Design and 3D Printing of Low-Cost Functional Sports Devices for the Upper Limb
Abstract
:1. Introduction
- Passive prostheses have limited or absent functionality, as their main goal is to mimic the look of a natural limb as much as possible rather than be useful in a practical way. Some passive prostheses have a hook that can be moved with the intact hand or by interacting with the external environment to hold objects.
- Body-powered active prostheses are usually equipped with a hook mechanism, whose opening and closure are controlled by the movement of another part of the user’s body (e.g., the shoulder). The mechanical energy generated by body movements is transmitted via cables to the prosthetic hand.
- Externally powered active prostheses are driven by one or more motors. The most common are myoelectric prostheses, in which the motors are controlled by the electrical signals produced by muscle contraction and captured by electrodes.
- Hybrid active prostheses use both body-powered and externally powered mechanisms in the same device to operate different joints.
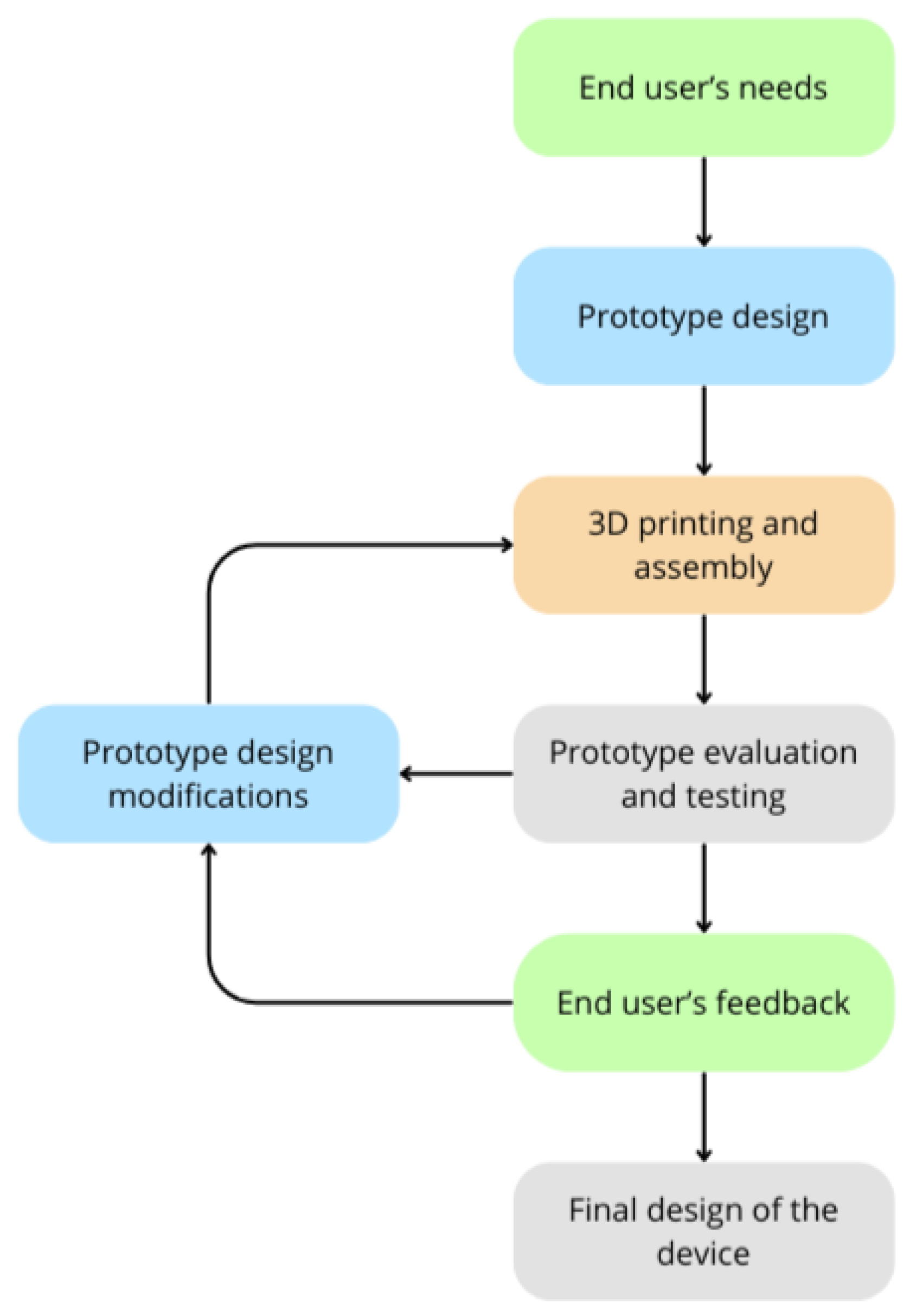
2. Design and 3D Printing Process
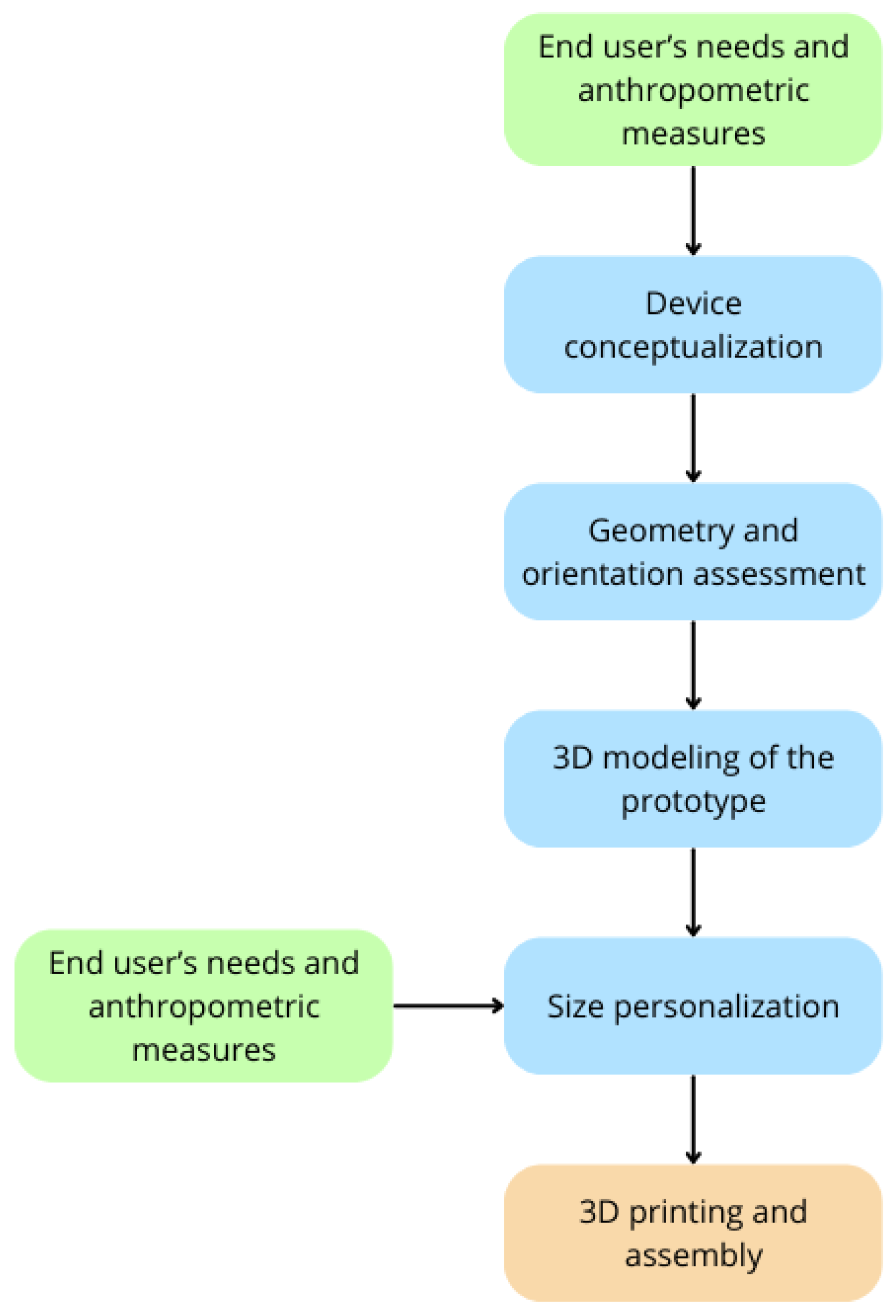
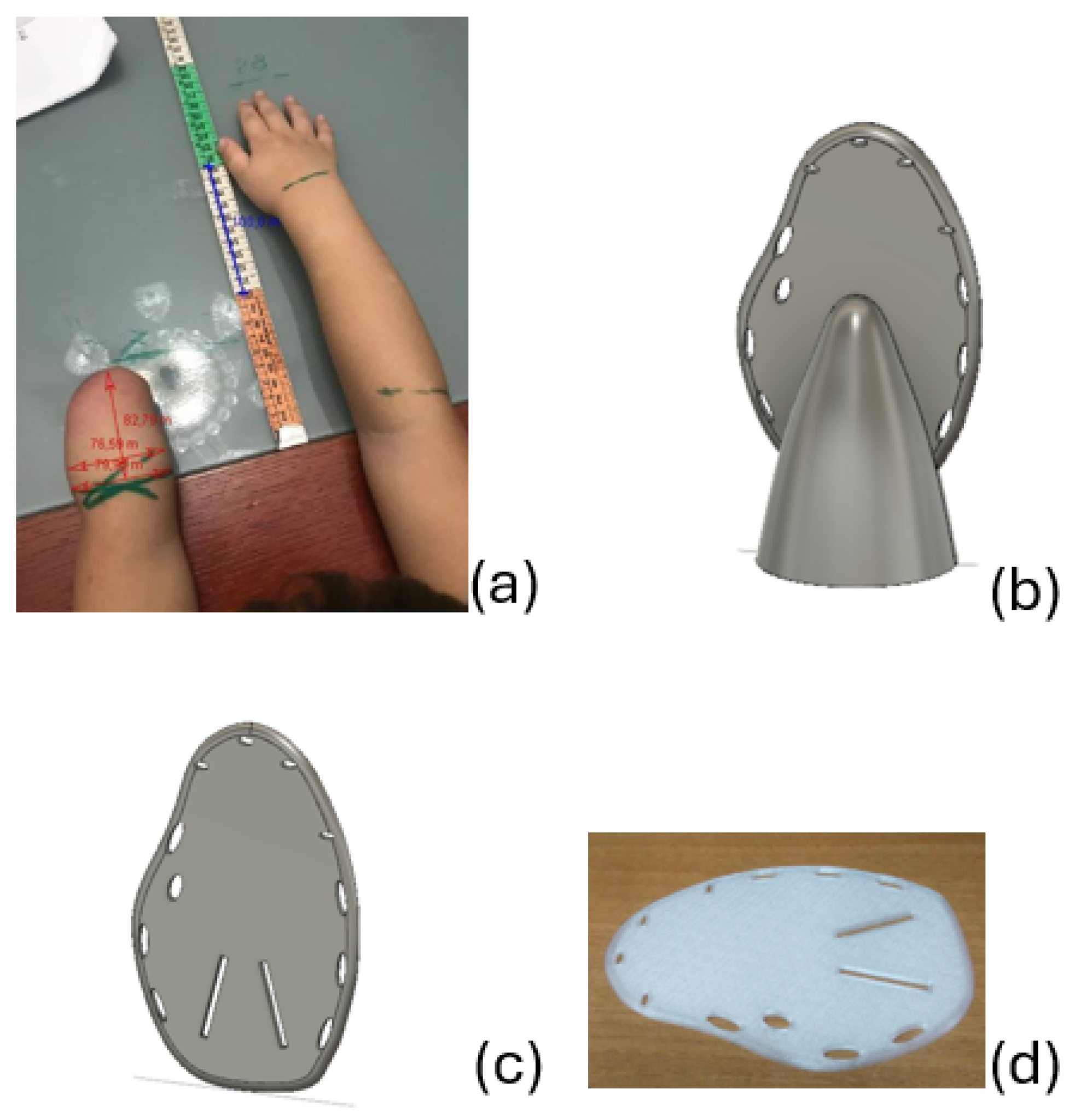
2.1. User-Centered Approach
- Draw lines around the wrists and elbows to make it easier to identify their position in the photograph;
- If an elbow-operated device has been requested, also trace a line on the widest point of the biceps;
- Extend the arms parallel to each other on a flat surface (such as a wall, the floor, or a table), placing a measuring tape at the center between the two arms;
- Take photographs in the positions indicated by the examples shown in the manual.
2.2. Prototype Design Process
- Mechanical properties. The goal is to make the assistive device as durable as possible through the optimal geometry of the parts that make up the prototype. If this evaluation is not done correctly, there is a risk of breakage of the assistive device itself.
- Printability. The main objective is to reduce the need for support structures during printing [15]. There are several reasons to aim for as few supports as possible: It reduces print time, requires less post-printing processing, uses less material, and, thus, reduces the overall production costs of the assistive device.
- Delamination. This phenomenon is defined as the separation between layers and it can occur during the printing process if the printer parameters, especially the material temperature and cooling speed, have not been properly set. However, the delamination phenomenon can also occur after the printing process and depend on the orientation of the layers: In this case, initially, the layers adhere well, but the application of forces in certain directions causes them to detach from each other. This problem can be avoided by reconsidering the shape and orientation of the printed object’s parts with respect to the print bed to ensure better mechanical properties.
- Ease of assembly. In case the device is made up of two or more pieces, the goal is to make it as easy as possible to assemble once the parts are printed.
