A Scoping Review on Accuracy and Acceptance of 3D-Printed Removable Partial Dentures
Abstract
:1. Introduction
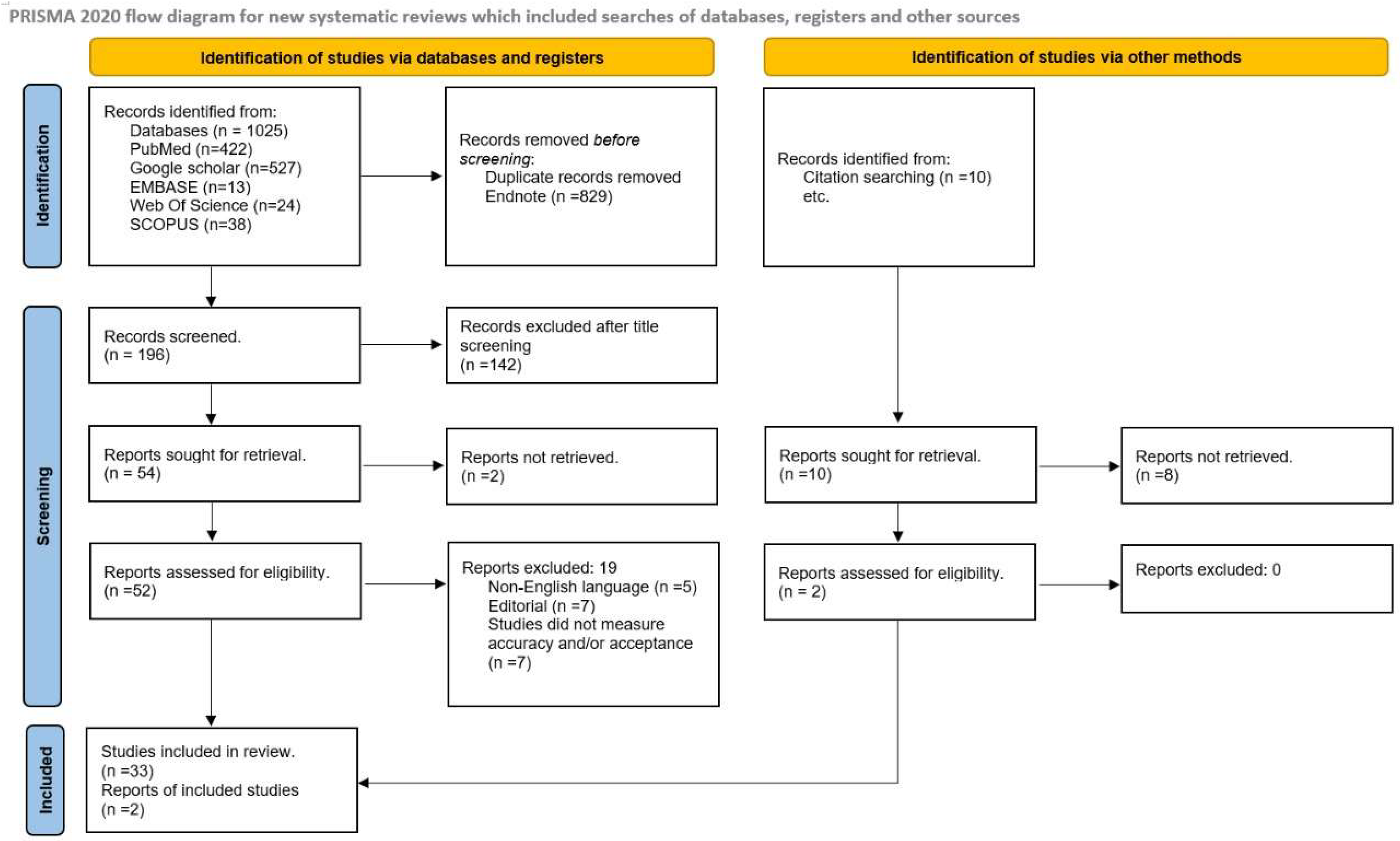
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction and Clinical Outcomes
3. Results
3.1. Characteristics of Included Studies
| Sr No. | Author/Year/Country | Study Design | Kennedy’s Classification | Control Group | Type of 3D Printer | Outcome |
|---|---|---|---|---|---|---|
| 1 | Anan and Saadi 2015 [47]; Syria | In vitro study (Experimental) | Mandibular class III modification 1 | Traditional technique | Light curing model technique | Fit accuracy of 3D-printed RPDs was better than traditional |
| 2 | Lee et al., 2017 [19]; South Korea | Clinical report | Maxillary and mandibular class I | Replica technique | Digital light projection (DLP) | The RPD constructed with the replica technique has varied results |
| 3 | Ye et al., 2017 [46]; China | Randomized control trial | Mandibular class I modification 1 | Lost wax- technique | Stereolithography (SLA) | The single design RPD prepared with a 3D printer was more accurately fit than those with the traditional technique |
| 4 | Arnold et al., 2018 [6]; Germany | Laboratory study | Maxillary class III modification 2 | Lost wax technique | Direct and indirect 3D printing techniques | The 3D-printed RPD has less fit |
| 5 | Soltanzadeh et al., 2018 [50]; USA | Laboratory study | Maxillary class III modification 1 | Lost wax technique | Indirect printing | The conventional RPD was more accurate |
| 6 | Torii et al., 2018 [28]; Japan | Experimental study | First molar simulation | Lost wax technique | indirect printing (CAD) | No significant difference was reported in the accuracy of fit within both techniques |
| 7 | Bajunaid et al., 2019 [10]; Saudi Arabia | Laboratory study | Mandibular class III | Lost wax technique | Direct CAD printers | 3D-printed RPDs are more accurate |
| 8 | Chen et al., 2019 [35]; China | Laboratory study | All classes | Lost wax technique | Direct CAD printing technique | 3D-printed RPDs are less fitting but clinically acceptable |
| 9 | Negm, Aboutaleb, and Alam-Eldein 2019 [22]; Egypt | Laboratory study | Maxillary class I | Stone cast model | Stereolithography (SLA) | RPDs prepared by 3D printers have less accuracy |
| 10 | Carneiro Pereira et al., 2019 [49]; Brazil | Clinical report | Mandibular class III modification 1 | Intra-oral scanner (Patients mouth) | Direct and indirect printing techniques | The 3D-printed RPDs have an acceptable clinical fit |
| 11 | Tregemen et al., 2019 [48]; South Carolina | Clinical trial | Mandibular and maxillary class I, II, and III | Stone cast model | Selective laser melting | 3D-printed RPDs have a better fit |
| 12 | Hayama et al., 2019 [17]; China | Clinical report | Mandibular class I | Intraoral scanners | Direct digital technique | 3D-printed RPD have an acceptable fit |
| 13 | Oka et al., 2019 [13]; Japan | Laboratory study | Mandibular and maxillary class I, II, and III | Lost wax technique | Direct CAD printing technique | 3D-printed RPD have an acceptable fit |
