Abstract
Introduction: Anterior Cruciate Ligament (ACL) injuries are a major concern in orthopedics, particularly affecting active individuals and often necessitating surgery. The incidence of ACL injuries is rising, especially in women, comprising half of knee joint injuries. These injuries, common in sports with pivoting actions, can lead to long-term joint issues like osteoarthritis. Advances in surgical methods and understanding of postoperative recovery are crucial for improving patient outcomes, with considerations for graft size, material, and reconstruction technique critical in the rehabilitation process. Material and Methods: A systematic review was conducted by searching PubMed, MEDLINE, and SCOPUS for studies from 2009 to 10 February 2024, focusing on “six-strand hamstring graft” outcomes in ACL reconstruction. Inclusion criteria were English publications on 6HS autografts’ biomechanical and clinical outcomes. Excluded were non-specific, BTB, or hybrid studies, and non-research articles. Out of 347 records, 9 were analyzed after rigorous screening and quality assessment. This review, emphasizing six-strand hamstring autografts, enriches orthopedic knowledge, particularly for ACL surgery. Results: This review evaluated studies on six-strand hamstring (6HS) autografts for ACL reconstruction, encompassing prospective, retrospective, and cadaveric studies with subjects ranging from 12 to 413. Findings indicate that 6HS autografts enhance knee stability and increase graft diameter, correlating with reduced graft failure rates and improved clinical outcomes, including high patient satisfaction and low re-injury rates. Rehabilitation varied, with recovery times quicker due to larger graft sizes, and most studies reported low complication rates, underscoring 6HS autografts’ efficacy in ACL surgery. Conclusions: Performing 6HS autografts in ACL reconstruction reveals that they offer improved knee stability and graft diameter, leading to better clinical outcomes. These autografts are associated with high patient satisfaction and low re-injury rates, suggesting their effectiveness in mimicking native ACL function and enhancing rehabilitation. However, research limitations highlight the need for further long-term, comprehensive studies.
1. Introduction
Anterior Cruciate Ligament (ACL) injuries represent a significant concern in orthopedic medicine, primarily affecting a young, active demographic, often leading to surgical intervention [1]. The complexity of ACL injuries and the varied outcomes of surgical interventions necessitate a comprehensive understanding of postoperative recovery [2,3,4]. This understanding is pivotal for guiding patient expectations, improving rehabilitation protocols, and enhancing surgical techniques. ACL injuries, which frequently occur in sports involving pivoting movements such as football, basketball, and skiing, not only disrupt an individual’s athletic and personal life but also pose a risk for long-term joint health, potentially leading to osteoarthritis [5].
The history of ACL arthroscopic reconstruction dates back over 30 years [6,7]. Semitendinosus/gracilis tendon, bone–patellar tendon–bone grafts are the preferred graft materials for primary ACL reconstruction [8]. Bone–patellar tendon–bone graft is one of the best graft choices because it allows bone-to-bone healing, leading to a faster return to function and sports activity [9], in particular in professional athletes with ACL injuries, even if a potential patellar fracture can occur, making it unsuitable for double-bundle reconstruction and anterior kneeling pain [9].
The decision to undergo anterior cruciate ligament reconstruction is often motivated by factors such as the patient’s age, activity level, and the degree of knee instability [10]. Despite the advancements in surgical techniques and postoperative care, the journey to full recovery remains a complex and multifaceted process, influenced by various biological, physiological, and psychological factors [11,12].
Graft size in ACL reconstruction plays a pivotal role in the biomechanical stability of the knee post-surgery. A larger graft diameter has been associated with better outcomes in terms of knee stability and lower rates of graft failure [13,14]. Studies suggest that grafts with a diameter of at least 8 mm are associated with a reduced risk of revision surgery compared to smaller grafts [15]. This is because larger grafts more closely mimic the native ACL’s size and strength, providing better resistance to the forces exerted on the knee during physical activities [16]. However, there is a balance to be struck, as excessively large grafts can lead to tunnel widening and may not fit properly in smaller patients, potentially leading to complications. Therefore, the choice of graft size should be tailored to the individual, considering factors such as the patient’s size, activity level, and the size of their native ACL [17].
The number of strands in the graft also influences the outcome of ACL reconstruction. Double-bundle techniques, which use two grafts to replicate the native ACL’s anatomy more accurately, have been shown to provide better rotational stability compared to single-bundle techniques [18]. This is particularly important in sports that involve a lot of pivoting and changing direction, as it may help to better prevent re-injury. However, the increased complexity of double-bundle techniques may lead to longer surgical times and a more challenging rehabilitation process. Some studies have found no significant difference in outcomes between single- and double-bundle techniques in the general population, suggesting that the choice should be based on the specific needs and goals of the patient, as well as the surgeon’s expertise [19].
The purpose of this literature review is to evaluate the biomechanical and clinical outcomes of six-strand hamstring (6HS) autografts in ACL reconstruction, aiming to provide insights into their effectiveness and application in clinical settings.
2. Materials and Methods
Protocol Design: For this systematic review, we followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [20] (Prospero ID no. 544405).
2.1. Search Strategy
This systematic review followed PRISMA guidelines. Two independent reviewers (O.A.V. and N.A.V.) will execute a comprehensive literature search in PubMed, MEDLINE, and SCOPUS databases, including publications from 2009 up to 10 February 2024. The search strategy will utilize specific keywords and phrases such as “six-strand hamstring graft” and “6-strand hamstring graft” to ensure the inclusion of relevant studies. This search will be complemented by manual searches of the reference lists of included studies and review articles to identify any additional studies not captured in the database searches.
2.2. Inclusion and Exclusion Criteria
Studies will be included based on the following criteria: (1) written in English, (2) reporting on the biomechanical strength and properties of 6HS autografts, (3) discussing clinical outcomes following primary ACL reconstruction using 6HS autografts.
Exclusion criteria will include: (1) studies not reporting specific clinical or biomechanical outcomes of 6HS autografts, (2) use of Bone–Tendon–Bone (BTB) grafts or hybrid autografts–allografts, (3) systematic reviews, meta-analyses, editorial letters, commentaries, and conference abstracts.
2.3. Study Selection
After removing duplicates, titles and abstracts of the retrieved studies will be screened for eligibility. The full texts of potentially eligible studies will be reviewed for final inclusion. Any discrepancies between reviewers at any stage of the study selection process will be resolved through discussion or by consulting a third reviewer if necessary.
2.4. Data Extraction and Quality Assessment
Data on study characteristics, participant demographics, details of the 6HS autograft technique, biomechanical outcomes, clinical outcomes, and follow-up duration will be extracted for each included study. The methodological quality of the included studies will be assessed using suitable quality assessment tools, such as the Newcastle–Ottawa Scale for cohort studies or the Cochrane Collaboration’s tool for randomized trials, as applicable.
2.5. Data Synthesis and Analysis
Given the anticipated heterogeneity in study designs, outcomes, and measurements, a narrative synthesis will be conducted. This review will include summaries of biomechanical properties, clinical efficacy, rehabilitation protocols, and any reported complications or re-injury rates. Meta-analytical techniques will be applied where feasible to aggregate data and provide a quantitative summary of outcomes, employing random-effects models to accommodate between-study variability.