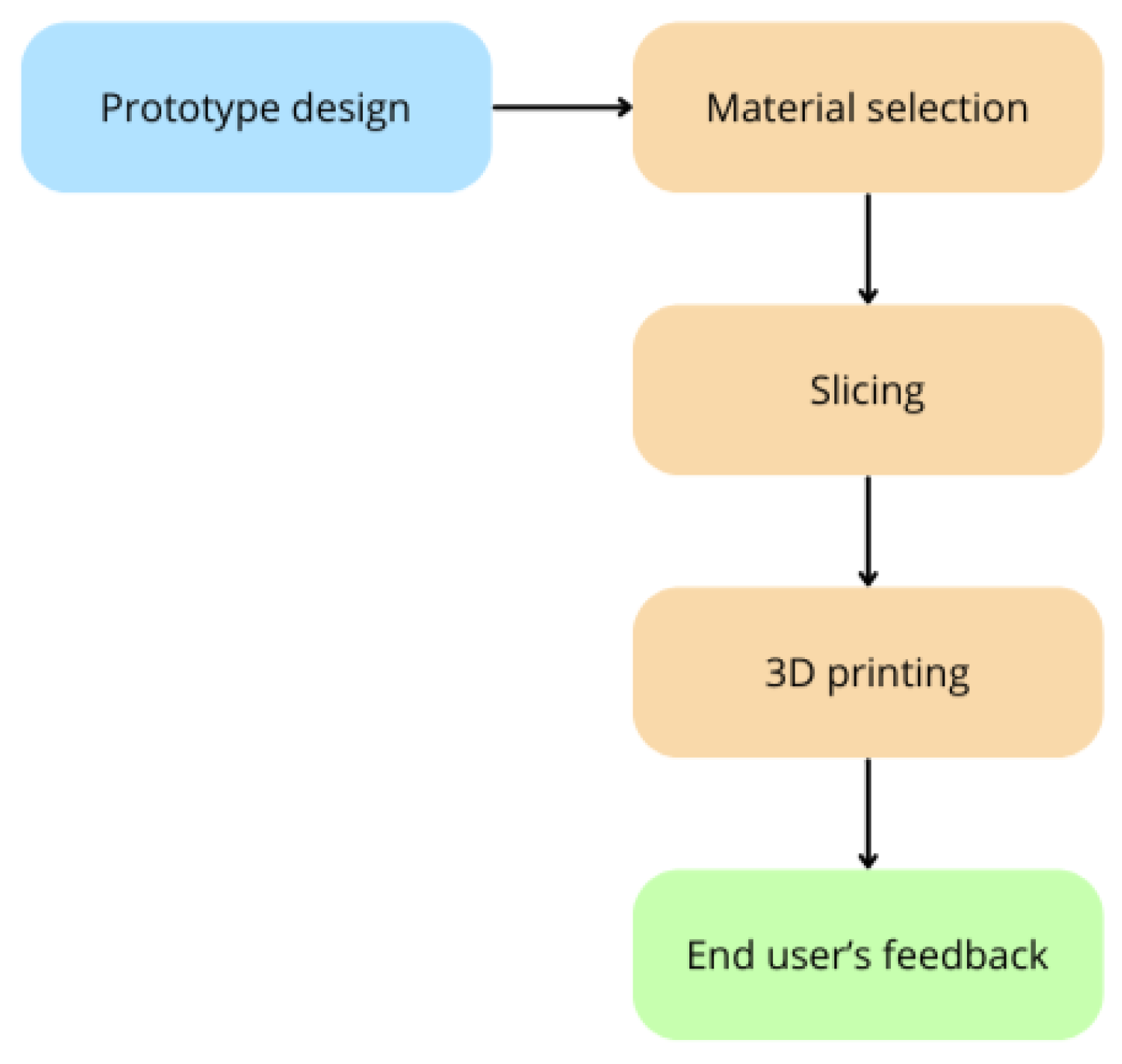
2.3. 3D Printing of the Prototype
- Polylactic acid (PLA) was chosen for its biocompatibility and non-toxic properties, which are essential to avoid adverse reactions when in contact with the skin. Specifically, the LATIGEA filament from LATI 3D (LATI 3D, Vedano Olona, Italy) was used. It is a PLA stabilized against hydrolysis and UV radiation, a feature that makes it particularly suitable for outdoor use. Additionally, this material can undergo a crystallization process through baking, enhancing its mechanical strength and making it resistant to high temperatures (up to 100 °C).
- Thermoplastic polyurethane (TPU) is an elastomer that combines the properties of thermoplastics and rubbers due to its alternating rigid and flexible segments. The elasticity of TPU depends on the proportion of these two types of chemical sequences [16]. This material was chosen for its high resistance to impacts, wear, abrasion, and cuts.
- Polypropylene (PP) was selected for its durability and mechanical strength, and it is also particularly lightweight due to its low density [17]. The LATENE filament from LATI 3D was used, which is a PP filament with antibacterial additives. It is resistant to high temperatures (up to 100 °C) and resistant to hydrocarbons, acids, and strong bases. These characteristics make this material well-suited for chemically aggressive environments, such as a pool water environment.
- Polyethylene terephthalate glycol (PETG) was chosen for its mechanical properties and thermal resistance. Specifically, recycled filament from LATI 3D was used, which is derived from post-industrial waste that does not face contamination issues like post-consumer waste.
3. Results
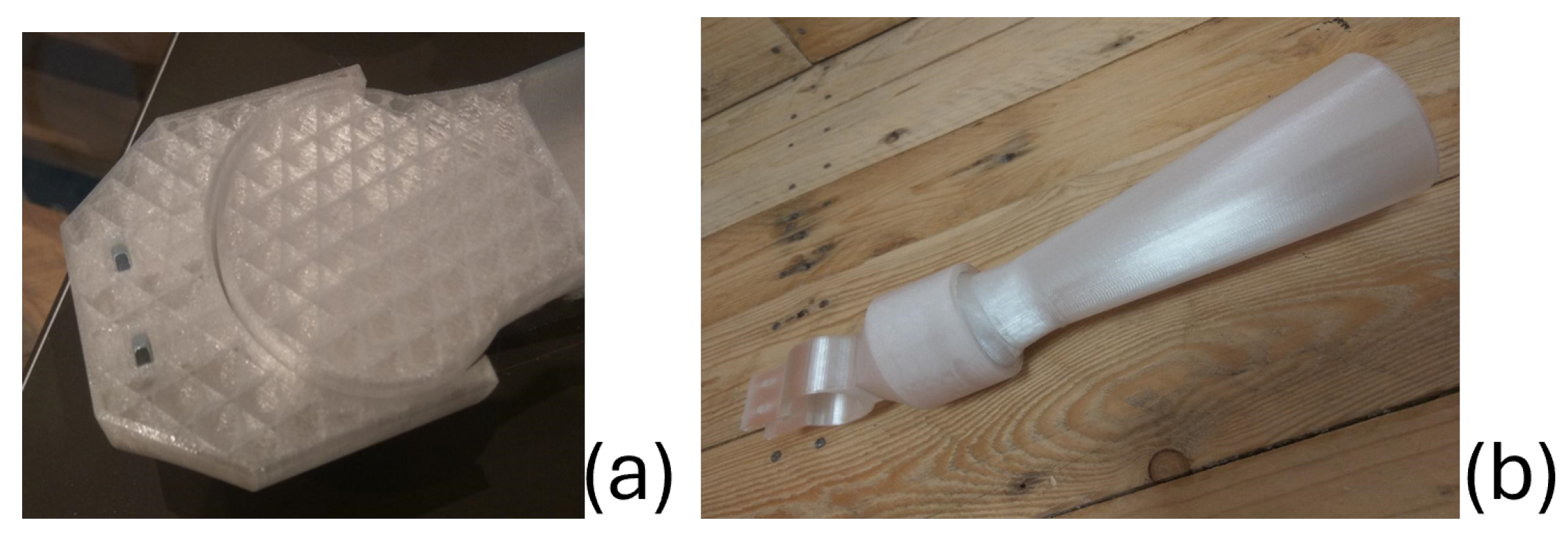
3.1. Swimming Aid
- There is no stable way to securely attach the socket to the limb.
