Predicting the Need for Insulin Treatment: A Risk-Based Approach to the Management of Women with Gestational Diabetes Mellitus
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Clinical Characteristics
3.2. Multivariable Logistic Regression
3.3. Prediction Statistics for Treatment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- American Diabetes Association. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes. Diabetes Care 2018, 41 (Suppl. S1), 13–27. [CrossRef] [Green Version]
- Kamana, K.C.; Shakya, S.; Zhang, H. Gestational Diabetes Mellitus and Macrosomia: A Literature Review. Ann. Nutr. Metab. 2015, 66 (Suppl. S2), 14–20. [Google Scholar] [CrossRef]
- Pedersen, J. Diabetes and Pregnancy: Blood Sugar of Newborn Infants During Fasting and Glucose Administration. Nord. Med. 1952, 47, 1049. [Google Scholar] [PubMed]
- American College of Obstetricians and Gynecologists. Practice Bulletin No. 173: Fetal Macrosomia. [Miscellaneous Article]. Obstet. Gynecol. 2016, 128, 195–209. [Google Scholar] [CrossRef]
- Vounzoulaki, E.; Khunti, K.; Abner, S.C.; Tan, B.K.; Davies, M.J.; Gillies, C.L. Progression to Type 2 Diabetes in Women with a Known History of Gestational Diabetes: Systematic Review and Meta-analysis. BMJ 2020, 369, 1361. [Google Scholar] [CrossRef]
- Kampmann, U.; Madsen, L.R.; Skajaa, G.O.; Iversen, D.S.; Moeller, N.; Ovesen, P. Gestational Diabetes: A Clinical Update. World J. Diabetes 2015, 6, 1065–1072. [Google Scholar] [CrossRef]
- The HAPO Study Cooperative Research Group. Hyperglycemia and Adverse Pregnancy Outcomes. N. Engl. J. Med. 2008, 358, 1991–2002. [Google Scholar] [CrossRef] [Green Version]
- Crowther, C.A.; Hiller, J.E.; Moss, J.R.; McPhee, A.J.; Jeffries, W.S.; Robinson, J.S. Effect of Treatment of Gestational Diabetes Mellitus on Pregnancy Outcomes. N. Engl. J. Med. 2005, 352, 2477–2486. [Google Scholar] [CrossRef] [Green Version]
- Ovesen, P.G.; Fuglsang, J.; Andersen, M.B.; Wolff, C.; Petersen, O.B.; McIntyre, H.D. Temporal Trends in Gestational Diabetes Prevalence, Treatment, and Outcomes at Aarhus University Hospital, Skejby, between 2004 and 2016. J. Diabetes Res. 2018, 2018, 5937059. [Google Scholar] [CrossRef] [Green Version]
- Bogdanet, D.; Egan, A.; Reddin, C.; Kirwan, B.; Carmody, L.; Dunne, F. ATLANTIC DIP: Despite Insulin Therapy in Women with IADPSG Diagnosed GDM, Desired Pregnancy Outcomes Are Still Not Achieved. What are we missing? Diabetes Res. Clin. Pract. 2018, 136, 116–123. [Google Scholar] [CrossRef]
- Barnes, R.A.; Wong, T.; Ross, G.P.; Jalaludin, B.B.; Wong, V.W.; Smart, C.E.; Collins, C.E.; MacDonald-Wicks, L.; Flack, J.R. A Novel Validated Model for the Prediction of Insulin Therapy Initiation and Adverse Perinatal Outcomes in Women with Gestational Diabetes Mellitus. Diabetologia 2016, 59, 2331–2338. [Google Scholar] [CrossRef] [PubMed]