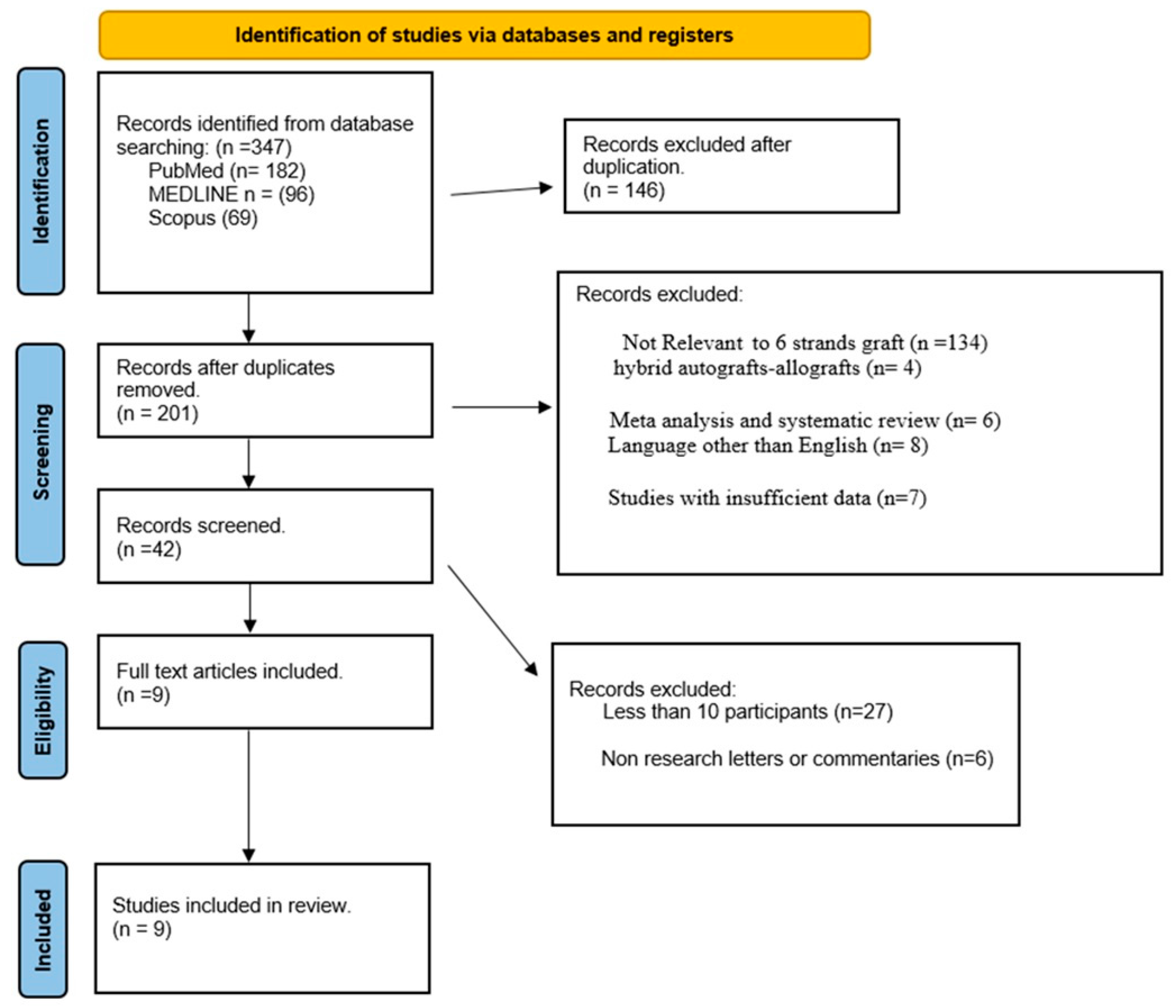
A comprehensive database search yielded 347 records, which, after removing 146 duplicates, left 201 for evaluation. Subsequent screening excluded records based on relevance, type, language, and data sufficiency, reducing the number to 42. Further exclusions for participant numbers and document type led to the final selection of 9 full-text articles. These studies, focusing on the biomechanical and clinical outcomes of six-strand hamstring autografts in ACL reconstruction, were analyzed in detail. The outcome of this systematic review provides valuable insights into the efficacy of 6HS autografts in ACL surgery, enhancing the evidence base for orthopedic clinical practice (Figure 1).
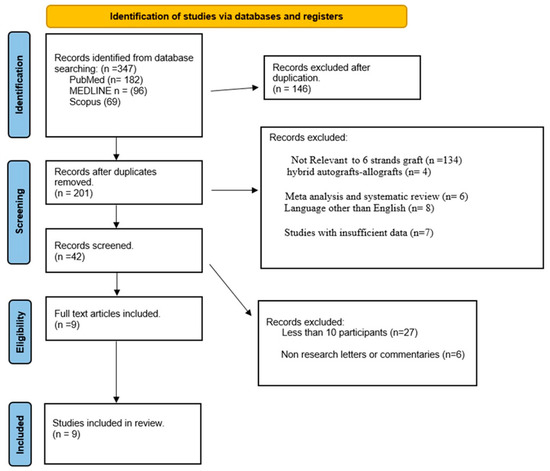
Figure 1.
Flow diagram for the literature review detailing the database search.
3. Results
This literature review analyzed studies focusing on the biomechanical and clinical outcomes of six-strand hamstring (6HS) autografts for anterior cruciate ligament (ACL) reconstruction. Nine studies were included in this review [21,22,23,24,25,26,27,28,29]. The studies varied in design, including prospective randomized clinical trials, retrospective cohort studies, and cadaveric studies, with sample sizes ranging from 12 to 413 subjects.
3.1. Biomechanical Outcomes
The six-strand hamstring autografts consistently showed improved biomechanical outcomes compared to traditional four-strand grafts. Enhanced knee stability, increased graft diameter, and superior rotational stability were recurrent themes. Specifically, the 6HS autografts facilitated an increased likelihood of achieving a graft diameter of 8 mm or greater, which is correlated with lower rates of graft failure. Studies like Laoruengthana et al. [21] and Nazari et al. [22] highlighted significant improvements in knee stability and graft size, respectively.
3.2. Clinical Outcomes
Clinically, patients with 6HS autografts reported high satisfaction levels, improved quality of life, and low re-injury rates. The use of 6HS autografts potentially enabled a more effective and faster rehabilitation process, allowing patients to confidently return to normal activities and sports. For instance, Attia et al. [23] noted high levels of knee functionality and very low re-injury rates, indicating favorable clinical outcomes.
3.3. Rehabilitation and Recovery
Rehabilitation protocols varied across the studies, with most patients returning to sports and normal activities between 5 and 12 months post-operation. The larger graft sizes associated with 6HS autografts were suggested to contribute to faster recovery times, as indicated in the study by Tutkus et al. [28].
3.4. Complications and Follow-Up
Complication rates were low, with some studies reporting no complications. The follow-up duration across the studies ranged from 16 to 44.27 months, providing a substantial postoperative period to assess the outcomes of the 6HS autografts.
3.5. Overall Efficacy
The 6HS autografts demonstrated a consistent trend of improved biomechanical and clinical outcomes. They were associated with better knee stability, larger graft diameters, higher patient satisfaction, and potentially shorter rehabilitation periods. These findings underscore the efficacy of 6HS autografts in ACL reconstruction, suggesting that they can be a reliable option in clinical practice, particularly for patients requiring stronger and more stable grafts. Table 1 and Table 2 show all the details.