- The socket and the paddle need to be printed with layers oriented perpendicularly to each other, meaning separately. There is no way to later combine the two parts.
- Using glue on the print bed;
- Applying 3M (3M, Saint Paul, MN, USA) double-sided adhesive tape on the print bed;
- Placing adhesive PP tape on the print bed;
- Using a glass print bed.
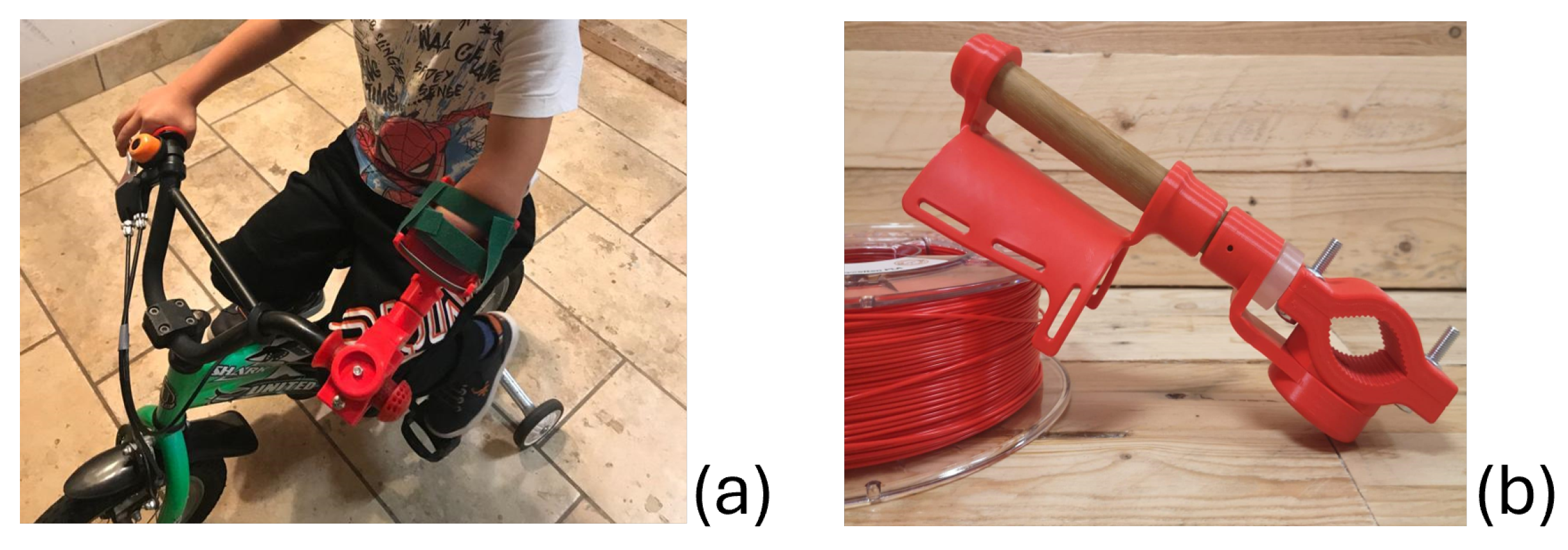
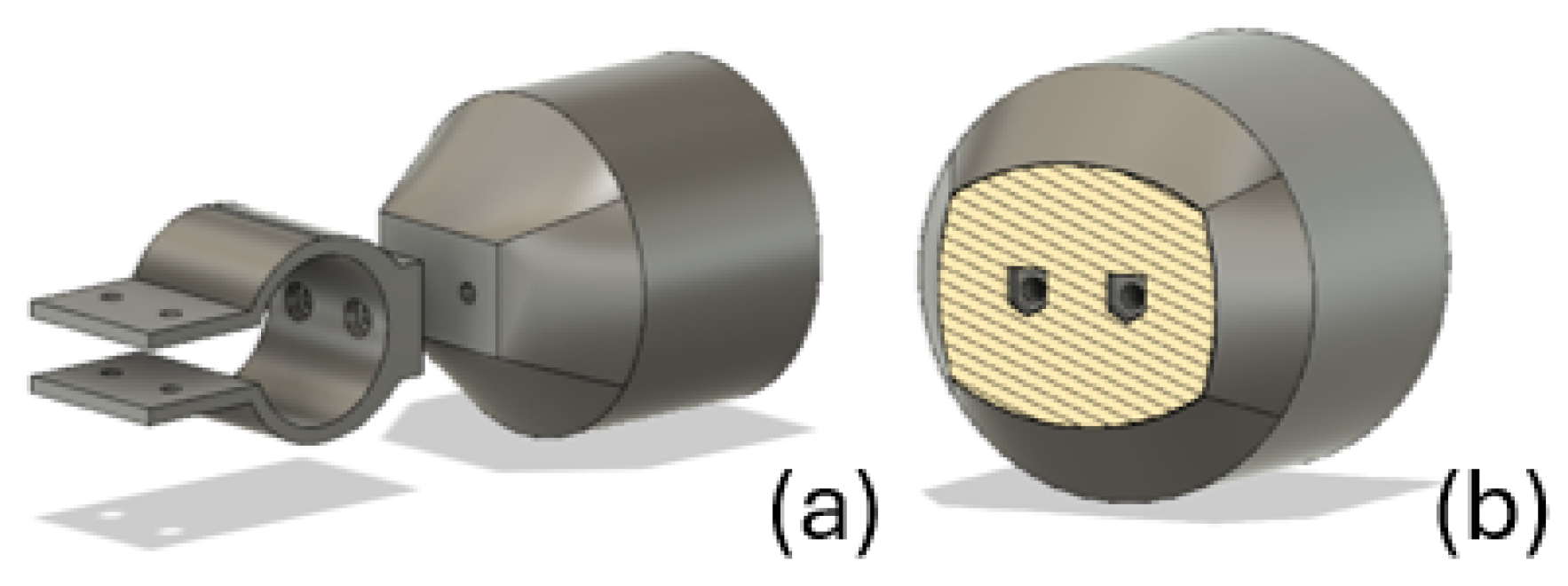
3.2. Non-Binding Bicycle Aid
3.3. Binding Bicycle Aid
- The dimensions of the first device were no longer adequate, as the child had grown, and the measurements of his arm had changed since the previous request was made. The new measurements were provided by the parents, who also took some photographs that were used for further analysis with the Tracker software.
- The child wanted to learn to ride a bicycle without training wheels. With this system, the child could remove the arm from the support as the constraint did not offer excessive resistance. To increase his sense of security and control over the bicycle, he and his parents requested a device that completely encloses the arm, limiting its motion.
- The velcro system might be impractical for a young child, as they would need assistance from their parents to secure the device.