- Pertot, T.; Molyneaux, L.; Tan, K.; Ross, G.P.; Yue, D.K.; Wong, J. Can Common Clinical Parameters Be Used to Identify Patients Who Will Need Insulin Treatment in Gestational Diabetes Mellitus? Diabetes Care 2011, 34, 2214–2216. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mendez-Figueroa, H.; Daley, J.; Lopes, V.V.; Coustan, D.R. Predicting the Need for Medical Therapy in Patients with Mild Gestational Diabetes. Am. J. Perinatol. 2014, 31, 105–112. [Google Scholar] [CrossRef]
- Souza, A.C.; Costa, R.A.; Paganoti, C.F.; Rodrigues, A.S.; Zugaib, M.; Hadar, E.; Hod, M.; Francisco, R.P.V. Can We Stratify the Risk for Insulin Need in Women Diagnosed Early with Gestational Diabetes by Fasting Blood Glucose? J. Matern.-Fetal Neonatal Med. 2018, 32, 2036–2041. [Google Scholar] [CrossRef] [PubMed]
- Thériault, S.; Giguère, Y.; Massé, J.; Girouard, J.; Forest, J.C. Early Prediction of Gestational Diabetes: A Practical Model Combining Clinical and Biochemical Markers. Clin. Chem. Lab. Med. 2015, 54, 509–518. [Google Scholar] [CrossRef]
- Sapienza, A.D.; Francisco, R.P.V.; Trindade, T.C.; Zugaib, M. Factors Predicting the Need for Insulin Therapy in Patients with Gestational Diabetes Mellitus. Diabetes Res. Clin. Pract. 2010, 88, 81–86. [Google Scholar] [CrossRef]
- Liao, L.D.; Ferrara, A.; Greenberg, M.B.; Ngo, A.L.; Feng, J.; Zhang, Z.; Bradshaw, P.T.; Hubbard, A.E.; Zhu, Y. Development and Validation of Prediction Models for Gestational Diabetes Treatment Modality Using Supervised Machine Learning: A Population-based Cohort Study. BMC Med. 2022, 20, 307. [Google Scholar] [CrossRef] [PubMed]
- Eleftheriades, M.; Chatzakis, C.; Papachatzopoulou, E.; Papadopoulos, V.; Lambrinoudaki, I.; Dinas, K.; Chrousos, G.; Sotiriadis, A. Prediction of Insulin Treatment in Women with Gestational Diabetes Mellitus. Nutr. Diabetes 2021, 11, 30. [Google Scholar] [CrossRef]
- Du, R.; Li, L. Estimating the Risk of Insulin Requirement in Women Complicated by Gestational Diabetes Mellitus: A Clinical Nomogram. Diabetes Metab. Syndr. Obes. 2021, 14, 2473–2482. [Google Scholar] [CrossRef]
- Lee, S.H.; Yu, J.; Han, K.; Lee, S.W.; You, S.Y.; Kim, H.S.; Cho, J.H.; Yoon, K.H.; Kim, M.K. Predicting the Risk of Insulin-Requiring Gestational Diabetes before Pregnancy: A Model Generated from a Nationwide Population-Based Cohort Study in Korea. Endocrinol. Metab. 2023, 38, 129–138. [Google Scholar] [CrossRef]
- Ford, H.L.; Champion, I.; Wan, A.; Reddy, M.; Mol, B.W.; Rolnik, D.L. Predictors for Insulin Use in Gestational Diabetes Mellitus. Eur. J. Obs. Gynecol. Reprod. Biol. 2022, 272, 177–181. [Google Scholar] [CrossRef]
- Godkendt på Sandbjergmødet 2014: Gestationel Diabetes Mellitus (GDM). Screening og Diagnose. Available online: http://gynobsguideline.dk/wp/wp-content/uploads/2013/02/GDM-Sandbjerg-2014-godkendt-2014.pdf (accessed on 2 March 2020).
- Godkendt på Sandbjergmødet 2007: Behandling af Gestationel Diabetes Mellitus. Available online: http://gynobsguideline.dk/sandbjerg/Behandling af gestationel diabetes mellitus.pdf (accessed on 2 March 2020).
