Severe Attrition and Poor Satisfaction in Patients Undergoing Telerehabilitation vs. Standard In-Person Rehabilitation after Arthroscopic Rotator Cuff Repairs and Anterior Cruciate Ligament Reconstructions
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Setting
2.2. Ethics Approval
2.3. Patient Eligibility Criteria
2.4. Randomization and Blinding
2.5. ACLR Surgical Technique and Rehabilitation
2.6. ARCR Surgical Technique and Rehabilitation
2.7. Telerehabilitation’s Set-Up and Implementation
2.8. Survey Description and Outcomes Evaluated
2.9. Sample Size Determination and Statistical Analysis
3. Results
3.1. Cohort Demographics
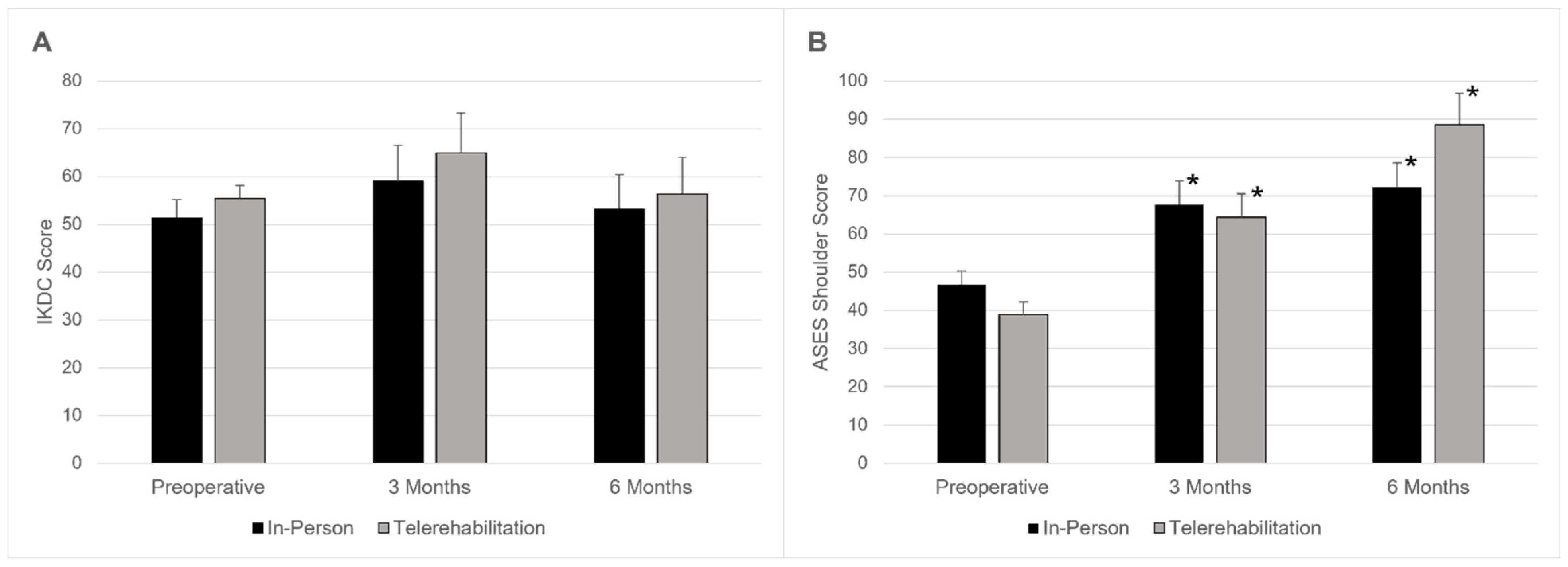
3.2. Patient-Reported Outcomes over Time
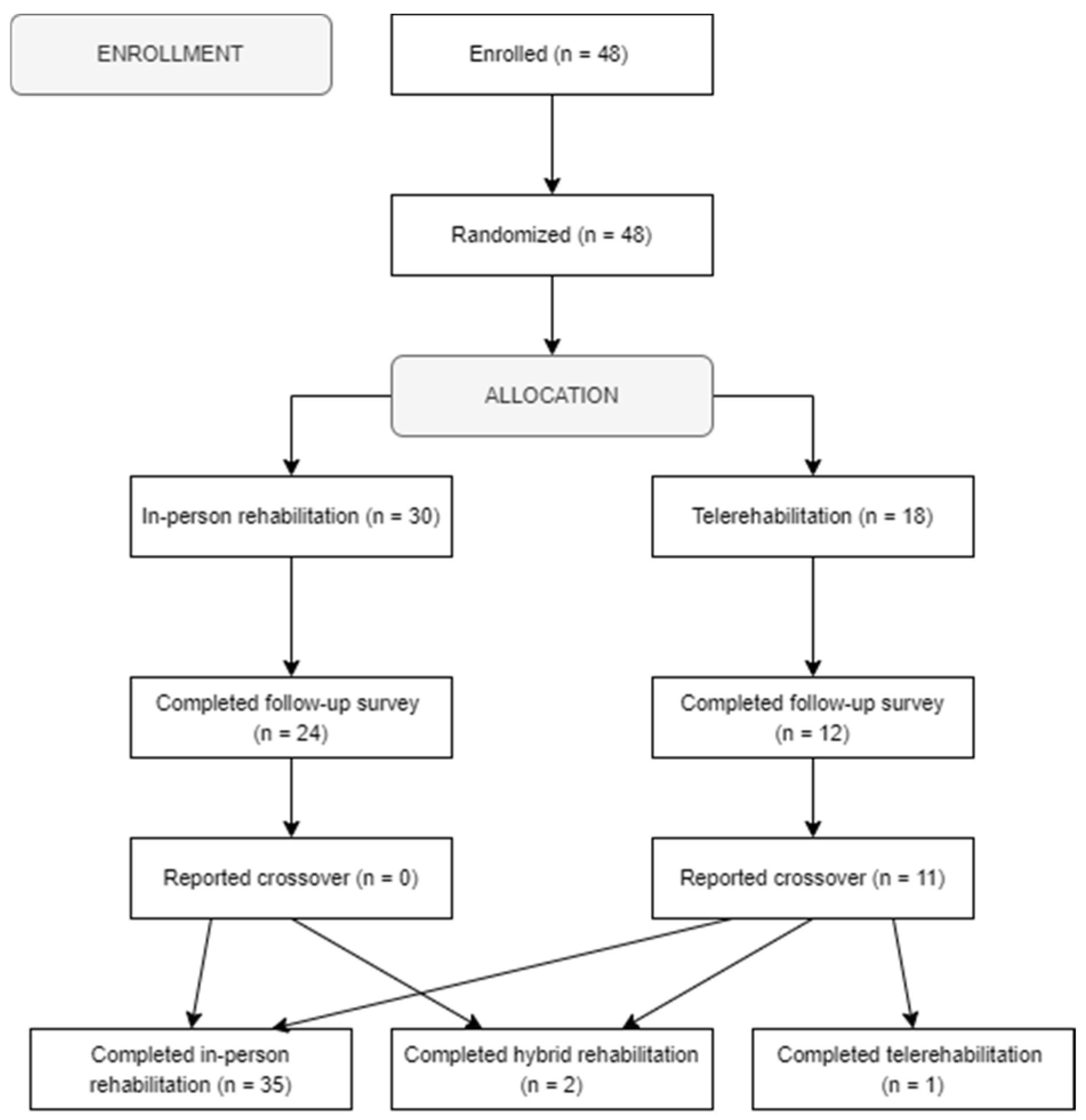
3.3. Attrition, Crossover, and Final Interventions
3.4. Satisfaction with Rehabilitation Modality
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
- AAOS: Board or committee member.
- Arthrex, Inc: Paid consultant; research support.
- Arthroscopy: Editorial or governing board.
- Arthroscopy Association of North America: Board or committee member.
- Journal of Cartilage and Joint Preservation: Editorial or governing board.
- JRF Ortho: Paid consultant.
- Mitek: Paid consultant.
- Orcosa, Inc: Research support.
- Springer: Publishing royalties, financial or material support.
- AAOS: Board or committee member.
- American Orthopaedic Association: Board or committee member.
- Arthrex, Inc: Paid consultant; Paid presenter or speaker.
- Arthroscopy Association of North America: Board or committee member.
- Better PT: Stock or stock options.
- Cartiheal: Research support.
- Cartilage, Bulletin of the Hospital For Joint Diseases: Editorial or governing board.
