The Freehand Technique: The Ability of the Human Eye to Identify Implant Sites on the Patient
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Orentlicher, G.; Horowitz, A.; Abboud, M. Computer-guided implant surgery: Indications and guidelines for use. Compend. Contin. Educ. Dent. 2012, 33, 720–732. [Google Scholar] [PubMed]
- D’Haese, J.; Ackhurst, J.; Wismeijer, D.; De Bruyn, H.; Tahmaseb, A. Current state of the art of computer-guided implant surgery. Periodontology 2017, 73, 121–133. [Google Scholar] [CrossRef] [PubMed]
- Nickenig, H.J.; Wichmann, M.; Hamel, J.; Schlegel, K.A.; Eitner, S. Evaluation of the difference in accuracy between implant placement by virtual planning data and surgical guide templates versus the conventional free-hand method—A combined in vivo–in vitro technique using cone-beam CT (Part II). J. Cranio Maxillofac. Surg. 2010, 38, 488–493. [Google Scholar] [CrossRef] [PubMed]
- Graham RN, J.; Perriss, R.W.; Scarsbrook, A.F. DICOM demystified: A review of digital file formats and their use in radiological practice. Clin. Radiol. 2005, 60, 1133–1140. [Google Scholar] [CrossRef] [PubMed]
- Kalra, M.; Aparna, I.N.; Dhanasekar, B. Evolution of surgical guidance in implant dentistry. Dent. Update 2013, 40, 577–578, 581–582. [Google Scholar] [CrossRef] [PubMed]
- Kola, M.Z.; Shah, A.H.; Khalil, H.S.; Rabah, A.M.; Harby, N.M.H.; Sabra, S.A.; Raghav, D. Surgical templates for dental implant positioning; current knowledge and clinical perspectives. Niger. J. Surg. 2015, 21, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Scherer, U.; Stoetzer, M.; Ruecker, M.; Gellrich, N.C. See Template-guided vs. non-guided drilling in site preparation of dental implants. Clin. Oral Investig. 2015, 19, 1339–1346. [Google Scholar] [CrossRef] [PubMed]
- Schnutenhaus, S.; Edelmann, C.; Rudolph, H.; Dreyhaupt, J.; Luthardt, R.G. 3D accuracy of implant positions in template-guided implant placement as a function of the remaining teeth and the surgical procedure. A retrospective study. Clin. Oral Investig. 2018, 22, 2363–2372. [Google Scholar] [CrossRef] [PubMed]
- Younes, F.; Cosyn, J.; De Bruyckere, T.; Cleymaet, R.; Bouckaert, E.; Eghbali, A. A randomized controlled study on the accuracy of free-handed, pilot-drill guided and fully guided implant surgery in partially edentulous patients. J. Clin. Periodontol. 2018, 45, 721–732. [Google Scholar] [CrossRef]