- Marsal, K.; Persson, P.; Larsen, T.; Lilja, H.; Selbing, A.; Sultan, B. Intrauterine Growth Curves Based on Ultrasonically Estimated Foetal Weights. Acta Paediatr. 1996, 85, 843–848. [Google Scholar] [CrossRef] [PubMed]
- Carter, J.V.; Pan, J.; Rai, S.N.; Galandiuk, S. ROC-ing Along: Evaluation and Interpretation of Receiver Operating Characteristic Curves. Surgery 2016, 159, 1638–1645. [Google Scholar] [CrossRef]
- Wong, V.W.; Jalaludin, B. Gestational Diabetes Mellitus: Who Requires Insulin Therapy? Aust. N. Z. J. Obstet. Gynaecol. 2011, 51, 432–436. [Google Scholar] [CrossRef] [PubMed]
- Koning, S.H.; Scheuneman, K.A.; Lutgers, H.L.; Korteweg, F.J.; Berg, G.V.D.; Sollie, K.M.; Roos, A.; van Loon, A.J.; Links, T.P.; van Tol, K.M.; et al. Risk Stratification for Healthcare Planning in Women with Gestational Diabetes Mellitus. Neth. J. Med. 2016, 74, 262–269. [Google Scholar] [PubMed]
- González-Quintero, V.H.; Istwan, N.B.; Rhea, D.J.; Tudela, C.M.; Flick, A.A.; de la Torre, L.; Stanziano, G.J. Antenatal Factors Predicting Subsequent Need for Insulin Treatment in Women with Gestational Diabetes. J. Women’s Health 2008, 17, 1183–1187. [Google Scholar] [CrossRef] [PubMed]
- Akinci, B.; Celtik, A.; Yener, S.; Yesil, S. Is Fasting Glucose Level During Oral Glucose Tolerance Test an Indicator of the Insulin Need in Gestational Diabetes? Diabetes Res. Clin. Pract. 2008, 82, 219–225. [Google Scholar] [CrossRef]
- Hoffman, L.; Nolan, C.; Wilson, J.D.; Oats, J.J.N.; Simmons, D. Gestational Diabetes Mellitus—Management Guidelines: The Australasian Diabetes in Pregnancy Society. Med. J. Aust. 1998, 169, 93–97. [Google Scholar] [CrossRef]
- Makgoba, M.; Savvidou, M.; Steer, P. An Analysis of the Interrelationship Between Maternal Age, Body Mass Index and Racial Origin in the Development of Gestational Diabetes Mellitus. BJOG 2012, 119, 276–282. [Google Scholar] [CrossRef]
- Laurie, J.G.; McIntyre, H.D. A Review of the Current Status of Gestational Diabetes Mellitus in Australia-The Clinical Impact of Changing Population Demographics and Diagnostic Criteria on Prevalence. Int. J. Environ. Res. Public Health 2020, 17, 9387. [Google Scholar] [CrossRef] [PubMed]
