu, Y.; Zeng, X.; Fu, H.; Yu, W. Conversion of Failed Proximal Femoral Nail Antirotation to Uncemented or Cemented Femoral Component Fixation: A Multicentre Retrospective Study with a Median 10-Year Follow-Up. BMC Musculoskelet. Disord. 2022, 23, 375. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.; Han, X.; Chen, W.; Mao, S.; Zhao, M.; Zhang, X.; Han, G.; Ye, J.; Chen, M.; Zhuang, J. Conversion from a Failed Proximal Femoral Nail Anti-Rotation to a Cemented or Uncemented Total Hip Arthroplasty Device: A Retrospective Review of 198 Hips with Previous Intertrochanteric Femur Fractures. BMC Musculoskelet. Disord. 2020, 21, 791. [Google Scholar] [CrossRef]
- Godoy-Monzon, D.; Diaz Dilernia, F.; Piccaluga, F.; Cid Casteulani, A.; Turus, L.; Buttaro, M. Conversion Total Hip Arthroplasty with a Proximally Modular, Distal Fixation Reconstruction Prosthesis Following Cephalomedullar Nail Failure. HIP Int. 2020, 30, 26–33. [Google Scholar] [CrossRef]
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Methodological Index for Non-Randomized Studies (MINORS): Development and Validation of a New Instrument: Methodological Index for Non-Randomized Studies. ANZ J. Surg. 2003, 73, 712–716. [Google Scholar] [CrossRef]
- Boldin, C.; Seibert, F.J.; Fankhauser, F.; Peicha, G.; Grechenig, W.; Szyszkowitz, R. The Proximal Femoral Nail (PFN)—A Minimal Invasive Treatment of Unstable Proximal Femoral Fractures: A Prospective Study of 55 Patients with a Follow-up of 15 Months. Acta Orthop. Scand. 2003, 74, 53–58. [Google Scholar] [CrossRef]
- Luthringer, T.A.; Elbuluk, A.M.; Behery, O.A.; Cizmic, Z.; Deshmukh, A.J. Salvage of Failed Internal Fixation of Intertrochanteric Hip Fractures: Clinical and Functional Outcomes of Total Hip Arthroplasty versus Hemiarthroplasty. Arthroplast. Today 2018, 4, 383–391. [Google Scholar] [CrossRef]
- Smith, A.; Denehy, K.; Ong, K.L.; Lau, E.; Hagan, D.; Malkani, A. Total Hip Arthroplasty Following Failed Intertrochanteric Hip Fracture Fixation Treated with a Cephalomedullary Nail. Bone Jt. J. 2019, 101, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Neri, T.; Philippot, R.; Klasan, A.; Putnis, S.; Leie, M.; Boyer, B.; Farizon, F. Dual Mobility Acetabular Cups for Total Hip Arthroplasty: Advantages and Drawbacks. Expert Rev. Med. Devices 2018, 15, 835–845. [Google Scholar] [CrossRef] [PubMed]

| Author | Year of Publication | Study Design | N° Patients | Age | M/F | Salvage Procedure | Average Follow-Up |
|---|---|---|---|---|---|---|---|
| Godoy-Monzon et al. [27] | 2019 | Retrospective analysis of the outcomes of conversion THA using a modular stem following a CMN failure | 28 | 72.7 (62–83) | 11/17 | THA = 28 PHA = 0 | 64 months |
| Yu et al. [26] | 2020 | Retrospective analysis of the outcomes of failed PFNAs converted to a UTA or CTA in elderly individuals | 198 | 66 (62–71) | 92/106 | THA = 198 PHA = 0 | 65 months |
| Innocenti et al. [24] | 2021 | Retrospective analysis of the outcome and complication rate in a group of elderly patients who underwent PFR as a salvage treatment after CMN mechanical failures | 21 | 85.3 (78–93) | 16/5 | THA = 14 PHA = 7 | 37 months |
| Shi et al. [25] | 2022 | Retrospective analysis of the outcomes of the conversion of failed PFNAs to uncemented versus hybrid THAs in the elderly population | 236 | 66.4 (65–71) | 125/111 | THA = 236 PHA = 0 | 120 months |