| 14 | Wu et al., 2020 [44]; China | Clinical report | Mandibular class I modification 1 | Intraoral scanners | Selective laser melting | 3D-printed RPD have an acceptable fit |
| 15 | Xie et al., 2020 [39]; China | Laboratory study | First molar simulation | Lost wax technique | Direct CAD printing | 3D-printed RPDs have better fit |
| 16 | Yoon et al., 2021 [40]; China | Laboratory study | Maxillary class I | Stone cast | Direct 3D printing | Acceptable fit |
| 17 | Hussein and Hussein 2022 [11]; Saudi Arabia | Laboratory study | Maxillary class III and Mandibular class 1 | Lost wax technique | Digital light processing | No effect on the accuracy of fit |
| 18 | Saadaldin et al., 2022 [36]; Egypt | Laboratory Study | Not mentioned | Lost wax technique | Selective laser melting technique | Better accuracy fit of SLM-prepared RPDs |
| 19 | Rokshad et al., 2022 [24]; Germany | Laboratory study | Maxillary class III modification 1 | Convectional technique | Digital light processing | Acceptable fit |
| 20 | Peng et al., 2022 [14]; China | Laboratory study | Mandibular class II modification 2 | Lost wax technique | Direct and indirect 3D printing | 3D-printed RPDs have a better fit |
| 21 | Grymak et al., 2023 [32]; New Zealand | Laboratory study | Maxillary class III modification 1 | Stone cast | Selective laser melting | 3D-printed RPDs have better acceptance |
| Sr No. | Author/Year/Country | Study Design | Kennedy’s Classification | Type of 3D Printer | Outcome |
|---|---|---|---|---|---|
| 1. | Kattadiyil et al., 2014 [26]; USA | Clinical report | Maxillary class III | Stereolithographic | The finished prosthesis was successfully placed and used by the patient |
| 2. | Husain Omran 2014 [54]; Saudi Arabia | Case report | Maxillary class I | Digital light prototyping | Well-fitted silicone framework |
| 3. | Lee and Lee 2015 [18]; South Korea | Case report | Maxillary class I | Stereolithographic | Fit accuracy is satisfactory |
| 4. | Mansour et al., 2016 [43]; USA | Clinical report | Maxillary class I modification 1 | Stereolithography (SLA) | Fit of RPD prepared by rapid prototyping was highly satisfactory |
| 5. | Batalha and Araújo 2017 [41]; Brazil | Clinical report | Mandibular class I modification 1 | Digital light projection(DLP) | The accuracy of fit was satisfactory |
| 6. | Hu, Pei, and Wen 2017 [42]; China | Clinical report | Maxillary class I | Stereolithography (SLA) | The 3D-printed RPD is the best alternative to conservative RPD, and the accuracy of fit is acceptable |
| 7. | Gan et al., 2018 [45]; China | Randomized control trials | Dentate | Selective laser melting (SLM) | RPDs designed with 3D printers have an acceptable fit |
| 8. | Katreva et al., 2018 [25]; Bulgaria | Clinical case report | Mandibular class I | Stereolithography (SLA) | 3D-printed RPD appears to be more precise and accurate |
| 9. | Tasaka et al., 2019 [51]; Japan | Laboratory study | Mandibular class II modification 1 | Indirect printing | RPD fabricated by 3D printer has an acceptable fit |