- Fidia: Paid consultant; research support.
- Flexion Therapeutics: Paid consultant
- Jaypee Publishing: Publishing royalties, financial or material support.
- Joint Restoration Foundation: Paid consultant.
- Organogenesis: Paid consultant; Paid presenter or speaker; research support.
- Smith & Nephew: Paid consultant; paid presenter or speaker.
- Springer: Publishing royalties, financial or material support.
- Subchondral Solutions: Paid consultant.
- Vericel: Paid consultant; Paid presenter or speaker.
- Arthrex, Inc: Research support.
- Bulletin for the Hospital for Joint Diseases: Editorial or governing board.
- JBJS Reviews: Editorial or governing board.
- Mitek: Research support.
- Smith & Nephew: Research support.
- Wolters Kluwer Health—Lippincott Williams & Wilkins: Publishing royalties, financial or material support.
- AAOS: Board or committee member.
- Arthroscopy Association of North America: Board or committee member.
- Mitek: Paid consultant.
- Stryker: Research support.
- ETH
- Arthroscopy: Editorial or governing board.
- European Society for Surgery of the Shoulder and Elbow: Board or committee member.
- Journal of Shoulder and Elbow Surgery: Editorial or governing board.
References
- Perednia, D.A.; Allen, A. Telemedicine technology and clinical applications. JAMA 1995, 273, 483–488. [Google Scholar] [CrossRef] [PubMed]
- Laskowski, E.R.; Johnson, S.E.; Shelerud, R.A.; Lee, J.A.; Rabatin, A.E.; Driscoll, S.W.; Moore, B.J.; Wainberg, M.C.; Terzic, C.M. The Telemedicine Musculoskeletal Examination. Mayo Clin. Proc. 2020, 95, 1715–1731. [Google Scholar] [CrossRef] [PubMed]
- Del Hoyo, J.; Aguas, M. Cost-effectiveness of Telemedicine-directed Specialized vs Standard Care for Patients with Inflammatory Bowel Diseases in a Randomized Trial. Clin. Gastroenterol. Hepatol. 2021, 19, 206–207. [Google Scholar] [CrossRef] [PubMed]
- Cui, S.; Sedney, C.L.; Daffner, S.D.; Large, M.J.; Davis, S.K.; Crossley, L.; France, J.C. Effects of telemedicine triage on efficiency and cost-effectiveness in spinal care. Spine J. 2021, 21, 779–784. [Google Scholar] [CrossRef] [PubMed]
- Kruse, C.S.; Lee, K.; Watson, J.B.; Lobo, L.G.; Stoppelmoor, A.G.; Oyibo, S.E. Measures of Effectiveness, Efficiency, and Quality of Telemedicine in the Management of Alcohol Abuse, Addiction, and Rehabilitation: Systematic Review. J. Med. Internet Res. 2020, 22, e13252. [Google Scholar] [CrossRef] [PubMed]
- Rozycki, S.W.; Marvin, K.M.; Landers, J.T.; Davis, K.L.; Ambrosio, A.A. Telemedicine Proof of Concept and Cost Savings during Underway Naval Operations. Telemed. J. e-Health 2021, 27, 503–507. [Google Scholar] [CrossRef] [PubMed]
- Benis, A.; Banker, M.; Pinkasovich, D.; Kirin, M.; Yoshai, B.E.; Benchoam-Ravid, R.; Ashkenazi, S.; Seidmann, A. Reasons for Utilizing Telemedicine during and after the COVID-19 Pandemic: An Internet-Based International Study. J. Clin. Med. 2021, 10, 5519. [Google Scholar] [CrossRef]
- Mishra, V. Factors affecting the adoption of telemedicine during COVID-19. Indian J. Public Health 2020, 64, S234–S236. [Google Scholar] [CrossRef] [PubMed]