- Otaghsara, S.S.; Joda, T.; Thieringer, F.M. Accuracy of dental implant placement using static versus dynamic computer-assisted implant surgery: An in vitro study. J. Dent. 2023, 132, 104487. [Google Scholar] [CrossRef]
- Alqutaibi, A.Y. CAD-CAM surgically-guided oral implant site expansion and implant placement in severely atrophic maxilla. J. Taibah Univ. Med. Sci. 2020, 15, 153–159. [Google Scholar] [CrossRef]
- Gargallo-Albiol, J.; Barootchi, S.; Marqués-Guasch, J.; Wang, H.L. Fully Guided Versus Half-Guided and Freehand Implant Placement: Systematic Review and Meta-analysis. Int. J. Oral Maxillofac. Implant. 2020, 35, 1159–1169. [Google Scholar] [CrossRef]
- Alevizakos, V.; Mitov, G.; Stoetzer, M.; von See, C. A retrospective study of the accuracy of template-guided versus freehand implant placement: A nonradiologic method. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2019, 128, 220–226. [Google Scholar] [CrossRef] [PubMed]
- Behneke, M.; Burwinkel, N. Behneke Factors influencing transfer accuracy of cone beam CT-derived template-based implant placement. Clin. Oral Implant. Res. 2012, 23, 416–423. [Google Scholar] [CrossRef]
- Gargallo-Albiol, J.; Barootchi, S.; Salomó-Coll, O.; Wang, H.L. Advantages anddisadvantages of implant navigation surgery. A systematic review. Ann. Anat. 2019, 225, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Sancho-Puchades, M.; Alfaro, F.H.; Naenni, N.; Jung, R.; Hammerle, C.; Schneider, D. A Randomized Controlled Clinical Trial Comparing Conventional and Computer-Assisted Implant Planning and Placement in Partially Edentulous Patients. Part 2: Patient Related Outcome Measures. Int. J. Periodontics Restor. Dent. 2019, 39, e99–e110. [Google Scholar] [CrossRef]
- Choi, W.; Nguyen, B.C.; Doan, A.; Girod, S.; Gaudilliere, B.; Gaudilliere, D. Freehand versus guided surgery. Factors influencing accuracy of dental implant placement. Implant Dent. 2017, 26, 500–509. [Google Scholar]
- Kramer, F.J.; Baethge, C.; Swennen, G.; Rosahl, S. Navigated vs. conventional implant insertion for maxillary single tooth replacement. Clin. Oral Implant. Res. 2005, 16, 60–68. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Ou, Q.; Lin, X.; Wang, Y. Comparison between a Computer-Aided Surgical Template and the Free-Hand Method: A Systematic Review and Meta-Analysis. Implant Dent. 2019, 28, 578–589. [Google Scholar] [CrossRef]
- Schnitman, P.A.; Hayashi, C.; Han, R.K. Why guided when freehand is easier, quicker, and less costly? J. Oral Implantol. 2014, 40, 670–678. [Google Scholar] [CrossRef]
