Abstract
This manuscript introduces a novel two-step technique for fabricating mobile dentures post-extraction to streamline prosthodontic rehabilitation. The study utilizes various materials, including dental polymers, metals, ceramics, and composite materials, each chosen for their unique properties that contribute to the final prosthesis’s functionality, durability, and esthetics. The detailed procedure involves an initial occlusal registration immediately following tooth extraction, capturing precise occlusal relationships and a comprehensive dental impression. This approach reduces clinical visits and leverages optimal alveolar ridge morphology. The expected results highlight the efficiency of the technique, reducing treatment time without compromising quality and potentially improving patient satisfaction and prosthodontic outcomes. This innovative method conclusively promises rapid, efficient, and patient-centered dental rehabilitation, emphasizing the need for future research to validate its effectiveness and explore long-term outcomes.
1. Introduction
1.1. Background
The fabrication of mobile dentures following dental extractions is a cornerstone in prosthodontic rehabilitation, aiming to restore masticatory function, esthetics, and overall quality of life [1]. Removable prosthodontics are a treatment option for patients who have lost one or more teeth. Fixed prosthodontics, such as bridges and crowns, are cemented or screwed to the patient’s existing teeth or dental implants, offering a non-removable solution that closely replicates the natural appearance and function genuine teeth. This approach ensures excellent stability and efficiency in chewing, contributing positively to oral health. However, fixed prosthodontics often require the alteration or preparation of adjacent healthy teeth, which can lead to potential long-term dental issues and necessitates a complex and rigorous maintenance regimen to prevent problems such as decay under the prosthetic or periodontal disease at the abutment sites. On the other hand, removable prosthodontics, like complete and partial dentures, provide a versatile and less invasive alternative that is generally more cost-effective and easier for patients to manage in daily cleaning and maintenance. Despite these benefits, they might lack the stability and comfort of fixed alternatives, as they can move during speech or eating, potentially leading to sore spots and diminished patient satisfaction. Removable options also typically require more frequent adjustments to accommodate changes in the oral cavity, adding to their long-term upkeep. Deciding between fixed and removable prosthodontics depends on several patient-specific factors, including the condition of remaining teeth, preference for permanence versus flexibility, esthetic considerations, and financial constraints. Each option presents unique advantages and challenges that should be carefully considered regarding the patient’s lifestyle, expectations, and overall oral health goals [2]. Removable prosthodontics are made of a base material, such as acrylic resin, that supports artificial teeth. Removable prosthodontics can be either complete or partial. Complete dentures replace all teeth in an arch, while partial dentures replace only some of the teeth. Manufacturing removable prosthodontics is a complex process involving several steps [3]. Traditional protocols for denture fabrication typically involve multiple clinical and laboratory steps, often extending over several weeks or even months. This time-consuming process can be a significant source of distress for patients, prolonging the adjustment and adaptation to the new prosthesis. In recent years, there has been a paradigm shift towards minimizing the number of clinical visits and reducing the overall treatment time without compromising the quality of the prosthodontic outcome [4,5].
During the realization of dentures, the pre-clinician diagnostic phases are essential. Initially, a comprehensive oral examination is conducted to assess the patient’s systemic and oral health, including the condition of any remaining teeth, the health of the oral mucosa, and the anatomical features of the jaw and oral cavity. This could lead to instrumental examinations, like radiography, to evaluate the periodontal status of residual teeth. Carefully analyzing the soft and hard tissues to highlight anomalies, such as exostoses or mandibular tori, is essential. Subsequently, we can proceed with the joint evaluation of the patient, highlighting the presence of temporomandibular anomalies. To evaluate the peri-oral soft tissues, we must consider the high esthetic value of a removable prosthetic rehabilitation. The importance of a thorough diagnosis and analysis of temporomandibular disease (TMD) in patients before the realization of removable dentures cannot be overstated. Accurate assessment of the temporomandibular joint (TMJ) and its function is crucial because TMD can significantly impact the overall success and functionality of the dentures. Patients with undiagnosed or untreated TMD may experience increased discomfort and complications with their prosthesis due to the added strain on their compromised joint structures [6]. This can lead to improper fitting of the denture, increased wear and damage, and decreased patient satisfaction and quality of life. Only after assessing the patient’s psychological state and being sure of their acceptance of a removable rehabilitation will it be possible to proceed to the subsequent phases [6,7].
This is followed by detailed dental impressions, which serve as the primary models for creating the dentures. Precise measurements of the maxillary and mandibular arches are taken to establish the spatial relationship between the two, ensuring that the dentures will align correctly during mastication. Additionally, esthetic considerations such as the color, size, and shape of the prosthetic teeth are decided in consultation with the patient, aiming to mimic natural teeth as closely as possible. This meticulous preparation phase is vital for crafting a functional, comfortable, and esthetically pleasing dental prosthesis that meets the specific needs and expectations of the patient.
This technique focuses on possibly rehabilitating an edentulous patient in the shortest possible time to avoid functional and esthetic discomfort. Studies such as those by Jogezai et al. have explored immediate loading protocols, emphasizing the importance of rapid rehabilitation in enhancing patient satisfaction and treatment acceptance [8]. However, the need for a concise yet comprehensive protocol for mobile denture fabrication, especially following dental extractions, remains a subject of clinical interest and scientific inquiry [9,10].
1.2. Materials Used in Removable Prosthesis Fabrication
Fabricating removable dental prostheses involves various materials, each selected for specific properties contributing to the final product’s functionality, durability, and esthetics. The primary materials include dental polymers, metals, ceramics, and composite materials [11,12,13,14,15].
1.2.1. Dental Polymers
Polymethylmethacrylate (PMMA) is a widely used material for denture bases. It is chosen for its ease of manipulation, acceptable color stability, and compatibility with the oral environment. PMMA’s properties include good esthetic qualities, such as translucency and color options that mimic natural gum tissue, and adequate mechanical strength. However, it can be prone to fracture under high impact and may undergo dimensional changes over time due to water absorption [16,17].
1.2.2. Metals
Metals used in removable prostheses include cobalt–chrome alloys, stainless steel, and sometimes gold. These materials are used mainly in the framework of partial dentures or for clasps and attachments. Metals offer high strength, rigidity, and resistance to wear and deformation, which are crucial for the structural integrity of partial dentures. Cobalt–chrome alloys are particularly valued for their favorable mechanical properties, biocompatibility, and minimal allergic potential [18].
1.2.3. Ceramics
Ceramic materials, such as porcelain, are sometimes used for artificial teeth in dentures due to their exceptional esthetic qualities, including color stability and resistance to wear. Porcelain teeth provide a high degree of natural appearance due to their translucency and color-matching capabilities. However, their brittleness and the potential for abrasion to opposing natural teeth limit their use [19,20].