- Thirunavukkarasu, A.; Alotaibi, N.H.; Al-Hazmi, A.H.; Alenzi, M.J.; Alshaalan, Z.M.; Alruwaili, M.G.; Alruwaili, T.A.M.; Alanazi, H.; Alosaimi, T.H. Patients’ Perceptions and Satisfaction with the Outpatient Telemedicine Clinics during COVID-19 Era in Saudi Arabia: A Cross-Sectional Study. Healthcare 2021, 9, 1739. [Google Scholar] [CrossRef]
- Kim, H.B.; Han, S.; Shin, H.; Lee, Y.H.; Lee, K.M.; Kwak, J.R.; Cho, Y.S.; Kim, H.; Lim, H.; Kim, G.W.; et al. Operation and management of a community treatment center using telemedicine for foreign patients with mild COVID-19 symptoms. Medicine 2021, 100, e27948. [Google Scholar] [CrossRef]
- Mahmoud, M.A.; Daboos, M.; Gouda, S.; Othman, A.; Abdelmaboud, M.; Hussein, M.E.; Akl, M. Telemedicine (virtual clinic) effectively delivers the required healthcare service for pediatric ambulatory surgical patients during the current era of COVID-19 pandemic: A mixed descriptive study. J. Pediatr. Surg. 2021, 57, 630–636. [Google Scholar] [CrossRef] [PubMed]
- Cheung, M.C.; Franco, B.B.; Meti, N.; Thawer, A.; Tahmasebi, H.; Shankar, A.; Loblaw, A.; Wright, F.C.; Fox, C.; Peek, N.; et al. Delivery of Virtual Care in Oncology: Province-Wide Interprofessional Consensus Statements Using a Modified Delphi Process. Curr. Oncol. 2021, 28, 5332–5345. [Google Scholar] [CrossRef]
- Fiani, B.; Siddiqi, I.; Lee, S.C.; Dhillon, L. Telerehabilitation: Development, Application, and Need for Increased Usage in the COVID-19 Era for Patients with Spinal Pathology. Cureus 2020, 12, e10563. [Google Scholar] [CrossRef]
- Eichler, S.; Salzwedel, A.; Rabe, S.; Mueller, S.; Mayer, F.; Wochatz, M.; Hadzic, M.; John, M.; Wegscheider, K.; Völler, H. The Effectiveness of Telerehabilitation as a Supplement to Rehabilitation in Patients After Total Knee or Hip Replacement: Randomized Controlled Trial. JMIR Rehabil. Assist. Technol. 2019, 6, e14236. [Google Scholar] [CrossRef] [PubMed]
- Piqueras, M.; Marco, E.; Coll, M.; Escalada, F.; Ballester, A.; Cinca, C.; Belmonte, R.; Muniesa, J.M. Effectiveness of an interactive virtual telerehabilitation system in patients after total knee arthoplasty: A randomized controlled trial. J. Rehabil. Med. 2013, 45, 392–396. [Google Scholar] [CrossRef] [PubMed]
- Russell, T.G.; Buttrum, P.; Wootton, R.; Jull, G.A. Internet-based outpatient telerehabilitation for patients following total knee arthroplasty: A randomized controlled trial. J. Bone Jt. Surg. Am. 2011, 93, 113–120. [Google Scholar] [CrossRef]
- Abdelshahed, M.; Mahure, S.A.; Kaplan, D.J.; Mollon, B.; Zuckerman, J.D.; Kwon, Y.W.; Rokito, A.S. Arthroscopic Rotator Cuff Repair: Double-Row Transosseous Equivalent Suture Bridge Technique. Arthrosc. Tech. 2016, 5, e1297–e1304. [Google Scholar] [CrossRef] [PubMed]
- Keel, S.; Schmid, A.; Keller, F.; Schoeb, V. Investigating the use of digital health tools in physiotherapy: Facilitators and barriers. Physiother. Theory Pract. 2023, 39, 1449–1468. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- Higgins, L.D.; Taylor, M.K.; Park, D.; Ghodadra, N.; Marchant, M.; Pietrobon, R.; Cook, C. Reliability and validity of the International Knee Documentation Committee (IKDC) Subjective Knee Form. Jt. Bone Spine 2007, 74, 594–599. [Google Scholar] [CrossRef]
