Abstract
The field of anesthesia has always been at the forefront of innovation and technology, and the integration of Artificial Intelligence (AI) represents the next frontier in anesthesia care. The use of AI and its subtypes, such as machine learning, has the potential to improve efficiency, reduce costs, and ameliorate patient outcomes. AI can assist with decision making, but its primary advantage lies in empowering anesthesiologists to adopt a proactive approach to address clinical issues. The potential uses of AI in anesthesia can be schematically grouped into clinical decision support and pharmacologic and mechanical robotic applications. Tele-anesthesia includes strategies of telemedicine, as well as device networking, for improving logistics in the operating room, and augmented reality approaches for training and assistance. Despite the growing scientific interest, further research and validation are needed to fully understand the benefits and limitations of these applications in clinical practice. Moreover, the ethical implications of AI in anesthesia must also be considered to ensure that patient safety and privacy are not compromised. This paper aims to provide a comprehensive overview of AI in anesthesia, including its current and potential applications, and the ethical considerations that must be considered to ensure the safe and effective use of the technology.
1. Introduction
The field of anesthesia has always been at the forefront of innovation and technology [1]. From the introduction of ether in the mid-19th century to the development of modern anesthetic agents, anesthesia care has continuously evolved to improve patient outcomes [2]. As a result of technological progress, anesthesia has become increasingly safe, precise, and tailored to individual patient needs.
Artificial intelligence (AI) is an emerging technology that has the potential to revolutionize healthcare delivery [3]. AI refers to the development of computer systems that can perform tasks that would usually require human intelligence, such as learning, reasoning, problem solving, decision making, and perception. On the other hand, Machine Learning (ML) is a subset of AI that focuses on enabling machines to learn from data without being explicitly programmed. ML algorithms can analyze data, learn from it, and make predictions or decisions based on that learning. Deep learning is a subset of ML that involves training artificial neural networks with multiple layers to recognize patterns in data. It is used in image and speech recognition, natural language processing, and other applications. Other AI subsets are robotics, computer vision, and expert systems that are designed to mimic the decision-making abilities of a human expert in a particular domain [4].
The integration of AI and ML represents the next frontier in anesthesia care, with the potential to further improve efficiency, reduce costs, and enhance patient safety [4]. This technology is being increasingly used in various aspects of anesthesia care, including preoperative evaluation, intraoperative monitoring, and postoperative management. For example, predictive algorithms can be used to forecast patient responses to anesthesia, allowing clinicians to optimize dosing and minimize the risk of adverse events [5]. Automated systems can also monitor vital signs during surgery and alert clinicians when intervention is required [6]. Additionally, AI can be used to identify patient-specific risk factors for postoperative complications, enabling clinicians to take proactive steps to reduce complications [7].
Interestingly, in the field of anesthesiology, AI can also offer virtual simulations and training programs for enhancing the skills and knowledge of anesthesiologists. Multiple studies have demonstrated the efficacy of AI in assisting in the evaluation of trainee performance in anesthesia. For instance, interesting perspectives regard the application of AI techniques to increase learning efficiency in the field of ultrasound-guided regional anesthesia [8].
Despite these benefits, the use of AI in anesthesia also raises ethical concerns that must be carefully considered. These concerns are mostly related to privacy, transparency, and bias, although several issues should be necessarily addressed. For instance, there have been concerns raised regarding the possibility of AI being utilized to gather and retain patient data without explicit consent [9]. Furthermore, there exists a potential risk of bias within AI algorithms, which could disproportionately affect specific patient groups [10].
This paper provides an overview of AI in anesthesia, discusses the ethical implications of its use, and explores its current and potential clinical applications.
2. AI in Anesthesia
AI involves the development of algorithms that can learn and improve from data, for helping clinicians in the decision-making process. In anesthesia, AI algorithms can assist anesthesiologists in making clinical decisions in different contexts. However, the primary advantage of AI lies in empowering anesthesiologists to adopt a proactive approach to address clinical issues. For example, AI has been used for presurgical evaluation [11,12,13], to predict patient responses to anesthesia [14], to automate drug dosing [15], to monitor patients during surgery [6], and other purposes [16,17,18,19,20,21,22,23,24,25,26,27] (Table 1).

Table 1.
Potential applications of AI in anesthesia.
Although with limitations due to classification difficulties, the applications of AI in anesthesia can be schematically summarized into Clinical Decision Support System (CDSS) applications and pharmacological and mechanical robotic systems. Furthermore, tele-anesthesia includes strategies of telemedicine (preoperative assessment and post-operative monitoring), as well as device networking for improving logistics in the operating room and augmented reality approaches for training and assistance (Figure 1). AI can also be used to reduce costs by automating tasks that are currently performed by anesthesiologists.