- Laafira, A.; White, S.W.; Griffin, C.J.; Graham, D. Impact of the New IADPSG Gestational Diabetes Diagnostic Criteria on Pregnancy Outcomes in Western Australia. Aust. N. Z. J. Obstet. Gynaecol. 2016, 56, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Fadl, H.; Saeedi, M.; Montgomery, S.; Magnuson, A.; Schwarcz, E.; Berntorp, K.; Sengpiel, V.; Storck-Lindholm, E.; Strevens, H.; Wikström, A.-K.; et al. Changing Diagnostic Criteria for Gestational Diabetes in Sweden—A Stepped Wedge National Cluster Randomised Controlled Trial—The CDC4G Study Protocol. BMC Pregnancy Childbirth 2019, 19, 398. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buckley, B.S.; Harreiter, J.; Damm, P.; Corcoy, R.; Chico, A.; Simmons, D.; Vellinga, A.; Dunne, F.; on behalf of the DALI Core Investigator Group. Gestational Diabetes Mellitus in Europe: Prevalence, Current Screening Practice and Barriers to Screening. A Review. Diabet. Med. 2012, 29, 844–854. [Google Scholar] [CrossRef] [PubMed]
- Heleniak, T.; Grunfelder, J.; Rispling, L.; Norlén, G. State of the Nordic Region 2018. Theme 1: Demography; Nordic Council of Ministers: Copenhagen, Denmark, 2018; Volume 2, pp. 48–58. [Google Scholar]

| Variable | Category | n | All GDM n = 1104 | GDM-Diet n = 822 | GDM-Insulin n = 282 | p |
|---|---|---|---|---|---|---|
| Maternal age, years * | 1104 | 31.9 (5.0) | 31.8 (5.0) | 32.0 (5.0) | 0.513 | |
| Maternal age, years ^ | ≤30 | 1104 | 442 (40.0%) | 328 (39.9%) | 114 (40.4%) | 0.888 |
| >30 | 662 (60.0%) | 494 (60.1%) | 168 (59.6%) | |||
| Ethnicity ^ | Caucasian | 948 (86.9%) | 710 (87.0%) | 238 (86.6%) | 0.549 | |
| Afro-Caribbean | 132 (12.1%) | 95 (11.6%) | 37 (13.5%) | |||
| Asian | 5 (0.5%) | 5 (0.6%) | 0 (0.0%) | |||
| Oriental | 4 (0.4%) | 4 (0.5%) | 0 (0.0%) | |||
| Other | 2 (0.2%) | 2 (0.3%) | 0 (0.0%) | |||
| Ethnicity ^ | Caucasian | 1091 | 948 (86.9%) | 710 (87.0%) | 238 (86.6%) | 0.837 |
| Non-Caucasian | 143 (13.1%) | 106 (13.0%) | 37 (13.5%) | |||