- Wylie, J.D. Functional outcomes assessment in shoulder surgery. World J. Orthop. 2014, 5, 623. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, G.M.; Artino, A.R., Jr. Analyzing and interpreting data from likert-type scales. J. Grad. Med. Educ. 2013, 5, 541–542. [Google Scholar] [CrossRef] [PubMed]
- Nwachukwu, B.U.; Sullivan, S.W.; Rauck, R.C.; James, E.W.; Burger, J.A.; Altchek, D.W.; Allen, A.A.; Williams, R.J., 3rd. Patient-Reported Outcomes and Factors Associated with Achieving the Minimal Clinically Important Difference after ACL Reconstruction: Results at a Mean 7.7-Year Follow-up. JB JS Open Access 2021, 6, e21.00056. [Google Scholar] [CrossRef]
- Malavolta, E.A.; Yamamoto, G.J.; Bussius, D.T.; Assuncao, J.H.; Andrade-Silva, F.B.; Gracitelli, M.E.C.; Ferreira Neto, A.A. Establishing minimal clinically important difference for the UCLA and ASES scores after rotator cuff repair. Orthop. Traumatol. Surg. Res. 2022, 108, 102894. [Google Scholar] [CrossRef] [PubMed]
- Vuolio, S.; Winblad, I.; Ohinmaa, A.; Haukipuro, K. Videoconferencing for orthopaedic outpatients: One-year follow-up. J. Telemed. Telecare 2003, 9, 8–11. [Google Scholar] [CrossRef] [PubMed]
- Sathiyakumar, V.; Apfeld, J.C.; Obremskey, W.T.; Thakore, R.V.; Sethi, M.K. Prospective randomized controlled trial using telemedicine for follow-ups in an orthopedic trauma population: A pilot study. J. Orthop. Trauma 2015, 29, e139–e145. [Google Scholar] [CrossRef]
- Pastora-Bernal, J.M.; Martín-Valero, R.; Barón-López, F.J.; Estebanez-Pérez, M.J. Evidence of benefit of telerehabitation after orthopedic surgery: A systematic review. J. Med. Internet Res. 2017, 19, e142. [Google Scholar] [CrossRef] [PubMed]
- Buvik, A.; Bugge, E.; Knutsen, G.; Småbrekke, A.; Wilsgaard, T. Quality of care for remote orthopaedic consultations using telemedicine: A randomised controlled trial. BMC Health Serv. Res. 2016, 16, 483. [Google Scholar] [CrossRef]
- Buvik, A.; Bergmo, T.S.; Bugge, E.; Smaabrekke, A.; Wilsgaard, T.; Olsen, J.A. Cost-effectiveness of telemedicine in remote orthopedic consultations: Randomized controlled trial. J. Med. Internet Res. 2019, 21, e11330. [Google Scholar] [CrossRef]
- Kane, L.T.; Thakar, O.; Jamgochian, G.; Lazarus, M.D.; Abboud, J.A.; Namdari, S.; Horneff, J.G. The role of telehealth as a platform for postoperative visits following rotator cuff repair: A prospective, randomized controlled trial. J. Shoulder Elb. Surg. 2020, 29, 775–783. [Google Scholar] [CrossRef] [PubMed]
- Sharareh, B.; Schwarzkopf, R. Effectiveness of telemedical applications in postoperative follow-up after total joint arthroplasty. J. Arthroplast. 2014, 29, 918–922.e1. [Google Scholar] [CrossRef]
- Marsh, J.; Hoch, J.S.; Bryant, D.; MacDonald, S.J.; Naudie, D.; McCalden, R.; Howard, J.; Bourne, R.; McAuley, J. Economic evaluation of web-based compared with in-person follow-up after total joint arthroplasty. J. Bone Jt. Surg. 2014, 96, 1910–1916. [Google Scholar] [CrossRef] [PubMed]
- Marsh, J.D.; Bryant, D.M.; MacDonald, S.J.; Naudie, D.D.; McCalden, R.W.; Howard, J.L.; Bourne, R.B.; McAuley, J.P. Feasibility, effectiveness and costs associated with a web-based follow-up assessment following total joint arthroplasty. J. Arthroplast. 2014, 29, 1723–1728. [Google Scholar] [CrossRef]
