Abstract
Reactive oxygen species (ROS) have emerged as regulators of key processes supporting neuronal growth, function, and plasticity across lifespan. At normal physiological levels, ROS perform important roles as secondary messengers in diverse molecular processes such as regulating neuronal differentiation, polarization, synapse maturation, and neurotransmission. In contrast, high levels of ROS are toxic and can ultimately lead to cell death. Excitable cells, such as neurons, often require high levels of metabolic activity to perform their functions. As a consequence, these cells are more likely to produce high levels of ROS, potentially enhancing their susceptibility to oxidative damage. In addition, because neurons are generally post-mitotic, they may be subject to accumulating oxidative damage. Thus, maintaining tight control over ROS concentration in the nervous system is essential for proper neuronal development and function. We are developing a more complete understanding of the cellular and molecular mechanisms for control of ROS in these processes. This review focuses on ROS regulation of the developmental and functional properties of neurons, highlighting recent in vivo studies. We also discuss the current evidence linking oxidative damage to pathological conditions associated with neurodevelopmental and neurodegenerative disorders.
1. Introduction
Oxygen-derived free radicals, such as the superoxide anion (O2•−) and hydroxyl radical (•OH), as well as non-radical molecules, such as hydrogen peroxide (H2O2), are collectively known as reactive oxygen species (ROS) [1,2]. ROS are produced as metabolic by-products in different subcellular locations [1,3], including mitochondria [4], endoplasmic reticulum [5], peroxisome [6], plasma membrane [7] and cytosol [8]. Exposure to pathogens, harmful chemicals, heat, UV radiation [9], and heavy metals [10] that potentially damage mitochondria can induce cycles of ROS production and increase cellular ROS concentration. ROS are highly reactive and have the capacity to interact with different biomolecules. At high concentration, ROS can damage DNA, protein, and lipid and disrupt the plasma membrane [1,11], ultimately leading to cell death [12]. Oxidative damage is implicated in several pathological conditions, including major neurodegenerative diseases such as Alzheimer’s and Parkinson’s disease [13], muscular dystrophy [14], and other disease conditions such as chronic inflammation and tissue injury [15], diabetes mellitus [16], and cancer [17]. Further, toxic oxidative metabolites can potentiate necrosis and apoptosis following neuronal injury [18]. To protect from the deleterious effects of oxidative damage, healthy cells need to be equipped with dedicated protective mechanisms such as antioxidant synthesis. Antioxidants can be either enzymatic (superoxide dismutase, catalase, glutathione peroxidases) or nonenzymatic biochemicals (flavonoid, ascorbic acid, tocopherol, etc.) [19]. When antioxidants fail to maintain the cellular ROS concentration within an appropriate physiological range, oxidative stress occurs.
Controlled Synthesis of ROS and Its Physiological Importance
When acting at appropriately controlled physiological levels, ROS serve important roles as signaling molecules. Indeed, evolutionarily conserved enzymes are dedicated to ROS synthesis. Phagocytic NADPH oxidase (Phox), the first enzyme found to anabolize ROS, was discovered over sixty years ago [20]. Since this time, well over 50 ROS generating enzymes have been identified in human cells [21]. Transmembrane protein NADPH oxidase (nicotinamide adenine dinucleotide phosphate oxidase) serves as the major anabolic source of ROS. In particular, the human genome encodes seven catalytic components of the NADPH oxidase (nicotinamide adenine dinucleotide phosphate oxidase) complex, i.e., NOX 1-5 and DUOX1-2 [20,21,22]. The NOX family enzymes, such as NOX2, reduce oxygen to superoxide [20] via transmembrane electron transport. NOX-produced superoxide is the source of all ROS (hydrogen peroxide, hydroxy radical, etc.) in the phagosome and, by killing invading pathogens, ROS serve essential roles in host defense [23]. Dual oxidases (DUOX1-2) reduce extracellular oxygen by transferring electrons from intracellular NADPH and synthesizing hydrogen peroxide (H2O2), a non-radical form of ROS [24]. Superoxide is also catabolized by the major antioxidant enzyme, superoxide dismutase, to produce H2O2. H2O2 is an important second messenger in various cellular signaling pathways [25]. For example, H2O2 inhibits phosphatase activity to regulate tyrosine phosphorylation during insulin signaling [26,27], activates MAP kinases in endothelial cells [28], and regulates ion channels and Ca2+ signaling in neurons [29].
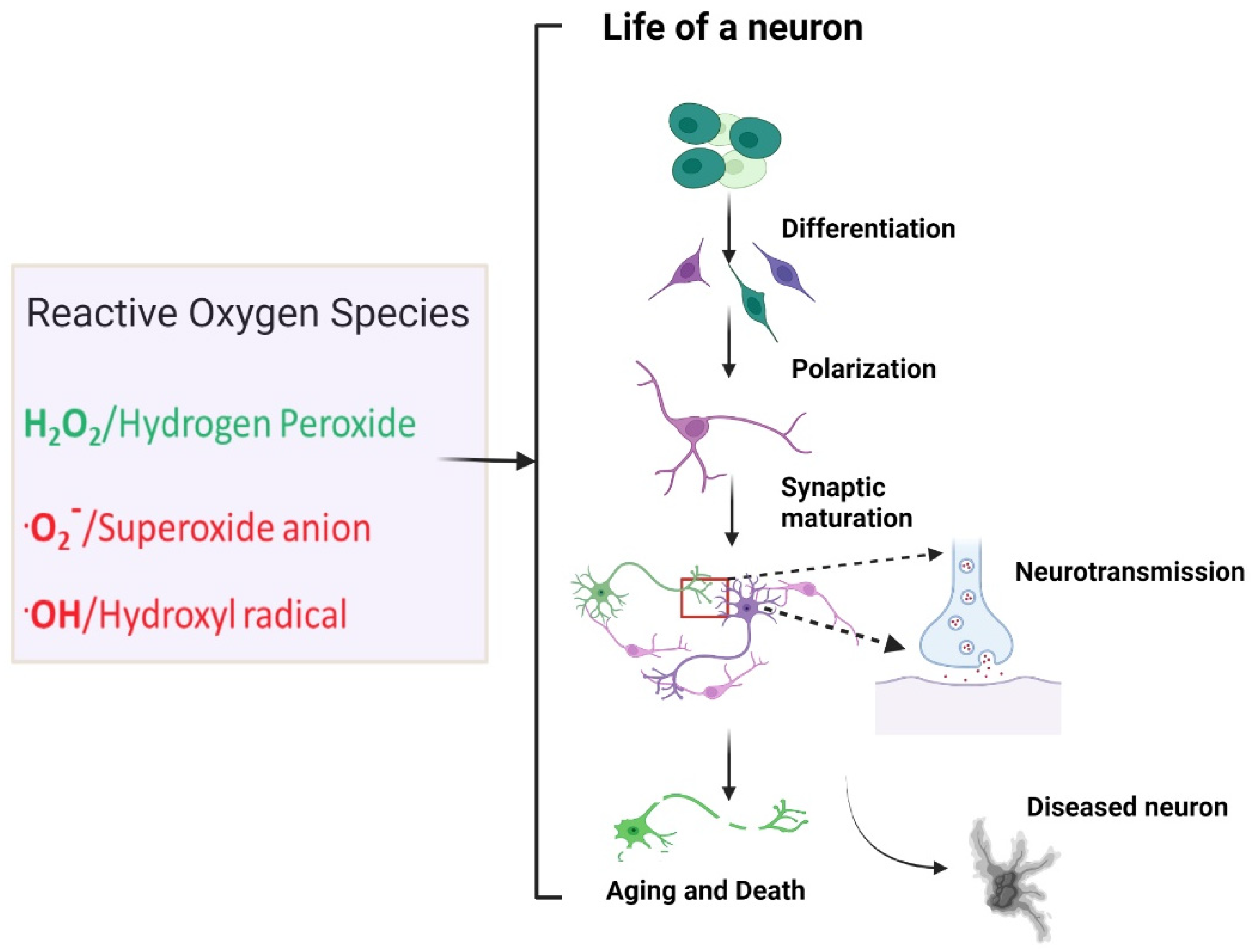
In the next section, we will focus on the roles that ROS play in neuronal development and function. NOX enzymes are highly expressed in neurons, glia (microglia, astrocytes), and neurovascular tissues [30]. In particular, ROS have crucial signaling roles in processes underlying neuronal development and neural circuit assembly. This poses the following interesting question: how do ROS manage to affect the life of a neuron in both positive and negative ways? The studies outlined in this review suggest that ROS have specific roles in either neuronal development and function or neuronal death depending on the nature of ROS, ROS concentration, site of action, and age of the organism (Figure 1).
Figure 1.
Influence of reactive oxygen species in the life of a neuron. Under normal conditions, the diffusible nonradical ROS, hydrogen peroxide, is synthesized physiologically and is a key regulator of processes fundamental to neuronal development and function, including neuronal differentiation, polarization, synaptic maturation, neuropeptide secretion, and neurotransmitter receptor transport. On the other hand, uncontrolled ROS production by damaged mitochondria, especially of superoxide and hydroxyl radicals, are potentially detrimental. Uncontrolled ROS may damage neurons, promote neuronal decline, and exacerbate neurodegenerative pathology. Created with BioRender.com (accessed on 17 February 2022).
2. ROS in Neurodevelopment
ROS signaling is an important regulator of neuronal differentiation and polarization, axon outgrowth, synapse formation, and synapse maturation [3,25]. In the following sections, we explore the relationship between ROS signaling and neurodevelopment with discussion of examples from both in vitro and in vivo studies.
2.1. ROS in Neurogenesis and Differentiation
Neurons are generated from neural stem cells and neuronal progenitors during neurogenesis. NADPH oxidases, particularly NOX2, are expressed in the developing brain during embryogenesis [25,31]. Cortical progenitors and progenitor-derived neurons actively synthesize ROS [32], suggesting that ROS may perform signaling roles in early neurogenesis. Consistent with this idea, ROS levels influence the timing of neurogenesis in the murine embryo [33]. Neuronal differentiation from primary neuronal progenitor cells and the establishment of neuronal identity depend on a complex array of biochemical interactions between growth factors such as nerve growth factor (NGF) [34] and other molecular regulators. NGF treatment triggers an increase in ROS in cultured PC12 cells. Prevention of ROS production inhibits NGF-triggered differentiation of PC12 cells, indicating that ROS may have important intracellular signaling roles during neuronal differentiation [35]. Additional evidence for ROS regulation of neuronal differentiation comes from studies of Neuregulins, a large family of EGF-like signaling molecules that are highly expressed in the nervous system. Neuregulin activation of ErbB receptor tyrosine kinases induces neurite outgrowth in PC12 cells through activation of the MAP kinase signaling pathway [36]. Interestingly, neuregulin treatment was also found to increase intracellular ROS. Treatment with a ROS scavenger inhibited both neuregulin-induced Ras and ERK activation and neuronal differentiation, implicating ROS in the molecular regulation of neuregulin-mediated differentiation [37]. Further investigation revealed that the kinetics of cellular ROS production is an important factor in the cellular decision to divide or differentiate [37].
