ATTR Variant Amyloidosis in Patients with Dysphagia
Abstract
1. Introduction
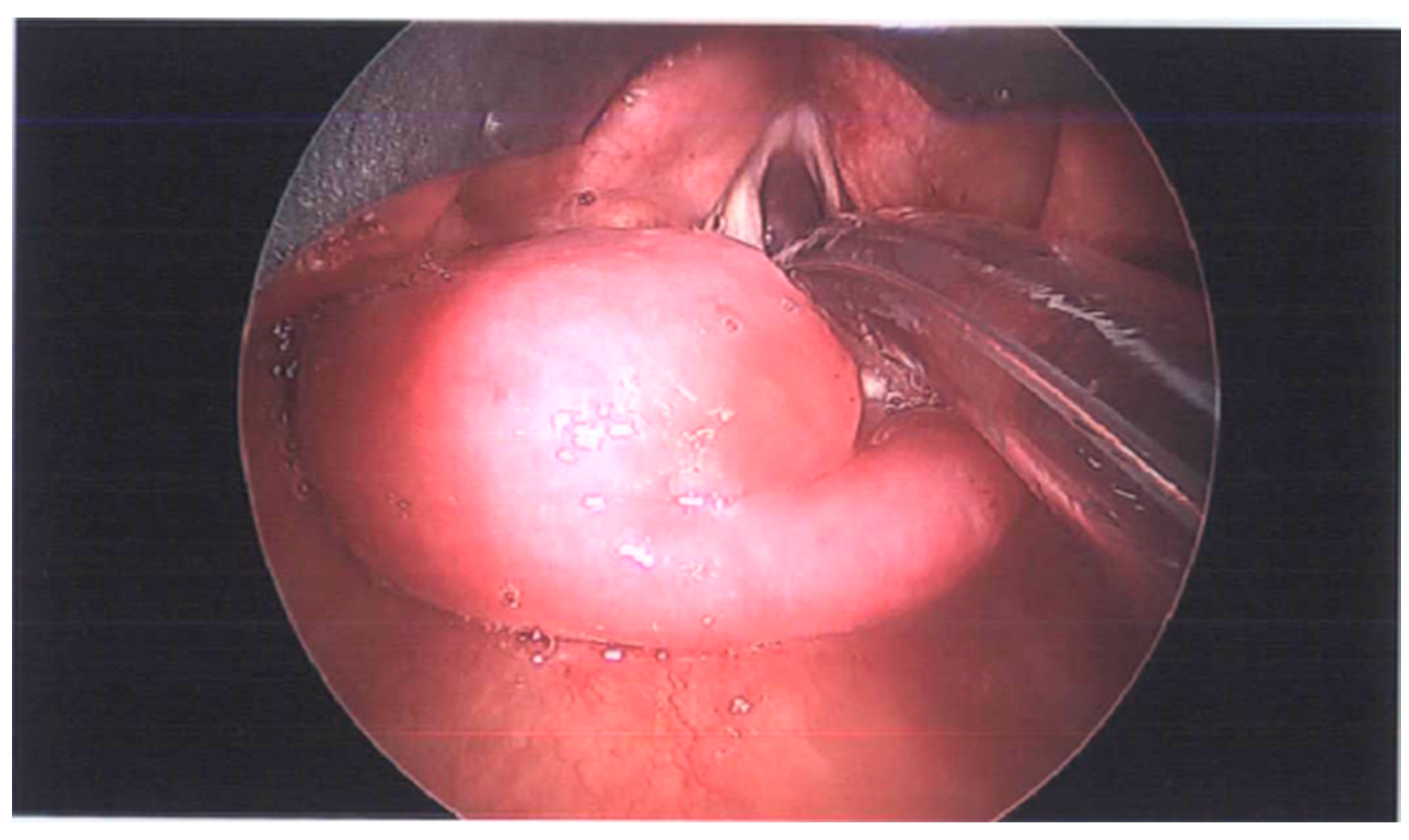
2. Detailed Case Description
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wechalekar, A.D.; Gillmore, J.D.; Hawkins, P.N. Systemic amyloidosis. Lancet 2016, 387, 2641–2654. [Google Scholar] [CrossRef] [PubMed]
- Rudy, S.F.; Jeffery, C.C.; Damrose, E.J. Clinical characteristics of laryngeal versus nonlaryngeal amyloidosis. Laryngoscope 2018, 128, 670–674. [Google Scholar] [CrossRef]
- Falk, R.H.; Comenzo, R.L.; Skinner, M. The Systemic Amyloidoses. N. Engl. J. Med. 1997, 337, 898–909. [Google Scholar] [CrossRef] [PubMed]
- Hazenberg, B.P.C. Amyloidosis: A clinical overview. Rheum. Dis. Clin. 2013, 39, 323–345. [Google Scholar] [CrossRef]
- Hammami, B.; Mnejja, M.; Kallel, S.; Bouguecha, L.; Chakroun, A.; Charfeddine, I.; Ghorbel, A. Hypopharyngeal amyloidosis: A case report. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2010, 127, 83–85. [Google Scholar] [CrossRef]
- Stevenson, R.; Witteles, R.; Damrose, E.; Arai, S.; Lafayette, R.A.; Schrier, S.; Afghahi, A.; Liedtke, M. More Than a Frog in the Throat: A Case Series and Review of Localized Laryngeal Amyloidosis. Arch. Otolaryngol. Neck Surg. 2012, 138, 509–511. [Google Scholar] [CrossRef] [PubMed]
- Harris, G.; Lachmann, H.; Hawkins, P.; Sandhu, G. One Hundred Cases of Localized Laryngeal Amyloidosis—Evidence for Future Management. Laryngoscope 2021, 131, E1912–E1917. [Google Scholar] [CrossRef]
- Gertz, M.A.; Benson, M.D.; Dyck, P.J.; Grogan, M.; Coelho, T.; Cruz, M.; Berk, J.L.; Plante-Bordeneuve, V.; Schmidt, H.H.; Merlini, G. Diagnosis, Prognosis, and Therapy of Transthyretin Amyloidosis. J. Am. Coll. Cardiol. 2015, 66, 2451–2466. [Google Scholar] [CrossRef]
- Connors, L.H.; Lim, A.; Prokaeva, T.; Roskens, V.A.; Costello, C.E. Tabulation of human transthyretin (TTR) variants, 2003. Amyloid 2003, 10, 160–184. [Google Scholar] [CrossRef]
- Vieira, M.; Saraiva, M.J. Transthyretin: A multifaceted protein. Biomol. Concepts 2014, 5, 45–54. [Google Scholar] [CrossRef]
- Hellman, U.; Alarcon, F.; Lundgren, H.E.; Suhr, O.B.; Bonaiti-PelliÉ, C.; Planté-Bordeneuve, V. Heterogeneity of penetrance in familial amyloid polyneuropathy, ATTR Val30Met, in the Swedish population. Amyloid 2008, 15, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Teng, C.; Li, P.; Bae, J.Y.; Pan, S.; Dixon, R.A.F.; Liu, Q. Diagnosis and treatment of transthyretin-related amyloidosis cardiomyopathy. Clin. Cardiol. 2020, 43, 1223–1231. [Google Scholar] [CrossRef] [PubMed]