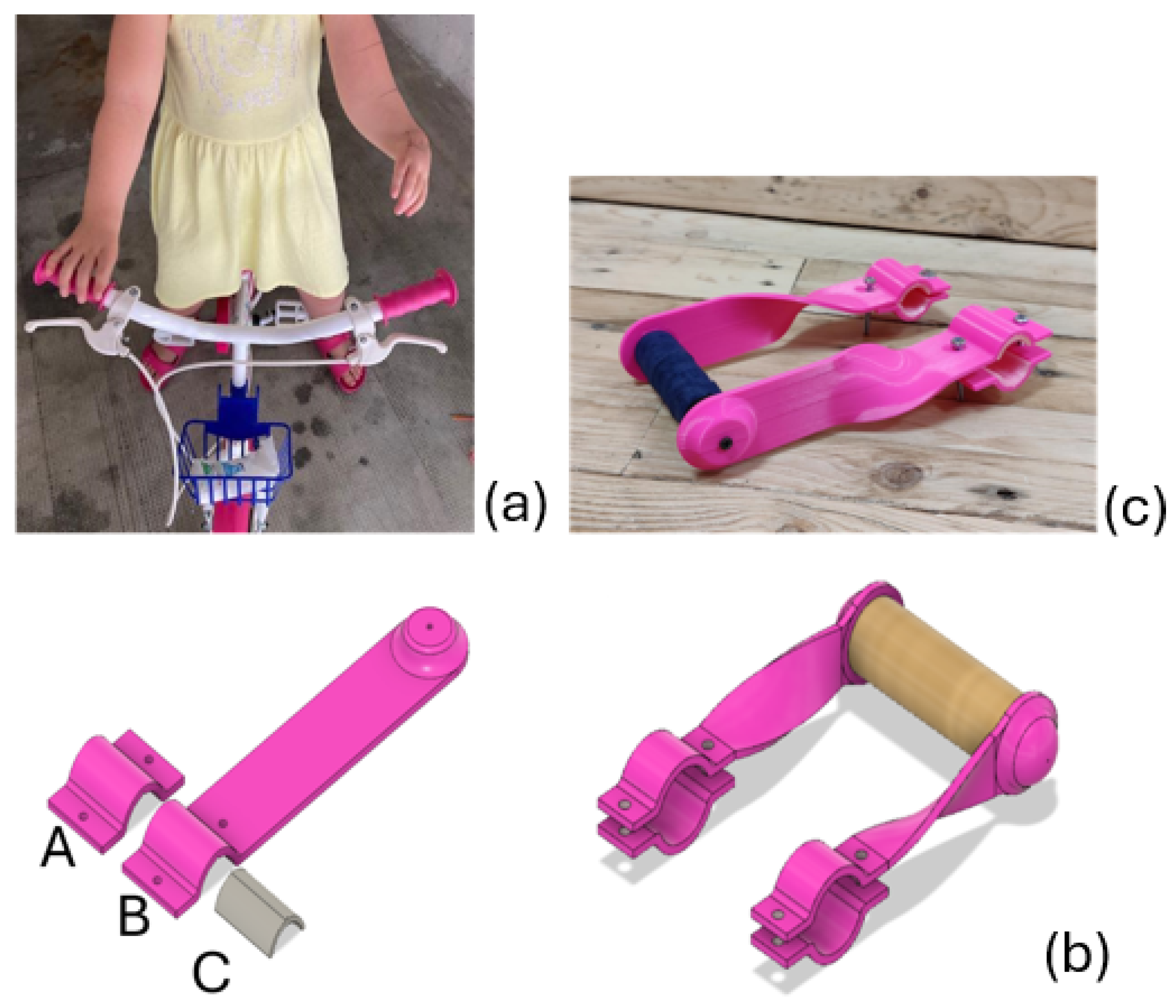
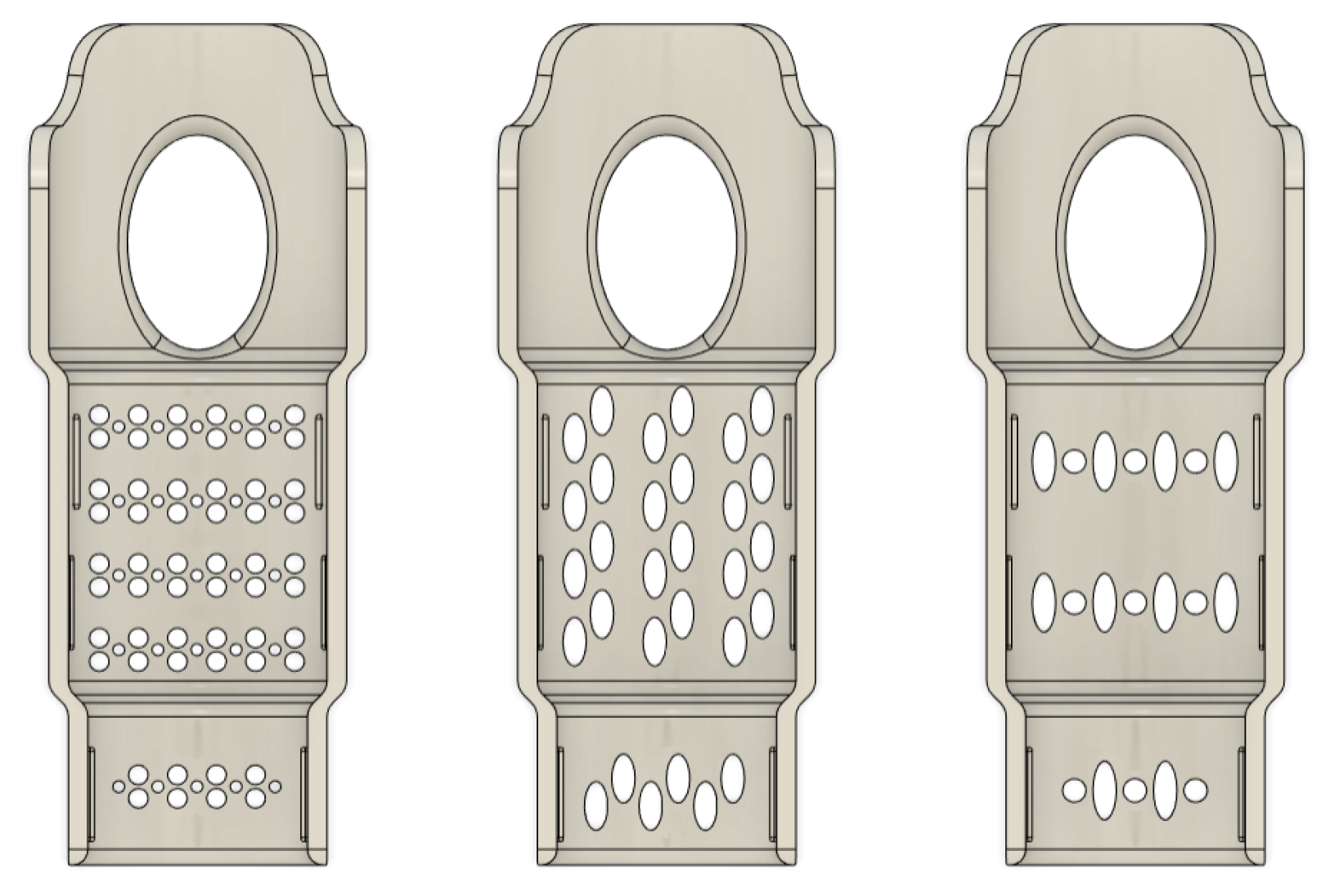
3.4. Handlebar Extender Bicycle Aid
- Piece A is the smaller pink piece;
- Piece B constitutes the handlebar extension;
- Piece C is the gray curved piece.