- Yogui, F.C.; Verri, F.R.; de Luna Gomes, J.M.; Lemos, C.A.; Cruz, R.S.; Pellizzer, E.P. Comparison between computer-guided and free hand dental implant placement surgery: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2021, 50, 242–250. [Google Scholar] [CrossRef]
- Tang, T.; Huang, Z.; Liao, L.; Gu, X.; Zhang, J.; Zhang, X. Factors that influence direction deviation in freehand implant placement. J. Prosthodont. 2019, 28, 511–518. [Google Scholar] [CrossRef]
- Arısan, V.; Karabuda, C.Z.; Mumcu, E.; Özdemir, T. Implant positioning errors in freehand and computer-aided placement me thods: A single-blind clinical comparative study. Int. J. Oral Maxillofac. Implant. 2013, 28, 190–204. [Google Scholar] [CrossRef] [PubMed]
- Dimitrijevic, T.; Kahler, B.; Evans, G.; Collins, M.; Moule, A. Depth and distance perception of dentists and dental students. Oper. Dent. 2011, 36, 467–477. [Google Scholar] [CrossRef]
- Hillerup, S. Iatrogenic injury to oral branches of the trigeminal nerve: Records of 449 cases. Clin. Oral Investig. 2007, 11, 133–142. [Google Scholar] [CrossRef]
- Payer, M.; Kirmeier, R.; Jakse, N.; Pertl, C.; Wegscheider, W.; Lorenzoni, M. Surgical factors influencing mesiodistal implant angulation. Clin. Oral Implant. Res. 2008, 19, 265–270. [Google Scholar] [CrossRef] [PubMed]
- Jaemsuwan, S.; Arunjaroensuk, S.; Kaboosaya, B.; Subbalekha, K.; Mattheos, N.; Pimkhaokham, A. Comparison of the accuracy of implant position among freehand implant placement, static and dynamic computer-assisted implant surgery in fully edentulous patients: A non-randomized prospective study. Int. J. Oral Maxillofac. Surg. 2023, 52, 264–271. [Google Scholar] [CrossRef] [PubMed]
- Hama, D.R.; Mahmood, B.J. Comparison of accuracy between free-hand and surgical guide implant placement among experien ced and non-experienced dental implant practitioners: An in vitro study. J. Periodontal Implant Sci. 2023, 53, 388. [Google Scholar] [CrossRef]
- Schulz, M.C.; Rittmann, L.; Range, U.; Lauer, G.; Haim, D. The use of orientation templates and free-hand implant insertion in artificial mandibles-an experimental laboratory examination in fifth-year dental students. Dent. J. 2018, 6, 43. [Google Scholar] [CrossRef]
- Schulz, M.C.; Hofmann, F.; Range, U.; Lauer, G.; Haim, D. Pilot-drill guided vs.full-guided implant insertion in artificial mandibles-a prospective laboratorystudy in fifth-year dental students. Int. J. Implant Dent. 2019, 5, 23. [Google Scholar] [CrossRef]