- Puig-Carrion, G.D.; Reyentovich, A.; Katz, S.D. Diagnosis and treatment of heart failure in hereditary transthyretin amyloidosis. Clin. Auton. Res. 2019, 29, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa, M.; Sekijima, Y.; Yazaki, M.; Tojo, K.; Yoshinaga, T.; Doden, T.; Koyama, J.; Yanagisawa, S.; Ikeda, S.-I. Carpal tunnel syndrome: A common initial symptom of systemic wild-type ATTR (ATTRwt) amyloidosis. Amyloid 2016, 23, 58–63. [Google Scholar] [CrossRef]
- Chadwick, M.A.; Buckland, J.R.; Mason, P.; Randall, C.J.; Theaker, J. A rare case of dysphagia: Hypopharyngeal amyloidosis masquerading as a post-cricoid tumour. J. Laryngol. Otol. 2002, 116, 54–56. [Google Scholar] [CrossRef]
- Ghekiere, O.; Desuter, G.; Weynand, B.; Coche, E. Hypopharyngeal Amyloidoma. Am. J. Roentgenol. 2003, 181, 1720–1721. [Google Scholar] [CrossRef]
- Bartier, S.; Bodez, D.; Kharoubi, M.; Canouï-Poitrine, F.; Chatelin, V.; Henrion, C.; Coste, A.; Damy, T.; Béquignon, E. Pharyngo-laryngeal involvement in systemic amyloidosis with cardiac involvement: A prospective observational study. Amyloid 2019, 26, 216–224. [Google Scholar] [CrossRef]
- Ohki, M.; Kikuchi, S. Dysphagia due to systemic light chain amyloidosis revealed by videoendoscopic and videofluorographic swallowing examinations. Otolaryngol. Case Rep. 2018, 6, 4–6. [Google Scholar] [CrossRef]
- Muchtar, E.; Derudas, D.; Mauermann, M.; Liewluck, T.; Dispenzieri, A.; Kumar, S.K.; Dingli, D.; Lacy, M.Q.; Buadi, F.K.; Hayman, S.R.; et al. Systemic Immunoglobulin Light Chain Amyloidosis–Associated Myopathy: Presentation, Diagnostic Pitfalls, and Outcome. Mayo Clin. Proc. 2016, 91, 1354–1361. [Google Scholar] [CrossRef]
- Rubinow, A.; Burakoff, R.; Cohen, A.S.; Harris, L.D. Esophageal manometry in systemic amyloidosis. A study of 30 patients. Am. J. Med. 1983, 75, 951–956. [Google Scholar] [CrossRef]
- Abbas, Z.; Abid, S.; Rehman, N.U.; Pervez, S. Primary amyloidosis of gut presenting with dysphagia. J. Pak. Med. 1995, 45, 274–275. [Google Scholar]
- Iida, T.; Yamano, H.; Nakase, H. Systemic amyloidosis with gastrointestinal involvement: Diagnosis from endoscopic and histological views. J. Gastroenterol. Hepatol. 2018, 33, 583–590. [Google Scholar] [CrossRef] [PubMed]
- Andrew, J. Cowan, Martha Skinner, David C. Seldin; et al. Amyloidosis of the gastrointestinal tract: A 13-year, single-center, referral experience. Haematologica 2013, 98, 141–146. [Google Scholar] [CrossRef]