1.2.4. Composite Materials
Dental composites are increasingly being used for artificial teeth and modifications or repairs to dentures. These materials offer an excellent balance between esthetics and mechanical properties, with improved wear resistance compared to acrylic teeth and better impact strength than porcelain. Composites can be easily adjusted and polished, making them ideal for intraoral modifications [21,22,23].
1.2.5. Soft Liners
Soft liner materials, including silicone-based materials and soft acrylics, are used to improve the comfort of dentures, especially in cases with bony undercuts or sensitive tissues. These materials can absorb masticatory forces, reducing pressure points and improving the distribution of occlusal loads [24].
1.3. Articulators
Articulators in prosthodontics are mechanical devices used for simulating the temporomandibular joint and jaw movements, aiding in the accurate fabrication of dental prostheses, including mobile dentures. There are several types, ranging from simple to highly complex:
1. Non-adjustable or simple articulators can replicate basic opening and closing movements. They are used for simple restorations that do not require extensive occlusal detailing.
2. Semi-adjustable articulators can simulate more natural jaw movements, including lateral and protrusive movements. They are used for more complex restorations, balancing functionality and cost.
3. Fully adjustable articulators: These replicate the full range of mandibular movements and can be customized to match the patient’s specific jaw movements, which are recorded via face-bow transfers and other measurements. They are used for the most complex and precise dental restorations, including high-end mobile dentures, where occlusal harmony and function are crucial.
4. Virtual or digital articulators: with the advancement of digital dentistry, virtual articulation software simulates jaw movements digitally, allowing for precise design and fabrication of dentures using CAD/CAM technologies [25,26,27].
Each type of articulator has its specific use, depending on the complexity of the dental prosthesis being fabricated and the level of occlusal detail required.
1.4. Aim
The present manuscript introduces a novel two-step technique aimed at streamlining the process of mobile denture fabrication post-extraction, potentially redefining the conventional timelines and procedures of removable prosthodontics. Its primary aim is to reduce the number of clinical visits required, thus enhancing patient satisfaction and potentially improving prosthodontic outcomes. By integrating occlusal registration and immediate impression techniques immediately post-extraction, the technique captures optimal alveolar ridge morphology, which is crucial for the functional and esthetic success of the dentures. This approach promises to maintain high standards of care and streamline the overall treatment timeline, offering a more efficient and patient-centered approach to prosthodontic rehabilitation.
2. Materials and Equipment
In standard procedures, the realization of a removable prosthodontic appliance is a meticulous multi-step process, combining clinical assessments and dental laboratory techniques to create a functional and esthetically pleasing dental prosthesis. A detailed patient evaluation and preliminary impressions are initially obtained to develop diagnostic models. These models help in the accurate planning of the prosthesis. Following this, definitive impressions are made using specialized materials to capture an exact negative of the oral structures used to create master casts. Subsequent steps involve recording the jaw’s relations to establish the spatial relationship between the maxillary and mandibular arches, which is crucial for the correct alignment of prosthetic teeth. Artificial teeth are then selected and arranged based on esthetic and functional criteria, ensuring that they mimic natural teeth as closely as possible in size, shape, and color. A trial insertion follows, where a wax model of the denture set is tested within the patient’s mouth, allowing for necessary adjustments before the final processing. This phase transitions into the processing and finishing of the denture, where the wax model is converted into the actual prosthesis using materials like acrylic resin. After thorough polishing and refinements, the prosthesis is ready for delivery. The final steps include post-insertion adjustments to optimize comfort and functionality, ensuring the integration of the prosthesis into the patient’s daily life. This comprehensive approach strives to restore the patient’s masticatory function and esthetics. It emphasizes minimizing clinic visits and enhancing overall treatment efficiency, underscoring the evolution of modern prosthodontics toward patient-centered care [5,28].
The proposed technique for mobile denture fabrication encompasses two pivotal steps that are strategically designed to optimize clinical efficiency while ensuring prosthetic precision and patient comfort using standard materials (Table 1) (Figure 1, Figure 2, Figure 3, Figure 4 and Figure 5).

Table 1.
The first column shows the different phases. The second column shows the detailed procedures. The third column shows the main author of each procedure.
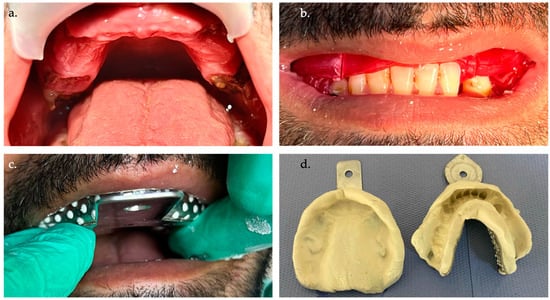
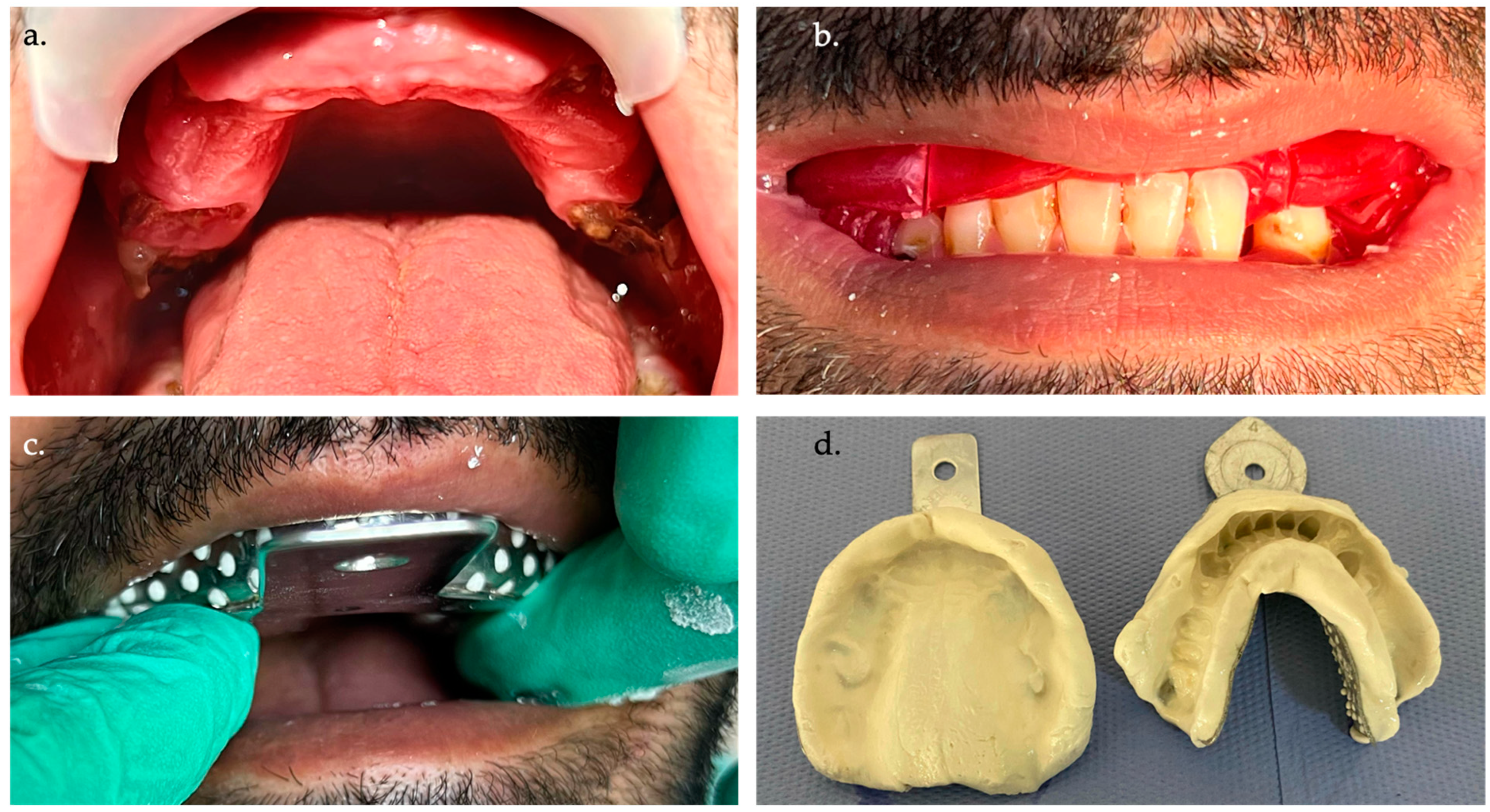
Figure 1.