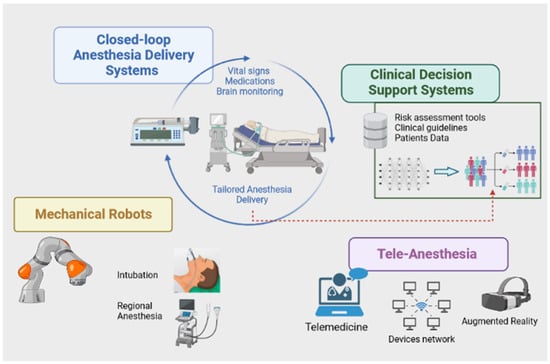
Figure 1.
Infographic of potential modalities for AI-based applications in anesthesia. AI-powered Clinical Decision Support Systems can help anesthesiologists in decision-making processes by analyzing patient data and providing real-time recommendations. Pharmacological robotic methods (closed-loop anesthesia delivery systems) can be used to deliver anesthesia, monitor vital signs, and adjust the dosage of medication as needed (tailored anesthesia delivery). Attempts with mechanical robots have been performed for intubation and nerve blocks. Tele-anesthesia includes strategies of telemedicine, such as preoperative assessment, postoperative monitoring, and remote consultations. This approach can help expand access to anesthesia services and improve patient outcomes, particularly in underserved areas. Created with BioRender.com (accessed on 18 April 2023).
Specifically, CDSS in anesthesia is a computer-based tool that assists anesthesia providers in making clinical decisions by providing real-time patient-specific recommendations and alerts based on patient data and medical knowledge. It can aid in the optimization of anesthesia care by offering automated recommendations on the dosing of anesthetic agents, fluid management, and other aspects of perioperative care. These systems can also help to identify potential drug interactions, allergies, and patient comorbidities that may impact the provision of anesthesia [28]. Predictive algorithms of CDSS can also be implemented to detect early signs of deterioration in different post-anesthesia scenarios [29]. Furthermore, artificial neural network systems have been employed to develop a predictive model for the duration of surgery and anesthesia emergence. This process aims to optimize anesthesia care and streamline the utilization of operating rooms [30].
Robotics represents an additional area where AI finds application within the field of anesthesia. A robot refers to a mechanical system that has the ability to engage with the environment through deliberate actions and interventions. Robotic systems in anesthesia can be grouped into pharmacological robots and mechanical robots. Pharmacological robots are devices that process continuously collected multiple clinical and biosignal data from hypnosis, analgesia, muscle relaxation, and other vital signs to ultimately predict the appropriate anesthesia dosage based on the patient’s individual needs [31]. This complex input–output process structures the so-called closed-loop anesthesia delivery system (CLAD). For example, the McSleepy intravenous sedation device was developed to automatically administer propofol, analgesics, and muscle relaxants [32].
Clinical experience with mechanical robots in anesthesia is limited. Some authors have proposed an intubation system using the Da Vinci surgical system or other approaches [33]. Interesting scenarios concern regional anesthesia, such as the Magellan robot used to perform peripheral nerve block [34]. Nevertheless, it seems that currently, robots lack the dexterity to perform these challenging anesthesia tasks.
AI-powered device networking can be used to improve logistics in the operating room by enabling seamless communication between anesthesia machines, patient monitors, and other medical devices. This can help streamline workflow, reduce errors, and improve patient safety. Augmented reality technology can be used for training and assistance in anesthesia. For example, it can provide real-time feedback during procedures, help train new anesthesiologists, and improve the accuracy of nerve blocks.
3. Ethical Implications
While the use of AI in anesthesia has the potential to improve patient outcomes, it also raises ethical concerns related to privacy, transparency, and other paramount issues (Table 2) [35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51]. Notably, these ethical issues can pose serious challenges in the development and implementation of AI translation systems [36].

Table 2.
Ethical issues of Artificial Intelligence in anesthesia.
Bias is a significant ethical concern related to AI in all medical fields. The accuracy and reliability of AI algorithms depend heavily on the quality and representativeness of the data used to train them. If the data used to train an AI model are biased in any way, the model will produce biased results. This can have severe consequences, leading to inaccurate diagnoses and treatment recommendations, particularly for underrepresented or historically marginalized patient populations. It could also perpetuate discrimination and exacerbate health disparities, resulting in unequal treatment of patients based on factors such as race, gender, and socioeconomic status [37]. Consequently, it is important to ensure that AI algorithms are developed and tested on diverse populations to reduce the risk of bias. In other words, data used to train AI algorithms must be diverse and representative of the populations that the algorithm will be used to serve [38,39]. Additionally, it is crucial to continually monitor and evaluate AI systems to detect and mitigate any bias that may arise over time. This can involve ongoing data collection, algorithm retraining, and regular audits of AI systems to ensure that they are performing fairly and equitably for all patients.