| Current smoker ^ | Yes | 1043 | 61 (5.9%) | 27 (3.4%) | 34 (14.1%) | <0.001 |
| Prepregnancy BMI, kg/m2 # | 1100 | 27.1 (8.8) | 26.1 (8.1) | 29.7 (10.3) | <0.001 | |
| Prepregnancy BMI, kg/m2 ^ | <30 | 1100 | 746 (67.8%) | 600 (73.3%) | 146 (52.0%) | <0.001 |
| ≥30 | 354 (32.3%) | 219 (36.7%) | 135 (48.0%) | |||
| Nulliparous ^ | Yes | 1104 | 490 (44.4%) | 385 (46.8%) | 105 (37.2%) | 0.005 |
| Prior history of GDM ^ | Yes | 614 | 216 (35.2%) | 127 (29.1%) | 89 (50.3%) | <0.001 |
| Prior fetal macrosomia ^ | Yes | 614 | 43 (7.0%) | 26 (6.0%) | 17 (9.6%) | 0.117 |
| Family history of diabetes ^ | Yes | 1104 | 635 (57.5%) | 493 (60.0%) | 142 (50.4%) | 0.005 |
| Gestational age at OGTT, weeks # | 1053 | 28 (4) | 28 (4) | 28 (9) | <0.001 | |
| Gestational age at OGTT, weeks ^ | <24 | 1053 | 232 (22.0%) | 141 (17.8%) | 91 (35.1%) | <0.001 |
| ≥24 | 821 (78.0%) | 653 (82.2%) | 168 (64.9%) | |||
| 2-h OGTT result, mmol/L # | 1051 | 9.8 (1.5) | 9.7 (1.1) | 10.8 (2.6) | <0.001 | |
| 2-h OGTT result, mmol/L ^ | <10.7 | 1051 | 757 (72.0%) | 633 (79.9%) | 124 (47.9%) | <0.001 |
| ≥10.7 | 294 (28.0%) | 159 (20.1%) | 135 (52.1%) | |||
| HbA1c at diagnosis, %[mmol/mol] # | 1085 | 5.4 (2.8) [35 (7)] | 5.3 (2.7) [34 (6)] | 5.7 (3.0) [39 (9)] | <0.001 | |
| HbA1c at diagnosis, %[mmol/mol] ^ | <5.5 [37] | 1085 | 688 (63.4%) | 595 (74.0%) | 93 (33.1%) | <0.001 |
| ≥5.5 [37] | 397 (36.6%) | 209 (26.0%) | 188 (66.9%) | |||
| HbA1c prior to delivery, %[mmol/mol] # | 915 | 5.5 (2.8) [37 (7)] | 5.4 (2.6) [35 (5)] | 5.8 (2.7) [40 (7)] | <0.001 | |
| HbA1c differences, %[mmol/mol] # | 919 | 2.3 (2.4) [2 (3)] | 2.3 (2.4) [2 (3)] | 2.2 (2.7) [1 (6)] | 0.032 |
| Variable | Category | n | All GDM n = 1104 | GDM-Diet n = 822 | GDM-Insulin n = 282 | p |
|---|---|---|---|---|---|---|
| Onset of labor ^ | Spontaneous | 1032 | 448 (25.2%) | 377 (45.9%) | 71 (25.2%) | <0.001 |
| Induction of labor | 447 (50.4%) | 305 (37.1%) | 142 (50.4%) | |||
| C-section | 137 (12.4%) | 76 (9.3%) | 61 (21.6%) | |||
| Mode of birth ^ | Vaginal | 1098 | 771 (70.2%) | 604 (73.7%) | 167 (60.1%) | <0.001 |