(a) Intraoral photo of the patient at the first appointment in the pre-dental extraction phase. (b) Centric registration with red wax in the pre-extraction phase. (c) The patient undergoes an alginate impression of the dental arches. (d) Cleaned and disinfected impressions are ready to be sent to the dental laboratory.
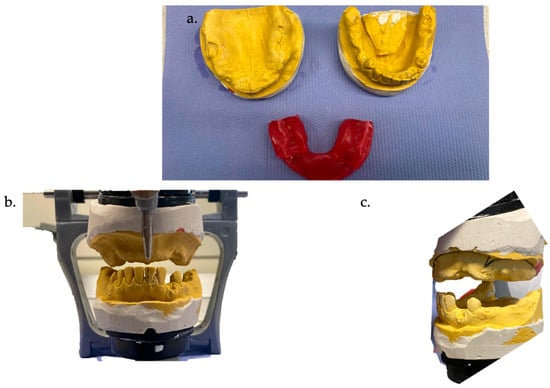
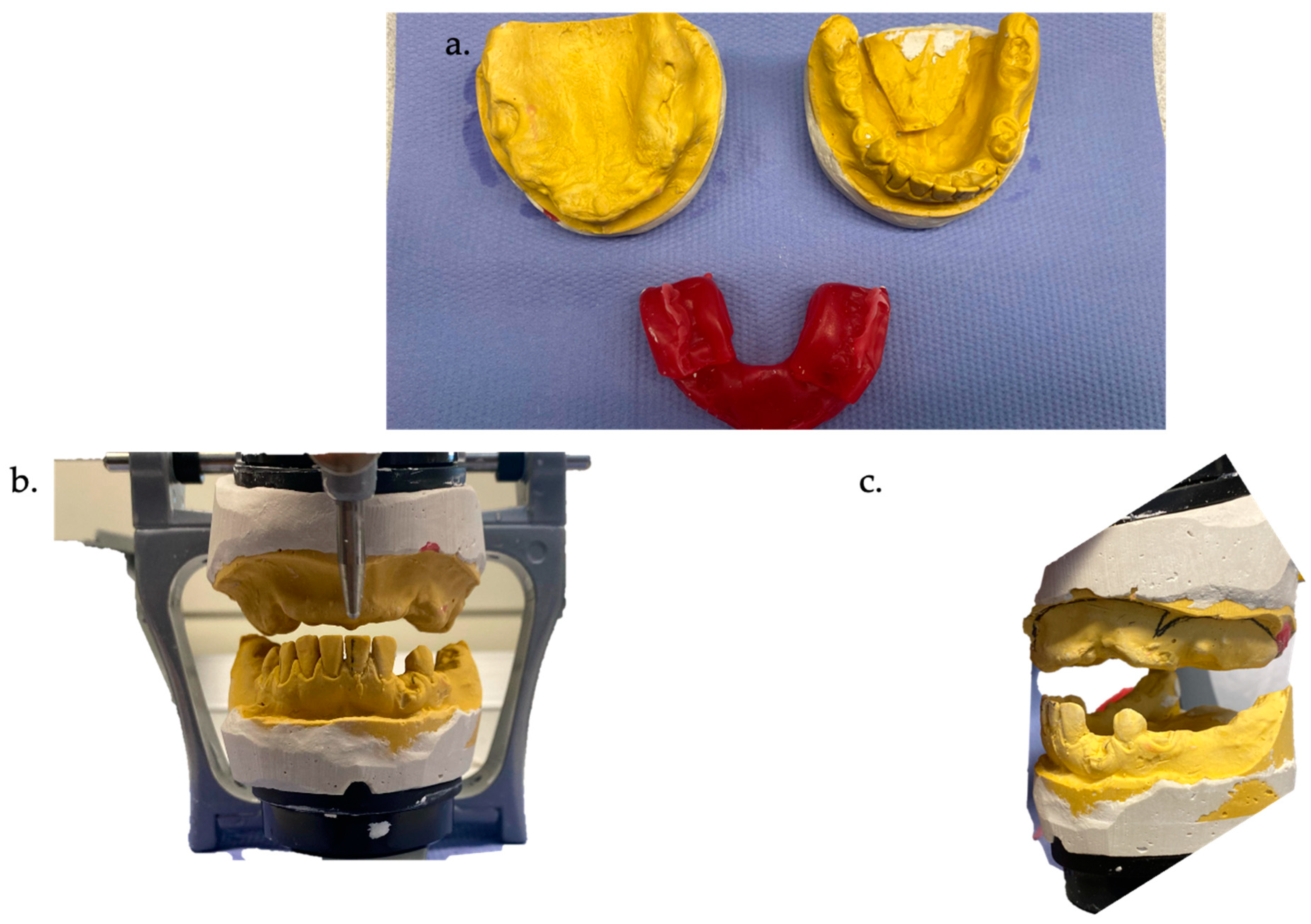
Figure 2.
(a) Dental models in plaster and red wax with first centric registration. (b) Dental models mounted in articulator front view. (c) Dental models mounted in articulator lateral view.