- Tada, S.; Lida, M.; Iwashita, A.; Matsui, T.; Fuchigami, T.; Yamamoto, T.; Yao, T.; Fujishima, M. Endoscopic and biopsy findings of the upper digestive tract in patients with amyloidosis. Gastrointest. Endosc. 1990, 36, 10–14. [Google Scholar] [CrossRef] [PubMed]
- Coelho, T.; Maurer, M.S.; Suhr, O.B. THAOS—The Transthyretin Amyloidosis Outcomes Survey: Initial report on clinical manifestations in patients with hereditary and wild-type transthyretin amyloidosis. Curr. Med. Res. Opin. 2013, 29, 63–76. [Google Scholar] [CrossRef]
- Garcia, Y.; Collins, A.B.; Stone, J.R. Abdominal fat pad excisional biopsy for the diagnosis and typing of systemic amyloidosis. Human Pathol. 2018, 72, 71–79. [Google Scholar] [CrossRef]
- Witteles, R. Cardiac Amyloidosis. 2016. Available online: https://www.acc.org/latest-in-cardiology/articles/2016/07/07/14/59/cardiac-amyloidosis (accessed on 9 May 2023).
- Conaghan, P.; Chung, D.; Vaughan, R. Recurrent laryngeal nerve palsy associated with mediastinal amyloidosis. Thorax 2000, 55, 436. [Google Scholar] [CrossRef]
- Batista, J.A.d.S.; Carrera, L.R.; Viriato, A.R.; Novaes, M.A.C.; de Morais, R.J.L.; Oliveira, F.T.; Marques, W.; Costa, M.C.M. Involvement of cranial nerves in ATTR Ile127Val amyloidosis. Eur. J. Med. Genet. 2022, 65, 104524. [Google Scholar] [CrossRef]
- Ruberg, F.L.; Grogan, M.; Hanna, M.; Kelly, J.W.; Maurer, M.S. Transthyretin Amyloid Cardiomyopathy: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2019, 73, 2872–2891. [Google Scholar] [CrossRef]
- See, A.S.Y.; Ho, J.S.-Y.; Chan, M.Y.; Lim, Y.C.; Yeo, T.-C.; Chai, P.; Wong, R.C.; Lin, W.; Sia, C.-H. Prevalence and Risk Factors of Cardiac Amyloidosis in Heart Failure: A Systematic Review and Meta-Analysis. Hear. Lung Circ. 2022, 31, 1450–1462. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ng, C.H.L.; Berry, G.J.; Damrose, E.J. ATTR Variant Amyloidosis in Patients with Dysphagia. Surgeries 2023, 4, 275-282. https://doi.org/10.3390/surgeries4020028
Ng CHL, Berry GJ, Damrose EJ. ATTR Variant Amyloidosis in Patients with Dysphagia. Surgeries. 2023; 4(2):275-282. https://doi.org/10.3390/surgeries4020028
Chicago/Turabian StyleNg, Christina Hui Lee, Gerald J. Berry, and Edward J. Damrose. 2023. "ATTR Variant Amyloidosis in Patients with Dysphagia" Surgeries 4, no. 2: 275-282. https://doi.org/10.3390/surgeries4020028
APA StyleNg, C. H. L., Berry, G. J., & Damrose, E. J. (2023). ATTR Variant Amyloidosis in Patients with Dysphagia. Surgeries, 4(2), 275-282. https://doi.org/10.3390/surgeries4020028