| 10. | Takahashi et al., 2020 [38]; USA | Laboratory study | First molar simulation | Direct and indirect printing | Acceptable fit |
| 11. | Tasaka et al., 2020 [27]; Japan | Laboratory study | Mandibular class II modification 2 | Direct and indirect printing | 3D-printed RPDs have a better fit |
| 12. | Cabrita et al., 2021 [55]; USA | Clinical report | Mandibular class I | Selective laser melting | 3D-printed RPD have an acceptable fit |
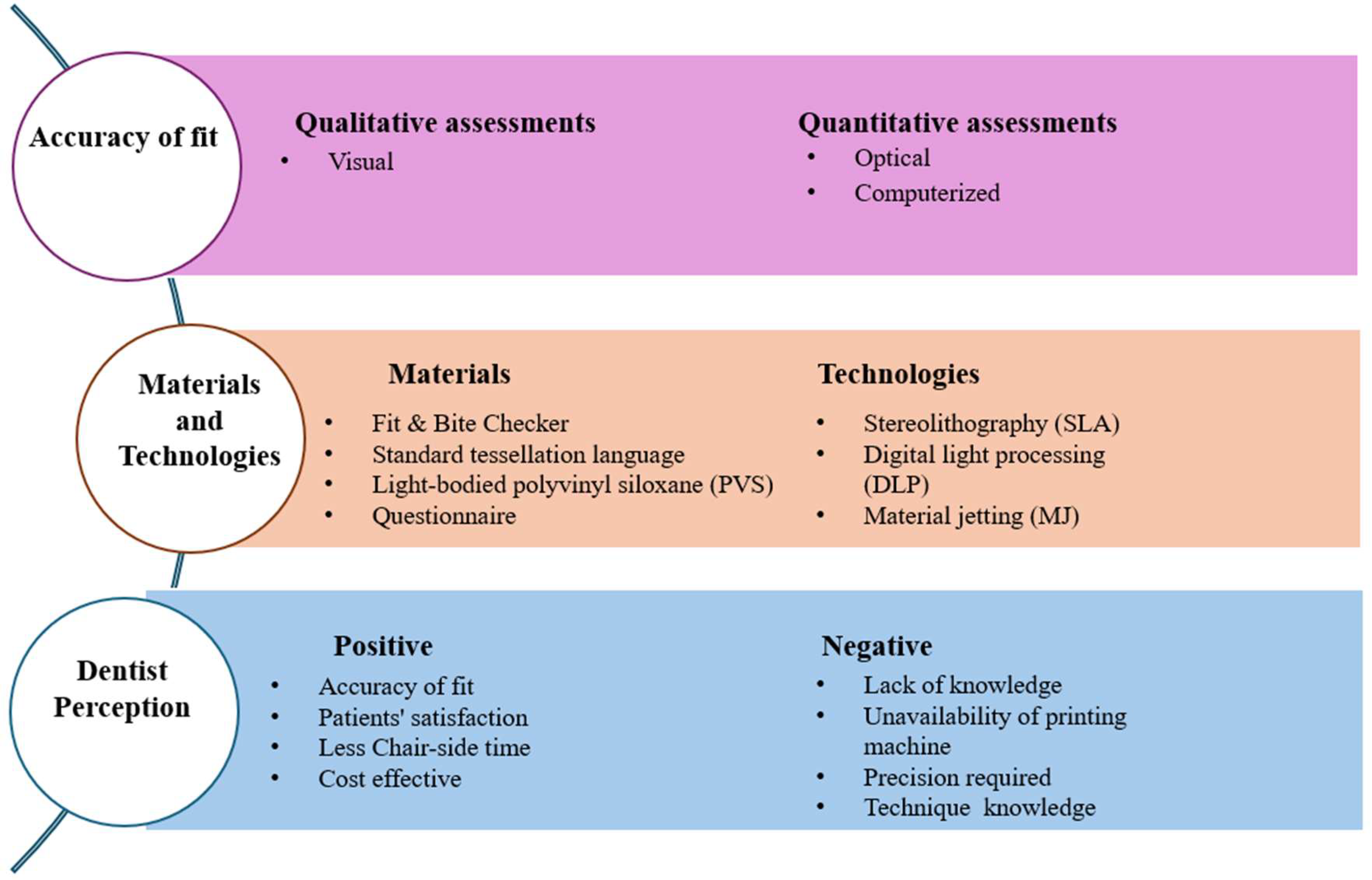
3.2. Comparison of the Method Utilized for Assessment of Fit of 3D-Printed RPDs
3.3. Qualitative Assessment Method (Visual Method)
3.4. Quantitative Assessment Method (Computerized and Optical)
Dentist’s Perception of Acceptance of 3D-Printed RPDs
4. Discussion
5. Conclusions
Supplementary Materials
Funding
Acknowledgments
Conflicts of Interest
References
- ISO 5725-1:1994; Accuracy (Trueness and Precision) of Measurement Methods and Results — Part 1: General Principles and Definitions. International Organization for Standardization: Geneva, Switzerland, 1994.
- Al Mortadi, N.; Alzoubi, K.H.; Williams, R. A Scoping Review on the Accuracy of Fit of Removable Partial Dentures in a Developing Digital Context. Clin. Cosmet. Investig. Dent. 2020, 12, 551–562. [Google Scholar] [CrossRef]
- Almufleh, B.; Emami, E.; Alageel, O.; de Melo, F.; Seng, F.; Caron, E.; Nader, S.A.; Al-Hashedi, A.; Albuquerque, R.; Feine, J.; et al. Patient satisfaction with laser-sintered removable partial dentures: A crossover pilot clinical trial. J. Prosthet. Dent. 2018, 119, 560–567.e561. [Google Scholar] [CrossRef] [PubMed]
- Dunham, D.; Brudvik, J.S.; Morris, W.J.; Plummer, K.D.; Cameron, S.M. A clinical investigation of the fit of removable partial dental prosthesis clasp assemblies. J. Prosthet. Dent. 2006, 95, 323–326. [Google Scholar] [CrossRef] [PubMed]
- Eggbeer, D.; Bibb, R.; Williams, R. The computer-aided design and rapid prototyping fabrication of removable partial denture frameworks. Proc. Inst. Mech. Eng. H 2005, 219, 195–202. [Google Scholar] [CrossRef]
- Arnold, C.; Hey, J.; Schweyen, R.; Setz, J.M. Accuracy of CAD-CAM-fabricated removable partial dentures. J. Prosthet. Dent. 2018, 119, 586–592. [Google Scholar] [CrossRef]
- Bibb, R.; Eggbeer, D.; Williams, R. Rapid manufacture of removable partial denture frameworks. Rapid Prototyp. J. 2006, 12, 95–99. [Google Scholar] [CrossRef]
- Campbell, S.D.; Cooper, L.; Craddock, H.; Hyde, T.P.; Nattress, B.; Pavitt, S.H.; Seymour, D.W. Removable partial dentures: The clinical need for innovation. J. Prosthet. Dent. 2017, 118, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Williams, R.J.; Bibb, R.; Eggbeer, D.; Collis, J. Use of CAD/CAM technology to fabricate a removable partial denture framework. J. Prosthet. Dent. 2006, 96, 96–99. [Google Scholar] [CrossRef] [PubMed]
- Bajunaid, S.O.; Altwaim, B.; Alhassan, M.; Alammari, R. The Fit Accuracy of Removable Partial Denture Metal Frameworks Using Conventional and 3D Printed Techniques: An In Vitro Study. J. Contemp. Dent. Pract. 2019, 20, 476–481. [Google Scholar] [CrossRef]