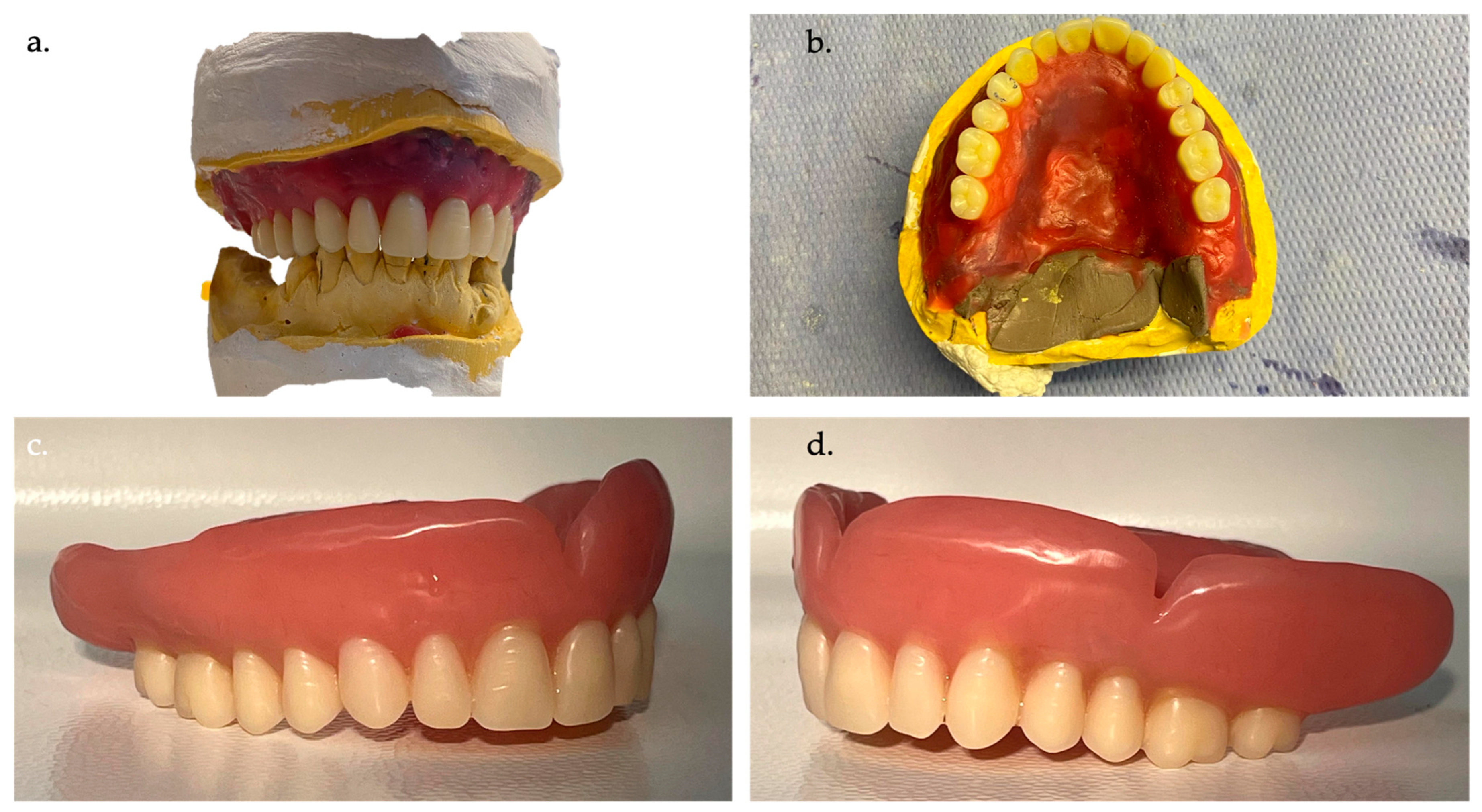
Figure 3.
(a) Test teeth with resin base in position; the wax rims in the lateral posterior sector are evident. The functional and esthetic test is satisfactory, considering the single step up to this point. (b) Relining the resin base with polysulfide material is performed with trial assembly and simultaneous occlusal and mucosal functionalization (heated wax rims). (c) Resin base with polymerized material, front view. (d) Resin base with polymerized material, palatal view.
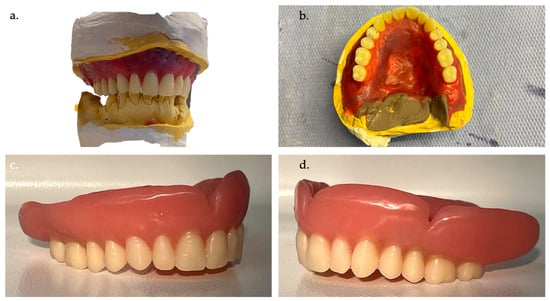
Figure 4.
(a) The assembly of the new plaster model obtained in the definitive articulator shows that the dental technician has already assembled the teeth in the lateral posterior sectors. (b) Occlusal view of the resin base with relining material (polysulphide) during the creation of the definitive model. (c) Completed removable total prosthesis, right side view. (d) Completed removable total prosthesis, left lateral view.

Figure 5.
(a) Completed removable total prosthesis, front view. (b,c) Delivered denture.
3. Detailed Procedures
The patient comes to our observation requesting a removable rehabilitation of the upper arch. Patient ASA2 has no contraindications to the treatment and does not complain of painful symptoms in the oral cavity. He does not report any anomalies, noises, or pain during chewing attributed to TMJ pathologies. Upon intraoral physical examination, the patient presents with several root residues in the upper arch. The lower arch presents a condition of oligodontia and does not require treatment. In the first step, an occlusal registration is performed immediately following the extraction of the designated teeth. This step is crucial for capturing the precise occlusal relationships and vertical dimensions of occlusion, which are fundamental for the functional success of the prosthesis. The occlusal registration is conducted during the same appointment as the extraction of the teeth, thereby reducing the number of clinical visits. If the patient is already edentulous or his vertical height is significantly altered, following this protocol will be much more difficult. This is followed by an alginate dental impression immediately after extracting the remaining teeth. This approach not only streamlines the clinical workflow but also capitalizes on the residual alveolar ridge morphology before significant resorption occurs, a concept supported by studies emphasizing the importance of immediate impressions in capturing the optimal ridge anatomy [29].
It is necessary to report as much information as possible on the first wax block, such as the midline and the smile line. At this point, the dental technician can mount the plaster models obtained from our dental impressions in the articulator. This assembly will follow the occlusal registration obtained through the first wax mark; this will allow the dental technician to carry out a first assembly of the teeth on the resin base of the prosthesis, using the front sector only, respecting the color taken during the first session.
The dental technician will create a wax base on the plaster model obtained to assemble the dental elements blocked in wax. However, a wax rim will remain in the posterior and lateral posterior sectors, which will be used for occlusal registration during the second step [30].
Having obtained this rigid resin base with the teeth of the frontal sector mounted, it will be possible to proceed with carrying out all the esthetic and phonetic tests, evaluating the function of the canine and incisor guides and, above all, the median and canine line from an esthetic point of view. A precise and reliable centric position will be obtained by heating the wax rims of the posterior sector and bringing the patient into the centric position. If the teeth in the frontal sector are not congruent with the occlusion, they will be adapted, or if this is not possible, the protocol will start again with a new wax rim positioned on the resin base once the teeth have been removed.