To address ethical concerns, governments must play a critical role in the regulatory process [40]. They must establish regulatory frameworks that outline the legal requirements for the use of AI in medical applications. These frameworks must also set up technical standards that ensure the accuracy, reliability, and safety of AI systems, as well as guidelines for the ethical use of AI. Nevertheless, the development of ethical frameworks for AI in medicine requires a collaborative effort among various stakeholders to ensure that AI systems meet the highest standards of data protection and ethical considerations. Other stakeholders, such as healthcare providers, industry, patients, ethics experts, and standards organizations, should also be involved in the development and implementation of ethical frameworks for AI in medicine. Healthcare providers, for example, can provide valuable insights into the practical application of AI in the medical field, while patients can provide input on their preferences and concerns regarding the use of AI in their healthcare. Moreover, ethics experts and standards organizations can provide guidance on the ethical principles and values that should guide the development and use of AI in medicine, while industry representatives can provide expertise on the technical capabilities and limitations of AI systems.
One of the most pressing concerns in AI is the potential for sensitive patient data to be exposed or compromised, leading to breaches of privacy and confidentiality [41]. This can occur through various means, such as hacking, theft, or unintentional disclosure by employees. Such breaches can have severe consequences, including financial losses, damage to reputation, and even harm to patients. Therefore, it is crucial to establish robust security protocols to prevent such breaches from occurring. This involves implementing measures such as encryption, access controls, and regular system updates to protect against cyber threats. It is also important to provide staff training on data protection and maintain strict compliance with relevant regulations, such as the Health Insurance Portability and Accountability Act (HIPAA). It is a federal law in the United States that mandates the establishment of national standards to safeguard confidential patient health information, ensuring it is not revealed without explicit consent or awareness of the patient [42]. In addition to these measures, ensuring the highest standards of data protection requires a comprehensive approach that encompasses both technical and organizational aspects. This involves identifying and assessing potential risks, developing policies and procedures to address them, and regularly reviewing and updating these measures to ensure their effectiveness.
A special issue is represented by biobanks and clinical–biological integration repositories. These biorepositories collect, store, and distribute biological specimens and associated data for use in research, especially in the field of precision medicine. Specimens can include human tissue, blood, urine, DNA, and other biomolecules. Several biobanks aggregate data from a substantial number of patients. For example, the United Kingdom Biobank is one of the largest and most well-known biobanks, housing extensive health and genetic data from over 500,000 participants [43]. The Framingham Heart Study was developed for identifying risk factors for cardiovascular diseases. It has collected data and biological samples from multiple generations of participants since 1948 [44]. Moreover, the Cancer Genome Atlas is a biobank focused on cancer research. This repository contains genomic data, including DNA sequencing results, from thousands of cancer patients, helping researchers identify genetic alterations and potential therapeutic targets [45]. Overall, biobanks are valuable resources for researchers studying genetics, diseases, and drug development, among other areas of research. They may operate under strict ethical guidelines and protocols to ensure the privacy and confidentiality of the individuals whose specimens are being stored, and to ensure that the use of the specimens is for research purposes that are in the public interest. Obviously, many efforts must be made from a taxonomic and methodological point of view to allow for the data. In addition, the data protection policy will have to comply with uniform international standards [46].
To increase the credibility of AI-based systems, it is essential to establish predictive error rates and ensure transparency and explainability of AI algorithms [47]. Model explainability refers to the ability of AI and machine learning models to provide clear and interpretable explanations of their decision-making process. Techniques such as decision trees, rule-based systems, SHapley Additive exPlanations (SHAP), local interpretable model-agnostic explanations (LIME), heat maps, and saliency maps can be used to achieve model explainability, allowing users to gain insights, trust, and transparency in the decision-making process of AI systems [48].
It is important to ensure that AI systems are developed and implemented in a way that promotes equitable access to healthcare, including addressing issues of cost and training. AI systems can require expensive hardware and software, as well as specialized training and expertise, which may not be available to all healthcare providers, particularly in low-resource settings. This can result in unequal access to AI-powered healthcare solutions, limiting their potential to improve healthcare outcomes and exacerbating existing disparities [49].
Finally, ethicists should be involved in AI projects from the beginning to ensure that ethical considerations are integrated into the development and implementation of AI systems [50]. This step is crucial for addressing concerns proactively. Therefore, it is important to showcase how AI can help healthcare professionals to augment their capabilities and improve patient outcomes [51].
Scientific Output, Ongoing Research, and Perspectives
Research on AI in anesthesia is rapidly developing [52]. A recent bibliometric analysis evaluated the scientific output of the argument [53]. The analysis found that, regarding the topics being studied, researchers are primarily focused on anesthesia management. They are currently exploring the use of automatic anesthetic administration, also known as closed-loop anesthesia [54]. Other areas of interest include postoperative complications, such as postoperative delirium [55], perioperative transfusion medicine, and predicting the risk of bleeding [56]. Additionally, researchers are investigating models that can accurately estimate the depth of anesthesia [57] and emergence timing [30,58], and can be useful to predict difficult endotracheal intubation [59] and perioperative hypotension [60]. These research areas demonstrate that the primary objective of studying AI in anesthesia is to improve clinical management by accurately predicting potential complications and suggesting optimal therapeutic strategies in real time [61]. Interestingly, the anesthesia process is also a topic of interest. For instance, some researchers, such as Lee et al. [62], have applied deep learning processes to develop a metric called the explainable consciousness indicator. This metric simultaneously calculates two aspects of consciousness: arousal and awareness. Nevertheless, several research gaps need to be filled. For example, a recent editorial has pointed out a significant difference in the number of AI-related articles published in technical journals compared to medical journals [63]. This emphasizes that the translation of AI research into clinical practice continues to encounter numerous challenges [64].