Table 1.
Comparative of studies on 6-strand hamstring autografts, reconstruction, biomechanical efficacy, clinical outcomes, and rehabilitation.

Table 2.
Outcomes of six-strand hamstring autografts in ACL reconstruction: a multidimensional analysis.
4. Discussion
This systematic review comprehensively evaluates the biomechanical and clinical efficacy of six-strand hamstring (6HS) autografts for anterior cruciate ligament (ACL) reconstruction. The collective evidence from the included studies, which span prospective randomized trials, retrospective cohort studies, and cadaveric research, supports the notion that 6HS autografts provide enhanced biomechanical stability and favorable clinical outcomes, making them a compelling option in ACL surgery.
4.1. Biomechanical Efficacy
The biomechanical superiority of 6HS autografts, as demonstrated in this review, is a critical factor in their efficacy for ACL reconstruction. Enhanced knee stability, increased graft diameter, and superior rotational stability are key attributes that define the biomechanical advantage of 6HS autografts over traditional four-strand grafts. For example, the work by Laoruengthana et al. [21] and Nazari et al. [22] showed that 6HS autografts consistently achieve a graft diameter of 8 mm or greater, a dimension correlated with reduced graft failure and re-injury rate. This larger diameter mimics the native ACL more closely, providing better resistance to the forces exerted on the knee during physical activities. Dai et al. (2016) has shown that 6HS autografts exhibit superior biomechanical properties in terms of load-bearing capacity and stiffness, which are crucial for the long-term success of ACL reconstruction and the prevention of osteoarthritis development in the knee joint [30]. For instance, biomechanical testing has shown that 6HS autografts can withstand higher peak loads before failure compared to traditional four-strand grafts, which translates to a lower risk of graft rupture during high-impact activities. Furthermore, the integration of the 6HS autograft with the bone is a critical factor in the long-term success of the reconstruction [28,30]. The larger surface area of the graft promotes better osseointegration and faster biological healing, facilitating a more robust anchorage within the bone tunnels [30]. This not only accelerates the rehabilitation process but also minimizes the potential for graft slippage or pull-out, which are common complications associated with smaller grafts.
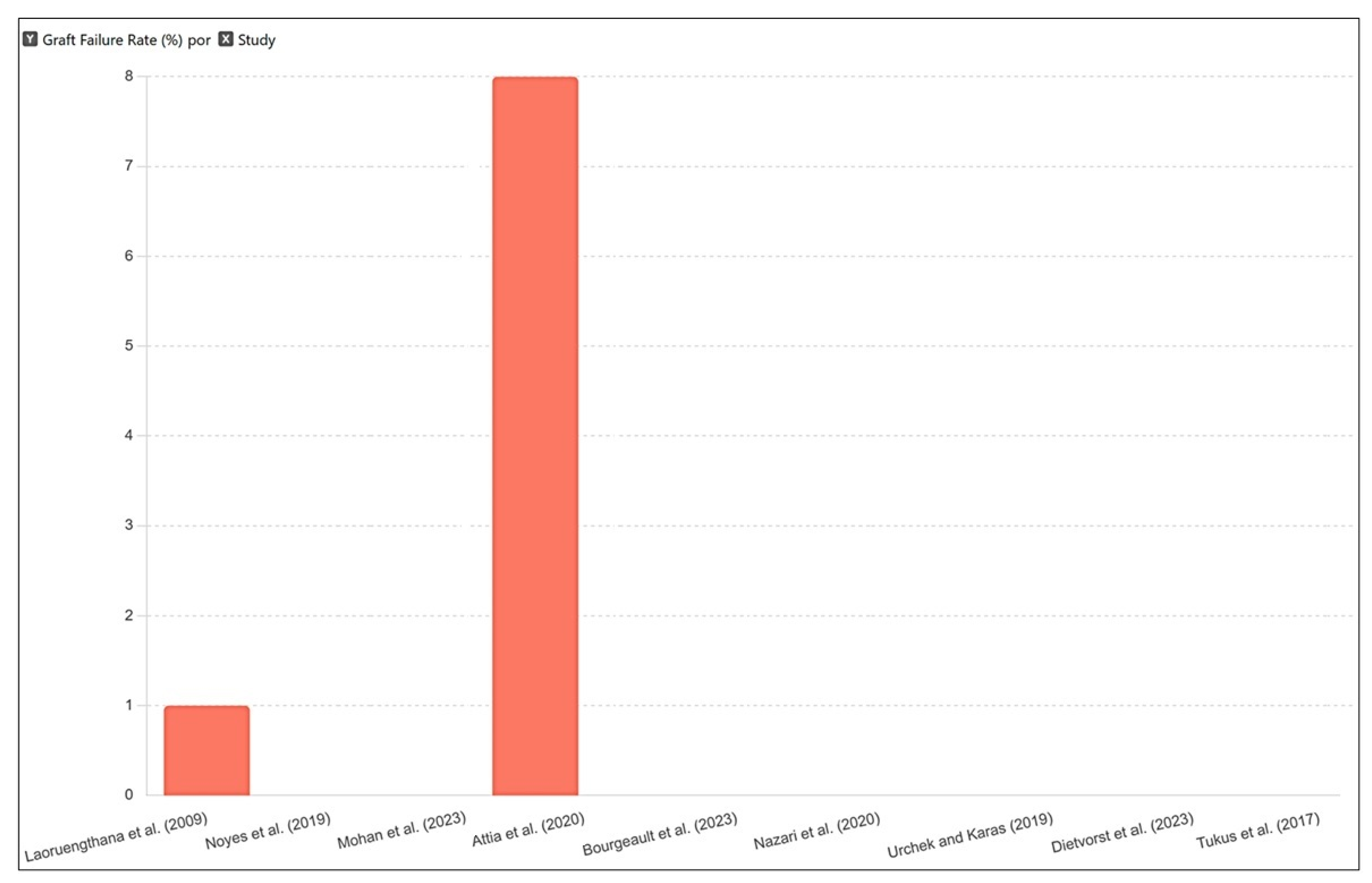
While 6HS autografts demonstrate robust outcomes, graft failure remains a potential risk, influenced by various factors. The size and handling of the graft are crucial; larger grafts, like those used in 6HS reconstructions, are typically associated with lower failure rates due to their strength and biomechanical compatibility with the knee’s natural movements. Surgical technique is another vital factor. The precision in tunnel placement and the efficacy of graft fixation play fundamental roles in the initial stability and long-term integration of the graft. Incorrect tunnel placement or suboptimal fixation can lead to abnormal mechanics and increased graft strain, potentially leading to failure (Figure 2).
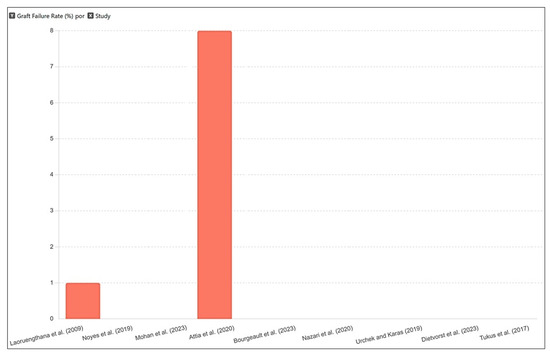
Figure 2.