Having ensured the absence of any pain reported by the patient during the tests and a stable position of the resin base on the palate, it will be possible to proceed with the precision impression that will be functionalized with polysulphide-based pastes [31,32,33,34]. Polysulfides are hydrophobic elastomers of natural origin with a relatively low cost, excellent tear resistance, and viscoelastic characteristics. They also have a long polymerization time, which allows the detection of secondary mucodynamic impressions in totally or partially edentulous patients. It is a material often criticized for its difficult processing and organoleptic characteristics. The poor dimensional stability of the material requires the technician to pour the impressions within 30 min of removal from the oral cavity [35].
The impression material is then kneaded and placed on the resin base, closing the patient in a centric position and functionalizing the soft tissues (mucosa of the lips and the genials). The resin base with the polymerized impression material can be removed, and the patient can proceed to the last delivery step.
The prosthesis can thus be delivered following an occlusal and esthetic check. The post-extraction mucous membranes and alveoli will not yet have reached complete maturation and healing, but this allows the patient to have a full set of teeth and restore function and esthetics within a few days.
4. Expected Results
4.1. Clinical Implications
The choice of material for a removable prosthesis has significant implications for clinical outcomes. Dentists must consider the patient’s specific needs, including the condition of the oral tissues, masticatory efficiency, esthetic preferences, and any allergies or sensitivities. The longevity and success of a removable prosthesis also depend on proper maintenance by the patient, including regular cleaning and avoiding practices that could damage the prosthesis, such as using it to open bottles or chewing hard foods.
Creating a removable prosthodontic with standard protocols involves meticulously detailed procedures that span several critical steps designed to ensure that the prosthesis meets both functional and esthetic requirements for the patient. This process typically encompasses the following:
1. Patient evaluation and preliminary impressions: initial consultation and assessment of the patient’s oral health status are conducted, followed by taking preliminary impressions of the arches to create diagnostic models;
2. Definitive impressions and master cast fabrication: this entails using more precise impression materials to capture detailed oral structures to create master casts;
3. Jaw relation records: this entails determining and recording the spatial relationship between the upper and lower jaws to guide the proper alignment of the denture teeth;
4. Selection and arrangement of denture teeth: the appropriate size, shape, and color of artificial teeth are chosen based on esthetic and occlusal requirements, and this is followed by their precise arrangement;
5. Trial insertion: this is a test fitting of the denture with the arranged teeth set in wax, allowing for adjustments in esthetics and occlusion before final processing;
6. Processing and finishing: this is the conversion of the wax denture into its final form by replacing the wax with a denture base material, usually acrylic resin, which is followed by polishing and finishing touches;
7. Delivery and post-insertion adjustments: the finished denture is handed to the patient, followed by making necessary adjustments to enhance comfort and function, ensuring satisfactory integration into the oral cavity [36,37,38].
Each step requires detailed attention to technical and clinical details, ensuring that the final prosthesis meets the patient’s function, comfort, and appearance needs. From a clinical perspective, this approach significantly reduces the number of patient visits required, directly enhancing patient convenience and satisfaction. Financially, by optimizing materials and reducing chair time, the technique potentially lowers the overall cost of denture fabrication for patients. For clinicians, the technique offers a more efficient workflow, allowing for rapid prosthodontic rehabilitation while maintaining high standards of care. This innovative method redefines conventional timelines and procedures in removable prosthodontics, emphasizing efficiency and patient-centered care.
4.2. Literature Discussions
The innovative two-step technique for mobile denture fabrication presents a significant advancement in removable prosthodontics, potentially setting a new standard for efficiency and patient-centered care. One of the most notable advantages of this technique is the reduction in the number of clinical visits, which directly correlates with patient convenience and satisfaction. Additionally, by performing the impression immediately post-extraction, the technique harnesses the most favorable ridge anatomy, potentially enhancing the stability and retention of the final denture. The strategic timing of the occlusal registration also ensures that the vertical dimension of the occlusion is accurately captured, a crucial determinant of the functional and esthetic success of the prosthesis. However, it is imperative to consider this technique’s potential limitations and challenges. The condensed timeline necessitates meticulous clinical execution and may leave limited room for error correction. The immediate post-extraction phase is also characterized by tissue inflammation and healing dynamics, which may introduce variables that could impact the final denture fit and comfort. Comparative studies, such as those by Heartwell et al. [39], have emphasized the importance of considering the biological and healing factors in immediate denture protocols. Therefore, while the proposed two-step protocol offers substantial benefits, it requires a high level of clinical expertise and a thorough understanding of the biological processes involved in post-extraction healing.
Cherkashin BF et al. [40] developed a protocol for setting artificial teeth in completely removable prosthodontics without bite ridge landmarks based on comprehensive dentistry literature and clinical experience, leading to more efficient prosthesis fabrication for patients with complete secondary dementia. Von Stein-Lausnitz M et al. [41] conducted a double-blinded randomized controlled trial to assess the impact of face-bow registration on occlusal parameters in complete denture remounting, revealing no substantial differences between face-bow and mean setting methods in changing the vertical dimension [42]. Steinmassl PA et al. [43] evaluated various CAD/CAM denture systems, highlighting these technologies’ potential to reduce patient visits and improve denture adaptation, with each system offering unique advantages based on the dentist’s expertise and patient needs. Alhallak KR et al. [44] review the use of 3D printing technologies for manufacturing removable prosthodontics, focusing on advantages like time efficiency, satisfying clinical outcomes, and securing patient records while noting challenges such as material strength, esthetics, and biocompatibility, urging further studies. Suzuki Y et al. [45] analyze the laboratory efficiency of additive manufacturing for removable prosthodontic frameworks, comparing surface roughness, fitness accuracy, and retentive forces with conventional methods, finding areas where additive manufacturing falls short or matches traditional techniques. Davda K et al. [46] investigated the trueness and precision of copy denture templates made via conventional and 3D printing methods, finding that 3D-printed templates significantly improved trueness and accuracy over traditional methods, highlighting the potential of 3D printing in dental prosthetics. Bilgin MS et al. [47] review CAD/CAM and rapid prototyping technologies for removable prosthodontic fabrication, covering technological advancements, techniques, and the transition towards digital planning and manufacturing while noting current limitations and the need for technical expertise in traditional methods. In their clinical study, Lo Russo et al. assessed the accuracy of a two-step scanning strategy for intraoral scans of edentulous mandibular arches, comparing these with conventional polysulfide impressions. The results showed no significant distortion or differences in 3D deviations when comparing the scans to the impressions, indicating the reliability of the two-step scanning method. However, the analysis revealed significant regional variations, although these did not differ significantly between corresponding regions on both arch sides [48].