- Hussein, M.O.; Hussein, L.A. Trueness of 3D printed partial denture frameworks: Build orientations and support structure density parameters. J. Adv. Prosthodont. 2022, 14, 150. [Google Scholar] [CrossRef]
- Alharbi, N.; Osman, R.B.; Wismeijer, D. Factors Influencing the Dimensional Accuracy of 3D-Printed Full-Coverage Dental Restorations Using Stereolithography Technology. Int. J. Prosthodont. 2016, 29, 503–510. [Google Scholar] [CrossRef] [PubMed]
- Oka, Y.; Sasaki, J.; Wakabayashi, K.; Nakano, Y.; Okamura, S.Y.; Nakamura, T.; Imazato, S.; Yatani, H. Fabrication of a radiopaque fit-testing material to evaluate the three-dimensional accuracy of dental prostheses. Dent. Mater. 2016, 32, 921–928. [Google Scholar] [CrossRef]
- Peng, P.W.; Hsu, C.Y.; Huang, H.Y.; Chao, J.C.; Lee, W.F. Trueness of removable partial denture frameworks additively manufactured with selective laser melting. J. Prosthet. Dent. 2022, 127, 122–127. [Google Scholar] [CrossRef] [PubMed]
- Torabi, K.; Farjood, E.; Hamedani, S. Rapid Prototyping Technologies and their Applications in Prosthodontics, a Review of Literature. J. Dent. 2015, 16, 1–9. [Google Scholar]
- Lang, L.A.; Tulunoglu, I. A critically appraised topic review of computer-aided design/computer-aided machining of removable partial denture frameworks. Dent. Clin. N. Am. 2014, 58, 247–255. [Google Scholar] [CrossRef]
- Hayama, H.; Fueki, K.; Wadachi, J.; Wakabayashi, N. Trueness and precision of digital impressions obtained using an intraoral scanner with different head size in the partially edentulous mandible. J. Prosthodont. Res. 2018, 62, 347–352. [Google Scholar] [CrossRef]
- Lee, J.H. Completely digital approach to fabricating a crown under an existing partial removable dental prosthesis by using an intraoral digital scanner in a single appointment. J. Prosthet. Dent. 2016, 115, 668–671. [Google Scholar] [CrossRef]
- Lee, J.W.; Park, J.M.; Park, E.J.; Heo, S.J.; Koak, J.Y.; Kim, S.K. Accuracy of a digital removable partial denture fabricated by casting a rapid prototyped pattern: A clinical study. J. Prosthet. Dent. 2017, 118, 468–474. [Google Scholar] [CrossRef]
- Mamoun, J.S. The path of placement of a removable partial denture: A microscope-based approach to survey and design. J. Adv. Prosthodont. 2015, 7, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Baig, M.R.; Tan, K.B.; Nicholls, J.I. Evaluation of the marginal fit of a zirconia ceramic computer-aided machined (CAM) crown system. J. Prosthet. Dent. 2010, 104, 216–227. [Google Scholar] [CrossRef]
- Negm, E.E.; Aboutaleb, F.A.; Alam-Eldein, A.M. Virtual Evaluation of the Accuracy of Fit and Trueness in Maxillary Poly(etheretherketone) Removable Partial Denture Frameworks Fabricated by Direct and Indirect CAD/CAM Techniques. J. Prosthodont. 2019, 28, 804–810. [Google Scholar] [CrossRef] [PubMed]
- Preshaw, P.M.; Walls, A.W.; Jakubovics, N.S.; Moynihan, P.J.; Jepson, N.J.; Loewy, Z. Association of removable partial denture use with oral and systemic health. J. Dent. 2011, 39, 711–719. [Google Scholar] [CrossRef] [PubMed]