Graft failure rates across studies on 6HS autografts. The failure rates are quite low across all studies, highlighting the reliability and effectiveness of the 6HS autografts [21,22,23,24,25,26,27,28,29].
4.2. Clinical Outcomes
Clinically, the adoption of 6HS autografts in ACL reconstruction met with positive outcomes. High levels of patient satisfaction, improved quality of life, and notably low re-injury rates characterize the postoperative recovery of patients receiving 6HS autografts. Yang et al. [14] highlighted the efficacy of 6HS autografts in achieving high knee functionality and significantly low re-injury rates, demonstrating their reliability in clinical practice. Recent clinical evaluations, like those by Ren et al. [31], observed that patients with 6HS autografts tend to have a faster return to sports and a higher likelihood of regaining pre-injury activity levels compared to those with traditional four-strand grafts. These findings suggest that 6HS autografts facilitate a more effective rehabilitation process, possibly due to their biomechanical properties that closely align with the native ACL [32].
4.3. Rehabilitation and Recovery
The recovery trajectory with 6HS autografts appears to be more accelerated, with patients often returning to sports and normal activities within 5 to 12 months post-operation. The larger graft sizes associated with 6HS autografts may be a contributing factor to the expedited recovery, as indicated in the study by Tutkus et al. [28]. This suggests a direct correlation between graft size and rehabilitation speed, underscoring the importance of graft selection in ACL reconstruction.
4.4. Long-Term Outcomes and Complications
The long-term efficacy of 6HS autografts in maintaining knee stability and function is supported by the low complication rates observed in the studies. Follow-up periods extending up to 44 months provide a robust framework for assessing the durability and effectiveness of these grafts over time. Clinically, the effectiveness of six-strand hamstring (6HS) autografts in anterior cruciate ligament (ACL) reconstruction is supported by evidence demonstrating high levels of patient satisfaction, improved quality of life, and lower re-injury rates. These outcomes suggest that 6HS autografts are robust and durable, capable of withstanding the demands of daily activities and sports, thus enabling a more efficient and potentially faster rehabilitation process [33,34,35,36]. For instance, Yang et al. [14] observed very low re-injury rates and high functional outcomes with 6HS autografts, emphasizing their clinical effectiveness. Additionally, recent studies, such as those by Chen et al. [37], corroborated these findings, noting the biomechanical advantages and positive patient-reported outcomes associated with these larger grafts.
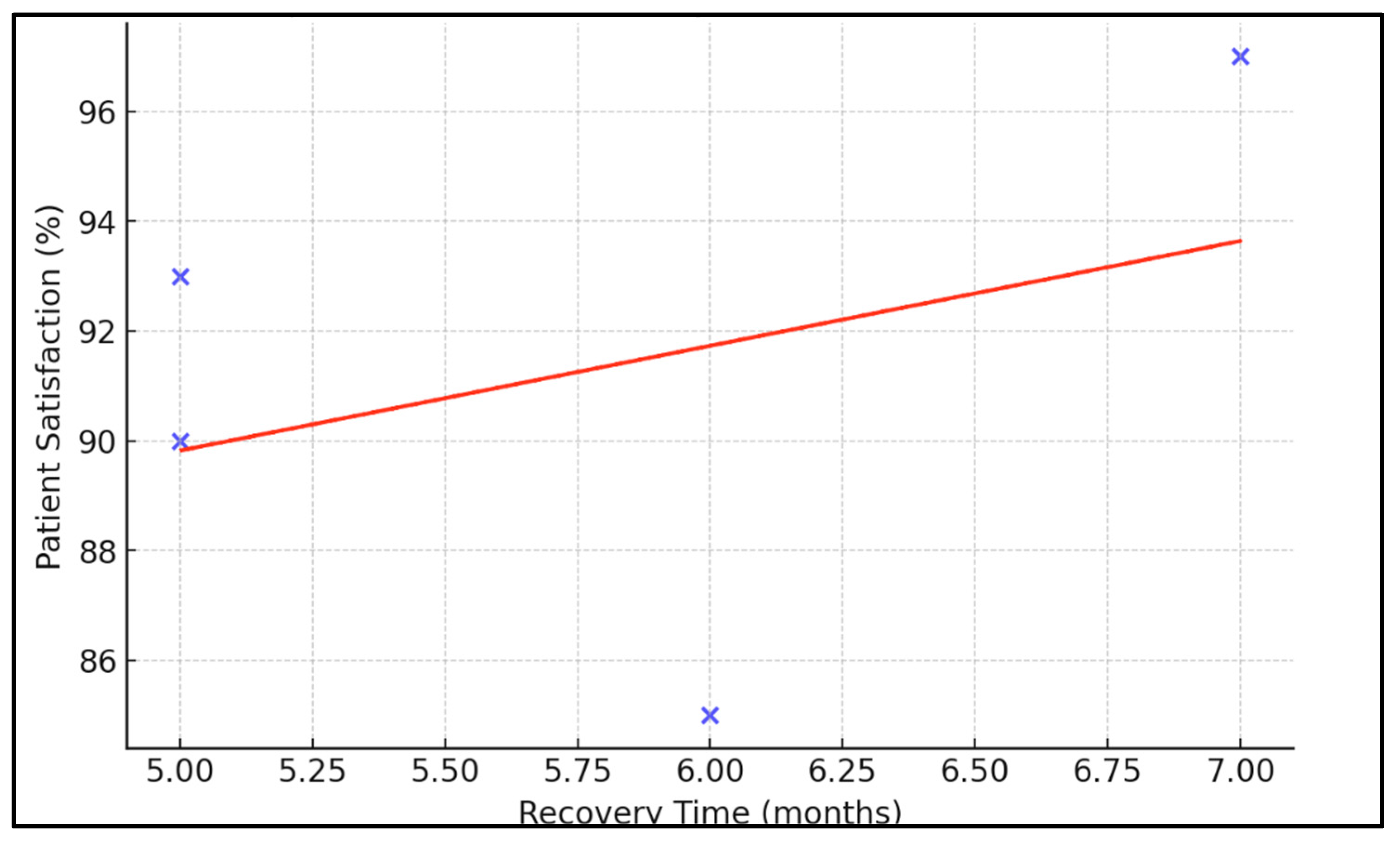
The impact of 6HS autografts on the rehabilitation process is particularly significant. Most of the reviewed studies suggest that the increased graft size not only enhances biomechanical stability but also facilitates quicker recovery timelines [38,39,40] (Figure 3). This is crucial for athletes and active individuals who prioritize a rapid and safe return to their pre-injury levels of activity [41,42,43]. Research by Saki et al. [10] reinforced this point, demonstrating that patients with 6HS autografts often experience a shorter rehabilitation period and a quicker return to sports, underscoring the functional benefits of these grafts.
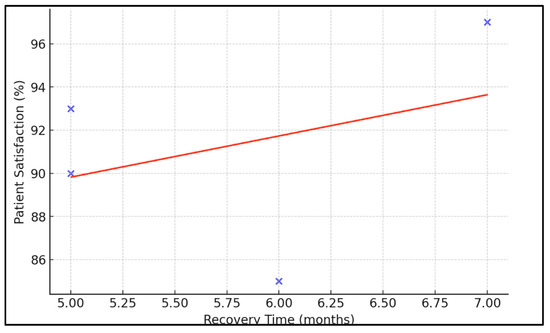
Figure 3.