The utilization of AI in anesthesia has sparked significant interest, as evidenced by the numerous ongoing studies. These investigations hold considerable potential for the future of AI in this medical domain and its capacity to enhance patient care.
French researchers are utilizing a natural language processing approach to categorize adverse events that occur during the perioperative period and streamline their analysis, according to a study (ClinicalTrials.gov Identifier: NCT05185479). The development of a predictive model that uses AI techniques is the main objective of the PINES project. This model will accurately forecast the actions of neuromuscular blocking agents, enabling the prediction of the time required to achieve complete neuromuscular recovery (train-of-four [TOF] ratio >0.95). Ultimately, this model may serve as a decision support tool for healthcare providers in the management of neuromuscular blocking drug timing and dosing, as well as the administration of their reversal agents (NCT05471882). A research project is being conducted to explore a new CDSS application in anesthesiology. This application incorporates risk assessment tools and clinical guidelines, guided by AI, in the preoperative assessment process. The study aims to compare the effectiveness of this new approach with the current standard preoperative assessment workflow by conducting research on actual patients. A total of 480 participants will be randomly assigned to either the CDSS group (preoperative assessment using the CDSS application) or the Control group (standard preoperative assessment workflow) (NCT05284227). Finally, a multicenter, prospective, observational study is being conducted under the University of Oxford’s guidance to evaluate ultrasound image analysis in ultrasound-guided regional anesthesia. The study compares the accuracy of anatomical structure identification on ultrasound images between human experts and an AI device (ScanNav Anatomy PNB) (NCT04983771).
While these are just a few examples, the findings of these studies will provide crucial evidence for better defining the potential applications of AI in anesthesia. Furthermore, these results will aid in the design of increasingly rigorous studies, ultimately advancing our understanding of this promising field.
The prospects for the development of AI applied to anesthesia are truly very interesting [65]. They include the optimization of the anesthesia workplace and the development of functionally interconnected systems in the operating room (Internet of Things), managed with AI apps and smartphones for improving logistics. For example, monitors, lights, and other devices can be connected to various AI systems. The design of tele-anesthesia approaches, by combining telemedicine and wearable healthcare technologies for preoperative evaluation and postoperative monitoring, is a fascinating prospect, especially since tele-anesthesia can be combined with augmented reality (AR) approaches for assistance and training purposes. In particular, AR seamlessly integrates computer-generated information into the real-world environment, creating a truly immersive and enhanced experience for users. Recent advancements in both hardware and software have made AR more affordable and user-friendly. In the realm of perioperative medicine, AR could play a significant role, particularly in the precise identification of anatomical structures for procedures such as regional blocks and vascular access. Moreover, AR has proven to be a valuable tool in pediatric care, effectively reducing anxiety among young patients during procedures. Other potential applications of AR in anesthesia are training and education, real-time monitoring and feedback, and preoperative planning [66].
Concerning simulation and training, AI can be used to develop sophisticated anesthesia simulators and virtual training environments. These systems can provide realistic scenarios for trainees to practice their skills, make clinical decisions, and gain experience in managing various anesthesia situations. For example, AI-guided solutions have the potential to enhance the entire training process in ultrasound-guided regional anesthesia (UGRA). A recent scoping review discovered that these strategies could enhance various aspects, such as optimizing and interpreting sonographic images, visualizing needle advancement, and facilitating local anesthetic injection. However, despite notable advancements in the implementation of AI-guided UGRA, the absence of randomized control trials remains a notable gap [67].
4. Conclusions
AI is an emerging technology with the potential to revolutionize anesthesia care and improve patient outcomes. However, its use also raises ethical concerns related to privacy, transparency, and bias. The responsible development and use of AI in anesthesia require collaboration between healthcare providers, technology developers, and patients to ensure that the technology is used in a way that prioritizes patient safety, privacy, and equity. Furthermore, it is important to ensure that AI algorithms are developed and tested on diverse populations and that patients have control over their data. Finally, as AI continues to progress, anesthesiologists must carefully navigate the integration of AI into clinical practice, considering both the safety and ethical dimensions. By fostering an environment of responsible AI implementation, the field of anesthesia can harness the full potential of this technology while upholding the highest standards of patient care and societal values.