| Author | Initial Fracture (AO/OTA) | Femoral Nail | Cause of Failure | Time from Failure to Artrhoplasty | Implant | Surgical Approach |
|---|---|---|---|---|---|---|
| Godoy-Monzon et al. [27] | Not specified | PFN—Synthes (13) TFN—Synthes (9) Gamma3—Stryker (6) | Osteoarthritis (11) AVN/head collapse (7) Pseudarthrosis (5) CMN migration (4) CMN breakage (1) | 12.6 months (range 7–20) | Uncemented MFSs stem (23) or Cemented MFSs stem (5)—Waldemar Link Uncemented modular cup (24) or Cemented all-poly cup (4)—Waldemar Link | Posterolateral approach |
| Yu et al. [26] | 31A1 (35) 31A2 (118) 31A3 (45) | PFNA—Smith&Nephew (198) | Instability (48) Mechanical failure (45) Both (105) | <1 year (32) 1–2 years (109) >2 years (57) | UTA (98) Corail uncemented stem (DePuy) and Reflection uncemented cup (Smith&Nephew CTA (100) Exeter stem and cup (Stryker) | Not specified |
| Innocenti et al. [24] | 31A2.2 (3) 31A2.3 (9) 31A3.3 (9) | PFNA—Synthes (9) CHIMAERA—Orthofix (6) Gamma3—Stryker (4) INTERTAN—Smith&Nephew (2) | Nail breakage (17) Lag screw cut-out (4) | 9.6 months (range 8–14) | Modular DM Delta TT cup (14)—Lima or Bioplar head (7)—VarioCup-Link Megasystem C-Link cemented PFR (21)—Waldemar Link | Direct lateral approach |
| Shi et al. [25] | 31A1 (93) 31A2 (143) | PFNA—Synthes (236) | Instability (118) Mechanical failure (87) Both (31) | <2 years (154) ≥2 years (82) | UTA (116) Corail uncemented stem (DePuy) and Continuum cup (Zimmer Biomet) HTA (120) Exeter stem (Stryker) and Continuum cup (Zimmer Biomet) | Not specified |
| Year | Author | MINORS | A Clearly Stated Aim | Inclusion of Consecutive Patients | Prospective Collection of Data | Endpoint Appropriate for Aim of Study | Unbiased Assessment of Study Endpoint | Follow-Up Period Appropriate | Loss of Follow-Up Less than 5% | Prospective Calculation of Study Size | Adequate Control Group | Contemporary Group | Baseline Equivalence of Groups | Adequate Statistical Analysis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2020 | Godoy-Monzon [27] | 11 | 2 | 2 | 1 | 2 | 0 | 2 | 2 | |||||
| 2020 | Yu [26] | 21 | 2 | 2 | 1 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| 2021 | Innocenti [24] | 10 | 2 | 2 | 1 | 2 | 0 | 2 | 1 | |||||
| 2022 | Shi [25] | 20 | 2 | 2 | 1 | 2 | 0 | 2 | 1 | 2 | 2 | 2 | 2 | 2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pantè, S.; Braconi, L.; Cottino, U.; Dettoni, F.; Rossi, R. Salvage Hip Arthroplasty in Nail Failure: A Systematic Review. Prosthesis 2023, 5, 1343-1356. https://doi.org/10.3390/prosthesis5040092
Pantè S, Braconi L, Cottino U, Dettoni F, Rossi R. Salvage Hip Arthroplasty in Nail Failure: A Systematic Review. Prosthesis. 2023; 5(4):1343-1356. https://doi.org/10.3390/prosthesis5040092
Chicago/Turabian StylePantè, Salvatore, Lorenzo Braconi, Umberto Cottino, Federico Dettoni, and Roberto Rossi. 2023. "Salvage Hip Arthroplasty in Nail Failure: A Systematic Review" Prosthesis 5, no. 4: 1343-1356. https://doi.org/10.3390/prosthesis5040092
APA StylePantè, S., Braconi, L., Cottino, U., Dettoni, F., & Rossi, R. (2023). Salvage Hip Arthroplasty in Nail Failure: A Systematic Review. Prosthesis, 5(4), 1343-1356. https://doi.org/10.3390/prosthesis5040092