Relationship between recovery times and patient satisfaction. Each point represents a different study, plotted according to the average recovery time and corresponding patient satisfaction percentage. The red line indicates the general trend between recovery time and satisfaction.
Furthermore, the complication rates associated with 6HS autografts are notably low, adding to their appeal in clinical settings. The long-term follow-up in these studies, which extends up to 44 months, offers a robust assessment of the durability and long-term effectiveness of 6HS autografts in ACL reconstruction. This extensive follow-up period is crucial for understanding the sustained performance of these grafts and their impact on joint health over time [44,45,46]. The clinical adoption of 6HS autografts in ACL reconstruction is justified by their demonstrated ability to provide stable, durable, and effective outcomes. Their contribution to enhanced patient satisfaction, lower re-injury rates, and expedited recovery, coupled with a favorable complication profile, underscores the value of 6HS autografts as a preferred option in ACL reconstruction, especially for individuals with high physical demands or those at increased risk of graft failure. Future research should aim to expand these findings with larger and more diverse patient cohorts to fully establish the long-term benefits and potential limitations of 6HS autografts in ACL surgery [24,47,48,49].
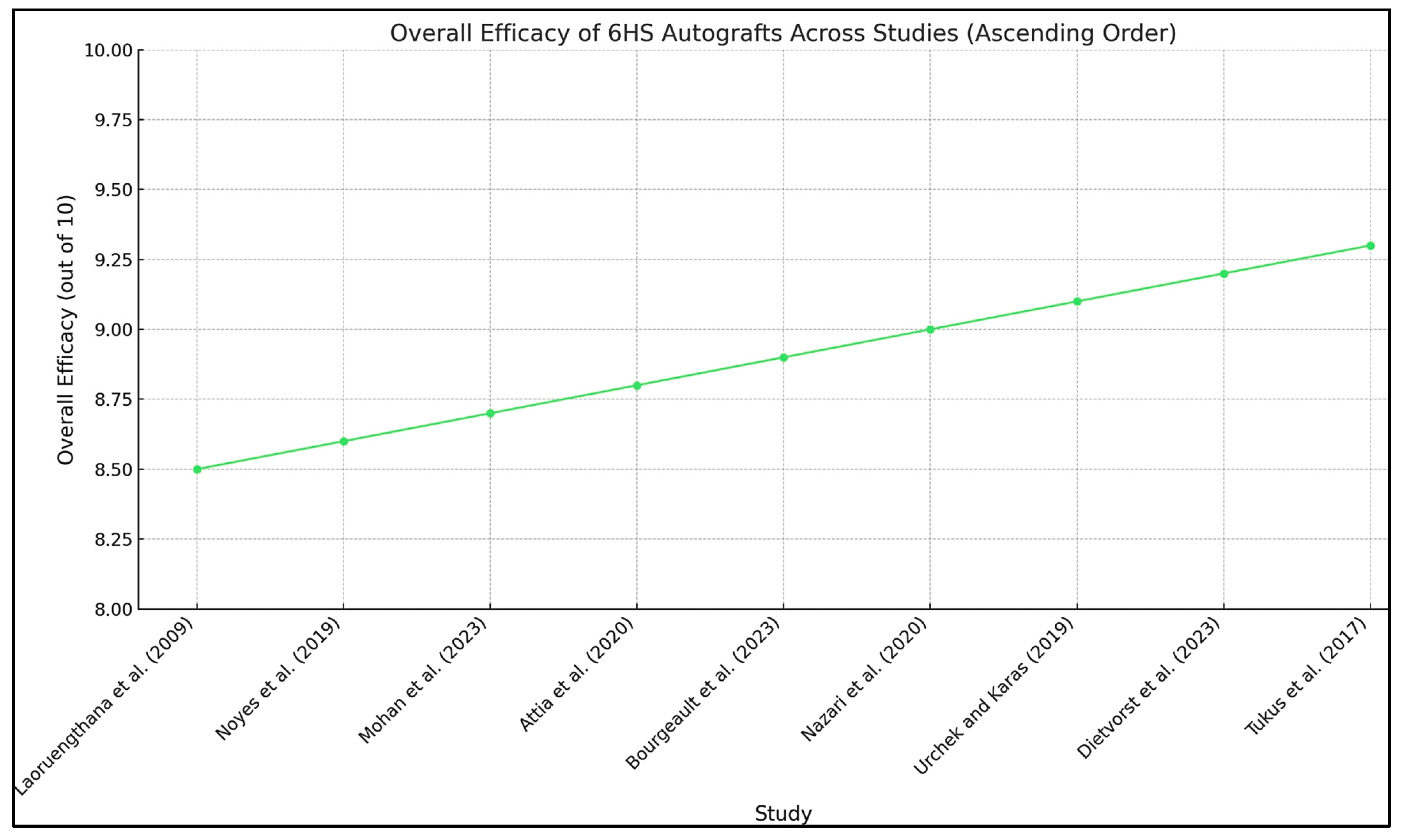
Moreover, long-term follow-up studies are essential to fully understand the durability of these grafts and their impact on knee joint health over time. Investigating the biomechanical properties of 6HS autografts in various patient populations, including those with different activity levels and biomechanical demands, would further refine the selection criteria for this graft option in ACL reconstruction surgery [21,22,23,24,25,26,27,28,29,50,51,52] (Figure 4).
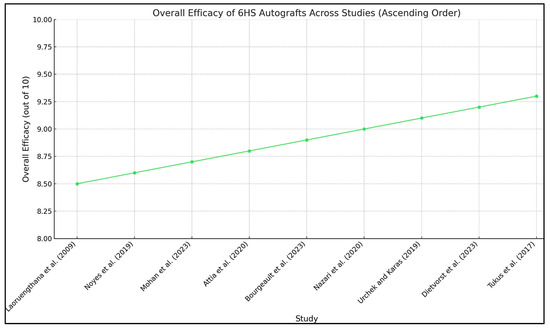
Figure 4.
The composite scores are consistently high across the studies, indicating strong performance of the 6HS autografts in ACL reconstruction. Green trendline shows a slight upward trend, suggesting improvements or increasingly positive outcomes in more recent studies or in studies with more refined surgical techniques and post-operative care [21,22,23,24,25,26,27,28,29].
4.5. Limitations of This Study
Heterogeneity of studies: The included studies vary in terms of design, sample size, and methodological quality, which could affect the consistency and generalizability of the findings. The variation in study protocols, surgical techniques, and outcome measures might lead to heterogeneity in the results, complicating the process of drawing definitive conclusions.
Limited long-term data: While some studies provide follow-up periods extending to over 44 months, there is still a need for longer-term data to fully understand the durability and outcomes of 6HS autografts in ACL reconstruction. The long-term risks, such as the development of osteoarthritis and graft longevity, remain less well-defined.
Sample size and population diversity: Many studies included in the review may have small sample sizes or may not represent a diverse patient population. This limitation could affect the applicability of the findings to broader, more heterogeneous populations, including variations in age, activity level, and comorbid conditions.
Comparative analysis: The review primarily focuses on 6HS autografts, with less emphasis on direct comparisons with other graft types like the four-strand hamstring, patellar tendon, or synthetic grafts. This limitation may restrict the understanding of the relative advantages or disadvantages of 6HS autografts in ACL reconstruction.