Author Contributions
Conceptualization, M.C. and E.G.B.; methodology, M.C.T.; investigation, M.C. and E.P.; resources, M.C.; data curation, M.C.T. and E.P.; writing—original draft preparation, M.C.; writing—review and editing, M.C. and E.P.; visualization, M.C.T.; supervision, M.C.; project administration, M.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The authors acknowledge the contribution of Muzio Maria Rosaria in designing the tables of this manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Moon, J.S.; Cannesson, M. A Century of Technology in Anesthesia & Analgesia. Anesth. Analg. 2022, 135 (Suppl. S2), S48–S61. [Google Scholar] [CrossRef]
- Petermann, H.; Böhrer, H.; Witte, W. Von der Äthernarkose zur “grünen” Anästhesie: Herausforderungen in der Anästhesiologie der letzten 175 Jahre [From ether anesthesia to “green” anesthesia: Challenges in anesthesiology over the last 175 years]. Anaesthesist 2021, 70, 832–842. [Google Scholar] [CrossRef]
- Stanfill, M.H.; Marc, D.T. Health Information Management: Implications of Artificial Intelligence on Healthcare Data and Information Management. Yearb. Med. Inform. 2019, 28, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Bellini, V.; Valente, M.; Gaddi, A.V.; Pelosi, P.; Bignami, E. Artificial intelligence and telemedicine in anesthesia: Potential and problems. Minerva Anestesiol. 2022, 88, 729–734. [Google Scholar] [CrossRef] [PubMed]
- Bihorac, A.; Ozrazgat-Baslanti, T.; Ebadi, A.; Motaei, A.; Madkour, M.; Pardalos, P.M.; Lipori, G.; Hogan, W.R.; Efron, P.A.; Moore, F.; et al. MySurgeryRisk: Development and Validation of a Machine-learning Risk Algorithm for Major Complications and Death After Surgery. Ann. Surg. 2019, 269, 652–662. [Google Scholar] [CrossRef]
- Lee, H.C.; Ryu, H.G.; Chung, E.J.; Jung, C.W. Prediction of Bispectral Index during Target-controlled Infusion of Propofol and Remifentanil: A Deep Learning Approach. Anesthesiology 2018, 128, 492–501. [Google Scholar] [CrossRef]
- Hofer, I.S.; Lee, C.; Gabel, E.; Baldi, P.; Cannesson, M. Development and validation of a deep neural network model to predict postoperative mortality, acute kidney injury, and reintubation using a single feature set. NPJ Digit. Med. 2020, 3, 58. [Google Scholar] [CrossRef]
- Hewson, D.W.; Bedforth, N.M. Closing the gap: Artificial intelligence applied to ultrasound-guided regional anaesthesia. Br. J. Anaesth. 2023, 130, 245–247. [Google Scholar] [CrossRef]
- Kovarik, C.L.; Sanabria, B.; Stoff, B.K. Image Consent and the Development of Image-Based Artificial Intelligence. JAMA Dermatol. 2022, 158, 589. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.; Hu, J. Bias in Artificial Intelligence: Basic Primer. Clin. J. Am. Soc. Nephrol. 2023, 18, 394–396. [Google Scholar] [CrossRef] [PubMed]
- Solanki, S.L.; Pandrowala, S.; Nayak, A.; Bhandare, M.; Ambulkar, R.P.; Shrikhande, S.V. Artificial intelligence in perioperative management of major gastrointestinal surgeries. World J. Gastroenterol. 2021, 27, 2758–2770. [Google Scholar] [CrossRef]
- Li, Y.Y.; Wang, J.J.; Huang, S.H.; Kuo, C.L.; Chen, J.Y.; Liu, C.F.; Chu, C.C. Implementation of a machine learning application in preoperative risk assessment for hip repair surgery. BMC Anesthesiol. 2022, 22, 116. [Google Scholar] [CrossRef] [PubMed]
- Chiew, C.J.; Liu, N.; Wong, T.H.; Sim, Y.E.; Abdullah, H.R. Utilizing Machine Learning Methods for Preoperative Prediction of Postsurgical Mortality and Intensive Care Unit Admission. Ann. Surg. 2020, 272, 1133–1139. [Google Scholar] [CrossRef] [PubMed]
- Corey, K.M.; Kashyap, S.; Lorenzi, E.; Lagoo-Deenadayalan, S.A.; Heller, K.; Whalen, K.; Balu, S.; Heflin, M.T.; McDonald, S.R.; Swaminathan, M.; et al. Development and validation of machine learning models to identify high-risk surgical patients using automatically curated electronic health record data (Pythia): A retrospective, single-site study. PLoS Med. 2018, 15, e1002701. [Google Scholar] [CrossRef]