- Rokhshad, R.; Tehrani, A.M.; Nahidi, R.; Zarbakhsh, A. Fit of removable partial denture frameworks fabricated from 3D printed patterns versus the conventional method: An in vitro comparison. J. Prosthet. Dent. 2024, 131, 1144–1149. [Google Scholar] [CrossRef]
- Katreva, I.; Dikova, T.; Tonchev, T. 3D printing–an alternative of conventional crown fabrication: A case report. J. IMAB–Annu. Proceeding Sci. Pap. 2018, 24, 2048–2054. [Google Scholar] [CrossRef]
- Kattadiyil, M.T.; Mursic, Z.; AlRumaih, H.; Goodacre, C.J. Intraoral scanning of hard and soft tissues for partial removable dental prosthesis fabrication. J. Prosthet. Dent. 2014, 112, 444–448. [Google Scholar] [CrossRef] [PubMed]
- Tasaka, A.; Shimizu, T.; Kato, Y.; Okano, H.; Ida, Y.; Higuchi, S.; Yamashita, S. Accuracy of removable partial denture framework fabricated by casting with a 3D printed pattern and selective laser sintering. J. Prosthodont. Res. 2020, 64, 224–230. [Google Scholar] [CrossRef] [PubMed]
- Torii, M.; Nakata, T.; Takahashi, K.; Kawamura, N.; Shimpo, H.; Ohkubo, C. Fitness and retentive force of cobalt-chromium alloy clasps fabricated with repeated laser sintering and milling. J. Prosthodont. Res. 2018, 62, 342–346. [Google Scholar] [CrossRef]
- Mai, H.Y.; Mai, H.N.; Kim, H.J.; Lee, J.; Lee, D.H. Accuracy of Removable Partial Denture Metal Frameworks Fabricated by Computer-Aided Design/Computer-Aided Manufacturing Method: A Systematic Review and Meta-Analysis. J. Evid. Based Dent. Pract. 2022, 22, 101681. [Google Scholar] [CrossRef] [PubMed]
- Chobe, A.; Sushma, R.; Shashikiran, N.; Kore, A.R.; Shivakumar, K.; Vande, A. Study to Assess the Knowledge, Attitude and Practices of Additive Manufacturing Technology by Dental Practitioners in Dentistry across India-A Survey. Journal for ReAttach Ther. Dev. Divers. 2023, 6, 759–766. [Google Scholar]
- Urumova, M. Comparative study of retention of telescopic crowns fabricated by 3D printing (in vitro study). J. Int. Dent. Med. Res. 2023, 16, 13–19. [Google Scholar]
- Grymak, A.; Badarneh, A.; Ma, S.; Choi, J.J.E. Effect of various printing parameters on the accuracy (trueness and precision) of 3D-printed partial denture framework. J. Mech. Behav. Biomed. Mater. 2023, 140, 105688. [Google Scholar] [CrossRef]
- Azari, A.; Nikzad, S. The evolution of rapid prototyping in dentistry: A review. Rapid Prototyp. J. 2009, 15, 216–225. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Li, H.; Zhao, Y.; Zhang, X.; Wang, Y.; Lyu, P. Adaptation of removable partial denture frameworks fabricated by selective laser melting. J. Prosthet. Dent. 2019, 122, 316–324. [Google Scholar] [CrossRef]
- Saadaldin, S.A.; Rizkalla, A.S.; Eldwakhly, E.A.; Soliman, M.; Aldegheishem, A. Assessment of the fitness of removable partial denture frameworks manufactured using additive manufacturing/selective laser melting. Mater. Express 2022, 12, 735–742. [Google Scholar] [CrossRef]