Publication bias: As with any systematic review, there is a potential for publication bias, where studies with positive outcomes are more likely to be published than those with negative or inconclusive results. This bias could skew the overall findings of the review towards more favorable outcomes for 6HS autografts.
Confounding factors: The reviewed studies might not adequately control for confounding factors such as patient activity level, rehabilitation protocols, and surgical experience, which could influence the outcomes of ACL reconstruction with 6HS autografts.
Reporting of complications: The incidence and type of complications associated with 6HS autografts are not uniformly reported across the studies, leading to potential underestimation or inconsistent reporting of adverse outcomes.
Future studies should focus on long-term follow-up to assess the durability and sustained efficacy of 6HS autografts over extended periods, potentially spanning 5 to 10 years. Comparative studies with other graft types, such as four-strand hamstring, bone–patellar tendon–bone, and synthetic grafts, are essential to establish the relative benefits and limitations of 6HS autografts. Standardizing study protocols, surgical techniques, and outcome measures across multiple centers will help reduce variability and enhance the generalizability of findings.
Additionally, exploring the impact of patient demographics, including age, sex, BMI, and activity levels, on the outcomes of 6HS autografts will provide valuable insights for tailoring ACL reconstruction to individual patient needs. Identifying optimal rehabilitation protocols through randomized controlled trials will further improve recovery times and functional outcomes for patients.
5. Conclusions
This literature review comprehensively assesses the biomechanical and clinical outcomes of six-strand hamstring (6HS) autografts in anterior cruciate ligament (ACL) reconstruction. The synthesis of findings from various study designs, including prospective randomized clinical trials, retrospective cohort studies, and cadaveric studies, indicates that 6HS autografts provide enhanced biomechanical stability and favorable clinical outcomes. The biomechanical advantages of 6HS autografts, such as improved knee stability and increased graft diameter, contribute to their efficacy in ACL reconstruction. These characteristics facilitate a closer mimicry of the native ACL’s function, offering a promising option for patients requiring robust reconstructive solutions. Clinically, the use of 6HS autografts has been associated with high patient satisfaction, improved quality of life, and notably low re-injury rates, which underscores their potential for facilitating effective and faster rehabilitation processes. However, while the outcomes of 6HS autografts are promising, it is crucial to consider the limitations of the available studies, including heterogeneity in study designs, limited long-term data, and variations in sample sizes and population diversity. Future research should focus on addressing these gaps, particularly through long-term, large-scale, randomized controlled trials that can provide more definitive evidence on the effectiveness and safety of 6HS autografts in ACL reconstruction.
Author Contributions
Conceptualization, O.A.V., N.A.V., D.B., M.D.J.E.R. and N.M.; methodology, D.B., K.K.A., E.G. and N.M.; validation, E.B., M.D.J.E.R. and N.M.; formal analysis, O.A.V., E.G., O.K. and N.M.; investigation, O.A.V., E.G., M.D.J.E.R. and N.M.; resources, O.A.V., E.G., O.K. and N.M.; data curation, O.A.V., N.A.V. and M.D.J.E.R.; writing—original draft preparation, O.A.V., E.G., O.K. and N.M.; writing—review and editing, M.D.J.E.R. and N.M.; visualization, E.B., M.D.J.E.R., and N.M.; supervision, O.A.V. and N.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
Ondar Artysh Vyacheslavovich, Nikonova Alina Vladimirovna, Dzhunusov Bekzhan, and Khaizhok Konstantin Ayanovich are medical doctor employees of the company JSC Group of Companies MEDSI (123056, Moscow, Russian Federation). The company did not have a role in the design of the study, in the collection, analyses or interpretation of data, in the writing of the manuscript or in the decision to publish the results.
References
- Goncharov, E.N.; Koval, O.A.; Bezuglov, E.N.; Goncharov, N.G. Anatomical features and significance of the anterolateral liga-ment of the knee. Int. Orthop. (SICOT) 2018, 42, 2859–2864. [Google Scholar] [CrossRef] [PubMed]
- Kaeding, C.C.; Léger-St-Jean, B.; Magnussen, R.A. Epidemiology and Diagnosis of Anterior Cruciate Ligament Injuries. Clin. Sports Med. 2017, 36, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Paudel, Y.R.; Sommerfeldt, M.; Voaklander, D. Increasing incidence of anterior cruciate ligament reconstruction: A 17-year population-based study. Knee Surg. Sports Traumatol. Arthrosc. 2022, 31, 248–255. [Google Scholar] [CrossRef] [PubMed]
- Strobel, M.J. Manual of Arthroscopic Surgery; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2002; Volume 1, p. 369. [Google Scholar]
- Goncharov, E.N.; Koval, O.A.; Dubrov, V.E.; Bezuglov, E.N.; Alekhin, A.A.; Goncharov, N.G. Mid-Term Results of Simultaneous Reconstruction of Anterior Cruciate and Anterolateral Ligaments in Athletes. Traumatol. Orthop. Russ. 2020, 26, 62–71. [Google Scholar] [CrossRef]
- Chambat, P.; Guier, C.; Sonnery-Cottet, B.; Fayard, J.M.; Thaunat, M. The evolution of ACL reconstruction over the last fifty years. Int. Orthop. 2013, 37, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Samuelsen, B.T.; Webster, K.E.; Johnson, N.R.; Hewett, T.E.; Krych, A.J. Hamstring Autograft versus Patellar Tendon Autograft for ACL Reconstruction: Is There a Difference in Graft Failure Rate? A Meta-analysis of 47,613 Patients. Clin. Orthop. Relat. Res. 2017, 475, 2459–2468. [Google Scholar] [CrossRef] [PubMed]
- Goncharov, E.N.; Koval, O.A.; Dubrov, V.E.; Bezuglov, E.N.; Filimonova, A.M.; Goncharov, N.G. Clinical experience with combined reconstruction of the anterior cruciate and anterolateral ligaments of the knee in sportsmen. Int. Orthop. (SICOT) 2019, 43, 2781–2788. [Google Scholar] [CrossRef] [PubMed]
- Rhatomy, S.; Asikin, A.I.Z.; Wardani, A.E.; Rukmoyo, T.; Lumban-Gaol, I.; Budhiparama, N.C. Peroneus longus autograft can be recommended as a superior graft to ham-string tendon in single-bundle ACL reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 3552–3559. [Google Scholar] [CrossRef]