Recent studies also provide evidence that ROS can act as signals for adult neurogenesis in both the central [38] and peripheral nervous systems [39]. Endogenous H2O2 regulates growth signaling to maintain proliferating adult hippocampal progenitor cells [40]. Similarly, inhibition of ROS biosynthesis retards proliferation and neurogenesis of neural stem cells in the adult newt brain [41]. These reports and additional accumulating evidence argue for a reconsideration of the view that ROS serve primarily deleterious roles in the nervous system and support a new acknowledgment of roles for ROS signaling in both embryonic and adult neurogenesis and differentiation.
2.2. ROS in Neurite Outgrowth and Polarization
The outgrowth of polarized axons and dendrites is a critical step in the development of brain circuits. Interestingly, ROS have emerged as positive regulators of this process. NOX synthesis of H2O2 can induce axon and dendrite formation and maturation [25]. Inhibition of the NOX complex disrupts the timing of neuronal polarization, shortens axonal length, and alters the actin cytoskeleton of cultured hippocampal neurons [42]. Furthermore, ROS regulate actin cytoskeletal dynamics and control neurite outgrowth in Aplysia neurons [43]. Recent evidence also suggests a potential role for ROS in the process of axonal specification. The polarity of hippocampal neurons is defined by a polarized distribution of evolutionarily conserved polarity proteins, such as mPar3 and mPar6. Phosphatidylinositol 3-kinase pathway (PI3′K) signaling is critical for achieving this polarized distribution [44]. Physiological levels of ROS have been shown to influence PI3′K signaling by inactivating phosphatase and tensin homolog (PTEN) [45]. It will therefore be interesting to investigate how changes in neuronal redox state might impact the subcellular distribution of polarity proteins and the selection of future axons. Normal physiological levels of ROS support neurite outgrowth and potentially axonal specification, but what molecular mechanisms are instrumental for maintaining physiological ROS concentrations in neurons? Recent findings have offered evidence that a novel feedforward mechanism involving NOX-mediated ROS production and intracellular Ca2+ signaling may have a central role [46]. Ryanodine receptor (RyR)-mediated Ca2+ release from the endoplasmic reticulum promotes axon extension and is supported by NOX-generated ROS. RyR activation also induces H2O2 production by NOX through a Rac-1 (Rac Family Small GTPase 1) dependent mechanism [46], offering a potential route for feedforward regulation. As our understanding of mechanisms for physiological regulation by ROS continues to evolve, continuing in vivo molecular studies will undoubtedly reveal new facets of the interplay between ROS and developmental regulators.
2.3. ROS Influence Growth Cone Guidance and Synaptic Maturation
Critical steps in the development of the nervous system include the growth of axons to meet their cellular partners and the subsequent formation of specialized connections called synapses. Axon outgrowth is a complex process involving dynamic changes in the neuronal cytoskeleton. These cytoskeletal dynamics are important for guiding the growing tip of the axon (growth cone) to its destination and are regulated by attractive or repulsive cues in the extracellular environment. Semaphorin is a major repulsive cue for axons, and semaphorin signaling can induce the collapse of growth cones [47]. Semaphorin3A (Sema3A) triggers microtubule disassembly through phosphorylation of the cytoskeletal component regulator, collapsin response mediator protein 2 (CRMP2) [48]. Sema3A triggers an increase in H2O2 in the growth cones of dorsal root ganglion axons through activation of the multidomain redox enzyme Mical. Subsequently, H2O2 oxidizes CRMP2, enabling phosphorylation by glycogen synthase kinase-3 (GSK-3) and promoting growth cone collapse [49]. Another recent study showed that NOX2 acts downstream of the Slit2/Robo2 signaling pathway during the growth and guidance of retinal ganglionic cell (RGC) axons in the zebrafish embryo [50]. Related studies have implicated ROS in the regulation of the growth of synapses. A genetic screen for mutants with synaptic overgrowth at the larval neuromuscular junction of Drosophila identified spinster mutants [51]. The causal mutation in spinster is a loss of function mutation in a putative lysosomal efflux permease. Lysosomal dysfunction in spinster mutants leads to an increased ROS burden. Interestingly, reduction of ROS in spinster mutants normalized the synaptic overgrowth phenotype, suggesting a link between synaptic overgrowth and oxidative stress [52]. Further work implicated ROS activation of the JNK pathway in synaptic growth [52].
Taken together, the findings described in these studies support an expanded view of physiological ROS regulation of key neurodevelopmental events, including axon guidance, synapse formation, and synapse maturation.
2.4. Mitochondrial ROS Facilitate Synaptic Pruning by Intrinsic Apoptosis
In most nervous systems, there is an excess of synaptic connections during early development compared with at maturity. Juvenile connections often undergo a refinement process called synaptic pruning, in which weaker or inappropriate connections are eliminated to generate the mature circuit [53,54]. Significant questions remain about the molecular pathways that identify such synapses and initiate their elimination. Mitochondrial ROS are emerging as potential cell-intrinsic factors important for synapse elimination [55,56]. Recent studies of motor behavior in Xenopus tadpoles suggest a regulatory role for mitochondrial ROS in synaptic pruning at the neuromuscular junction (NMJ) [56]. The authors found that forced synaptic inactivity increased mitochondrial ROS and mitochondria-targeted antioxidants reduced motor deficits associated with endogenous pruning. Interestingly, this model challenges the prevalent idea that increased neuronal activity is linked with an increase in mitochondrial ROS generation [57,58]. A follow-up communication from this group provided a hypothetical model accounting for their findings, which suggests that neuronal activity may mask a cue for pruning by suppressing mitochondrial ROS production [55]. Mitochondrial O2−/H2O2 concentration would therefore surpass the pruning threshold only at inactive synapses, thereby locally activating intrinsic apoptotic cell death signaling pathways to initiate synapse elimination or pruning [55]. Importantly, intrinsic apoptosis can be initiated, propagated and amplified by mitochondrial ROS [59,60,61]. Related studies of C. elegans neurons have shown that elimination of presynaptic material involves axonal mitochondria and apoptotic signaling [62], though specific roles for ROS in this process were not determined. An enhanced understanding of the molecular mechanisms that relate neuronal activity to ROS generation and their influence on the stability of synapses will perhaps emerge from ongoing investigations in this area.
2.5. Oxidative Damage in Neurodevelopmental Diseases
Interestingly, while physiological ROS have emerged as positive regulators of the processes underlying neuronal development, mounting evidence has also linked oxidative stress and damage with the pathophysiology of neurodevelopmental and neuropsychiatric diseases. Autism spectrum disorders (ASD) are a heterogeneous group of neurodevelopmental abnormalities that manifest as social and cognitive impairments in children and young adults. Post-mortem brain samples from temporal cortices and cerebella of autistic subjects showed a decrease in antioxidants such as glutathione (GSH) and reduced GSH/GSSG redox/antioxidant capacity [63]. Additionally, red blood cells of autistic children have altered antioxidant (SOD, catalase, and GSH) levels compared to controls [64,65]. For a detailed description of oxidative stress in ASD, readers should refer to the review by Pangrazzi [66]. Oxidative stress is also thought to influence the progression of disease pathology in schizophrenia patients [67,68]. Proteomic and metabolomic analyses of superior temporal gyrus and prefrontal cortex tissues from schizophrenic individuals revealed mitochondrial dysregulation, compromised brain metabolism, and oxidative stress [69,70]. Intriguingly, low levels of antioxidant enzymes such as GSH have also been reported in blood samples from patients with schizophrenia [67,71,72]. Because enzymatic activity remained unchanged [73], this result is most consistent with a reduction in GSH synthesis by antioxidant producing cells. Malondialdehyde (MDA) is generated by the peroxidation of membrane polyunsaturated fatty acids and is commonly used as a biomarker to assess oxidative stress [74]. High MDA levels have been reported in adult attention-deficit hyperactivity disorder (A-ADHD), which may point toward an association with oxidative stress [75,76,77]. Consistent with this, increased levels of MDA and decreased levels of the MDA catabolic enzymes paraoxonase and arylesterase were reported in patient serum. However, no correlation between these molecular parameters and disease severity was found [77]. Most studies investigating oxidative stress in the context of neurodevelopmental disease are heavily reliant on analysis of post-mortem tissue or blood serum. It is therefore difficult to assess causality from these analyses. Is oxidative damage a result of, or a cause of, neurodevelopmental abnormalities? Further investigation into important questions surrounding how ROS can both positively and negatively affect neurodevelopment will be critical for teasing apart this central problem of cause and effect. Future exploration of the molecular basis of oxidative damage in neurodevelopmental diseases may also help to identify novel drug targets and potential therapies.
3. Roles for ROS in Mature Neurons
3.1. ROS in Synaptic Plasticity
There is mounting evidence that reactive oxygen species contribute toward regulation of core neuronal functions such as neurotransmission and synaptic plasticity. Synaptic plasticity is the cellular foundation for learning and memory and refers to structural and molecular modifications at synapses that influence the strength of communication between neurons [78]. The cross-talk between ROS, Ca2+ influx, and age-related deficits in the synaptic plasticity of hippocampal neurons has been extensively reviewed elsewhere [79]. Likewise, there is a wide literature available exploring the link between ROS, synaptic plasticity, and memory [80,81,82]. Here we focus our discussion on several recent in vivo studies investigating the physiological regulation of synaptic plasticity by ROS. In Drosophila larvae, neuronal ROS were found to be instrumental for neuronal activity dependent structural plasticity of both pre and postsynaptic terminals [58]. Moreover, embryonic and larval motor neurons of Drosophila use ROS as key messengers in dendritic plasticity. For example, a recent Drosophila study showed that neuronal activity triggered extracellular H2O2 synthesis by Dual Oxidase. ROS entry into the neuron required neuronal aquaporin expression and was required for structural changes in dendritic arbors [83]. Recent work from C. elegans showed that intracellular ROS can modulate the transport and synaptic localization of AMPA-type glutamate receptors through regulation of neuronal Ca2+ signaling [84]. This study suggests a mechanistic link between physiological ROS, Ca2+ signaling, and excitatory glutamate neurotransmission. Further, studies in hippocampal neurons showed that strong Ca2+ transients prolong the lifetime of phosphorylated CREB, a key molecule involved in long-term memory, through enhanced mitochondrial super oxide production [85]. Changes in neuronal oxidative state may also alter Ca2+ signaling events that influence hippocampal memory formation [80]. Collectively, the available literature suggests that ROS regulate synaptic plasticity and memory formation in a Ca2+ dependent manner.