- Park, J.Y.; Song, Y.W.; Park, S.H.; Kim, J.H.; Park, J.M.; Lee, J.S. Clinical factors influencing implant positioning by guided surgery using a nonmetal sleeve template in the partially edentulous ridge: Multiple regression analysis of a prospective cohort. Clin. Oral Implant Res. 2020, 31, 1187–1198. [Google Scholar] [CrossRef] [PubMed]
- Afshari, A.; Shahmohammadi, R.; Mosaddad, S.A.; Pesteei, O.; Hajmohammadi, E.; Rahbar, M.; Alam, M.; Abbasi, K. Free-hand versus surgical guide implant placement. Adv. Mater. Sci. Eng. 2022, 2022, 6491134. [Google Scholar] [CrossRef]
- Shetty, S.R.; Murray, C.A.; Al Kawas, S.; Jaser, S.; Al-Rawi, N.; Talaat, W.; Narasimhan, S.; Shetty, S.; Adtani, P.; Hegde, S. Impact of fully guided implant planning software training on the knowledge acquisition and satisfaction of dental undergraduate students. Med. Educ. Online 2023, 28, 2239453. [Google Scholar] [CrossRef] [PubMed]
- Vermeulen, J. The accuracy of implant placement by experienced surgeons. Guided vs freehand approach in a simulated plastic model. Int. J. Oral Maxillofac. Implant. 2017, 32, 617–624. [Google Scholar] [CrossRef]
- Wang, X.; Shaheen, E.; Shujaat, S.; Meeus, J.; Legrand, P.; Lahoud, P.; do Nascimento Gerhardt, M.; Politis, C.; Jacobs, R. Influence of experience on dental implant placement: An in vitro comparison of freehand, static guided and dynamic navigation approaches. Int. J. Implant. Dent. 2022, 8, 42. [Google Scholar] [CrossRef]


|
Group 1
(III–IV Kennedy Class) |
Group 2
(I–II Kennedy Class) |
Group 3
(I–II Kennedy Class) | ||
|---|---|---|---|---|
|
Mono Edentulous Sites
(One Implant) |
Multiple Edentulous Sites
(Two Implants) |
Multiple Edentulous Sites
(Thee Implants) | TOTAL | |
| Patients | 12 | 6 | 5 | 23 |
| Templates | 12 | 6 | 5 | 23 |
| Spheres | 12 | 12 | 15 | 39 |
| Research Flow Chart | |||
|---|---|---|---|
| 1 >> | 2 >> | 3 >> | 4 >> |
| Initial patient selection Elegibility criteria: partial edentulism |
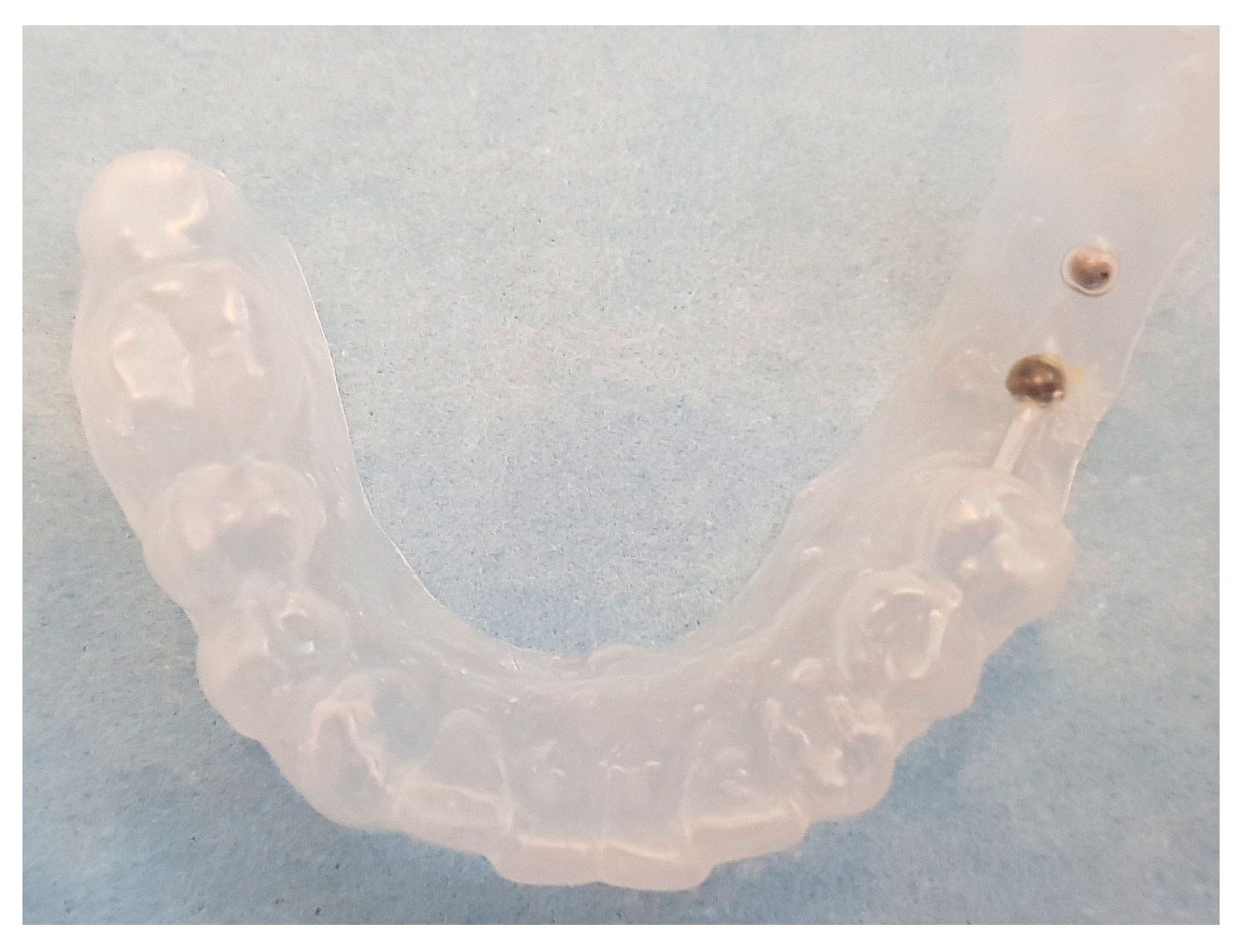
Initial identification of hypothetical implant sites (panoramic radiograph) | Drawing (permanent marker) of the implant sites on a plaster cast | Template construction |
| 5 >> | 6 >> | 7 >> | 8 |
|
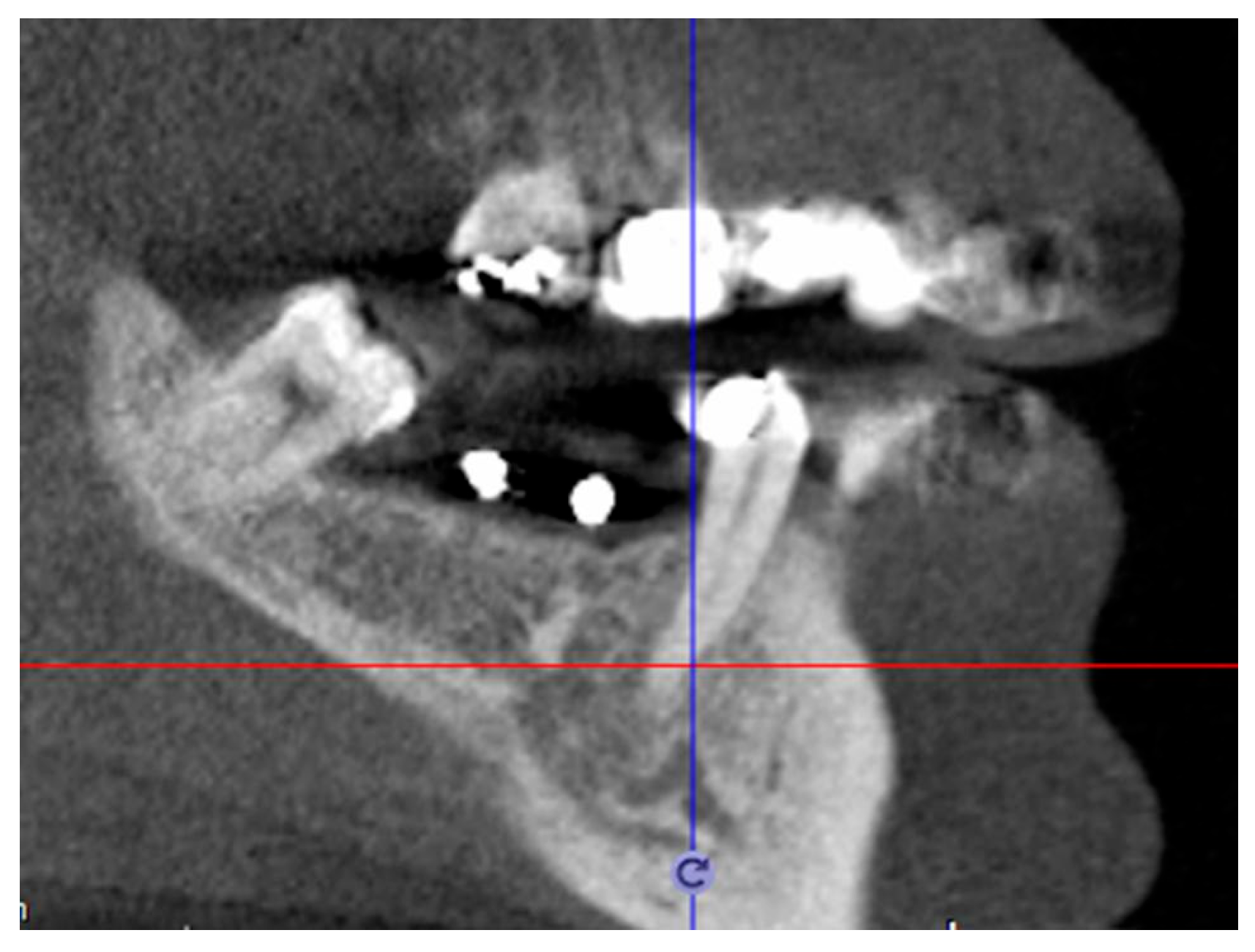
CBCT taken with template | Definitive patient selection Elegibility criteria: fixture position confirmed by CBCT |
Identification implant sites on the mucosa |
Check identification accuracy by template |
| Error Score | |||
|---|---|---|---|
| No Error | Minimal Error | Maximal Error | |