- Saki, F.; Shafiee, H.; Tahayori, B.; Ramezani, F. The effects of core stabilization exercises on the neuromuscular function of athletes with ACL reconstruction. Sci. Rep. 2023, 13, 2202. [Google Scholar] [CrossRef]
- Grooms, D.R.; Chaput, M.; Simon, J.E.; Criss, C.R.; Myer, G.D.; Diekfuss, J.A. Combining Neurocognitive and Functional Tests to Improve Return-to-Sport Decisions Following ACL Reconstruction. J. Orthop. Sports Phys. Ther. 2023, 53, 415–419. [Google Scholar] [CrossRef]
- Borque, K.A.; Laughlin, M.S.; Pinheiro, V.H.; Jones, M.; Williams, A. Rebranding the ‘anatomic’ ACL reconstruction: Current concepts. J. ISAKOS 2023, 8, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Dahduli, O.S.; AlHossan, A.M.; Al Rushud, M.A.; Alneghaimshi, M.M.; Alotaibi, S.F.; AlNour, M.K.; Al Otaibi, A.H.; AlAseeri, A.; AlBatati, S. Early Surgical Reconstruction Versus Rehabilitation for Patients with Anterior Cruciate Ligament Rupture: A Systematic Review and Meta-Analysis. Cureus 2023, 15, e43370. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Lu, W.; Luo, Y.; Li, J.; Huang, X.; You, T. A Novel Predictor of the Length and Size of ACL Grafts in Chinese Han Adults for ACL Reconstruction: An MRI Study. Orthop. Surg. 2024, 16, 481–489. [Google Scholar] [CrossRef] [PubMed]
- Tang, N.; Eren, M.; Gurpinar, T.; Ozturkmen, Y. A prospective randomized controlled study of hamstring and bone-free quadriceps tendons autografts in arthroscopic ACL reconstruction. Eur. J. Orthop. Surg. Traumatol. 2024, 34, 293–301. [Google Scholar] [CrossRef] [PubMed]
- Balki, S.; Göktaş, H.E.; Öztemur, Z. Kinesio taping as a treatment method in the acute phase of ACL reconstruction: A double-blind, placebo-controlled study. Acta Orthop. Traumatol. Turc. 2016, 50, 628–634. [Google Scholar] [CrossRef] [PubMed]
- Biset, A.; Douiri, A.; Robinson, J.R.; Laboudie, P.; Colombet, P.; Graveleau, N.; Bouguennec, N. Tibial tunnel expansion does not correlate with four-strand graft maturation after ACL reconstruction using adjustable cortical suspensory fixation. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 1761–1770. [Google Scholar] [CrossRef] [PubMed]
- Shen, X.; Liu, T.; Xu, S.; Chen, B.; Tang, X.; Xiao, J.; Qin, Y. Optimal Timing of Anterior Cruciate Ligament Reconstruction in Patients With Anterior Cruciate Ligament Tear: A Systematic Review and Meta-analysis. JAMA Netw. Open. 2022, 5, e2242742. [Google Scholar] [CrossRef] [PubMed]
- Goncharov, E.N.; Koval, O.A.; Bezuglov, E.N.; Vetoshkin, A.A.; Goncharov, N.G.; Encarnación Ramirez, M.; Nurmukhametov, R.; Montemurro, N. Outcome of Primary Anterior Cruciate Ligament Reconstruction with Peroneus Longus and Bone–Patellar Tendon–Bone Autografts: A Clinical Comparative Study. Surgeries 2023, 4, 434–445. [Google Scholar] [CrossRef]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 Explanation and Elaboration: Updated Guidance and Exemplars for Reporting Systematic Reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef] [PubMed]
- Laoruengthana, A.; Pattayakorn, S.; Chotanaputhi, T.; Kosiyatrakul, A. Clinical comparison between six-strand hamstring tendon and patellar tendon autograft in arthroscopic anterior cruciate ligament reconstruction: A prospective, randomized clinical trial. J. Med. Assoc. Thai. 2009, 92, 491–497. [Google Scholar]
- Nazari, G.; Barton, K.I.; Bryant, D.; Getgood, A.; Brown, C.H., Jr. Five- and six-strand hamstring grafts consistently produce appropriate graft diameters for anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 2940–2947. [Google Scholar] [CrossRef]
- Attia, A.K.; Nasef, H.; ElSweify, K.H.; Adam, M.A.; AbuShaaban, F.; Arun, K. Failure Rates of 5-Strand and 6-Strand vs Quadrupled Hamstring Autograft ACL Reconstruction: A Comparative Study of 413 Patients with a Minimum 2-Year Follow-up. Orthop. J. Sports Med. 2020, 8, 2325967120946326. [Google Scholar] [CrossRef] [PubMed]
- Mohan, R.; Kwaees, T.A.; Thomas, T.; Pydisetty, R. Cohort study of short-term outcomes after ACL-reconstruction using autograft with internal brace reinforcement versus isolated autograft demonstrating no significant difference. J. Orthop. 2023, 43, 115–120. [Google Scholar] [CrossRef] [PubMed]
- Dietvorst, M.; van der Steen, M.C.M.; van den Besselaar, M.; Janssen, R.P. Height is a predictor of hamstring tendon length and ACL graft characteristics in adolescents. BMC Musculoskelet. Disord. 2023, 24, 563. [Google Scholar] [CrossRef]
- Bourgeault-Gagnon, Y.; Leang, A.K.; Bédard, S.; Lebel, K.; Balg, F.; Vézina, F. Estimated diameter increase from a 4S to a 6S hamstring graft configuration—A cadaveric study. SICOT J. 2023, 9, 34. [Google Scholar] [CrossRef]
- Urchek, R.; Karas, S. Biomechanical Comparison of Quadriceps and 6-Strand Hamstring Tendon Grafts in Anterior Cruciate Ligament Reconstruction. Orthop. J. Sports Med. 2019, 7, 2325967119879113. [Google Scholar] [CrossRef] [PubMed]
- Tutkus, V.; Kluonaitis, K.; Silove, S.; Tutkuviene, J. ACL reconstruction using 5- or 6-strand hamstring autograft provides graft’s diameter bigger than 8 mm. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 1349–1356. [Google Scholar] [CrossRef]
- Noyes, F.R.; Huser, L.E.; Ashman, B.; Palmer, M. Anterior Cruciate Ligament Graft Conditioning Required to Prevent an Abnormal Lachman and Pivot Shift After ACL Reconstruction: A Robotic Study of 3 ACL Graft Constructs. Am. J. Sports Med. 2019, 47, 1376–1384. [Google Scholar] [CrossRef] [PubMed]
- Dai, C.; Wang, F.; Wang, X.; Wang, R.; Wang, S.; Tang, S. Arthroscopic single-bundle anterior cruciate ligament reconstruction with six-strand hamstring tendon allograft versus bone-patellar tendon-bone allograft. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 2915–2922. [Google Scholar] [CrossRef]
- Ren, Y.; Wang, J.; Ji, J.; Zhang, C.; Meng, Q. Comparison of Clinical Outcomes Between Modern Augmented ACL Repair and Autograft ACL Reconstruction: A Systematic Review and Meta-analysis of Studies With Minimum 2-Year Follow-up. Orthop. J. Sports Med. 2024, 12, 23259671231223743. [Google Scholar] [CrossRef]
- Charlton, W.P.H.; Randolph, D.A.; Lemos, S.; Shields, C.L. Clinical Outcome of Anterior Cruciate Ligament Reconstruction with Quadrupled Hamstring Tendon Graft and Bioabsorbable Interference Screw Fixation. Am. J. Sport. Med. 2003, 31, 518–521. [Google Scholar] [CrossRef] [PubMed]