3.2. ROS Influence Neurotransmission
Redox influences on neurotransmission have been described for small-molecule neurotransmitters. A pioneering study at the lobster neuromuscular junction showed that H2O2 exposure decreased release of the excitatory neurotransmitter glutamate [86]. There are numerous reports of ROS effects on GABA-mediated inhibitory neurotransmission and these have been extensively reviewed [87]. In particular, patch clamp recordings from cultured mouse hippocampal neurons and CA1 pyramidal neurons in hippocampal slices showed H2O2 directly modulates GABAA receptor function [88]. Studies of the frog neuromuscular junction showed that exposure to Zn2+ and Cd2+ enhances mitochondrial ROS levels, leading to desynchronization of cholinergic neurotransmitter release [89]. This effect was ameliorated by antioxidant treatment. More recent C. elegans studies have provided evidence that axonal mitochondria and ROS production can also modulate neuropeptide release. Blocking mitochondrial transport into axons or disrupting oxidative phosphorylation inhibited neuropeptide release [90]. In addition, increases in endogenously produced H2O2 from axonal mitochondria were shown to enhance neuropeptide secretion [91]. Changes in diet were sufficient to trigger rapid alterations in endogenous ROS. Elevated neuropeptide secretion in response to endogenous ROS triggered transcriptional activation of antioxidant response genes, offering a potential mechanism for neural control of oxidative stress responses. These studies point toward a role for ROS as secondary messengers that promote neuropeptide secretion.
While there is an increasing appreciation that ROS-mediated signaling plays a positive role in the regulation of neuronal development and function, abundant evidence also links ROS dysregulation with aging neurons and neurodegenerative disease.
4. The Dark Side of ROS in the Aging Brain
ROS accumulation in the aging nervous system can have detrimental effects. The management of ROS in the nervous system depends on the timing of ROS production, cellular location, and concentration [25]. The brain accounts for only 2% of human body weight, but utilizes more than 20% of the total metabolic energy [92,93,94]. Maintaining the ionic balance across neuronal membranes, neurotransmission, and protein trafficking are all metabolically demanding processes. A typical glutamatergic neuron may utilize as much as 1.64 × 105 ATP per glutamate-filled vesicle that is released, and the energy cost for one action potential is estimated to be 7.1 × 108 ATP/neuron/spike [95]. ROS are unavoidable by-products of ATP synthesis during aerobic metabolism, produced through premature electron leakage from the mitochondrial electron transport chain (ETC) complex, resulting in an incomplete reduction of oxygen [96]. In a quiescent state, 0.2% of the total oxygen consumed during mitochondrial respiration is converted into superoxide [97]. Ferrous ions are abundant in the brain and are another factor that may serve to increase the load of potentially harmful ROS in the brain. Ferrous ions can promote the conversion of non-radical hydrogen peroxide into hydroxyl radicals through the Fenton reaction [98]. Intriguingly, though ROS produced by mitochondria are often viewed as the villain in promoting neuronal decline with aging, one interesting study suggests neuronal mitochondria are victims of ROS produced by NOX, in particular NOX4 [99]. This in-vitro study showed NOX4 is expressed in neuronal mitochondria and produces superoxide [99]. Additionally, NOX4 was found to inhibit ETC complex 1 [100]; this might further increase ROS production during ATP synthesis. In the following section, we will explore the controversial relationship between aging and oxidative stress.
4.1. Oxidative Stress in Aging
A major theory of aging, termed the free radical theory (FRTA), regards ROS accumulation as one of the earliest hallmarks of aging [101]. According to this theory, mitochondrial dysfunction is a primary cause of global cellular damage and neuronal aging. As cells age, the efficacy of the electron transport chain decreases [102], leading to premature leakage of electrons during ATP synthesis and a potential increase in the cellular concentration of ROS. Though it is clear that high levels of ROS are toxic, the roles of ROS in aging are complex and remain controversial. Numerous studies across yeast, flies, and mice have highlighted the importance of antioxidant defense mechanisms. In particular, mutation of the major antioxidant sod genes, especially mitochondrial sod-2 in yeast [103,104,105], flies [106,107], and mice [108,109] severely reduce lifespan. However, over time, the role of ROS in aging has been challenged. Seminal work in C. elegans showed that deletion of the same mitochondrial antioxidant sod-2 extends lifespan [110,111,112] and knockout of all sod genes, and thus SOD activity in C. elegans resulted in normal longevity [113]. Similarly, mice that lack one copy of Sod2 (Sod2+/−) show prolonged lifespan compared to wild-type animals despite having enhanced mitochondrial oxidative stress [114]. Additionally, elevated mitochondrial ROS failed to accelerate aging in mice [114,115]. Conversely, mutation of the mitochondrial DNA polymerase accelerated aging in mice without any increase in oxidative stress markers [116,117]. Together, these results challenge the long standing FRTA theory. Interestingly, mild mitochondrial stress triggers cytoprotective pathways such as the mitochondrial unfolded protein response (mitoUPR) that may render animals less susceptible to subsequent physiological perturbations. This phenomenon is termed mitohormesis [118,119]. Activation of the mitoUPR was shown to promote the longevity of C. elegans mutants with impaired mitochondrial respiration, such as isp-1 and clk-1 mutants [120] (clk-1/human ortholog of coenzyme Q7 and isp-1/human ortholog of ubiquinol cytochrome c reductase). These mutants live longer [121,122] despite increased levels of ROS [123]. Organismal longevity may therefore reflect an integration of the damaging effects of ROS with the activation of pro-survival pathways through processes such as mitohormesis. It will be interesting to investigate the extent to which mitohormesis contributes to ROS regulation of neuronal development and function.
A revised view of aging argues that mitochondrial ROS are unlikely to be a primary cause but may act in combination with diverse epigenetic factors and a failure of quality control mechanisms to regulate the rate of aging in the brain [117]. Neurons are non-dividing cells [124], potentially accruing high levels of ROS over time and as a consequence are potentially susceptible to protein accumulation and DNA damage [125]. Additionally, oxidative stress is regarded as a risk factor in neurodegenerative diseases including Alzheimer’s disease, Parkinson’s disease, Huntington’s disease, and amyloid lateral sclerosis [13,126]. Below we briefly discuss evidence for involvement of oxidative damage in each.
4.2. Oxidative Damage in Neurodegenerative Disorders
Physiologically, aging is characterized by a heightened sensitivity to environmental stress. External stressors, such as pathogens [127], heat [128] and radiation [129] can all lead to mitochondrial damage. Mitochondrial injury can trigger a damaging cycle of ROS production where oxidative stress exacerbates additional cellular pathologies associated with neurodegenerative disease [126]. The role of oxidative damage is widely discussed in various models of Alzheimer’s disease (AD) [130]. A major pathological hallmark of AD is the formation of amyloid β (Aβ) plaques. Aβ was shown to accumulate in mitochondria and impact mitochondrial function prior to the development of widespread extracellular Aβ deposits [131]. Genetic and pharmacological manipulations that decrease mitochondrial superoxide have been shown to reverse Aβ-induced impairment of long-term potentiation in a mouse model of AD, implicating imbalances of mitochondrial ROS in the Aβ-induced disruption of hippocampal synaptic plasticity [132]. ROS imbalances are also associated with the occurrence of motor deficits, such as resting tremor and rigidity, that are commonly observed symptoms during the progression of Parkinson’s disease (PD). Evidence for oxidative damage in PD has been comprehensively reviewed by Dias and colleagues [133]. Progressive degeneration of dopaminergic neurons in the substantia nigra (SN) is a major pathological hallmark of PD [134,135], and ROS-mediated damage to dopaminergic neurons is observed in both animal models and post-mortem brains [135]. Studies of post-mortem samples from the brains of PD patients revealed increased levels of ROS-modified biomolecules such as peroxidized lipid and the presence of protein oxidative damage in the form of carbonylated proteins [136]. NOX1 activity has been shown to increase α-synuclein expression and aggregation in both cultures of human dopaminergic neurons and rat models of PD [137], suggesting a contribution of enzymatically synthesized ROS to PD pathology. Oxidative damage is also evident in cases of Huntington’s disease (HD) [138,139], another severe neurodegenerative disorder. An autosomal dominant mutation of the huntingtin (htt) gene produces an abnormal CAG repeat expansion and gives rise to characteristic symptoms of HD such as involuntary muscle movement and muscle dystonia [140]. As HD arises from modification of a single genetic locus, HD models are powerful for understanding how environmental stressors, such as ROS, may affect the progression of neurodegenerative pathophysiology. Interestingly, HD brain samples show elevated levels of the antioxidant enzymes SOD (Zn/Cu-SOD and mitochondrial MnSOD), glutathione peroxidase, and catalase [141], suggesting an oxidative insult to the system. Finally, mitochondrial oxidative damage has been demonstrated in amyloid lateral sclerosis (ALS) [142], which primarily affects motor neurons. Mutations in the antioxidant enzyme SOD are among the most common mutations in familial forms of ALS and the most widely used transgenic models of ALS [143]. Though unlikely to be the primary cause of motor neuron death, loss of SOD1 function in some instances of familial ALS may result in oxidative damage and contribute to disease progression. In addition, examination of spinal cord tissue from sporadic ALS patients has revealed traces of lipid peroxidation and protein glycoxidation, suggesting a strong association between oxidative damage and disease [144].
4.3. ROS in Secondary Brain Injury
Acute ischemic stroke induces a rapid increase in ROS in the brain that further exacerbates primary stroke damage [145]. In a rat model of ischemia, increases in cortical ROS levels were observed soon after middle cerebral artery occlusion [146]. A recent study of brain injury following intracerebral hemmorhage (ICH) also provided evidence for ROS involvement. Brain CT scans from patients with acute ICH showed that early and high dosage of ROS scavengers significantly reduced the volume of perihematomal edema [147], a quantifiable marker of secondary brain injury post ICH [148].
5. Emerging Concepts Linking Redox Biology and Neuroscience
The dual roles of ROS as both key signaling molecules and agents of damage in the nervous system have spurred intense interest from neurobiologists. Further investigation into concentration-dependent effects of ROS and mechanisms for regulation of cellular ROS levels will be critical for understanding how ROS impact neurons under both normal and pathophysiological conditions. Specifically, additional exploration of the diverse molecular regulators that balance ROS, the molecular pathways that maintain the threshold of ROS concentration, and the mechanisms that dictate ROS action in different physiological contexts is required. An improved understanding of neuronal redox biology may help to promote the development of targeted therapies that act through modulation of cell signaling. For example, in a mouse model of AD, dietary supplementation of the mitochondrial antioxidant coenzyme Q reduced brain protein carbonyl levels, a biomarker of oxidative damage [149]. Moreover, developing biomolecular screens to identify novel neuroprotective strategies against ROS has immense therapeutic potential. Recent work has demonstrated that Baicalin, a plant-derived flavonoid, acts via Akt/Nrf2 antioxidant signaling to provide neuroprotection in a mouse model of traumatic brain injury [150].