- Neckebroek, M.; Ionescu, C.M.; van Amsterdam, K.; De Smet, T.; De Baets, P.; Decruyenaere, J.; De Keyser, R.; Struys, M.M.R.F. A comparison of propofol-to-BIS post-operative intensive care sedation by means of target controlled infusion, Bayesian-based and predictive control methods: An observational, open-label pilot study. J. Clin. Monit. Comput. 2019, 33, 675–686. [Google Scholar] [CrossRef]
- Härkänen, M.; Haatainen, K.; Vehviläinen-Julkunen, K.; Miettinen, M. Artificial Intelligence for Identifying the Prevention of Medication Incidents Causing Serious or Moderate Harm: An Analysis Using Incident Reporters’ Views. Int. J. Environ. Res. Public Health 2021, 18, 9206. [Google Scholar] [CrossRef] [PubMed]
- Syrowatka, A.; Song, W.; Amato, M.G.; Foer, D.; Edrees, H.; Co, Z.; Kuznetsova, M.; Dulgarian, S.; Seger, D.L.; Simona, A.; et al. Key use cases for artificial intelligence to reduce the frequency of adverse drug events: A scoping review. Lancet Digit. Health 2022, 4, e137–e148. [Google Scholar] [CrossRef]
- Hashimoto, D.A.; Witkowski, E.; Gao, L.; Meireles, O.; Rosman, G. Artificial Intelligence in Anesthesiology: Current Techniques, Clinical Applications, and Limitations. Anesthesiology 2020, 132, 379–394. [Google Scholar] [CrossRef]
- Nagireddi, J.N.; Vyas, A.K.; Sanapati, M.R.; Soin, A.; Manchikanti, L. The Analysis of Pain Research through the Lens of Artificial Intelligence and Machine Learning. Pain Physician 2022, 25, E211–E243. [Google Scholar]
- Cascella, M.; Montomoli, J.; Bellini, V.; Bignami, E.G. Integrating data science and neural architecture techniques for automatic pain assessment in critically ill patients. Anaesth. Crit. Care Pain Med. 2023, 42, 101220. [Google Scholar] [CrossRef]
- Cobianchi, L.; Piccolo, D.; Dal Mas, F.; Agnoletti, V.; Ansaloni, L.; Balch, J.; Biffl, W.; Butturini, G.; Catena, F.; Coccolini, F.; et al. Surgeons’ perspectives on artificial intelligence to support clinical decision-making in trauma and emergency contexts: Results from an international survey. World J. Emerg. Surg. 2023, 18, 1. [Google Scholar] [CrossRef] [PubMed]
- McCoy, A.; Das, R. Reducing patient mortality, length of stay and readmissions through machine learning-based sepsis prediction in the emergency department, intensive care unit and hospital floor units. BMJ Open Qual. 2017, 6, e000158. [Google Scholar] [CrossRef]
- Loftus, T.J.; Vlaar, A.P.J.; Hung, A.J.; Bihorac, A.; Dennis, B.M.; Juillard, C.; Hashimoto, D.A.; Kaafarani, H.M.A.; Tighe, P.J.; Kuo, P.C.; et al. Executive summary of the artificial intelligence in surgery series. Surgery 2022, 171, 1435–1439. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, S.; Chat, G.P. Open artificial intelligence platforms in nursing education: Tools for academic progress or abuse? Nurse Educ. Pract. 2023, 66, 103537. [Google Scholar] [CrossRef] [PubMed]
- Cascella, M.; Montomoli, J.; Bellini, V.; Bignami, E. Evaluating the Feasibility of ChatGPT in Healthcare: An Analysis of Multiple Clinical and Research Scenarios. J. Med. Syst. 2023, 47, 33. [Google Scholar] [CrossRef] [PubMed]
- Bellini, V.; Cascella, M.; Cutugno, F.; Russo, M.; Lanza, R.; Compagnone, C.; Bignami, E.G. Understanding basic principles of Artificial Intelligence: A practical guide for intensivists. Acta Biomed. 2022, 93, e2022297. [Google Scholar] [CrossRef]
- Hassan, A.M.; Rajesh, A.; Asaad, M.; Nelson, J.A.; Coert, J.H.; Mehrara, B.J.; Butler, C.E. A Surgeon’s Guide to Artificial Intelligence-Driven Predictive Models. Am. Surg. 2023, 89, 11–19. [Google Scholar] [CrossRef]
- Freundlich, R.E.; Ehrenfeld, J.M. Anesthesia information management: Clinical decision support. Curr. Opin. Anaesthesiol. 2017, 30, 705–709. [Google Scholar] [CrossRef] [PubMed]
- Olsen, R.M.; Aasvang, E.K.; Meyhoff, C.S.; Dissing Sorensen, H.B. Towards an automated multimodal clinical decision support system at the post anesthesia care unit. Comput. Biol. Med. 2018, 101, 15–21. [Google Scholar] [CrossRef]