- Sharp, D.J.; Hamilton, W. Non-attendance at general practices and outpatient clinics. BMJ 2001, 323, 1081–1082. [Google Scholar] [CrossRef] [PubMed]
- Marsh, J.; Bryant, D.; MacDonald, S.J.; Naudie, D.; Remtulla, A.; McCalden, R.; Howard, J.; Bourne, R.; McAuley, J. Are patients satisfied with a web-based followup after total joint arthroplasty? Clin. Orthop. Relat. Res. 2014, 472, 1972–1981. [Google Scholar] [CrossRef]
- Kirby, D.J.; Fried, J.W.; Buchalter, D.B.; Moses, M.J.; Hurly, E.T.; Cardone, D.A.; Yang, S.S.; Virk, M.S.; Rokito, A.S.; Jazrawi, L.M.; et al. Patient and Physician Satisfaction with Telehealth During the COVID-19 Pandemic: Sports Medicine Perspective. Telemed. J. e-Health 2021, 27, 1151–1159. [Google Scholar] [CrossRef]
- Hurley, E.T.; Haskel, J.D.; Bloom, D.A.; Gonzalez-Lomas, G.; Jazrawi, L.M.; Bosco, J.A., III; Campbell, K.A. The Use and Acceptance of Telemedicine in Orthopedic Surgery During the COVID-19 Pandemic. Telemed. J. e-Health 2020, 27, 657–662. [Google Scholar] [CrossRef]
- Moffet, H.; Tousignant, M.; Nadeau, S.; Mérette, C.; Boissy, P.; Corriveau, H.; Marquis, F.; Cabana, F.; Ranger, P.; Belzile, É.L.; et al. In-Home Telerehabilitation Compared with Face-to-Face Rehabilitation After Total Knee Arthroplasty: A Noninferiority Randomized Controlled Trial. J. Bone Jt. Surg. 2015, 97, 1129–1141. [Google Scholar] [CrossRef]
- Moffet, H.; Tousignant, M.; Nadeau, S.; Mérette, C.; Boissy, P.; Corriveau, H.; Marquis, F.; Cabana, F.; Belzile, É.L.; Ranger, P. Patient satisfaction with in-home telerehabilitation after total knee arthroplasty: Results from a randomized controlled trial. Telemed. e-Health 2017, 23, 80–87. [Google Scholar] [CrossRef]
- Mojica, E.S.; Vasavada, K.; Hurley, E.T.; Lin, C.C.; Buzin, S.; Gonzalez-Lomas, G.; Alaia, M.J.; Strauss, E.J.; Jazrawi, L.M.; Campbell, K.A. Despite Equivalent Clinical Outcomes, Patients Report Less Satisfaction With Telerehabilitation Versus Standard In-Office Rehabilitation After Arthroscopic Meniscectomy: A Randomized Controlled Trial. Arthrosc. Sports Med. Rehabil. 2023, 5, e395–e401. [Google Scholar] [CrossRef] [PubMed]
- Morri, M.; Ruisi, R.; Culcasi, A.; Peccerillo, V. The Effectiveness of Telerehabilitation for Functional Recovery After Orthopedic Surgery: A Systematic Review and Meta-Analysis. Telemed. Rep. 2024, 5, 78–88. [Google Scholar] [CrossRef] [PubMed]
- Greiner, J.J.; Drain, N.P.; Lesniak, B.P.; Lin, A.; Musahl, V.; Irrgang, J.J.; Popchak, A.J. Self-Reported Outcomes in Early Postoperative Management After Shoulder Surgery Using a Home-Based Strengthening and Stabilization System with Telehealth. Sports Health 2023, 15, 599–605. [Google Scholar] [CrossRef] [PubMed]
- Salzler, M.J.; Lin, A.; Miller, C.D.; Herold, S.; Irrgang, J.J.; Harner, C.D. Complications after arthroscopic knee surgery. Am. J. Sports Med. 2014, 42, 292–296. [Google Scholar] [CrossRef] [PubMed]
- Gardner, E.C.; Podbielski, C.; Dunphy, E. Telerehabilitation to Address the Rehabilitation Gap in Anterior Cruciate Ligament Care: Survey of Physical Therapists/Care Providers. Telemed. Rep. 2024, 5, 18–35. [Google Scholar] [CrossRef] [PubMed]