Accurate diagnosis and thorough analysis of temporomandibular disorders (TMDs) are essential before the fabrication of removable dentures. TMDs can significantly affect dentures’ masticatory function, comfort, and overall success. The temporomandibular joint (TMJ) acts as a crucial interface in the biomechanics of mastication, which is directly influenced by the occlusal dynamics introduced by dentures [49]. In a systematic review, Nimonkar et al. [50] critically examine five peer-reviewed articles selected based on temporomandibular disease and removable dentures. These articles suggest that complete dentures, particularly when carefully designed to restore the vertical dimension and proper occlusal relationships, can significantly alleviate TMD symptoms in edentulous patients. Despite the inherent limitations of the data due to study heterogeneity, the findings advocate for the therapeutic role of complete dentures in potentially reversing TMD-related manifestations, enhancing masticatory function, and improving overall quality of life for edentulous individuals. The discussions within the review emphasize the necessity for well-fabricated dentures and highlight that while current studies support the benefits of dentures in TMD management, further high-quality randomized clinical trials are required to solidify these findings and optimize treatment protocols. This review provides a foundational perspective on the intersection of prosthodontics and temporomandibular health, pointing towards a nuanced understanding of the biomechanical and rehabilitative interactions facilitated by complete dentures in managing TMDs [49,50,51].
The two-step technique described herein for fabricating mobile dentures immediately post-extraction is designed to address current challenges in prosthodontic rehabilitation, particularly the need for rapid restoration of function and esthetics with minimal clinic visits. This technique leverages advanced material selection and streamlined clinical procedures to optimize treatment outcomes and patient satisfaction. In daily dental practice, the introduction of this technique has the potential to significantly influence the approach to denture fabrication. By reducing the number of patient visits and treatment duration, dental practitioners can enhance the efficiency of their practice and patient throughput. The materials used, including dental polymers, metals, ceramics, and composites, are selected for their durability, esthetic qualities, and biocompatibility, ensuring that the final prosthesis meets both functional and esthetic requirements [16,48].
It is crucial to understand that the success of this innovative technique hinges not only on the materials and technologies used but also on the meticulous execution of clinical and laboratory steps. The educational takeaway is the importance of a thorough understanding of material properties and the appropriate application of clinical techniques to optimize the outcome of the prosthesis. The two-step technique offers a rapid, efficient solution compared to traditional methods. However, it requires precise execution and coordination between the dental team and laboratory technicians. The primary limitation is the dependency on the clinician’s skill and the patient’s oral condition at the time of extraction, which can vary widely and affect the fit and function of the immediate denture.
In contrast, digital techniques, such as CAD/CAM and 3D printing, provide high precision and reproducibility without the same level of operator dependency. These methods allow for the creation of dentures with consistent quality and fit utilizing digital impressions that can be archived and reused for future prostheses. However, digital methods can be cost-prohibitive and require significant investments in technology and training. The aspect of sustainability in prosthodontic practices, particularly through the selection of materials and techniques, is increasingly important [13,14,29,36,51]. Moreover, the durability of the selected materials reduces the frequency of prosthesis replacement, thereby decreasing waste and promoting sustainability in dental practice.
4.3. Limitations
The technique presented here has different limitations, some absolute and some relative to the case. Those relating to the case are linked to the fact that the patient does not have intact dental elements but only root residues. Therefore, this could make occlusal registration more difficult. Furthermore, the patient is partially edentulous in the posterior sectors of the lower arch, which could facilitate delivery. Regarding the absolute limits, we must consider the need for a specific learning curve to carry out this technique. Materials such as polysulfide-based pastes are complex in their use and functionalization. The wax block must always be created first and used at the first meeting by the clinician. Suppose there are many extractions to be performed. In that case, it is necessary to record the occlusion in such a way as to obtain contact with both the mucosa and the teeth, then record the centricity after several extractions. The first dental assembly is highly operator-dependent and may not be suitable for the second step. The resin base with the dental test remains inside the resin, which is positioned in the flask.
5. Conclusions
The novel two-step technique for mobile denture fabrication post-extraction marks a significant leap forward in removable prosthodontics. By consolidating the clinical steps and harnessing the immediate post-extraction phase for impression and occlusal registration, this technique offers a promising avenue for rapid, efficient, and patient-centric prosthodontic rehabilitation. The reduction in clinical visits and the strategic use of immediate post-extraction tissue morphology underscore the patient-centered approach of this technique. However, the success of this innovative method hinges on meticulous clinical execution and a profound understanding of tissue dynamics post-extraction. Future research and clinical trials are warranted to validate this technique further, explore its long-term outcomes, and establish its position in the repertoire of prosthodontic treatment options. The potential for integrating advanced materials and technologies such as CAD and 3D printing into this technique could also be investigated, which would further enhance the precision and customization of dentures, particularly in terms of occlusal registration. This technique’s possibilities to redefine the standards of care in removable prosthodontics are immense, promising a new era of efficiency and patient satisfaction in dental rehabilitation.