- Huang, L.; Chen, X.; Liu, W.; Shih, P.C.; Bao, J. Automatic Surgery and Anesthesia Emergence Duration Prediction Using Artificial Neural Networks. J. Healthc. Eng. 2022, 2022, 2921775. [Google Scholar] [CrossRef] [PubMed]
- Wingert, T.; Lee, C.; Cannesson, M. Machine Learning, Deep Learning, and Closed Loop Devices-Anesthesia Delivery. Anesthesiol. Clin. 2021, 39, 565–581. [Google Scholar] [CrossRef] [PubMed]
- Wehbe, M.; Arbeid, E.; Cyr, S.; Mathieu, P.A.; Taddei, R.; Morse, J.; Hemmerling, T.M. A technical description of a novel pharmacological anesthesia robot. J. Clin. Monit. Comput. 2014, 28, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Hemmerling, T.M.; Wehbe, M.; Zaouter, C.; Taddei, R.; Morse, J. The Kepler intubation system. Anesth. Analg. 2012, 114, 590–594. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, B.D.; O’Sullivan, O.; Gal-lagher, A.G.; Shorten, G.D. Robotic assistance with needle guidance. Br. J. Anaesth. 2015, 114, 708–709. [Google Scholar] [CrossRef]
- Cobianchi, L.; Verde, J.M.; Loftus, T.J.; Piccolo, D.; Dal Mas, F.; Mascagni, P.; Garcia Vazquez, A.; Ansaloni, L.; Marseglia, G.R.; Massaro, M.; et al. Artificial Intelligence and Surgery: Ethical Dilemmas and Open Issues. J. Am. Coll. Surg. 2022, 235, 268–275. [Google Scholar] [CrossRef]
- Cascella, M.; Montomoli, J.; Bellini, V.; Vittori, A.; Biancuzzi, H.; Dal Mas, F.; Bignami, E.G. Crossing the AI Chasm in Neurocritical Care. Computers 2023, 12, 83. [Google Scholar] [CrossRef]
- Panch, T.; Mattie, H.; Atun, R. Artificial intelligence and algorithmic bias: Implications for health systems. J. Glob. Health 2019, 9, 010318. [Google Scholar] [CrossRef]
- Bellini, V.; Petroni, A.; Palumbo, G.; Bignami, E. Data quality and blockchain technology. Anaesth. Crit. Care Pain Med. 2019, 38, 521–522. [Google Scholar] [CrossRef]
- Raimundo, R.; Rosário, A. The Impact of Artificial Intelligence on Data System Security: A Literature Review. Sensors 2021, 21, 7029. [Google Scholar] [CrossRef]
- Harvey, H.B.; Gowda, V. Regulatory Issues and Challenges to Artificial Intelligence Adoption. Radiol. Clin. N. Am. 2021, 59, 1075–1083. [Google Scholar] [CrossRef]
- Nifakos, S.; Chandramouli, K.; Nikolaou, C.K.; Papachristou, P.; Koch, S.; Panaousis, E.; Bonacina, S. Influence of Human Factors on Cyber Security within Healthcare Organisations: A Systematic Review. Sensors 2021, 21, 5119. [Google Scholar] [CrossRef] [PubMed]
- Health Insurance Portability and Accountability Act of 1996 (HIPAA). Available online: https://www.cdc.gov/phlp/publications/topic/hipaa.html (accessed on 20 April 2023).
- Conroy, M.C.; Lacey, B.; Bešević, J.; Omiyale, W.; Feng, Q.; Effingham, M.; Sellers, J.; Sheard, S.; Pancholi, M.; Gregory, G.; et al. UK Biobank: A globally important resource for cancer research. Br. J. Cancer 2023, 128, 519–527. [Google Scholar] [CrossRef]
- Andersson, C.; Johnson, A.D.; Benjamin, E.J.; Levy, D.; Vasan, R.S. 70-year legacy of the Framingham Heart Study. Nat. Rev. Cardiol. 2019, 16, 687–698. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Luo, D.; Zhong, N.; Li, D.; Zheng, J.; Liao, H.; Li, Z.; Lin, X.; Chen, Q.; Zhang, C.; et al. GPC2 Is a Potential Diagnostic, Immunological, and Prognostic Biomarker in Pan-Cancer. Front. Immunol. 2022, 13, 857308. [Google Scholar] [CrossRef] [PubMed]
- Coppola, L.; Cianflone, A.; Grimaldi, A.M.; Incoronato, M.; Bevilacqua, P.; Messina, F.; Baselice, S.; Soricelli, A.; Mirabelli, P.; Salvatore, M. Biobanking in health care: Evolution and future directions. J. Transl. Med. 2019, 17, 172. [Google Scholar] [CrossRef]
- Amann, J.; Blasimme, A.; Vayena, E.; Frey, D.; Madai, V.I.; Precise4Q Consortium. Explainability for artificial intelligence in healthcare: A multidisciplinary perspective. BMC Med. Inform. Decis. Mak. 2020, 20, 310. [Google Scholar] [CrossRef]
- Arbelaez Ossa, L.; Starke, G.; Lorenzini, G.; Vogt, J.E.; Shaw, D.M.; Elger, B.S. Re-focusing explainability in medicine. Digit. Health 2022, 8, 1074488. [Google Scholar] [CrossRef] [PubMed]