Accumulating evidence suggests there may be differences in male and female vulnerability to neurodegenerative diseases. For instance, preclinical and clinical evidence suggest that women have higher risks for Alzheimer’s disease than men [151] and female AD patients suffer greater cognitive deterioration [152]. In contrast, the incidence of Parkinson’s disease is almost twice as high in males compared with females [153]. We still lack a molecular understanding of this sexual dimorphism and potential ROS involvement. As ROS affect almost every stage of neurodevelopment, it will be interesting to investigate whether redox modulation divergently influences the structure, function, and vulnerability of male and female nervous systems. Studies of ROS signaling and oxidative damage have typically relied heavily on biomarkers and oxidative stress assays. With the development of fluorescent sensors, we can now directly quantify ROS both in cell culture and in in vivo animal models. Genetically encoded ROS sensors such as HyPerRed [154] and redox-sensitive green fluorescent protein (roGFP) [155] offer significant advantages for investigating how physiological and environmental factors impact the redox environment of specific cell types and organelles. For example, studies using roGFP in C. elegans demonstrated that proteotoxic challenges triggered by aging had the opposite effects of the redox environments of the cytosol and endoplasmic reticulum [155]. In vivo quantification of H2O2 in the zebrafish embryo using HyPer was instrumental in demonstrating that spatiotemporal alterations in H2O2 regulate axon pathfinding [156]. Further, these sensors may be used in screens to identify novel neuron and glia signaling pathways involved in ROS regulation. Recent technical advances in fluorescent microscopy approaches have enabled the detection of redox alterations at the subcellular level using fluorescent ROS sensors. For example, two-photon fluorescence microscopy has been used to detect UV radiation induced ROS synthesis in epidermis [157]. Furthermore, super resolution or light-sheet microscopy approaches in combination with fluorescent ROS sensors offer immense potential for investigating the relationship between ROS accumulation and protein aggregation in neurodegenerative disease models. Additionally, recent advances in single cell transcriptomics present approaches with high power for investigating genetic factors that potentially contribute to cellular susceptibility to oxidative damage. For example, a recent single neuron RNA-sequencing study showed that an upregulation of mitochondrial respiratory chain complex genes is associated with oxidative damage in a mouse model of Parkinson’s disease [158]. Further, recent transcriptional profiling studies identified glutathione pathway genes as part of an oxidative stress gene signature shared across resident microglia and infiltrating macrophages in a multiple sclerosis model, uncovering a novel molecular signaling network [159]. ROS levels and redox alterations are gaining importance as indicators in therapeutic development, especially in efforts to identify drug candidates. Endogenous contrast MRI has proved useful for detecting brain ROS levels in patients before and after therapeutic interventions to manage oxidative damage [160]. Biosensors that rely on the detection of electroactive H2O2 produced by enzymatic reactions in the biosensors have recently been developed to detect neuronal release of glutamate and GABA in vivo. A microarray probe consisting of two such biosensors allowed continuous detection of glutamate and GABA in real time from cell culture or brain tissue samples [161]. The simultaneous detection of excitatory and inhibitory neurotransmitters may prove powerful in screens of drug candidates to treat brain disorders, such as epilepsy, associated with imbalances in excitation and inhibition. With the dramatic progress in biotechnology and nanomedicine over the last two decades [162], the effective delivery of ROS scavengers or other neuroprotective elements to ameliorate oxidative damage in the human brain may soon be closer to reality.
6. Significance
We have highlighted the context-dependent effects of reactive oxygen species throughout the life of a neuron, summarizing the latest advancements in the field as well as ongoing questions surrounding the roles for ROS signaling in neurodevelopmental processes and potentially destructive roles for ROS during age-related pathologies, neurodegenerative disorders, and cerebrovascular disease. Gaining an improved understanding of how ROS signaling regulates neuronal function and identifying protective molecular mechanisms that work to minimize oxidative damage in neurons will be critical for the continuing efforts to develop new therapeutic approaches to combat conditions associated with oxidative damage in the nervous system.
Author Contributions
K.B. literature mining, write up and figure; K.B. and K.A. conceptualization, discussion; K.B., K.A. and M.M.F. discussion and edits. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by National Science Foundation, grant number 1755019.
Acknowledgments
The authors thank members of the Francis laboratory for their helpful comments on the review.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Sharma, P.; Jha, A.B.; Dubey, R.S.; Pessarakli, M. Reactive Oxygen Species, Oxidative Damage, and Antioxidative Defense Mechanism in Plants under Stressful Conditions. J. Bot. 2012, 2012, 217037. [Google Scholar] [CrossRef]
- Riley, P.A. Free Radicals in Biology: Oxidative Stress and the Effects of Ionizing Radiation. Int. J. Radiat. Biol. 1994, 65, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Oswald, M.C.; Garnham, N.; Sweeney, S.T.; Landgraf, M. Regulation of Neuronal Development and Function by ROS. FEBS Lett. 2018, 592, 679–691. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Fang, H.; Groom, L.; Cheng, A.; Zhang, W.; Liu, J.; Wang, X.; Li, K.; Han, P.; Zheng, M.; et al. Superoxide Flashes in Single Mitochondria. Cell 2008, 134, 279–290. [Google Scholar] [CrossRef] [PubMed]
- Gross, E.; Sevier, C.S.; Heldman, N.; Vitu, E.; Bentzur, M.; Kaiser, C.A.; Thorpe, C.; Fass, D. Generating Disulfides Enzymatically: Reaction Products and Electron Acceptors of the Endoplasmic Reticulum Thiol Oxidase Ero1p. Proc. Natl. Acad. Sci. USA 2006, 103, 299–304. [Google Scholar] [CrossRef]
- del Río, L.A.; Sandalio, L.M.; Corpas, F.J.; Palma, J.M.; Barroso, J.B. Reactive Oxygen Species and Reactive Nitrogen Species in Peroxisomes. Production, Scavenging, and Role in Cell Signaling. Plant Physiol. 2006, 141, 330–335. [Google Scholar] [CrossRef] [PubMed]
- Crane, F.L.; Low, H. Reactive Oxygen Species Generation at the Plasma Membrane for Antibody Control. Autoimmun. Rev. 2008, 7, 518–522. [Google Scholar] [CrossRef] [PubMed]
- Kukreja, R.C.; Kontos, H.A.; Hess, M.L.; Ellis, E.F. PGH Synthase and Lipoxygenase Generate Superoxide in the Presence of NADH or NADPH. Circ. Res. 1986, 59, 612–619. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharyya, A.; Chattopadhyay, R.; Mitra, S.; Crowe, S.E. Oxidative Stress: An Essential Factor in the Pathogenesis of Gastrointestinal Mucosal Diseases. Physiol. Rev. 2014, 94, 329. [Google Scholar] [CrossRef]
- Georgiadou, E.C.; Kowalska, E.; Patla, K.; Kulbat, K.; Smolińska, B.; Leszczyńska, J.; Fotopoulos, V. Influence of Heavy Metals (Ni, Cu, and Zn) on Nitro-Oxidative Stress Responses, Proteome Regulation and Allergen Production in Basil (Ocimum basilicum L.) Plants. Front. Plant Sci. 2018, 9, 862. [Google Scholar] [CrossRef] [PubMed]
- Foyer, C.H.; Lopez-Delgado, H.; Dat, J.F.; Scott, I.M. Hydrogen Peroxide- and Glutathione-Associated Mechanisms of Acclimatory Stress Tolerance and Signalling. Physiol. Plant. 1997, 100, 241–254. [Google Scholar] [CrossRef]
- Pinto, E.; Sigaud-kutner, T.C.S.; Leitão, M.A.S.; Okamoto, O.K.; Morse, D.; Colepicolo, P. HEAVY METAL–INDUCED OXIDATIVE STRESS IN ALGAE1. J. Phycol. 2003, 39, 1008–1018. [Google Scholar] [CrossRef]
- Singh, A.; Kukreti, R.; Saso, L.; Kukreti, S. Oxidative Stress: A Key Modulator in Neurodegenerative Diseases. Molecules 2019, 24, 1583. [Google Scholar] [CrossRef] [PubMed]