- Soltanzadeh, P.; Su, J.-M.; Habibabadi, S.R.; Kattadiyil, M.T. Obturator fabrication incorporating computer-aided design and 3-dimensional printing technology: A clinical report. J. Prosthet. Dent. 2019, 121, 694–697. [Google Scholar] [CrossRef]
- Takahashi, K.; Torii, M.; Nakata, T.; Kawamura, N.; Shimpo, H.; Ohkubo, C. Fitness accuracy and retentive forces of additive manufactured titanium clasp. J. Prosthodont. Res. 2020, 64, 468–477. [Google Scholar] [CrossRef]
- Xie, W.; Zheng, M.; Wang, J.; Li, X. The effect of build orientation on the microstructure and properties of selective laser melting Ti-6Al-4V for removable partial denture clasps. J. Prosthet. Dent. 2020, 123, 163–172. [Google Scholar] [CrossRef]
- Yoon, J.-m.; Liu, Y.; Liu, Y.; Sun, Y.; Ye, H.; Zhou, Y. The accuracy of a novel 3D digital evaluation method of intraoral fitness for removable partial dentures. Comput. Biol. Med. 2022, 144, 105348. [Google Scholar] [CrossRef] [PubMed]
- Batalha, A.; Araújo, R.M. Development of removable partial dentures by using additive manufacture and casting processes. Arch. Mater. Sci. Eng. 2017, 87, 33–40. [Google Scholar] [CrossRef]
- Hu, F.; Pei, Z.; Wen, Y. Using Intraoral Scanning Technology for Three-Dimensional Printing of Kennedy Class I Removable Partial Denture Metal Framework: A Clinical Report. J. Prosthodont. 2019, 28, e473–e476. [Google Scholar] [CrossRef] [PubMed]
- Mansour, M.; Sanchez, E.; Machado, C. The Use of Digital Impressions to Fabricate Tooth-Supported Partial Removable Dental Prostheses: A Clinical Report. J. Prosthodont. 2016, 25, 495–497. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Li, Y.; Zhang, Y. Use of intraoral scanning and 3-dimensional printing in the fabrication of a removable partial denture for a patient with limited mouth opening. J. Am. Dent. Assoc. 2017, 148, 338–341. [Google Scholar] [CrossRef]
- Gan, N.; Ruan, Y.; Sun, J.; Xiong, Y.; Jiao, T. Comparison of Adaptation between the Major Connectors Fabricated from Intraoral Digital Impressions and Extraoral Digital Impressions. Sci. Rep. 2018, 8, 529. [Google Scholar] [CrossRef] [PubMed]
- Ye, H.; Ning, J.; Li, M.; Niu, L.; Yang, J.; Sun, Y.; Zhou, Y. Preliminary Clinical Application of Removable Partial Denture Frameworks Fabricated Using Computer-Aided Design and Rapid Prototyping Techniques. Int. J. Prosthodont. 2017, 30, 348–353. [Google Scholar] [CrossRef]
- Anan, M.T.M.; Al-Saadi, M.H. Fit accuracy of metal partial removable dental prosthesis frameworks fabricated by traditional or light curing modeling material technique: An in vitro study. Saudi Dent. J. 2015, 27, 149–154. [Google Scholar] [CrossRef]
- Tregerman, I.; Renne, W.; Kelly, A.; Wilson, D. Evaluation of removable partial denture frameworks fabricated using 3 different techniques. J. Prosthet. Dent. 2019, 122, 390–395. [Google Scholar] [CrossRef]
- Carneiro Pereira, A.L.; Martins de Aquino, L.M.; Carvalho Porto de Freitas, R.F.; Soares Paiva Tôrres, A.C.; da Fonte Porto Carreiro, A. CAD/CAM-fabricated removable partial dentures: A case report. Int. J. Comput. Dent. 2019, 22, 371–379. [Google Scholar]