| Distance between sphere in template—dot on mucosa | 0 distance | <2 mm | >2 mm |
|
Group 1
(III–IV Kennedy Class) |
Group 2
(I–II Kennedy Class) |
Group 3
(I–II Kennedy Class) | ||
|---|---|---|---|---|
|
Mono Edentulous Sites
(One Implant) |
Multiple Edentulous Sites
(Two Implants) |
Multiple Edentulous Sites
(Three Implants) | TOTAL | |
| Perfect match | 8 | 6 | 5 | 19 |
| Distance < 2 mm | 3 | 4 | 5 | 12 |
| Distance > 2 mm | 1 | 2 | 5 | 8 |
| Total | 12 | 12 | 15 | 39 |
| GROUP 1 (Only One Implant) | |||
|---|---|---|---|
| 1° Implant Site | 2° Implant Site | 3° Implant Site | |
| Perfect match | 8 | not applicable | not applicable |
| Distance < 2 mm | 3 | not applicable | not applicable |
| Distance > 2 mm | 1 | not applicable | not applicable |
| Total | 12 | 0 | 0 |
| GROUP 2 (Two Implants) | |||
|---|---|---|---|
| 1° Implant Site | 2° Implant Site | 3° Implant Site | |
| Perfect match | 5 | 1 | not applicable |
| Distance < 2 mm | 1 | 3 | not applicable |
| Distance > 2 mm | 0 | 2 | not applicable |
| Total | 6 | 6 | 0 |
| GROUP 3 (Three Implants) | |||
|---|---|---|---|
| 1° Implant Site | 2° Implant Site | 3° Implant Site | |
| Perfect match | 4 | 1 | 0 |
| Distance < 2 mm | 1 | 3 | 1 |
| Distance > 2 mm | 0 | 1 | 4 |
| Total | 5 | 5 | 5 |
|
Group 1
(III–IV Kennedy Class) (One Implant) |
Group 2
(I–II Kennedy Class) (Two Implants) |
Group 3
(I–II Kennedy Class) (Three Implants) | |
|---|---|---|---|
| Perfect match | 66% | 50% | 25% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cumbo, E.; Gallina, G.; Messina, P.; Caradonna, L.; Scardina, G.A. The Freehand Technique: The Ability of the Human Eye to Identify Implant Sites on the Patient. Prosthesis 2024, 6, 551-560. https://doi.org/10.3390/prosthesis6030039
Cumbo E, Gallina G, Messina P, Caradonna L, Scardina GA. The Freehand Technique: The Ability of the Human Eye to Identify Implant Sites on the Patient. Prosthesis. 2024; 6(3):551-560. https://doi.org/10.3390/prosthesis6030039
Chicago/Turabian StyleCumbo, Enzo, Giuseppe Gallina, Pietro Messina, Luigi Caradonna, and Giuseppe Alessandro Scardina. 2024. "The Freehand Technique: The Ability of the Human Eye to Identify Implant Sites on the Patient" Prosthesis 6, no. 3: 551-560. https://doi.org/10.3390/prosthesis6030039
APA StyleCumbo, E., Gallina, G., Messina, P., Caradonna, L., & Scardina, G. A. (2024). The Freehand Technique: The Ability of the Human Eye to Identify Implant Sites on the Patient. Prosthesis, 6(3), 551-560. https://doi.org/10.3390/prosthesis6030039