Author Contributions
Conceptualization, L.F. and G.C.; methodology, L.F., F.G., M.V., E.P. and S.V.; software, not applicable; validation, L.F., C.D. and G.C.; formal analysis, L.F. and V.R.; investigation, L.F.; resources, L.F.; data curation, L.F.; writing—original draft preparation, L.F.; writing—review and editing, L.F. and G.C.; visualization, L.F.; supervision, G.C.; project administration, L.F.; funding acquisition, G.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study because the implementation of this technique did not harm or cause harm to any human being; in any case, the materials used are already in use in dentistry.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The full data are available in the manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Tsunoda, A.; Kanazawa, H.; Ishige, T.; Kishimoto, S. A missing denture. Lancet 2004, 364, 1884. [Google Scholar] [CrossRef] [PubMed]
- Fiorillo, L.; Cervino, G.; de Stefanq, R.; Iannellq, G.; Cicciu, M. Socioeconomic behaviors on dental professions: A Google Trends investigation in Italy. Minerva Stomatol. 2020, 69, 309–316. [Google Scholar] [CrossRef] [PubMed]
- Dai, M.; Song, Q.; Lin, T.; Huang, X.; Xie, Y.; Wang, X.; Zheng, L.; Yue, J. Corrigendum: Tooth loss, denture use, and all-cause and cause-specific mortality in older adults: A community cohort study. Front. Public Health 2023, 11, 1360927. [Google Scholar] [CrossRef] [PubMed]
- Palomer, T.; Ramírez, V.; Ortuño, D. Relationship between oral health and depression: Data from the National Health Survey 2016–2017. BMC Oral Health 2024, 24, 188. [Google Scholar] [CrossRef] [PubMed]
- Campbell, S.D.; Cooper, L.; Craddock, H.; Hyde, T.P.; Nattress, B.; Pavitt, S.H.; Seymour, D.W. Removable partial dentures: The clinical need for innovation. J. Prosthet. Dent. 2017, 118, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Furquim, B.D.; Flamengui, L.M.; Conti, P.C. TMD and chronic pain: A current view. Dent. Press J. Orthod. 2015, 20, 127–133. [Google Scholar] [CrossRef]
- Galletti, C.; Lombardo, C.; La Barbiera, C.; Boronat-Català, M.; Almiñana-Pastor, P.J.; Sala Fernàndez, C.; Ramírez-Sebastià, A.; Muscatello, M.R.; Bruno, A.; Mento, C. Dental anxiety, Quality of Life and body image: Gender differences in Italian and Spanish population. Minerva Dent. Oral Sci. 2024, 73, 14–19. [Google Scholar] [CrossRef]
- Jogezai, U.; Laverty, D.; Walmsley, A. Immediate dentures part 1: Assessment and treatment planning. Dent. Update 2018, 45, 617–624. [Google Scholar] [CrossRef]
- Wang, C.; Gao, M.; Yu, Y.; Zhang, W.; Peng, X. Clinical analysis of denture rehabilitation after mandibular fibula free-flap reconstruction. Beijing Da Xue Xue Bao Yi Xue Ban 2024, 56, 66–73. [Google Scholar]
- Sokolowski, A.; Horak, D.; Behlau, A.; Madreiter-Sokolowski, C.; Lorenzoni, M.; Sokolowski, A. Evaluation of two printing techniques for maxillary removable partial denture frameworks. J. Prosthet. Dent. 2024, 131, 707.e1–707.e8. [Google Scholar] [CrossRef]
- Kim, M.C.; Byeon, D.J.; Jeong, E.J.; Go, H.B.; Yang, S.Y. Color stability, surface, and physicochemical properties of three-dimensional printed denture base resin reinforced with different nanofillers. Sci. Rep. 2024, 14, 1842. [Google Scholar] [CrossRef] [PubMed]
- Alhotan, A.; Raszewski, Z.; Chojnacka, K.; Mikulewicz, M.; Kulbacka, J.; Alaqeely, R.; Mirdad, A.; Haider, J. Evaluating the Translucency, Surface Roughness, and Cytotoxicity of a PMMA Acrylic Denture Base Reinforced with Bioactive Glasses. J. Funct. Biomater. 2023, 15, 16. [Google Scholar] [CrossRef] [PubMed]
- Yan, S.; Zhou, J.L.; Zhang, R.J.; Tan, F.B. Evaluation of the influence of different build angles on the surface characteristics, accuracy, and dimensional stability of the complete denture base printed by digital light processing. Heliyon 2024, 10, e24095. [Google Scholar] [CrossRef] [PubMed]
- Papathanasiou, I.; Kamposiora, P.; Papavasiliou, G.; Ferrari, M. The use of PEEK in digital prosthodontics: A narrative review. BMC Oral Health 2020, 20, 217. [Google Scholar] [CrossRef] [PubMed]
- Cervino, G.; Cicciù, M.; Herford, A.S.; Germanà, A.; Fiorillo, L. Biological and chemo-physical features of denture resins. Materials 2020, 13, 3350. [Google Scholar] [CrossRef] [PubMed]
- Yerliyurt, K.; Tasdelen, T.B.; Egri, O.; Egri, S. Flexural Properties of Heat-Polymerized PMMA Denture Base Resins Reinforced with Fibers with Different Characteristics. Polymers 2023, 15, 3211. [Google Scholar] [CrossRef]
- Garcia, A.; Sugio, C.Y.C.; de Azevedo-Silva, L.J.; Gomes, A.C.G.; Batista, A.U.D.; Porto, V.C.; Soares, S.; Neppelenbroek, K.H. Nanoparticle-modified PMMA to prevent denture stomatitis: A systematic review. Arch. Microbiol. 2021, 204, 75. [Google Scholar] [CrossRef] [PubMed]
- Ananya; Rani, P.; Sinha, T.; Prakash, J. Maxillary Cast Partial Denture and Mandibular Implant-Supported Metal-Ceramic Prosthesis with a Split Framework to Compensate for Mandibular Flexure: A Case Report. Cureus 2023, 15, e49071. [Google Scholar] [CrossRef]
- Kancyper, S.; Sierraalta, M.; Razzoog, M.E. All-ceramic surveyed crowns for removable partial denture abutments. J. Prosthet. Dent. 2000, 84, 400–402. [Google Scholar] [CrossRef]
- Yoon, T.H.; Madden, J.C.; Chang, W.G. A technique to restore worn denture teeth on a partial removable dental prosthesis by using ceramic onlays with CAD/CAM technology. J. Prosthet. Dent. 2013, 110, 331–332. [Google Scholar] [CrossRef]
- Pavarina, A.C.; Machado, A.L.; Vergani, C.E.; Giampaolo, E.T. Preparation of composite retentive areas for removable partial denture retainers. J. Prosthet. Dent. 2002, 88, 218–220. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, K.A.; Janzen, J.; Brackett, W.W.; Romero, M.F. Prototyping of increased vertical dimension of occlusion using an existing removable partial denture and composite resin: A case report. Gen. Dent. 2023, 71, 72–76. [Google Scholar] [PubMed]
- Mete, J.J.; Dange, S.P.; Khalikar, A.N.; Vaidya, S.P. Rehabilitation of anterior edentulous space by glass fiber reinforced composite removable partial denture during preadolescent period: A case report. J. Indian Prosthodont. Soc. 2011, 11, 195–198. [Google Scholar] [CrossRef] [PubMed]
- Whitsitt, J.A.; Battle, L.W.; Jarosz, C.J. Enhanced retention for the distal extension-base removable partial denture using a heat-cured resilient soft liner. J. Prosthet. Dent. 1984, 52, 447–448. [Google Scholar] [CrossRef] [PubMed]