- Terrill, J.R.; Radley-Crabb, H.G.; Iwasaki, T.; Lemckert, F.A.; Arthur, P.G.; Grounds, M.D. Oxidative Stress and Pathology in Muscular Dystrophies: Focus on Protein Thiol Oxidation and Dysferlinopathies. FEBS J. 2013, 280, 4149–4164. [Google Scholar] [CrossRef] [PubMed]
- Mittal, M.; Siddiqui, M.R.; Tran, K.; Reddy, S.P.; Malik, A.B. Reactive Oxygen Species in Inflammation and Tissue Injury. Antioxid. Redox Signal. 2014, 20, 1126. [Google Scholar] [CrossRef] [PubMed]
- Green, K.; Brand, M.D.; Murphy, M.P. Prevention of Mitochondrial Oxidative Damage as a Therapeutic Strategy in Diabetes. Diabetes 2004, 53, S110–S118. [Google Scholar] [CrossRef]
- Aggarwal, V.; Tuli, H.S.; Varol, A.; Thakral, F.; Yerer, M.B.; Sak, K.; Varol, M.; Jain, A.; Khan, M.A.; Sethi, G. Role of Reactive Oxygen Species in Cancer Progression: Molecular Mechanisms and Recent Advancements. Biomolecules 2019, 9, 735. [Google Scholar] [CrossRef] [PubMed]
- Poh Loh, K.; Huang, S.H.; De Silva, R.; Tan, B.K.H.; Zhu, Y.Z. Oxidative Stress: Apoptosis in Neuronal Injury. Curr. Alzheimer Res. 2006, 3, 327–337. [Google Scholar] [CrossRef]
- Balasaheb Nimse, S.; Pal, D. Free Radicals, Natural Antioxidants, and Their Reaction Mechanisms. RSC Adv. 2015, 5, 27986–28006. [Google Scholar] [CrossRef]
- Bedard, K.; Krause, K.-H. The NOX Family of ROS-Generating NADPH Oxidases: Physiology and Pathophysiology. Physiol. Rev. 2007, 87, 245–313. [Google Scholar] [CrossRef] [PubMed]
- Sies, H.; Jones, D.P. Reactive Oxygen Species (ROS) as Pleiotropic Physiological Signalling Agents. Nat. Rev. Mol. Cell Biol. 2020, 21, 363–383. [Google Scholar] [CrossRef]
- Sumimoto, H. Structure, Regulation and Evolution of Nox-Family NADPH Oxidases That Produce Reactive Oxygen Species. FEBS J. 2008, 275, 3249–3277. [Google Scholar] [CrossRef] [PubMed]
- El, J.; My, P.; Dang, C.; Gougerot, A.; Elbim, C. Phagocyte NADPH Oxidase: A Multicomponent Enzyme Essential for Host Defenses. Arch. Immunol. Ther. Exp. 2005, 53, 199–206. [Google Scholar]
- Wu, J.X.; Liu, R.; Song, K.; Chen, L. Structures of Human Dual Oxidase 1 Complex in Low-Calcium and High-Calcium States. Nat. Commun. 2021, 12, 155. [Google Scholar] [CrossRef] [PubMed]
- Wilson, C.; Muñoz-Palma, E.; González-Billault, C. From Birth to Death: A Role for Reactive Oxygen Species in Neuronal Development. Semin. Cell Dev. Biol. 2018, 80, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Denu, J.M.; Tanner, K.G. Specific and Reversible Inactivation of Protein Tyrosine Phosphatases by Hydrogen Peroxide: Evidence for a Sulfenic Acid Intermediate and Implications for Redox Regulation†. Biochemistry 1998, 37, 5633–5642. [Google Scholar] [CrossRef] [PubMed]
- Kwon, J.; Qu, C.K.; Maeng, J.S.; Falahati, R.; Lee, C.; Williams, M.S. Receptor-Stimulated Oxidation of SHP-2 Promotes T-Cell Adhesion through SLP-76–ADAP. EMBO J. 2005, 24, 2331–2341. [Google Scholar] [CrossRef] [PubMed]
- Djordjevic, T.; Pogrebniak, A.; BelAiba, R.S.; Bonello, S.; Wotzlaw, C.; Acker, H.; Hess, J.; Görlach, A. The Expression of the NADPH Oxidase Subunit P22phox Is Regulated by a Redox-Sensitive Pathway in Endothelial Cells. Free Radic. Biol. Med. 2005, 38, 616–630. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, M.C.; Sharma, R.V.; Davisson, R.L. Superoxide Mediates Angiotensin II-Induced Influx of Extracellular Calcium in Neural Cells. Hypertension 2005, 45, 717–723. [Google Scholar] [CrossRef] [PubMed]
- Nayernia, Z.; Jaquet, V.; Krause, K.-H. New Insights on NOX Enzymes in the Central Nervous System. Antioxid. Redox Signal. 2014, 20, 2815. [Google Scholar] [CrossRef] [PubMed]
- Mizuki, K.; Kadomatsu, K.; Hata, K.; Ito, T.; Fan, Q.W.; Kage, Y.; Fukumaki, Y.; Sakaki, Y.; Takeshige, K.; Sumimoto, H. Functional Modules and Expression of Mouse P40(Phox) and P67(Phox), SH3-Domain-Containing Proteins Involved in the Phagocyte NADPH Oxidase Complex. Eur. J. Biochem. 1998, 251, 573–582. [Google Scholar] [CrossRef] [PubMed]
- Tsatmali, M.; Walcott, E.C.; Makarenkova, H.; Crossin, K.L. Reactive Oxygen Species Modulate the Differentiation of Neurons in Clonal Cortical Cultures. Mol. Cell. Neurosci. 2006, 33, 345. [Google Scholar] [CrossRef] [PubMed]
- Forsberg, K.; Wuttke, A.; Quadrato, G.; Chumakov, P.M.; Wizenmann, A.; Di Giovanni, S. The Tumor Suppressor P53 Fine-Tunes Reactive Oxygen Species Levels and Neurogenesis via PI3 Kinase Signaling. J. Neurosci. 2013, 33, 14318. [Google Scholar] [CrossRef] [PubMed]
- Cattaneo, E.; McKay, R. Proliferation and Differentiation of Neuronal Stem Cells Regulated by Nerve Growth Factor. Nature 1990, 347, 762–765. [Google Scholar] [CrossRef] [PubMed]
- Suzukawa, K.; Miura, K.; Mitsushita, J.; Resau, J.; Hirose, K.; Crystal, R.; Kamata, T. Nerve Growth Factor-Induced Neuronal Differentiation Requires Generation of Rac1-Regulated Reactive Oxygen Species. J. Biol. Chem. 2000, 275, 13175–13178. [Google Scholar] [CrossRef]
- Vaskovsky, A.; Lupowitz, Z.; Erlich, S.; Pinkas-Kramarski, R. ErbB-4 Activation Promotes Neurite Outgrowth in PC12 Cells. J. Neurochem. 2000, 74, 979–987. [Google Scholar] [CrossRef]
- Goldsmit, Y.; Erlich, S.; Pinkas-Kramarski, R. Neuregulin Induces Sustained Reactive Oxygen Species Generation to Mediate Neuronal Differentiation. Cell. Mol. Neurobiol. 2001, 21, 753–769. [Google Scholar] [CrossRef] [PubMed]
- Claude, J.; Linnartz-Gerlach, B.; Kudin, A.P.; Kunz, W.S.; Neumann, H. Microglial CD33-Related Siglec-E Inhibits Neurotoxicity by Preventing the Phagocytosis-Associated Oxidative Burst. J. Neurosci. 2013, 33, 18270–18276. [Google Scholar] [CrossRef] [PubMed]
- Stemple, D.L.; Anderson, D.J. Isolation of a Stem Cell for Neurons and Glia from the Mammalian Neural Crest. Cell 1992, 71, 973–985. [Google Scholar] [CrossRef]
- Dickinson, B.C.; Peltier, J.; Stone, D.; Schaffer, D.V.; Chang, C.J. Nox2 Redox Signaling Maintains Essential Cell Populations in the Brain. Nat. Chem. Biol. 2010, 7, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Hameed, L.S.; Berg, D.A.; Belnoue, L.; Jensen, L.D.; Cao, Y.; Simon, A. Environmental Changes in Oxygen Tension Reveal ROS-Dependent Neurogenesis and Regeneration in the Adult Newt Brain. eLife 2015, 4. [Google Scholar] [CrossRef] [PubMed]
- Wilson, C.; Núñez, M.T.; González-Billault, C. Contribution of NADPH Oxidase to the Establishment of Hippocampal Neuronal Polarity in Culture. J. Cell Sci. 2015, 128, 2989–2995. [Google Scholar] [CrossRef]
- Munnamalai, V.; Suter, D.M. Reactive Oxygen Species Regulate F-Actin Dynamics in Neuronal Growth Cones and Neurite Outgrowth. J. Neurochem. 2009, 108, 644–661. [Google Scholar] [CrossRef] [PubMed]
- Shi, S.H.; Jan, L.Y.; Jan, Y.N. Hippocampal Neuronal Polarity Specified by Spatially Localized MPar3/MPar6 and PI 3-Kinase Activity. Cell 2003, 112, 63–75. [Google Scholar] [CrossRef]
- Leslie, N.R.; Bennett, D.; Lindsay, Y.E.; Stewart, H.; Gray, A.; Downes, C.P. Redox Regulation of PI 3-Kinase Signalling via Inactivation of PTEN. EMBO J. 2003, 22, 5501. [Google Scholar] [CrossRef]
- Wilson, C.; Muñoz-Palma, E.; Henríquez, D.R.; Palmisano, I.; Núñez, M.T.; Di Giovanni, S.; González-Billault, C. A Feed-Forward Mechanism Involving the NOX Complex and RyR-Mediated Ca2+ Release During Axonal Specification. J. Neurosci. 2016, 36, 11107–11119. [Google Scholar] [CrossRef]
- Yazdani, U.; Terman, J.R. The Semaphorins. Genome Biol. 2006, 7, 211. [Google Scholar] [CrossRef] [PubMed]
- Goshima, Y.; Nakamura, F.; Strittmatter, P.; Strittmatter, S.M. Collapsin-Induced Growth Cone Collapse Mediated by an Intracellular Protein Related to UNC-33. Nature 1995, 376, 509–514. [Google Scholar] [CrossRef] [PubMed]
- Morinaka, A.; Yamada, M.; Itofusa, R.; Funato, Y.; Yoshimura, Y.; Nakamura, F.; Yoshimura, T.; Kaibuchi, K.; Goshima, Y.; Hoshino, M.; et al. Thioredoxin Mediates Oxidation-Dependent Phosphorylation of CRMP2 and Growth Cone Collapse. Sci. Signal. 2011, 4, ra26. [Google Scholar] [CrossRef] [PubMed]
- Terzi, A.; Roeder, H.; Weaver, C.J.; Suter, D.M. Neuronal NADPH Oxidase 2 Regulates Growth Cone Guidance Downstream of Slit2/Robo2. Dev. Neurobiol. 2021, 81, 3. [Google Scholar] [CrossRef] [PubMed]
- Sweeney, S.T.; Davis, G.W. Unrestricted Synaptic Growth in Spinster—A Late Endosomal Protein Implicated in TGF-β-Mediated Synaptic Growth Regulation. Neuron 2002, 36, 403–416. [Google Scholar] [CrossRef]