- Piece B was printed flat to achieve the best possible orientation of the print layers. By overlapping parallel planes, weak points are avoided, resulting in improved mechanical properties. The curvatures are formed afterward through thermoforming.
- The positioning of the three parts on the printer bed was determined considering the print orientation and, consequently, the layering direction of the material. This orientation enhances resistance to usage, particularly in preventing layer delamination.
- To enhance friction between the device and the bicycle handlebar, the width of the parts in contact with it (pieces A and B) was increased, and piece C was introduced. This part features a textured surface on the inner side; it also includes a wedge on the opposite side to securely fit piece C into pieces A and B, which have a corresponding cavity.
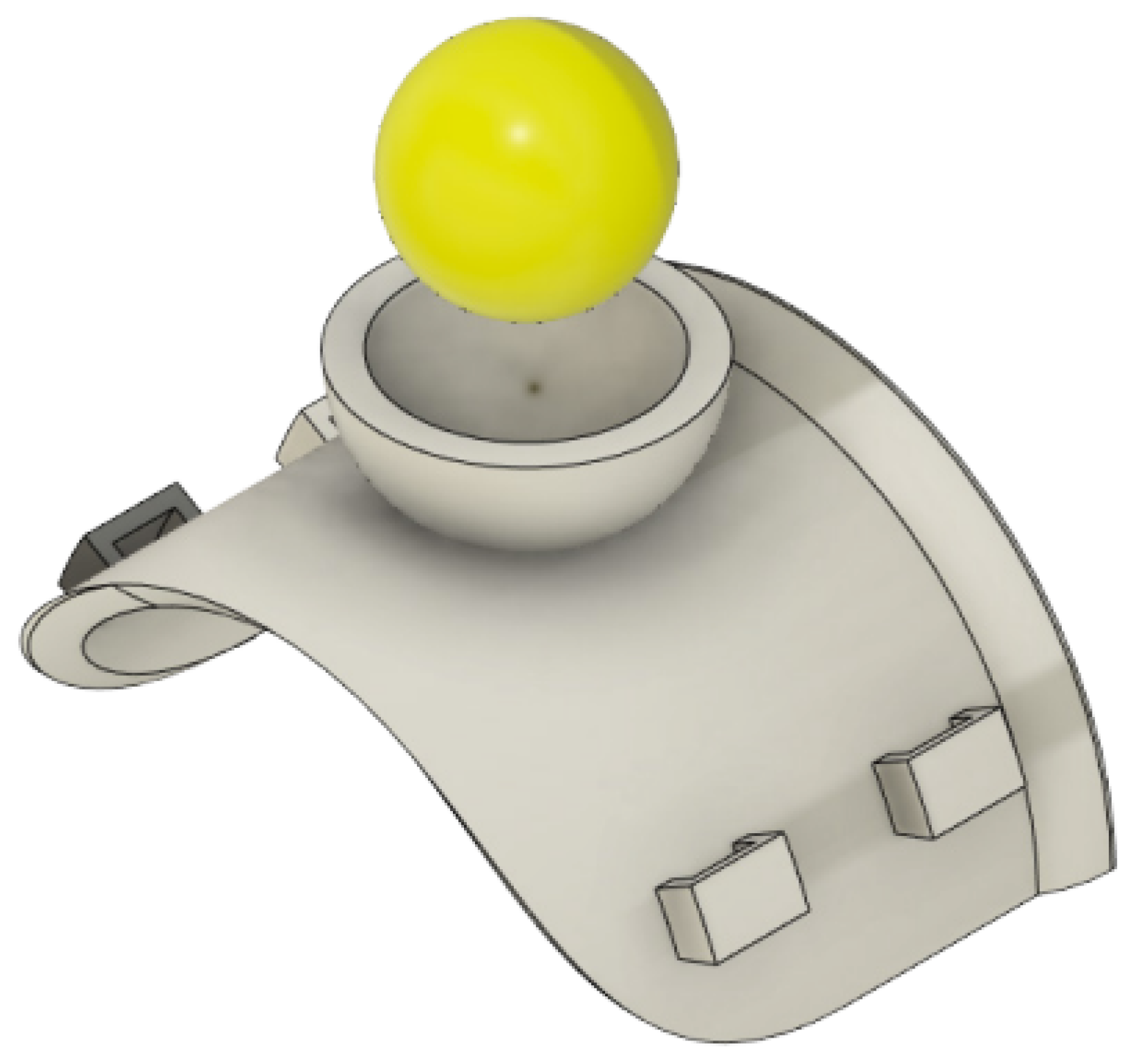
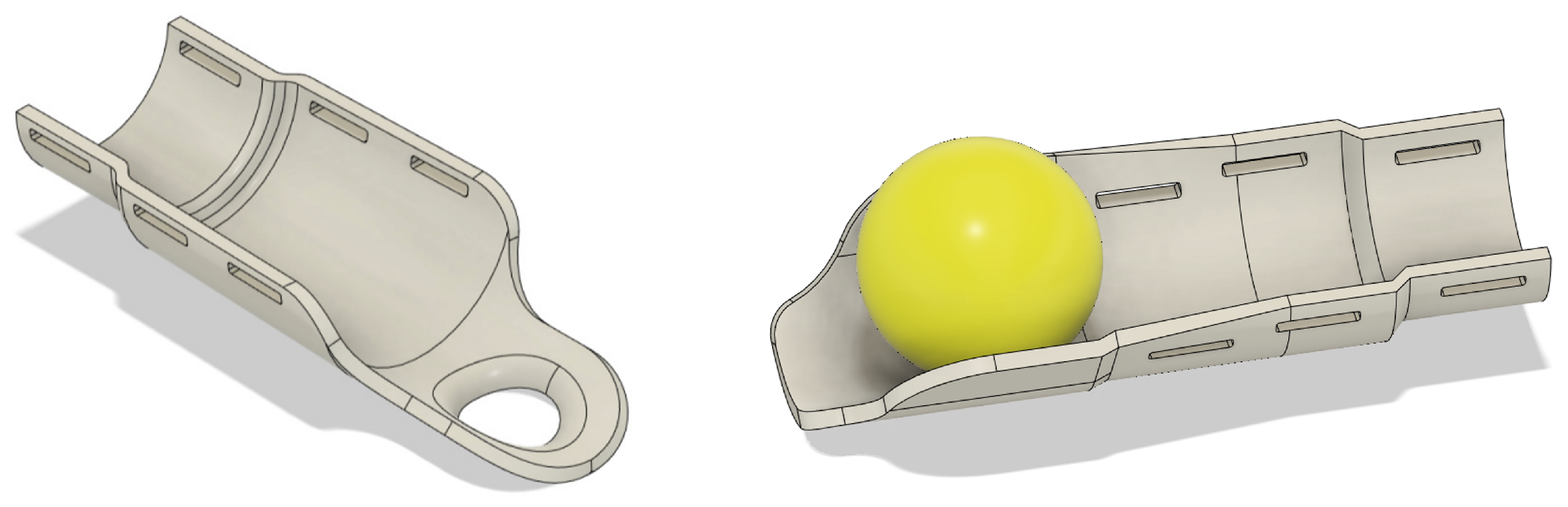
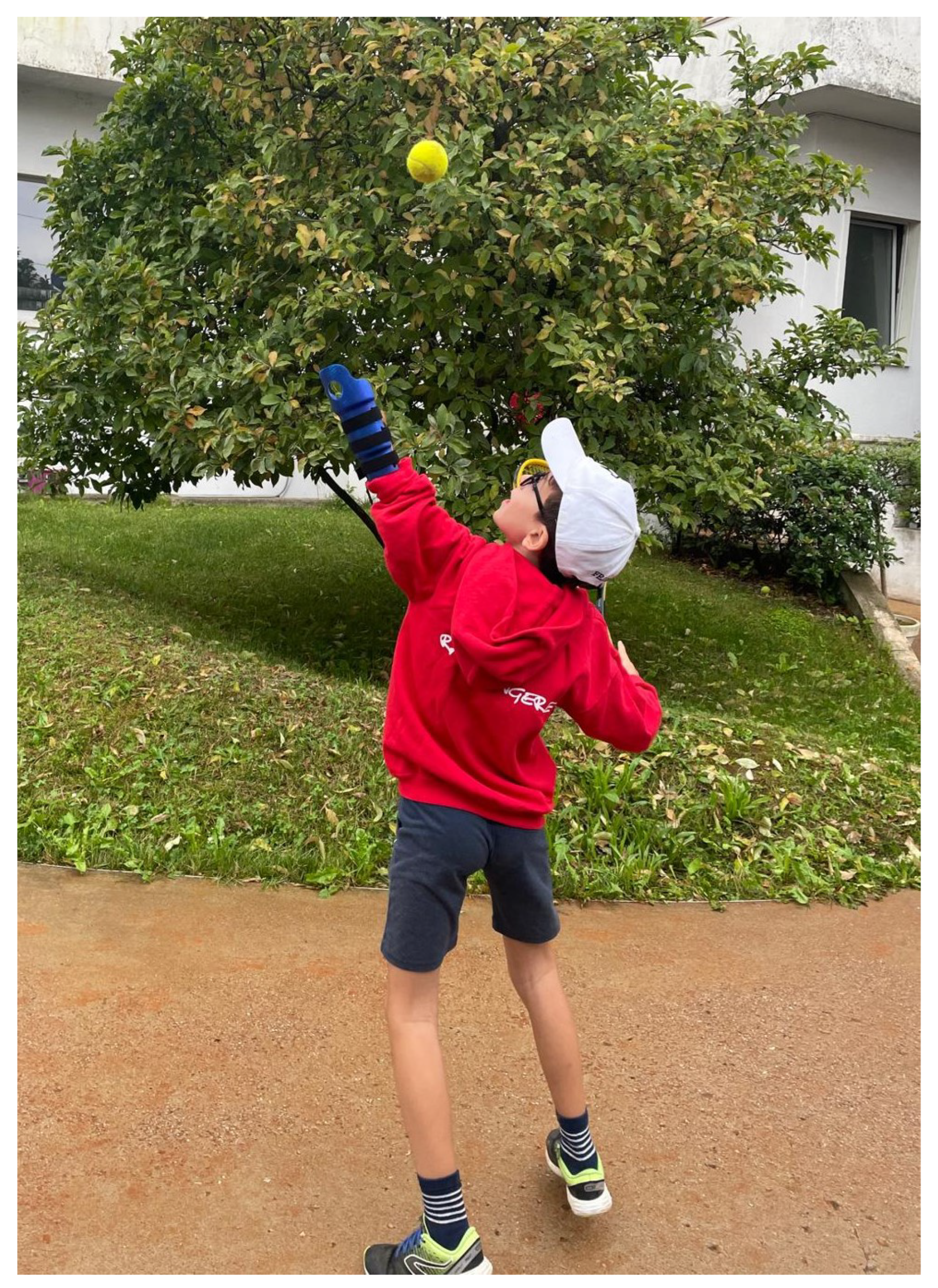
3.5. Tennis Serve Aid
- Holding the ball and the tennis racket in the same hand;
- Holding the racket under the underarm while throwing the ball;