- Van Vijven, M.; van Groningen, B.; Janssen, R.P.; van der Steen, M.C.; van Doeselaar, M.; Stefanoska, D.; van Donkelaar, C.C.; Ito, K.; Foolen, J. Local variations in mechanical properties of human hamstring tendon autografts for anterior cruciate ligament reconstruction do not translate to a mechanically inferior strand. J. Mech. Behav. Biomed. Mater. 2022, 126, 105010. [Google Scholar] [CrossRef] [PubMed]
- Montemurro, N.; Ortenzi, V.; Naccarato, G.A.; Perrini, P. Angioleiomyoma of the knee: An uncommon cause of leg pain. A systematic review of the literature. Interdiscip. Neurosurg. 2020, 22, 100877. [Google Scholar] [CrossRef]
- El-Azab, H.; Moursy, M.; Mohamed, M.A.; Elsayed, M. A comparison of the outcomes of anterior curciate ligament reconstruction with large-size graft versus reconstruction with average-size graft combined with extraarticular tenodesis. Injury 2023, 54, 976–982. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Zhao, J.; Shen, J.; Du, B.; Yuan, B. Anatomic single-bundle anterior cruciate ligament reconstruction in Asian population. ANZ J. Surg. 2013, 83, 262–267. [Google Scholar] [CrossRef]
- Chen, T.; Zhang, P.; Chen, J.; Hua, Y.; Chen, S. Long-Term Outcomes of Anterior Cruciate Ligament Reconstruction Using Either Synthetics With Remnant Preservation or Hamstring Autografts: A 10-Year Longitudinal Study. Am. J. Sports Med. 2017, 45, 2739–2750. [Google Scholar] [CrossRef] [PubMed]
- Tian, S.; Wang, B.; Liu, L.; Wang, Y.; Ha, C.; Li, Q.; Yang, X.; Sun, K. Irradiated Hamstring Tendon Allograft Versus Autograft for Anatomic Double-Bundle Anterior Cruciate Ligament Reconstruction: Midterm Clinical Outcomes. Am. J. Sports Med. 2016, 44, 2579–2588. [Google Scholar] [CrossRef]
- Goncharov, E.N.; Koval, O.A.; Nikolaevich Bezuglov, E.; Encarnacion Ramirez, M.D.; Engelgard, M.; Igorevich, E.I.; Saporiti, A.; Valentinovich Kotenko, K.; Montemurro, N. Stromal Vascular Fraction Therapy for Knee Osteoarthritis: A Systematic Review. Medicina 2023, 59, 2090. [Google Scholar] [CrossRef]
- Goncharov, E.N.; Koval, O.A.; Nikolaevich Bezuglov, E.; Engelgard, M.; Igorevich, E.I.; Velentinovich Kotenko, K.; Encarnacion Ramirez, M.D.; Montemurro, N. Comparative Analysis of Stromal Vascular Fraction and Alternative Mechanisms in Bone Fracture Stimulation to Bridge the Gap between Nature and Technological Advancement: A Systematic Review. Biomedicines 2024, 12, 342. [Google Scholar] [CrossRef]
- Sun, K.; Zhang, J.; Wang, Y.; Xia, C.; Zhang, C.; Yu, T.; Tian, S. Arthroscopic reconstruction of the anterior cruciate ligament with hamstring tendon autograft and fresh-frozen allograft: A prospective, randomized controlled study. Am. J. Sports Med. 2011, 39, 1430–1438. [Google Scholar] [CrossRef] [PubMed]
- Helito, C.P.; da Silva, A.G.; Sobrado, M.F.; Guimarães, T.M.; Gobbi, R.G.; Pécora, J.R. Small Hamstring Tendon Graft for Anterior Cruciate Ligament Reconstruction Combined With Anterolateral Ligament Reconstruction Results in the Same Failure Rate as Larger Hamstring Tendon Graft Reconstruction Alone. Arthroscopy 2023, 39, 1671–1679. [Google Scholar] [CrossRef] [PubMed]
- Mohtadi, N.; Barber, R.; Chan, D.; Paolucci, E.O. Complications and Adverse Events of a Randomized Clinical Trial Comparing 3 Graft Types for ACL Reconstruction. Clin. J. Sport Med. 2016, 26, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Lewandrowski, K.U.; Elfar, J.C.; Li, Z.M.; Burkhardt, B.W.; Lorio, M.P.; Winkler, P.A.; Oertel, J.M.; Telfeian, A.E.; Dowling, Á.; Vargas, R.A.A.; et al. The Changing Environment in Postgraduate Education in Orthopedic Surgery and Neurosurgery and Its Impact on Technology-Driven Targeted Interventional and Surgical Pain Management: Perspectives from Europe, Latin America, Asia, and The United States. J. Pers. Med. 2023, 13, 852. [Google Scholar] [CrossRef] [PubMed]
- Ignozzi, A.J.; Moran, T.E.; Werner, B.C. No Difference Could Be Detected in Clinical Outcomes of 5-Strand and Quadruple Hamstring Autografts of Similar Diameter in Anterior Cruciate Ligament Reconstruction: A Retrospective Cohort Study. HSS J. 2023, 19, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Moran, T.E.; Ramamurti, P.; Wells, D.K.; Thompson, X.; Hart, J.M.; Diduch, D.R.; Brockmeier, S.F.; Miller, M.D.; Gwathmey, W.F.; Werner, B.C. No Deficits in Functional Outcomes of the Contralateral Limb Are Seen When the Hamstring Is Harvested for Augmentation of Small Diameter Ipsilateral Hamstring Autograft. Arthrosc. Sports Med. Rehabil. 2023, 5, 100798. [Google Scholar] [CrossRef] [PubMed]
- Montemurro, N. Telemedicine: Could it represent a new problem for spine surgeons to solve? Global Spine J. 2022, 12, 1306–1307. [Google Scholar] [CrossRef] [PubMed]
- Yuan, W.; Qi, W.; Hu, T.; Zhang, J.; An, M.Y.; Zhao, G.; Wang, X.P.; Li, C.; Liu, Y. Outcomes of RigidFix Cross Pin Fixation in Femoral and Tibial Tunnel for Anterior Cruciate Ligament Reconstruction. Orthop. Surg. 2024, 16, 337–345. [Google Scholar] [CrossRef]
- Zaffagnini, S.; Marcheggiani Muccioli, G.M.; Grassi, A.; Roberti di Sarsina, T.; Raggi, F.; Signorelli, C.; Urrizola, F.; Spinnato, P.; Rimondi, E.; Marcacci, M. Over-the-top ACL Reconstruction Plus Extra-articular Lateral Tenodesis With Hamstring Tendon Grafts: Prospective Evaluation With 20-Year Minimum Follow-up. Am. J. Sports Med. 2017, 45, 3233–3242. [Google Scholar] [CrossRef] [PubMed]
- Igdir, V.; Gencer, B.; Dogan, O.; Caliskan, E.; Orhan, A.; Ozbudak, S.D. The effects of remnant-preserving anterior cruciate ligament reconstruction on proprioception: A prospective comparative study. Acta Orthop. Traumatol. Turc. 2023, 57, 109–115. [Google Scholar] [CrossRef]
- Montemurro, N.; Pierozzi, E.; Inchingolo, A.M.; Pahwa, B.; De Carlo, A.; Palermo, A.; Scarola, R.; Dipalma, G.; Corsalini, M.; Inchingolo, A.D.; et al. New biograft solution, growth factors and bone regenerative approaches in neurosurgery, dentistry, and orthopedics: A review. Eur Rev Med Pharmacol Sci. 2023, 27, 7653–7664. [Google Scholar]
- Movahedinia, M.; Movahedinia, S.; Hosseini, S.; Motevallizadeh, A.; Salehi, B.; Shekarchi, B.; Shahrezaee, M. Prediction of hamstring tendon autograft diameter using preoperative measurements with different cut-offs between genders. J. Exp. Orthop. 2023, 10, 4. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).