- Soltanzadeh, P.; Suprono, M.S.; Kattadiyil, M.T.; Goodacre, C.; Gregorius, W. An In Vitro Investigation of Accuracy and Fit of Conventional and CAD/CAM Removable Partial Denture Frameworks. J. Prosthodont. 2019, 28, 547–555. [Google Scholar] [CrossRef]
- Tasaka, A.; Kato, Y.; Odaka, K.; Matsunaga, S.; Goto, T.K.; Abe, S.; Yamashita, S. Accuracy of Clasps Fabricated with Three Different CAD/CAM Technologies: Casting, Milling, and Selective Laser Sintering. Int. J. Prosthodont. 2019, 32, 526–529. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.X.; Zeng, X.Y.; Wang, Z.M.; Guan, K.; Peng, C.W. Fabrication of removable partial denture framework by selective laser melting. Adv. Mater. Res. 2011, 317, 174–178. [Google Scholar] [CrossRef]
- Hussein, M.O.; Hussein, L.A. Optimization of digital light processing three-dimensional printing of the removable partial denture frameworks; the role of building angle and support structure diameter. Materials 2022, 15, 2316. [Google Scholar] [CrossRef] [PubMed]
- Hussein, M.O.; Hussein, L.A. Novel 3D modeling technique of removable partial denture framework manufactured by 3D printing technology. Int. J. Adv. Res. 2014, 9, 686–694. [Google Scholar]
- Cabrita, J.P.; Mendes, T.A.; Martins, J.P.; Lopes, L. Removable partial denture metal framework manufactured by selective laser melting technology—A clinical report. Rev. Port. De Estomatol. Med. Dentária E Cir. Maxilofac. 2021, 62, 109–113. [Google Scholar] [CrossRef]
- Ahmed, N.; Abbasi, M.S.; Haider, S.; Ahmed, N.; Habib, S.R.; Altamash, S.; Zafar, M.S.; Alam, M.K. Fit Accuracy of Removable Partial Denture Frameworks Fabricated with CAD/CAM, Rapid Prototyping, and Conventional Techniques: A Systematic Review. Biomed. Res. Int. 2021, 2021, 3194433. [Google Scholar] [CrossRef]
- Rudd, R.W.; Rudd, K.D. A review of 243 errors possible during the fabrication of a removable partial denture: Part I. J. Prosthet. Dent. 2001, 86, 251–261. [Google Scholar] [CrossRef]
- Wang, C.; Shi, Y.-F.; Xie, P.-J.; Wu, J.-H. Accuracy of digital complete dentures: A systematic review of in vitro studies. J. Prosthet. Dent. 2021, 125, 249–256. [Google Scholar] [CrossRef]
- Brudvik, J.S.; Reimers, D. The tooth-removable partial denture interface. J. Prosthet. Dent. 1992, 68, 924–927. [Google Scholar] [CrossRef]
| Author | Method of Assessment | Type of Measurement | Area of Measurement |
|---|---|---|---|
| Kattadiyil et al., 2014 [26] | Visual inspection (mouth mirror and probe) | Adaptation | Overall |
| Hussain Orman et al., 2014 [54] | Optical (Microscope) | Accuracy and adaptation | Overall |
| Batalha and Araújo 2017 [41] | Visual inspection (mouth mirror and probe) | Adaptation | Overall |
| Hu, Pei, and Wen 2017 [42] | Visual inspection (mouth mirror and probe) | Adaptation | Overall |
| Lee et al., 2017 [19] | Optical (Stereomicroscope) | Internal discrepancy | All components |
| Ye et al., 2017 [46] | Visual inspection (mouth mirror and probe) | Adaptation | Overall |
| Batalha and Araújo 2017 [26] | Optical (Stereomicroscope) | Gap distance | Different sections |