| Vacuum | 26 (2.4%) | 15 (1.8%) | 11 (4.0%) | |||
| Elective C-section | 153 (13.9%) | 98 (12.0%) | 55 (19.8%) | |||
| Emergency C-section | 148 (13.5%) | 103 (12.6%) | 45 (16.2%) | |||
| Gestation at birth, weeks # | 1104 | 39 (2) | 39 (2) | 38 (1) | <0.001 | |
| Infant sex ^ | Female | 1104 | 512 (46.4%) | 378 (46.0%) | 134 (47.5%) | 0.678 |
| Male | 592 (53.6%) | 444 (54.0%) | 148 (52.5%) | |||
| Apgar 1 min # | 1072 | 10 (1) | 10 (1) | 10 (1) | 0.002 | |
| Apgar 5 min # | 1069 | 10 (0) | 10 (0) | 10 (0) | 0.007 | |
| Apgar 10 min # | 997 | 10 (0) | 10 (0) | 10 (0) | 0.419 | |
| Birthweight, grams * | 1103 | 3515 (556) | 3464 (530) | 3663 (603) | <0.001 | |
| Birthweight, Z-score * | 1103 | 0.24 (1.24) | 0.032 (1.10) | 0.87 (1.44) | <0.001 | |
| Size category ^ | SGA | 1103 | 94 (8.5%) | 76 (9.3%) | 18 (6.4%) | <0.001 |
| AGA | 813 (73.7%) | 652 (79.3%) | 161 (57.3%) | |||
| LGA | 196 (17.8%) | 94 (11.4%) | 102 (36.3%) |
| Bivariable n = 1104 | Multivariable n = 978 | ||||||
|---|---|---|---|---|---|---|---|
| Variable | Category | OR | 95% CI | p | aOR | 95% CI | p |
| Family history of diabetes | No | 0.68 | 0.52, 0.89 | 0.005 | 0.87 | 0.61, 1.24 | 0.426 |
| Yes | 1 | — | — | 1 | — | — | |
| Current smoker | Smoker | 4.69 | 2.76, 7.94 | <0.001 | 4.20 | 2.21, 8.01 | <0.001 |
| Non-smoker | 1 | — | — | 1 | — | — | |
| Parity | Nulliparous | 1 | — | — | 1 | — | — |
| Multiparous | 1.49 | 1.13, 1.96 | 0.005 | 1.39 | 0.96, 2.00 | 0.078 | |
| Prepregnancy BMI, kg/m2 | <30 | 1 | — | — | 1 | — | — |
| ≥30 | 2.53 | 1.91, 3.35 | <0.001 | 1.71 | 1.19, 2.46 | 0.004 | |
| Gestational age at OGTT, weeks | <24 | 2.51 | 1.83, 3.43 | <0.001 | 2.86 | 1.92, 4.26 | <0.001 |
| ≥24 | 1 | — | — | 1 | — | — | |
| 2-h OGTT result, mmol/L | <10.7 | 1 | — | — | 1 | — | — |
| ≥10.7 | 4.33 | 3.21, 5.85 | <0.001 | 3.16 | 2.19, 4.57 | <0.001 | |
| HbA1c at diagnosis, %[mmol/mol] | <5.5 [37] | 1 | — | — | 1 | — | — |
| ≥5.5 [37] | 5.76 | 4.29, 7.72 | <0.001 | 3.79 | 2.64, 5.44 | <0.001 | |
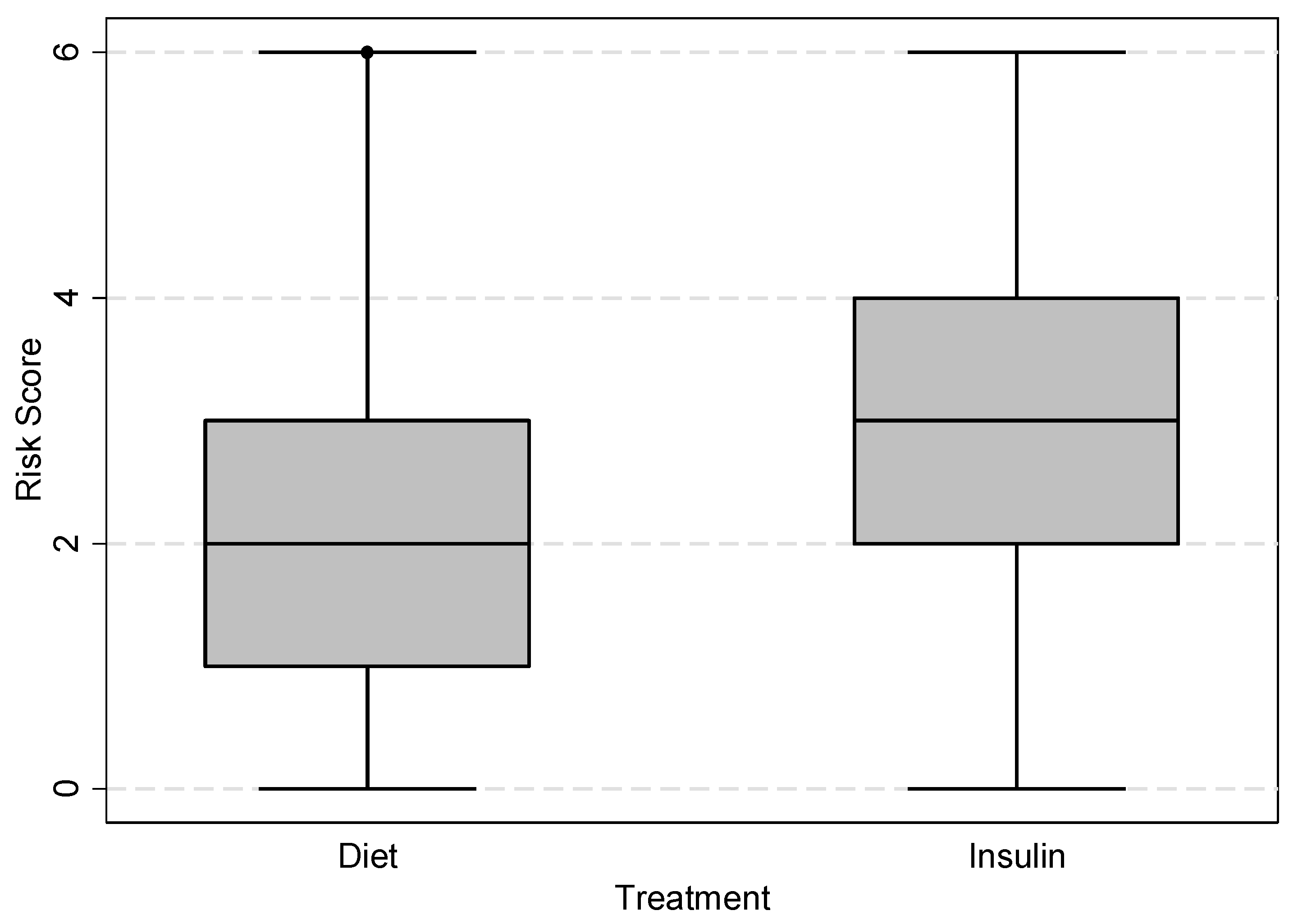
| Risk Score Tabulation | Prediction Statistics for Treatment | ||||||