- Aljohani, A.O.; Sghaireen, M.G.; Abbas, M.; Alzarea, B.K.; Srivastava, K.C.; Shrivastava, D.; Issrani, R.; Mathew, M.; Alsharari, A.H.L.; Alsharari, M.A.D.; et al. Comparative Evaluation of Condylar Guidance Angles Measured Using Arcon and Non-Arcon Articulators and Panoramic Radiographs—A Systematic Review and Meta-Analysis. Life 2023, 13, 1352. [Google Scholar] [CrossRef]
- Palaskar, J.N.; Joshi, N.P.; Hindocha, A.D.; Gunjal, A.P.; Balsaraf, K.D. Evaluation of Sagittal Inclination of Occlusal Plane and Horizontal Condylar Guidance Using Various Anterior Reference Points on Arcon and Nonarcon Articulators. Contemp. Clin. Dent. 2022, 13, 255–260. [Google Scholar] [CrossRef]
- Lepidi, L.; Galli, M.; Mastrangelo, F.; Venezia, P.; Joda, T.; Wang, H.L.; Li, J. Virtual Articulators and Virtual Mounting Procedures: Where Do We Stand? J. Prosthodont. 2021, 30, 24–35. [Google Scholar] [CrossRef]
- Cervino, G.; Sambataro, S.; Stumpo, C.; Bocchieri, S.; Murabito, F.; Fiorillo, L.; Meto, A.; Zecca, P.A.; Caprioglio, A.; Cicciù, M. Determination of the vertical dimension and the position of the occlusal plane in a removable prosthesis using cephalometric analysis and golden proportion. Appl. Sci. 2021, 11, 6948. [Google Scholar] [CrossRef]
- Baek, M.-W.; Lim, H.-C.; Noh, K.; Choi, S.-H.; Lee, D.-W. Dimensional Changes in Extraction Sockets: A Pilot Study Evaluating Differences between Digital and Conventional Impressions. Appl. Sci. 2022, 12, 7662. [Google Scholar] [CrossRef]
- Beckett, L.S. Accurate occlusal relations in partial denture construction. J. Prosthet. Dent. 1954, 4, 487–495. [Google Scholar] [CrossRef]
- Smith, P.K. The effect on the accuracy of polysulphide impression material after treating preparations with various agents. Aust. Dent. J. 1971, 16, 337–339. [Google Scholar] [CrossRef] [PubMed]
- Tolley, L.G.; Craig, R.G. Viscoelastic properties of elastomeric impression materials: Polysulphide, silicone and polyether rubbers. J. Oral Rehabil. 1978, 5, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Darvell, B.W. Aspects of the chemistry of polysulphide impression material. Aust. Dent. J. 1987, 32, 357–367. [Google Scholar] [CrossRef] [PubMed]
- Peroz, I. The dimensional stability of polyether, polysulphide and silicone impression materials as well as the hardness of casts after disinfection. Dtsch. Zahnarztl. Z. 1988, 43, 1066–1071. [Google Scholar] [PubMed]
- Al-Ansari, A. Which final impression technique and material is best for complete and removable partial dentures? Evid.-Based Dent. 2019, 20, 70–71. [Google Scholar] [CrossRef] [PubMed]
- Goncalves, T.; Forgerini, G.; Drummond, L.B.; Wanghon, Z.M.L.; Carmo Filho, L.C.D.; Philippi, A.G. Digital workflow to produce 3D-printed incisal facial indirect restoration with lingual rest seats to support a removable partial denture. J. Prosthet. Dent. 2023, in press. [Google Scholar] [CrossRef] [PubMed]
- Ciocca, L.; Maltauro, M.; Pierantozzi, E.; Breschi, L.; Montanari, A.; Anderlucci, L.; Meneghello, R. Evaluation of trueness and precision of removable partial denture metal frameworks manufactured with digital technology and different materials. J. Adv. Prosthodont. 2023, 15, 55–62. [Google Scholar] [CrossRef]
- Benyahia, H.; El Benaissi, A.; Bahij, L.; Merzouk, N.; Regragui, A. Impression techniques in Removable partial denture: Epidemiological study. Tunis Med. 2023, 101, 41–46. [Google Scholar]
- Heartwell, C.M.; Salisbury, F.W. Immediate complete dentures: An evaluation. J. Prosthet. Dent. 1965, 15, 615–624. [Google Scholar] [CrossRef]
- Cherkashin, B.F.; Furtsev, T.V. Protocol for teeth set-up in full denture without the use of wax rims and its theoretical justification. Stomatologiia 2023, 102, 50–55. [Google Scholar] [CrossRef]
- von Stein-Lausnitz, M.; Sterzenbach, G.; Helm, I.; Zorn, A.; Blankenstein, F.H.; Ruge, S.; Kordaß, B.; Beuer, F.; Peroz, I. Does a face-bow lead to better occlusion in complete dentures? A randomized controlled trial: Part I. Clin. Oral Investig. 2018, 22, 773–782. [Google Scholar] [CrossRef] [PubMed]
- Risciotti, E.; Squadrito, N.; Montanari, D.; Iannello, G.; Macca, U.; Tallarico, M.; Cervino, G.; Fiorillo, L. Digital Protocol to Record Occlusal Analysis in Prosthodontics: A Pilot Study. J. Clin. Med. 2024, 13, 1370. [Google Scholar] [CrossRef] [PubMed]
- Steinmassl, P.A.; Klaunzer, F.; Steinmassl, O.; Dumfahrt, H.; Grunert, I. Evaluation of Currently Available CAD/CAM Denture Systems. Int. J. Prosthodont. 2017, 30, 116–122. [Google Scholar] [CrossRef] [PubMed]
- Alhallak, K.R.; Nankali, A. 3D Printing Technologies for Removable Dentures Manufacturing: A Review of Potentials and Challenges. Eur. J. Prosthodont. Restor. Dent. 2022, 30, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, Y.; Shimizu, S.; Waki, T.; Shimpo, H.; Ohkubo, C. Laboratory efficiency of additive manufacturing for removable denture frameworks: A literature-based review. Dent. Mater. J. 2021, 40, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Davda, K.; Osnes, C.; Dillon, S.; Wu, J.; Hyde, P.; Keeling, A. An Investigation into the Trueness and Precision of Copy Denture Templates Produced by Rapid Prototyping and Conventional Means. Eur. J. Prosthodont. Restor. Dent. 2017, 25, 186–192. [Google Scholar] [CrossRef] [PubMed]
- Bilgin, M.S.; Baytaroğlu, E.N.; Erdem, A.; Dilber, E. A review of computer-aided design/computer-aided manufacture techniques for removable denture fabrication. Eur. J. Dent. 2016, 10, 286–291. [Google Scholar] [CrossRef]
- Lo Russo, L.; Sorrentino, R.; Esperouz, F.; Zarone, F.; Ercoli, C.; Guida, L. Assessment of distortion of intraoral scans of edentulous mandibular arch made with a 2-step scanning strategy: A clinical study. J. Prosthet. Dent. 2023, in press. [Google Scholar] [CrossRef]
- Minervini, G.; Fiorillo, L.; Russo, D.; Lanza, A.; D’Amico, C.; Cervino, G.; Meto, A.; Di Francesco, F. Prosthodontic Treatment in Patients with Temporomandibular Disorders and Orofacial Pain and/or Bruxism: A Review of the Literature. Prosthesis 2022, 4, 253–262. [Google Scholar] [CrossRef]
- Nimonkar, S.; Godbole, S.; Belkhode, V.; Nimonkar, P.; Pisulkar, S. Effect of Rehabilitation of Completely Edentulous Patients with Complete Dentures on Temporomandibular Disorders: A Systematic Review. Cureus 2022, 14, e28012. [Google Scholar] [CrossRef]
- Santos, M.; Azevedo, L.; Fonseca, P.; Viana, P.; Araújo, F.; Villarinho, E.; Fernandes, G.; Correia, A. The Success Rate of the Adhesive Partial Fixed Prosthesis after Five Years: A Systematic Review. Prosthesis 2023, 5, 282–294. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).