- Koski, E.; Murphy, J. AI in Healthcare. Stud. Health Technol. Inform. 2021, 284, 295–299. [Google Scholar] [CrossRef]
- Banja, J. How Might Artificial Intelligence Applications Impact Risk Management? AMA J. Ethics. 2020, 22, E945–E951. [Google Scholar] [CrossRef]
- Keskinbora, K.H. Medical ethics considerations on artificial intelligence. J. Clin. Neurosci. 2019, 64, 277–282. [Google Scholar] [CrossRef]
- Alexander, J.C.; Romito, B.T.; Çobanoğlu, M.C. The present and future role of artificial intelli-gence and machine learning in anesthesiology. Int. Anesthesiol. Clin. 2020, 58, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Cascella, M.; Perri, F.; Ottaiano, A.; Cuomo, A.; Wirz, S.; Coluccia, S. Trends in Research on Artificial Intelligence in Anesthesia: A VOSviewer-Based Biblio-metric Analysis. Intel. Artificial. 2022, 25, 126–137. [Google Scholar] [CrossRef]
- Miyaguchi, N.; Takeuchi, K.; Kashima, H.; Morita, M.; Morimatsu, H. Predicting anesthetic infusion events using machine learning. Sci. Rep. 2021, 11, 23648. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.; You, J.; Peng, Y.; Feng, Y. Machine Learning Algorithm Using Electronic Chart-Derived Data to Predict Delirium after Elderly Hip Fracture Surgeries: A Retrospective Case-Control Study. Front. Surg. 2021, 8, 634629. [Google Scholar] [CrossRef]
- Walczak, S.; Velanovich, V. Prediction of perioperative transfusions using an artificial neural network. PLoS ONE 2020, 15, e0229450. [Google Scholar] [CrossRef]
- Afshar, S.; Boostani, R.; Sanei, S. A Combinatorial Deep Learning Structure for Precise Depth of Anesthesia Estimation from EEG Signals. IEEE J. Biomed. Health Inform. 2021, 25, 3408–3415. [Google Scholar] [CrossRef] [PubMed]
- Cascella, M.; Bimonte, S.; Di Napoli, R. Delayed Emergence from Anesthesia: What We Know and How We Act. Local Reg. Anesth. 2020, 13, 195–206. [Google Scholar] [CrossRef]
- Cuendet, G.L.; Schoettker, P.; Yüce, A.; Sorci, M.; Gao, H.; Perruchoud, C.; Thiran, J.-P. Facial Image Analysis for Fully Automatic Prediction of Difficult Endotracheal Intubation. IEEE Trans. Biomed. Eng. 2016, 63, 328–339. [Google Scholar] [CrossRef]
- Joosten, A.; Alexander, B.; Duranteau, J.; Taccone, F.S.; Creteur, J.; Vincent, J.L.; Cannesson, M.; Rinehart, J. Feasibility of closed-loop titration of norepinephrine infusion in patients undergoing moderate- and high-risk surgery. Br. J. Anaesth 2019, 123, 430–438. [Google Scholar] [CrossRef]
- Connor, C.W. Artificial Intelligence and Machine Learning in Anesthesiology. Anesthesiology 2019, 131, 1346–1359. [Google Scholar] [CrossRef]
- Lee, M.; Sanz, L.R.D.; Barra, A.; Wolff, A.; Nieminen, J.O.; Boly, M.; Rosanova, M.; Casarotto, S.; Bodart, O.; Annen, J.; et al. Quantifying arousal and awareness in altered states of consciousness using interpretable deep learning. Nat. Commun. 2022, 13, 1064. [Google Scholar] [CrossRef] [PubMed]
- Lonsdale, H.; Jalali, A.; Gálvez, J.A.; Ahumada, L.M.; Simpao, A.F. Artificial Intelligence in Anesthesiology: Hype, Hope, and Hurdles. Anesth. Analg. 2020, 130, 1111–1113. [Google Scholar] [CrossRef] [PubMed]
- Singh, M.; Nath, G. Artificial intelligence and anesthesia: A narrative review. Saudi. J. Anaesth. 2022, 16, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Stradolini, F.; Tuoheti, A.; Kilic, T.; Ntella, S.L.; Tamburrano, N.; Huang, Z.; De Micheli, G.; Demarchi, D.; Carrara, S. An IoT Solution for Online Monitoring of Anesthetics in Human Serum Based on an Integrated Fluidic Bioelectronic System. IEEE Trans. Biomed. Circuits Syst. 2018, 12, 1056–1064. [Google Scholar] [CrossRef]
- Privorotskiy, A.; Garcia, V.A.; Babbitt, L.E.; Choi, J.E.; Cata, J.P. Augmented reality in anesthesia, pain medicine and critical care: A narrative review. J. Clin. Monit. Comput. 2022, 36, 33–39. [Google Scholar] [CrossRef]
- Viderman, D.; Dossov, M.; Seitenov, S.; Lee, M.H. Artificial intelligence in ultrasound-guided regional anesthesia: A scoping review. Front. Med. 2022, 9, 994805. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).