- Throwing the ball using the racket;
- Holding the ball between the bicep and the forearm.
- Open cup: There are no other supports around the ball, which makes the device less invasive by avoiding coming in contact with the legs and sides of the child; a drawback is the reduced control on the ball (Figure 11).
- Closed cup: In this case, walls were added to the sides of the cup, enabling a better control while lifting the ball (Figure 11).
4. User Feedback
- How often is the aid being used? (i.e., never, 2/3 times a week, every day, other);
- Is the aid you are using now still suitable or has it become small? (i.e., it is fine, it is small, other);
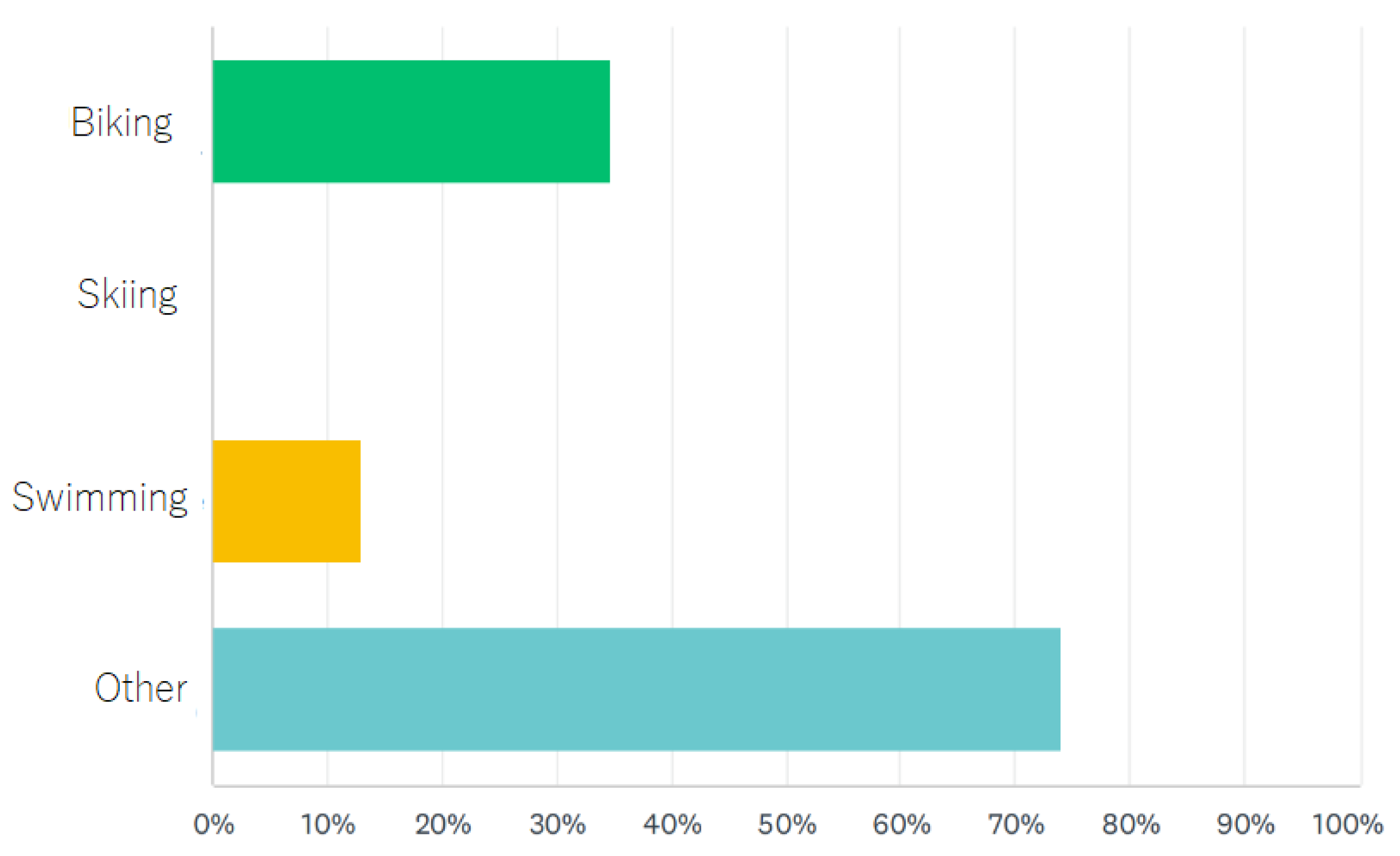
- If Io Do Una Mano were to develop new physical activity aids, which ones would be useful? (i.e., cycling, skiing, swimming, other);
- How could the Io Do Una Mano service be improved? (open question);
- What does he/she use the aid for? (i.e., going to school, playing, for physical activity, eating, other);
- What customization would he/she like to have in the next assistive device? (open question);
- What sport/hobby does he/she practice? (open question).