| Arnold et al., 2018 [6] | Optical (Light microscope) | Gap distance | Clasp |
| Gan et al., 2018 [45] | Optical (Stereomicroscope) | Gap distance | All components |
| Soltanzadeh et al., 2018 [50] | Computerized (Geomagic) | Gap distance | All components |
| Torii et al., 2018 [28] | Optical (Profile projector) | Gap distance | Rest, 3-point clasp |
| Bajunaid et al., 2019 [10] | Optical (Digital microscope) | Gap distances | Rest |
| Chen et al., 2019 [35] | Computerized (Geomagic NX image) | Gap distance | Overall |
| Negm, Aboutaleb, and Alam-Eldein 2019 [22] | Computerized (Geomagic) | Gap distance | Overall |
| Oka et al., 2019 [13] | Computerized | Adaptation | Overall |
| Soltanzadeh et al., 2018 [35] | Computerized (Geomagic) | Trueness | All components |
| Carneiro Pereira et al., 2019 [49] | Visual inspection (mouth mirror and probe) | Adaptation | Overall |
| Tasaka et al., 2019 [51] | Computerized (GOM Inspect) | Average deviation | All components |
| Tregemen et al., 2019 [48] | Visual inspection (mouth mirror and probe) | Adaptation | Overall |
| Takahashi et al., 2020 [38] | Optical (Profile projector) | Gap distance | Clasp |
| Tasaka et al., 2020 [27] | Computerized (GOM Inspect) | Average deviation | Clasp |
| Wu et al., 2020 [44] | Visual inspection (mouth mirror and probe) | Adaptation | Overall |
| Xie et al., 2020 [39] | Optical (Stereomicroscope) | Gap distance | 3-point clasp |
| Cabrita et al., 2021 [55] | Visual inspection (mouth mirror and probe) | Adaptation | Overall |
| Peng et al., 2022 [14] | Computerized (Geomagic) | Trueness | Overall |
| Rokshad et al., 2022 [24] | Computerized (Geomagic Control X) | Adaptation and Gap measurement | All areas |
| Grymak et al., 2023 [32] | Computerized (Geomagic Control X) | Adaptation | Overall |
| Hussain and Hussain 2022 [11] | Computerized (Geomagic Control X) | Trueness | Overall |
| Authors | Study Design | Dentist Perception | Long-Term Prognosis |
|---|---|---|---|
| Urumova et al., 2021 [30]; Bulgaria | Questionnaire | Cost effective and reduces chair-side timing | More clinical studies are required for the analysis of long-term prognosis |
| Chobe et al., 2023 [31]; India | Questionnaire | Cost effective and easily acceptable | Not mentioned |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Porwal, A. A Scoping Review on Accuracy and Acceptance of 3D-Printed Removable Partial Dentures. Prosthesis 2025, 7, 16. https://doi.org/10.3390/prosthesis7010016
Porwal A. A Scoping Review on Accuracy and Acceptance of 3D-Printed Removable Partial Dentures. Prosthesis. 2025; 7(1):16. https://doi.org/10.3390/prosthesis7010016
Chicago/Turabian StylePorwal, Amit. 2025. "A Scoping Review on Accuracy and Acceptance of 3D-Printed Removable Partial Dentures" Prosthesis 7, no. 1: 16. https://doi.org/10.3390/prosthesis7010016
APA StylePorwal, A. (2025). A Scoping Review on Accuracy and Acceptance of 3D-Printed Removable Partial Dentures. Prosthesis, 7(1), 16. https://doi.org/10.3390/prosthesis7010016