|---|---|---|---|---|---|---|---|
| Risk Score | Total n = 1104 | GDM-Diet n = 822 | GDM-Insulin n = 282 | Risk Score | Total n = 1104 | GDM-Diet n = 822 | GDM-Insulin n = 282 |
| 0 | 37 (3.4%) | 36 (4.4%) | 1 (0.4%) | <3 | 642 (58.2%) | 565 (68.7%) | 77 (27.3%) |
| 1 | 275 (24.9%) | 250 (30.4%) | 25 (8.9%) | ≥3 | 462 (41.9%) | 257 (31.3%) | 205 (72.7%) |
| 2 | 330 (29.9%) | 279 (33.9%) | 51 (18.1%) | Total | 1104 (100.0%) | 822 (100.0%) | 282 (100.0%) |
| 3 | 263 (23.8%) | 175 (21.3%) | 88 (31.2%) | Sensitivity 72.7% (95% CI 67.1, 77.8) Specificity 68.7% (95% CI 65.4, 71.9) PPV 44.4% (95% CI 39.8, 49.0) NPV 88.0% (95% CI 85.2, 90.4) | |||
| 4 | 144 (13.0%) | 62 (7.5%) | 82 (29.1%) | ||||
| 5 | 43 (3.9%) | 16 (2.0%) | 27 (9.6%) | ||||
| 6 | 12 (1.1%) | 4 (0.5%) | 8 (2.8%) | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koefoed, A.S.; McIntyre, H.D.; Gibbons, K.S.; Poulsen, C.W.; Fuglsang, J.; Ovesen, P.G. Predicting the Need for Insulin Treatment: A Risk-Based Approach to the Management of Women with Gestational Diabetes Mellitus. Reprod. Med. 2023, 4, 133-144. https://doi.org/10.3390/reprodmed4030014
Koefoed AS, McIntyre HD, Gibbons KS, Poulsen CW, Fuglsang J, Ovesen PG. Predicting the Need for Insulin Treatment: A Risk-Based Approach to the Management of Women with Gestational Diabetes Mellitus. Reproductive Medicine. 2023; 4(3):133-144. https://doi.org/10.3390/reprodmed4030014
Chicago/Turabian StyleKoefoed, Anna S., H. David McIntyre, Kristen S. Gibbons, Charlotte W. Poulsen, Jens Fuglsang, and Per G. Ovesen. 2023. "Predicting the Need for Insulin Treatment: A Risk-Based Approach to the Management of Women with Gestational Diabetes Mellitus" Reproductive Medicine 4, no. 3: 133-144. https://doi.org/10.3390/reprodmed4030014
APA StyleKoefoed, A. S., McIntyre, H. D., Gibbons, K. S., Poulsen, C. W., Fuglsang, J., & Ovesen, P. G. (2023). Predicting the Need for Insulin Treatment: A Risk-Based Approach to the Management of Women with Gestational Diabetes Mellitus. Reproductive Medicine, 4(3), 133-144. https://doi.org/10.3390/reprodmed4030014