5. Conclusions
6. Future Developments
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Al-Dewik, N.; Samara, M.; Younes, S.; Al-Jurf, R.; Nasrallah, G.; Al-Obaidly, S.; Salama, H.; Olukade, T.; Hammuda, S.; Marlow, N.; et al. Prevalence, predictors, and outcomes of major congenital anomalies: A population-based register study. Sci. Rep. 2023, 13, 2198. [Google Scholar] [CrossRef] [PubMed]
- Oelmeier, K.; Schmitz, R.; Dera, I.; Plaßmann, M.; Braun, J.; Willy, D.; Sourouni, M.; Köster, H.A.; Steinhard, J.; Röpke, A.; et al. Congenital Limb Defects: A Retrospective Cohort Study and Overview of the Literature. Ultraschall Der Med. Eur. J. Ultrasound 2022, 44, e241–e247. [Google Scholar] [CrossRef]
- Wilcox, W.R.; Coulter, C.P.; Schmitz, M.L. Congenital limb deficiency disorders. Clin. Perinatol. 2015, 2, 281–300. [Google Scholar] [CrossRef] [PubMed]
- Maat, B.; Smit, G.; Plettenburg, D.; Breedveld, P. Passive prosthetic hands and tools: A literature review. Prosthet. Orthot. Int. 2018, 42, 66–74. [Google Scholar] [CrossRef] [PubMed]
- Toledo, C.; Leija, L.; Munoz, R.; Vera, A.; Ramirez, A. Upper limb prostheses for amputations above elbow: A review. In Proceedings of the 2009 Pan American Health Care Exchanges, Mexico City, Mexico, 16–20 March 2009; pp. 104–108. [Google Scholar]
- Ten Kate, J.; Smit, G.; Breedveld, P. 3D-printed upper limb prostheses: A review. Disabil. Rehabil. Assist. Technol. 2017, 12, 300–314. [Google Scholar] [CrossRef] [PubMed]
- Davids, J.R.; Wagner, L.V.; Meyer, L.C.; Blackhurst, D.W. Prosthetic management of children with unilateral congenital below-elbow deficiency. JBJS 2006, 88, 1294–1300. [Google Scholar] [CrossRef]
- Golea-Vasluian, E.; van Wijk, I.; Dijkstra, P.U.; Reinders-Messelink, H.; van der Sluis, C.K. Adaptive devices in young people with upper limb reduction deficiencies: Use and satisfaction. J. Rehabil. Med. 2015, 47, 346–355. [Google Scholar] [CrossRef] [PubMed]
- Parry-Hill, J.L.; Ashbrook, D.L. Challenges and Opportunities in DFO-AT: A Study of e-NABLE. 2016. Available online: http://scholarworks.rit.edu/article/1808 (accessed on 21 January 2025).
- Rahman, Z.; Barakh Ali, S.F.; Ozkan, T.; Charoo, N.A.; Reddy, I.K.; Khan, M.A. Additive manufacturing with 3D printing: Progress from bench to bedside. AAPS J. 2018, 20, 101. [Google Scholar] [CrossRef]
- Fink, C.; Diamond, Y. Prosthesis Options and Management in Upper Extremity Amputation. Oper. Tech. Orthop. 2023, 33, 101061. [Google Scholar] [CrossRef]
- Eime, R.M.; Young, J.A.; Harvey, J.T.; Charity, M.J.; Payne, W.R. A systematic review of the psychological and social benefits of participation in sport for children and adolescents: Informing development of a conceptual model of health through sport. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 98. [Google Scholar] [CrossRef]
- Warburton, D.E.; Nicol, C.W.; Bredin, S.S. Health benefits of physical activity: The evidence. Cmaj 2006, 174, 801–809. [Google Scholar] [CrossRef]
- Jara, C.A.; Esquembre, F.; Christian, W.; Candelas, F.A.; Torres, F.; Dormido, S. A new 3D visualization Java framework based on physics principles. Comput. Phys. Commun. 2012, 183, 231–244. [Google Scholar] [CrossRef]
- Calderan, P. Stampa 3D: Il Manuale per Hobbisti e Maker; Number 8; Apogeo Editore: Milan, Italy, 2015. [Google Scholar]
- Sher, D.; Marinoni, D. Stampa 3D: Tutto Quello che c’e’da Sapere Sull’unica Rivoluzione Possibile; HOEPLI EDITORE: Milan, Italy, 2015. [Google Scholar]
- Bertolino, M.; Battegazzore, D.; Arrigo, R.; Frache, A. Designing 3D printable polypropylene: Material and process optimisation through rheology. Addit. Manuf. 2021, 40, 101944. [Google Scholar] [CrossRef]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bogliolo, M.; Turolla, L.; Salvatore, F.; Segre, J.; Parodi, E.; Casadio, M. Design and 3D Printing of Low-Cost Functional Sports Devices for the Upper Limb. Prosthesis 2025, 7, 17. https://doi.org/10.3390/prosthesis7010017
Bogliolo M, Turolla L, Salvatore F, Segre J, Parodi E, Casadio M. Design and 3D Printing of Low-Cost Functional Sports Devices for the Upper Limb. Prosthesis. 2025; 7(1):17. https://doi.org/10.3390/prosthesis7010017
Chicago/Turabian StyleBogliolo, Michela, Lea Turolla, Francesco Salvatore, James Segre, Elena Parodi, and Maura Casadio. 2025. "Design and 3D Printing of Low-Cost Functional Sports Devices for the Upper Limb" Prosthesis 7, no. 1: 17. https://doi.org/10.3390/prosthesis7010017
APA StyleBogliolo, M., Turolla, L., Salvatore, F., Segre, J., Parodi, E., & Casadio, M. (2025). Design and 3D Printing of Low-Cost Functional Sports Devices for the Upper Limb. Prosthesis, 7(1), 17. https://doi.org/10.3390/prosthesis7010017