- Milton, V.J.; Jarrett, H.E.; Gowers, K.; Chalak, S.; Briggs, L.; Robinson, I.M.; Sweeney, S.T. Oxidative Stress Induces Overgrowth of the Drosophila Neuromuscular Junction. Proc. Natl. Acad. Sci. USA 2011, 108, 17521–17526. [Google Scholar] [CrossRef] [PubMed]
- Feinberg, I. Schizophrenia: Caused by a Fault in Programmed Synaptic Elimination during Adolescence? J. Psychiatr. Res. 1982, 17, 319–334. [Google Scholar] [CrossRef]
- Sakai, J. Core Concept: How Synaptic Pruning Shapes Neural Wiring during Development and, Possibly, in Disease. Proc. Natl. Acad. Sci. USA 2020, 117, 16096–16099. [Google Scholar] [CrossRef] [PubMed]
- Cobley, J.N. Synapse Pruning: Mitochondrial ROS with Their Hands on the Shears. BioEssays 2018, 40, 1800031. [Google Scholar] [CrossRef]
- Sidlauskaite, E.; Gibson, J.W.; Megson, I.L.; Whitfield, P.D.; Tovmasyan, A.; Batinic-Haberle, I.; Murphy, M.P.; Moult, P.R.; Cobley, J.N. Mitochondrial ROS Cause Motor Deficits Induced by Synaptic Inactivity: Implications for Synapse Pruning. Redox Biol. 2018, 16, 344–351. [Google Scholar] [CrossRef] [PubMed]
- Hongpaisan, J.; Winters, C.A.; Andrews, S.B. Strong Calcium Entry Activates Mitochondrial Superoxide Generation, Upregulating Kinase Signaling in Hippocampal Neurons. J. Neurosci. 2004, 24, 10878–10887. [Google Scholar] [CrossRef] [PubMed]
- Oswald, M.C.W.; Brooks, P.S.; Zwart, M.F.; Mukherjee, A.; West, R.J.H.; Giachello, C.N.G.; Morarach, K.; Baines, R.A.; Sweeney, S.T.; Landgraf, M. Reactive Oxygen Species Regulate Activity- Dependent Neuronal Plasticity in Drosophila. eLife 2018, 7, e39393. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Perez, C.; Roy, S.S.; Naghdi, S.; Lin, X.; Davies, E.; Hajnóczky, G. Bid-Induced Mitochondrial Membrane Permeabilization Waves Propagated by Local Reactive Oxygen Species (ROS) Signaling. Proc. Natl. Acad. Sci. USA 2012, 109, 4497–4502. [Google Scholar] [CrossRef]
- Ricci, J.-E.; Gottlieb, R.A.; Green, D.R. Caspase-Mediated Loss of Mitochondrial Function and Generation of Reactive Oxygen Species during Apoptosis. J. Cell Biol. 2003, 160, 65–75. [Google Scholar] [CrossRef] [PubMed]
- Redza-Dutordoir, M.; Averill-Bates, D.A. Activation of Apoptosis Signalling Pathways by Reactive Oxygen Species. Biochim. Biophys. Acta 2016, 1863, 2977–2992. [Google Scholar] [CrossRef]
- Meng, L.; Mulcahy, B.; Cook, S.J.; Neubauer, M.; Wan, A.; Jin, Y.; Yan, D. The Cell Death Pathway Regulates Synapse Elimination through Cleavage of Gelsolin in Caenorhabditis Elegans Neurons. Cell Rep. 2015, 11, 1737–1748. [Google Scholar] [CrossRef]
- Rose, S.; Melnyk, S.; Pavliv, O.; Bai, S.; Nick, T.G.; Frye, R.E.; James, S.J. Evidence of Oxidative Damage and Inflammation Associated with Low Glutathione Redox Status in the Autism Brain. Transl. Psychiatry 2012, 2, e134. [Google Scholar] [CrossRef] [PubMed]
- James, S.J.; Melnyk, S.; Jernigan, S.; Pavliv, O.; Trusty, T.; Lehman, S.; Seidel, L.; Gaylor, D.W.; Cleves, M.A. A Functional Polymorphism in the Reduced Folate Carrier Gene and DNA Hypomethylation in Mothers of Children with Autism. Am. J. Med. Genet. B Neuropsychiatr. Genet. 2010, 153B, 1209–1220. [Google Scholar] [CrossRef] [PubMed]
- Al-Gadani, Y.; El-Ansary, A.; Attas, O.; Al-Ayadhi, L. Metabolic Biomarkers Related to Oxidative Stress and Antioxidant Status in Saudi Autistic Children. Clin. Biochem. 2009, 42, 1032–1040. [Google Scholar] [CrossRef]
- Pangrazzi, L.; Balasco, L.; Bozzi, Y. Oxidative Stress and Immune System Dysfunction in Autism Spectrum Disorders. Int. J. Mol. Sci. 2020, 21, 3293. [Google Scholar] [CrossRef]
- Bitanihirwe, B.K.Y.; Woo, T.-U.W. Oxidative Stress in Schizophrenia: An Integrated Approach. Neurosci. Biobehav. Rev. 2011, 35, 878. [Google Scholar] [CrossRef] [PubMed]
- Reddy, R.D.; Yao, J.K. Free Radical Pathology in Schizophrenia: A Review. Prostaglandins Leukot. Essent. Fat. Acids 1996, 55, 33–43. [Google Scholar] [CrossRef]
- Martins-de-Souza, D.; Gattaz, W.F.; Schmitt, A.; Novello, J.C.; Marangoni, S.; Turck, C.W.; Dias-Neto, E. Proteome Analysis of Schizophrenia Patients Wernicke’s Area Reveals an Energy Metabolism Dysregulation. BMC Psychiatry 2009, 9, 17. [Google Scholar] [CrossRef] [PubMed]
- Prabakaran, S.; Swatton, J.E.; Ryan, M.M.; Huffaker, S.J.; Huang, J.T.J.; Griffin, J.L.; Wayland, M.; Freeman, T.; Dudbridge, F.; Lilley, K.S.; et al. Mitochondrial Dysfunction in Schizophrenia: Evidence for Compromised Brain Metabolism and Oxidative Stress. Mol. Psychiatry 2004, 9, 684–697. [Google Scholar] [CrossRef]
- Dadheech, G.; Mishra, S.; Gautam, S.; Sharma, P. Evaluation of Antioxidant Deficit in Schizophrenia. Indian J. Psychiatry 2008, 50, 16. [Google Scholar] [CrossRef] [PubMed]
- Yao, J.K.; Leonard, S.; Reddy, R. Altered Glutathione Redox State in Schizophrenia. Dis. Markers 2006, 22, 83. [Google Scholar] [CrossRef] [PubMed]
- Kuloglu, M.; Ustundag, B.; Atmaca, M.; Canatan, H.; Ertan Tezcan, A.; Cinkilinc, N. Lipid Peroxidation and Antioxidant Enzyme Levels in Patients with Schizophrenia and Bipolar Disorder. Cell Biochem. Funct. 2002, 20, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Esterbauer, H.; Schaur, R.J.; Zollner, H. Chemistry and Biochemistry of 4-Hydroxynonenal, Malonaldehyde and Related Aldehydes. Free Radic. Biol. Med. 1991, 11, 81–128. [Google Scholar] [CrossRef]
- Bulut, M.; Selek, S.; Gergerlioglu, H.S.; Savas, H.A.; Yilmaz, H.R.; Yuce, M.; Ekici, G. Malondialdehyde Levels in Adult Attention-Deficit Hyperactivity Disorder. J. Psychiatry Neurosci. 2007, 32, 435. [Google Scholar]
- Popa-Wagner, A.; Mitran, S.; Sivanesan, S.; Chang, E.; Buga, A.M. ROS and Brain Diseases: The Good, the Bad, and the Ugly. Oxid. Med. Cell. Longev. 2013, 2013, 963520. [Google Scholar] [CrossRef]
- Bulut, M.; Selek, S.; Bez, Y.; Cemal Kaya, M.; Gunes, M.; Karababa, F.; Celik, H.; Asuman Savas, H. Lipid Peroxidation Markers in Adult Attention Deficit Hyperactivity Disorder: New Findings for Oxidative Stress. Psychiatry Res. 2013, 209, 638–642. [Google Scholar] [CrossRef] [PubMed]
- Citri, A.; Malenka, R.C. Synaptic Plasticity: Multiple Forms, Functions, and Mechanisms. Neuropsychopharmacology 2007, 33, 18–41. [Google Scholar] [CrossRef] [PubMed]
- Hidalgo, C.; Arias-Cavieres, A. Calcium, Reactive Oxygen Species, and Synaptic Plasticity. Physiology 2016, 31, 201–215. [Google Scholar] [CrossRef] [PubMed]
- Massaad, C.A.; Klann, E. Reactive Oxygen Species in the Regulation of Synaptic Plasticity and Memory. Antioxid. Redox Signal. 2011, 14, 2013. [Google Scholar] [CrossRef] [PubMed]
- Kishida, K.T.; Klann, D.E. Sources and Targets of Reactive Oxygen Species in Synaptic Plasticity and Memory. Antioxid. Redox Signal. 2006, 9, 233–244. [Google Scholar] [CrossRef]
- Knapp, L.T.; Klann, E. Role of Reactive Oxygen Species in Hippocampal Long-Term Potentiation: Contributory or Inhibitory? J. Neurosci. Res. 2002, 70, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Dhawan, S.; Myers, P.; Bailey, D.M.D.; Ostrovsky, A.D.; Evers, J.F.; Landgraf, M. Reactive Oxygen Species Mediate Activity-Regulated Dendritic Plasticity Through NADPH Oxidase and Aquaporin Regulation. Front. Cell. Neurosci. 2021, 15, 237. [Google Scholar] [CrossRef] [PubMed]
- Doser, R.L.; Amberg, G.C.; Hoerndli, F.J. Reactive Oxygen Species Modulate Activity-Dependent AMPA Receptor Transport in C. Elegans. J. Neurosci. 2020, 40, 7405–7420. [Google Scholar] [CrossRef] [PubMed]
- Hongpaisan, J.; Winters, C.A.; Andrews, S.B. Calcium-Dependent Mitochondrial Superoxide Modulates Nuclear CREB Phosphorylation in Hippocampal Neurons. Mol. Cell. Neurosci. 2003, 24, 1103–1115. [Google Scholar] [CrossRef] [PubMed]
- Colton, C.A.; Colton, J.S.; Gilbert, D.L. Changes in Synaptic Transmission Produced by Hydrogen Peroxide. J. Free Radic. Biol. Med. 1986, 2, 141–148. [Google Scholar] [CrossRef]
- Beltrán González, A.N.; López Pazos, M.I.; Calvo, D.J. Reactive Oxygen Species in the Regulation of the GABA Mediated Inhibitory Neurotransmission. Neuroscience 2020, 439, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Penna, A.; Wang, D.S.; Yu, J.; Lecker, I.; Brown, P.M.G.E.; Bowie, D.; Orser, B.A. Hydrogen Peroxide Increases GABAA Receptor-Mediated Tonic Current in Hippocampal Neurons. J. Neurosci. 2014, 34, 10624. [Google Scholar] [CrossRef] [PubMed]
- Tsentsevitsky, A.N.; Zakyrjanova, G.F.; Petrov, A.M. Cadmium Desynchronizes Neurotransmitter Release in the Neuromuscular Junction: Key Role of ROS. Free Radic. Biol. Med. 2020, 155, 19–28. [Google Scholar] [CrossRef]