| In-Person (n = 10) | Telerehabilitation (n = 6) | p Value | |
|---|---|---|---|
| Age | 39.6 ± 15.3 | 36.2 ± 10.6 | >0.99 |
| Sex | |||
| Male | 3 (30%) | 2 (33%) | >0.99 |
| Female | 7 (70%) | 4 (67%) | |
| BMI | 28.0 ± 7.6 | 30.3 ± 6.1 | 0.32 |
| KL Grade | |||
| 0 | 7 (70%) | 5 (83%) | >0.99 |
| 1 | 1 (10%) | 0 (0%) | |
| 2 | 2 (20%) | 1 (17%) | |
| Preoperative IKDC score | 51.4 ± 15.2 | 55.4 ± 10.8 | 0.43 |
| In-Person (n = 20) | Telerehabilitation (n = 12) | p Value | |
|---|---|---|---|
| Age | 58.0 ± 10.5 | 57.2 ± 7.8 | 0.58 |
| Sex | |||
| Male | 8 (40%) | 6 (50%) | 0.72 |
| Female | 12 (60%) | 6 (50%) | |
| BMI | 31.0 ± 7.5 | 27.2 ± 5.7 | 0.13 |
| KL Grade | |||
| 0 | 10 (50%) | 7 (58%) | 0.38 |
| 1 | 2 (10%) | 3 (25%) | |
| 2 | 4 (20%) | 2 (17%) | |
| 3 | 4 (20%) | 0 (0%) | |
| Preoperative ASES score | 46.7 ± 18.1 | 38.9 ± 18.9 | 0.46 |
| In-Person (n = 35) | Telerehabilitation (n = 3) | p Value | |
|---|---|---|---|
| Overall satisfaction (%) | 90 ± 16 | 70 ± 27 | 0.21 |
| Confidence with correctly performing exercises (1–5) | 4.6 ± 0.7 | 3.7 ± 1.5 | 0.23 |
| Questions and concerns appropriately addressed (1–5) | 4.8 ± 0.4 | 5.0 ± 0.0 | 0.44 |
| Confidence with return to daily activities (1–5) | 4.5 ± 0.7 | 4.3 ± 0.6 | 0.56 |
| Confidence with return to sports (1–5) | 3.7 ± 1.1 | 2.7 ± 1.5 | 0.17 |
| Availability of equipment and space (1–5) | 4.7 ± 0.6 | 3.7 ± 0.6 | 0.02 * |
| Telerehabilitation-specific questions | |||
| Number of visits | n/a | 3.0 ± 1.7 | n/a |
| Ability to adopt and use new technology (1–5) | n/a | 4.7 ± 0.6 | n/a |
| Video quality of calls (1–5) | n/a | 4.7 ± 0.6 | n/a |
| Cost savings (1–5) | n/a | 4.0 ± 1.0 | n/a |
| Ability to attend more visits (1–5) | n/a | 4.5 ± 0.7 | n/a |
| Would undergo rehabilitation modality again | 34 (97%) | 2 (67%) | 0.15 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vasavada, K.D.; Shankar, D.S.; Avila, A.; Mojica, E.S.; Hurley, E.T.; Lehane, K.; Buzin, S.D.; Oeding, J.F.; Stein, S.M.; Gonzalez-Lomas, G.; et al. Severe Attrition and Poor Satisfaction in Patients Undergoing Telerehabilitation vs. Standard In-Person Rehabilitation after Arthroscopic Rotator Cuff Repairs and Anterior Cruciate Ligament Reconstructions. Surgeries 2024, 5, 627-639. https://doi.org/10.3390/surgeries5030050
Vasavada KD, Shankar DS, Avila A, Mojica ES, Hurley ET, Lehane K, Buzin SD, Oeding JF, Stein SM, Gonzalez-Lomas G, et al. Severe Attrition and Poor Satisfaction in Patients Undergoing Telerehabilitation vs. Standard In-Person Rehabilitation after Arthroscopic Rotator Cuff Repairs and Anterior Cruciate Ligament Reconstructions. Surgeries. 2024; 5(3):627-639. https://doi.org/10.3390/surgeries5030050
Chicago/Turabian StyleVasavada, Kinjal D., Dhruv S. Shankar, Amanda Avila, Edward S. Mojica, Eoghan T. Hurley, Kevin Lehane, Scott D. Buzin, Jacob F. Oeding, Spencer M. Stein, Guillem Gonzalez-Lomas, and et al. 2024. "Severe Attrition and Poor Satisfaction in Patients Undergoing Telerehabilitation vs. Standard In-Person Rehabilitation after Arthroscopic Rotator Cuff Repairs and Anterior Cruciate Ligament Reconstructions" Surgeries 5, no. 3: 627-639. https://doi.org/10.3390/surgeries5030050