- Jia, Q.; Sieburth, D. Mitochondrial Hydrogen Peroxide Positively Regulates Neuropeptide Secretion during Diet-Induced Activation of the Oxidative Stress Response. Nat. Commun. 2021, 12, 1–22. [Google Scholar] [CrossRef]
- Zhao, T.; Hao, Y.; Kaplan, J.M. Axonal Mitochondria Modulate Neuropeptide Secretion Through the Hypoxic Stress Response in Caenorhabditis Elegans. Genetics 2018, 210, 275–285. [Google Scholar] [CrossRef] [PubMed]
- Sparaco, M.; Gaeta, L.M.; Santorelli, F.M.; Passarelli, C.; Tozzi, G.; Bertini, E.; Simonati, A.; Scaravilli, F.; Taroni, F.; Duyckaerts, C.; et al. Friedreich’s Ataxia: Oxidative Stress and Cytoskeletal Abnormalities. J. Neurol. Sci. 2009, 287, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Rolfe, D.F.S.; Brown, G.C. Cellular Energy Utilization and Molecular Origin of Standard Metabolic Rate in Mammals. Physiol. Rev. 1997, 77, 731–758. [Google Scholar] [CrossRef]
- Weil, A. Metabolism of the Nervous System. J. Neuropathol. Exp. Neurol. 1958, 17, 661. [Google Scholar] [CrossRef][Green Version]
- Attwell, D.; Laughlin, S.B. An Energy Budget for Signaling in the Grey Matter of the Brain. J. Cereb. Blood Flow Metab. 2001, 21, 1133–1145. [Google Scholar] [CrossRef] [PubMed]
- Jastroch, M.; Divakaruni, A.S.; Mookerjee, S.; Treberg, J.R.; Brand, M.D. Mitochondrial Proton and Electron Leaks. Essays Biochem. 2010, 47, 53. [Google Scholar] [CrossRef] [PubMed]
- Addabbo, F.; Montagnani, M.; Goligorsky, M.S. Mitochondria and Reactive Oxygen Species. Hypertension 2009, 53, 885–892. [Google Scholar] [CrossRef] [PubMed]
- Gerlach, M.; Ben-Shachar, D.; Riederer, P.; Youdim, M.B.H. Altered Brain Metabolism of Iron as a Cause of Neurodegenerative Diseases? J. Neurochem. 1994, 63, 793–807. [Google Scholar] [CrossRef] [PubMed]
- Case, A.J.; Li, S.; Basu, U.; Tian, J.; Zimmerman, M.C. Mitochondria in Cardiovascular Physiology and Disease: Mitochondrial-Localized NADPH Oxidase 4 Is a Source of Superoxide in Angiotensin II-Stimulated Neurons. Am. J. Physiol. Hear. Circ. Physiol. 2013, 305, H19. [Google Scholar] [CrossRef]
- Kozieł, R.; Pircher, H.; Kratochwil, M.; Lener, B.; Hermann, M.; Dencher, N.A.; Jansen-Dürr, P. Mitochondrial Respiratory Chain Complex I Is Inactivated by NADPH Oxidase Nox4. Biochem. J. 2013, 452, 231–239. [Google Scholar] [CrossRef] [PubMed]
- HARMAN, D. The Free Radical Theory of Aging: Effect of Age on Serum Copper Levels. J. Gerontol. 1965, 20, 151–153. [Google Scholar] [CrossRef]
- López-Otín, C.; Blasco, M.A.; Partridge, L.; Serrano, M.; Kroemer, G. The Hallmarks of Aging. Cell 2013, 153, 1194. [Google Scholar] [CrossRef] [PubMed]
- Longo, V.D.; Gralla, E.B.; Valentine, J.S. Superoxide Dismutase Activity Is Essential for Stationary Phase Survival in Saccharomyces Cerevisiae. Mitochondrial Production of Toxic Oxygen Species in Vivo. J. Biol. Chem. 1996, 271, 12275–12280. [Google Scholar] [CrossRef] [PubMed]
- Fabrizio, P.; Liou, L.L.; Moy, V.N.; Diaspro, A.; Valentine, J.S.; Gralla, E.B.; Longo, V.D. SOD2 Functions Downstream of Sch9 to Extend Longevity in Yeast. Genetics 2003, 163, 35–46. [Google Scholar] [CrossRef] [PubMed]
- Wawryn, J.; Krzepiłko, A.; Myszka, A.; Biliński, T. Deficiency in Superoxide Dismutases Shortens Life Span of Yeast Cells. Acta Biochim. Pol. 1999, 46, 249–253. [Google Scholar] [CrossRef] [PubMed]
- Kirby, K.; Hu, J.; Hilliker, A.J.; Phillips, J.P. RNA Interference-Mediated Silencing of Sod2 in Drosophila Leads to Early Adult-Onset Mortality and Elevated Endogenous Oxidative Stress. Proc. Natl. Acad. Sci. USA 2002, 99, 16162–16167. [Google Scholar] [CrossRef] [PubMed]
- Duttaroy, A.; Paul, A.; Kundu, M.; Belton, A. A Sod2 Null Mutation Confers Severely Reduced Adult Life Span in Drosophila. Genetics 2003, 165, 2295–2299. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Huang, T.T.; Carlson, E.J.; Melov, S.; Ursell, P.C.; Olson, J.L.; Noble, L.J.; Yoshimura, M.P.; Berger, C.; Chan, P.H.; et al. Dilated Cardiomyopathy and Neonatal Lethality in Mutant Mice Lacking Manganese Superoxide Dismutase. Nat. Genet. 1995, 11, 376–381. [Google Scholar] [CrossRef]
- Lebovitz, R.M.; Zhang, H.; Vogel, H.; Cartwright, J.; Dionne, L.; Lu, N.; Huang, S.; Matzuk, M.M. Neurodegeneration, Myocardial Injury, and Perinatal Death in Mitochondrial Superoxide Dismutase-Deficient Mice. Proc. Natl. Acad. Sci. USA 1996, 93, 9782–9787. [Google Scholar] [CrossRef] [PubMed]
- Van Raamsdonk, J.M.; Hekimi, S. Reactive Oxygen Species and Aging in Caenorhabditis Elegans: Causal or Casual Relationship? Antioxid. Redox Signal. 2010, 13, 1911–1953. [Google Scholar] [CrossRef] [PubMed]
- Hekimi, S.; Lapointe, J.; Wen, Y. Taking a “Good” Look at Free Radicals in the Aging Process. Trends Cell Biol. 2011, 21, 569. [Google Scholar] [CrossRef]
- Van Raamsdonk, J.M.; Hekimi, S. Deletion of the Mitochondrial Superoxide Dismutase Sod-2 Extends Lifespan in Caenorhabditis Elegans. PLoS Genet. 2009, 5, e1000361. [Google Scholar] [CrossRef] [PubMed]
- Van Raamsdonk, J.M.; Hekimi, S. Superoxide Dismutase Is Dispensable for Normal Animal Lifespan. Proc. Natl. Acad. Sci. USA 2012, 109, 5785–5790. [Google Scholar] [CrossRef] [PubMed]
- Van Remmen, H.; Ikeno, Y.; Hamilton, M.; Pahlavani, M.; Wolf, N.; Thorpe, S.R.; Alderson, N.L.; Baynes, J.W.; Epstein, C.J.; Huang, T.T.; et al. Life-Long Reduction in MnSOD Activity Results in Increased DNA Damage and Higher Incidence of Cancer but Does Not Accelerate Aging. Physiol. Genom. 2004, 16, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Ikeno, Y.; Qi, W.; Chaudhuri, A.; Li, Y.; Bokov, A.; Thorpe, S.R.; Baynes, J.W.; Epstein, C.; Richardson, A.; et al. Mice Deficient in Both Mn Superoxide Dismutase and Glutathione Peroxidase-1 Have Increased Oxidative Damage and a Greater Incidence of Pathology but No Reduction in Longevity. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2009, 64, 1212. [Google Scholar] [CrossRef]
- Kujoth, C.C.; Hiona, A.; Pugh, T.D.; Someya, S.; Panzer, K.; Wohlgemuth, S.E.; Hofer, T.; Seo, A.Y.; Sullivan, R.; Jobling, W.A.; et al. Medicine: Mitochondrial DNA Mutations, Oxidative Stress, and Apoptosis in Mammalian Aging. Science 2005, 309, 481–484. [Google Scholar] [CrossRef] [PubMed]
- Stefanatos, R.; Sanz, A. The Role of Mitochondrial ROS in the Aging Brain. FEBS Lett. 2018, 592, 743–758. [Google Scholar] [CrossRef] [PubMed]
- Yun, J.; Finkel, T. Mitohormesis. Cell Metab. 2014, 19, 757–766. [Google Scholar] [CrossRef] [PubMed]
- Ristow, M.; Schmeisser, K. Mitohormesis: Promoting Health and Lifespan by Increased Levels of Reactive Oxygen Species (ROS). Dose-Response 2014, 12, 288–341. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; Senchuk, M.M.; Dues, D.J.; Johnson, B.K.; Cooper, J.F.; Lew, L.; Machiela, E.; Schaar, C.E.; DeJonge, H.; Blackwell, T.K.; et al. Mitochondrial Unfolded Protein Response Transcription Factor ATFS-1 Promotes Longevity in a Long-Lived Mitochondrial Mutant through Activation of Stress Response Pathways. BMC Biol. 2018, 16, 147. [Google Scholar] [CrossRef] [PubMed]
- Lakowski, B.; Hekimi, S. Determination of Life-Span in Caenorhabditis Elegans by Four Clock Genes. Science 1996, 272, 1010–1013. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Bussière, F.; Hekimi, S. Mitochondrial Electron Transport Is a Key Determinant of Life Span in Caenorhabditis Elegans. Dev. Cell 2001, 1, 633–644. [Google Scholar] [CrossRef]
- Lee, S.J.; Hwang, A.B.; Kenyon, C. Inhibition of Respiration Extends C. Elegans Life Span via Reactive Oxygen Species That Increase HIF-1 Activity. Curr. Biol. 2010, 20, 2131–2136. [Google Scholar] [CrossRef]
- Aranda-Anzaldo, A.; Dent, M.A.R. Why Cortical Neurons Cannot Divide, and Why Do They Usually Die in the Attempt? J. Neurosci. Res. 2017, 95, 921–929. [Google Scholar] [CrossRef] [PubMed]
- Castelli, V.; Benedetti, E.; Antonosante, A.; Catanesi, M.; Pitari, G.; Ippoliti, R.; Cimini, A.; d’Angelo, M. Neuronal Cells Rearrangement During Aging and Neurodegenerative Disease: Metabolism, Oxidative Stress and Organelles Dynamic. Front. Mol. Neurosci. 2019, 12, 132. [Google Scholar] [CrossRef] [PubMed]
- Angelova, P.R.; Abramov, A.Y. Role of Mitochondrial ROS in the Brain: From Physiology to Neurodegeneration. FEBS Lett. 2018, 592, 692–702. [Google Scholar] [CrossRef] [PubMed]
- Elesela, S.; Lukacs, N.W. Role of Mitochondria in Viral Infections. Life 2021, 11, 232. [Google Scholar] [CrossRef] [PubMed]
- White, M.G.; Saleh, O.; Nonner, D.; Barrett, E.F.; Moraes, C.T.; Barrett, J.N. Mitochondrial Dysfunction Induced by Heat Stress in Cultured Rat CNS Neurons. J. Neurophysiol. 2012, 108, 2203. [Google Scholar] [CrossRef]
- Kam, W.W.Y.; Banati, R.B. Effects of Ionizing Radiation on Mitochondria. Free Radic. Biol. Med. 2013, 65, 607–619. [Google Scholar] [CrossRef]
- Abramov, A.Y.; Berezhnov, A.V.; Fedotova, E.I.; Zinchenko, V.P.; Dolgacheva, L.P. Interaction of Misfolded Proteins and Mitochondria in Neurodegenerative Disorders. Biochem. Soc. Trans. 2017, 45, 1025–1033. [Google Scholar] [CrossRef]
- Caspersen, C.; Wang, N.; Yao, J.; Sosunov, A.; Chen, X.; Lustbader, J.W.; Xu, H.W.; Stern, D.; McKhann, G.; Yan, S. Du Mitochondrial Aβ: A Potential Focal Point for Neuronal Metabolic Dysfunction in Alzheimer’s Disease. FASEB J. 2005, 19, 2040–2041. [Google Scholar] [CrossRef] [PubMed]
- Ma, T.; Hoeffer, C.A.; Wong, H.; Massaad, C.A.; Zhou, P.; Iadecola, C.; Murphy, M.P.; Pautler, R.G.; Klann, E. Amyloid β-Induced Impairments in Hippocampal Synaptic Plasticity Are Rescued by Decreasing Mitochondrial Superoxide. J. Neurosci. 2011, 31, 5589. [Google Scholar] [CrossRef]
- Dias, V.; Junn, E.; Mouradian, M.M. The Role of Oxidative Stress in Parkinson’s Disease. J. Parkinsons. Dis. 2013, 3, 461. [Google Scholar] [CrossRef]
- Sulzer, D.; Surmeier, D.J. Neuronal Vulnerability, Pathogenesis, and Parkinson’s Disease. Mov. Disord. 2013, 28, 715–724. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.D.; Zhao, X.; Li, Y.; Li, G.R.; Liu, X.L. Damage to Dopaminergic Neurons by Oxidative Stress in Parkinson’s Disease (Review). Int. J. Mol. Med. 2018, 41, 1817–1825. [Google Scholar] [CrossRef] [PubMed]
- Beal, M.F. Oxidatively Modified Proteins in Aging and Disease. Free Radic. Biol. Med. 2002, 32, 797–803. [Google Scholar] [CrossRef]
- Cristóvão, A.C.; Guhathakurta, S.; Bok, E.; Je, G.; Yoo, S.D.; Choi, D.H.; Kim, Y.S. NADPH Oxidase 1 Mediates α-Synucleinopathy in Parkinson’s Disease. J. Neurosci. 2012, 32, 14465. [Google Scholar] [CrossRef]
- Browne, S.E.; Ferrante, R.J.; Beal, M.F. Oxidative Stress in Huntington’s Disease. Brain Pathol. 1999, 9, 147–163. [Google Scholar] [CrossRef]
- Kumar, A.; Ratan, R.R. Oxidative Stress and Huntington’s Disease: The Good, The Bad, and The Ugly. J. Huntingtons. Dis. 2016, 5, 217. [Google Scholar] [CrossRef] [PubMed]
- Schulte, J.; Littleton, J.T. The Biological Function of the Huntingtin Protein and Its Relevance to Huntington’s Disease Pathology. Curr. Trends Neurol. 2011, 5, 65–78. [Google Scholar]
- Quinti, L.; Naidu, S.D.; Träger, U.; Chen, X.; Kegel-Gleason, K.; Llères, D.; Connolly, C.; Chopra, V.; Low, C.; Moniot, S.; et al. KEAP1-Modifying Small Molecule Reveals Muted NRF2 Signaling Responses in Neural Stem Cells from Huntington’s Disease Patients. Proc. Natl. Acad. Sci. USA 2017, 114, E4676–E4685. [Google Scholar] [CrossRef] [PubMed]
- Shaw, I.C.; Fitzmaurice, P.S.; Mitchell, J.D.; Lynch, P.G. Studies on Cellular Free Radical Protection Mechanisms in the Anterior Horn from Patients with Amyotrophic Lateral Sclerosis. Neurodegeneration 1995, 4, 391–396. [Google Scholar] [CrossRef]
- Julien, J.P.; Kriz, J. Transgenic Mouse Models of Amyotrophic Lateral Sclerosis. Biochim. Biophys. Acta Mol. Basis Dis. 2006, 1762, 1013–1024. [Google Scholar] [CrossRef] [PubMed]
- Shibata, N.; Nagai, R.; Uchida, K.; Horiuchi, S.; Yamada, S.; Hirano, A.; Kawaguchi, M.; Yamamoto, T.; Sasaki, S.; Kobayashi, M. Morphological Evidence for Lipid Peroxidation and Protein Glycoxidation in Spinal Cords from Sporadic Amyotrophic Lateral Sclerosis Patients. Brain Res. 2001, 917, 97–104. [Google Scholar] [CrossRef]
- Rodrigo, R.; Fernandez-Gajardo, R.; Gutierrez, R.; Matamala, J.; Carrasco, R.; Miranda-Merchak, A.; Feuerhake, W. Oxidative Stress and Pathophysiology of Ischemic Stroke: Novel Therapeutic Opportunities. CNS Neurol. Disord. Drug Targets 2013, 12, 698–714. [Google Scholar] [CrossRef]
- Peters, O.; Back, T.; Lindauer, U.; Busch, C.; Megow, D.; Dreier, J.; Dirnagl, U. Increased Formation of Reactive Oxygen Species after Permanent and Reversible Middle Cerebral Artery Occlusion in the Rat. J. Cereb. Blood Flow Metab. 1998, 18, 196–205. [Google Scholar] [CrossRef]
- Kim, M.; Byun, J.; Chung, Y.; Lee, S.U.; Park, J.E.; Park, W.; Park, J.C.; Ahn, J.S.; Lee, S. Reactive Oxygen Species Scavenger in Acute Intracerebral Hemorrhage Patients: A Multicenter, Randomized Controlled Trial. Stroke 2021, 52, 1172–1181. [Google Scholar] [CrossRef]
- Urday, S.; Kimberly, W.T.; Beslow, L.A.; Vortmeyer, A.O.; Selim, M.H.; Rosand, J.; Simard, J.M.; Sheth, K.N. Targeting Secondary Injury in Intracerebral Haemorrhage—Perihaematomal Oedema. Nat. Rev. Neurol. 2015, 11, 111–122. [Google Scholar] [CrossRef]
- Wadsworth, T.L.; Bishop, J.A.; Pappu, A.S.; Woltjer, R.L.; Quinn, J.F. Evaluation of Coenzyme Q as an Antioxidant Strategy for Alzheimer’s Disease. J. Alzheimer’s Dis. 2008, 14, 225. [Google Scholar] [CrossRef] [PubMed]
- Fang, J.; Wang, H.; Zhou, J.; Dai, W.; Zhu, Y.; Zhou, Y.; Wang, X.; Zhou, M. Baicalin Provides Neuroprotection in Traumatic Brain Injury Mice Model through Akt/Nrf2 Pathway. Drug Des. Devel. Ther. 2018, 12, 2497. [Google Scholar] [CrossRef]
- Fisher, D.W.; Bennett, D.A.; Dong, H. Sexual Dimorphism in Predisposition to Alzheimer’s Disease. Neurobiol. Aging 2018, 70, 308. [Google Scholar] [CrossRef] [PubMed]
- Irvine, K.; Laws, K.R.; Gale, T.M.; Kondel, T.K. Greater Cognitive Deterioration in Women than Men with Alzheimer’s Disease: A Meta Analysis. J. Clin. Exp. Neuropsychol. 2012, 34, 989–998. [Google Scholar] [CrossRef]
- Baldereschi, M.; Di Carlo, A.; Rocca, W.A.; Vanni, P.; Maggi, S.; Perissinotto, E.; Grigoletto, F.; Amaducci, L.; Inzitari, D. Parkinson’s Disease and Parkinsonism in a Longitudinal Study. Neurology 2000, 55, 1358–1363. [Google Scholar] [CrossRef]
- Ermakova, Y.G.; Bilan, D.S.; Matlashov, M.E.; Mishina, N.M.; Markvicheva, K.N.; Subach, O.M.; Subach, F.V.; Bogeski, I.; Hoth, M.; Enikolopov, G.; et al. Red Fluorescent Genetically Encoded Indicator for Intracellular Hydrogen Peroxide. Nat. Commun. 2014, 5, 5222. [Google Scholar] [CrossRef]
- Kirstein, J.; Morito, D.; Kakihana, T.; Sugihara, M.; Minnen, A.; Hipp, M.S.; Nussbaum-Krammer, C.; Kasturi, P.; Hartl, F.U.; Nagata, K.; et al. Proteotoxic Stress and Ageing Triggers the Loss of Redox Homeostasis across Cellular Compartments. EMBO J. 2015, 34, 2334–2349. [Google Scholar] [CrossRef]
- Gauron, C.; Meda, F.; Dupont, E.; Albadri, S.; Quenech’Du, N.; Ipendey, E.; Volovitch, M.; Del Bene, F.; Joliot, A.; Rampon, C.; et al. Hydrogen Peroxide (H2O2) Controls Axon Pathfinding during Zebrafish Development. Dev. Biol. 2016, 414, 133–141. [Google Scholar] [CrossRef] [PubMed]
- Hanson, K.M.; Clegg, R.M. Two-Photon Fluorescence Imaging and Reactive Oxygen Species Detection Within the Epidermis. Methods Mol. Biol. 2005, 289, 413–421. [Google Scholar] [CrossRef] [PubMed]
- Zhong, J.; Tang, G.; Zhu, J.; Wu, W.; Li, G.; Lin, X.; Liang, L.; Chai, C.; Zeng, Y.; Wang, F.; et al. Single-Cell Brain Atlas of Parkinson’s Disease Mouse Model. J. Genet. Genom. 2021, 48, 277–288. [Google Scholar] [CrossRef] [PubMed]
- Mendiola, A.S.; Ryu, J.K.; Bardehle, S.; Meyer-Franke, A.; Ang, K.K.H.; Wilson, C.; Baeten, K.M.; Hanspers, K.; Merlini, M.; Thomas, S.; et al. Transcriptional Profiling and Therapeutic Targeting of Oxidative Stress in Neuroinflammation. Nat. Immunol. 2020, 21, 513. [Google Scholar] [CrossRef] [PubMed]
- Tain, R.-W.; Scotti, A.M.; Li, W.; Zhou, X.J.; Cai, K. Imaging Short-Lived Reactive Oxygen Species (ROS) with Endogenous Contrast MRI. J. Magn. Reson. Imaging 2018, 47, 222. [Google Scholar] [CrossRef]
- Hossain, I.; Tan, C.; Doughty, P.T.; Dutta, G.; Murray, T.A.; Siddiqui, S.; Iasemidis, L.; Arumugam, P.U. A Novel Microbiosensor Microarray for Continuous Ex Vivo Monitoring of Gamma-Aminobutyric Acid in Real-Time. Front. Neurosci. 2018, 12, 500. [Google Scholar] [CrossRef] [PubMed]
- Nash, K.M.; Ahmed, S. Nanomedicine in the ROS-Mediated Pathophysiology: Applications and Clinical Advances. Nanomedicine 2015, 11, 2033. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).