Abstract
The prevalence of overweight and obesity is rising dramatically worldwide, including in Australia. Therefore, the necessity of identifying the risk factors of overweight and obesity is pivotal. The main objective of this study is to investigate the influence of neighbourhood socio-economic circumstances and place of residence on obesity amongst Australian adults. This study has used nationally representative panel data on 183,183 person-year observations from 26,032 unique Australian adults from the Household, Income, and Labour Dynamics in Australia (HILDA). Random-effects logistic regression technique was employed to examine the relationships. The prevalence of overweight and obesity has been found at approximately 34% and 24%, respectively. The most striking result to emerge from the analyses is that adults living in the most socio-economic disadvantaged area were 2.04 times (AOR: 2.04, 95% CI: 1.57–2.65) and adults from regional cities of Australia were 1.71 times (AOR: 1.71, 95% CI: 1.34–2.19) more prone to be obese compared to their healthy counterparts. The prevalence of overweight and obesity is very high among Australian adults, especially those living in disadvantaged neighbourhoods and the regional cities. Unhealthy levels of BMI have costly impacts on the individual, the economy, and the health care system. Therefore, this study emphasises effective weight control strategies that can potentially tackle the obesity epidemic in Australia.
1. Introduction
Globally, obesity is an epidemic concern that imposes substantial health challenges. The prevalence of obesity has risen worldwide substantially irrespective of gender, among men (3% to 11%) and women (6% to 15%) over the last four decades [1]. In 2016, a global estimation reported that around 39% of the world population was overweight, of which 13% suffered from obesity [2]. Besides, more than one in two people in the Organisation for Economic Co-operation and Development (OECD) countries live with higher BMI, i.e., overweight or obesity [3]. The prevalence of obesity nearly doubled from 1980 to 2000 in Australia [4]. A recent study revealed that almost 26% of Australian adults aged 15 years and over were obese in 2019 [5]. Besides, it is predicted that the obesity rate in Australia might increase by 65% within 2025 [6].
The high and growing trends of overweight and obesity is a serious public health concern in Australia since it is associated with chronic diseases [7], disability [8], and poor self-rated physical and mental health outcomes [9]. Besides, there is evidence that obesity has an adverse and statistically significant effect on labour market outcomes in the Australian adult population in terms of job discrimination [10], job dissatisfaction [11], absenteeism [12], and presenteeism [13] in the workplace. Moreover, obesity is accountable for immense economic loss nationally because it adversely affects a country’s resources through the associated inverse health impacts [14]. It increases the risk of permanent and non-permanent work leave, low productivity, disability, and premature death [15]. Further, the probability of developing non-communicable diseases, such as cardiovascular disease, diabetes, asthma, arthritis, and depression, escalates because of overweight and obesity. Additionally, maternal obesity has been found positively associated with fetal and neonatal deaths [16]. Many of these non-communicable diseases could be prevented if healthy weight status could be maintained as obesity is highly preventable [2]. Interestingly, health-promoting behaviour in the lifestyle influences the weight status [17]. This circumstance induces a wide range of future research that will identify behavioural factors of obesity.
Earlier studies conducted in Australia focused on overweight and obesity trends that covered only specific dimensions. For example, prediction of higher BMI trends [6,18,19], costs of obesity [20], prevalence and factors of child obesity [21,22], and modelling for obesity prevention [23,24] are the most prominent. However, some cross-sectional studies executed outside of Australia determined the risk indicators of obesity [25,26,27,28]. These studies outlined that age [26,27], gender [26,27], marital status [26,28], residence [27,28], education [26,28], alcohol intake [28], physical activity [26], and ethnicity [26] are significant risk factors of overweight and obesity.
In the existing evidence, no study exclusively covers the influence of location, socio-economic circumstances, and behavioural parameters on weight status among Australian adults. Besides, identifying risk factors of pre-obesity and obesity based on longitudinal data assists a more precise approach, but previous efforts in this regard are lacking. Yet, a recent study conducted on longitudinal data found that ethnicity, residence, education, and age significantly impact weight status among Chinese adults [29]. However, that study ignores some important behavioural factors along with socio-economic areas.
Due to the lack of evidence that solves these problems, this study endeavours to determine the significance of location associated with obesity in Australia utilising longitudinal data. The present study aims to delineate up-to-date prevalence and examine the influence of location on weight status after adjusting and lifestyle factors. To attain the objective, this study systematically searches the answer to the following research question: Do neighbourhood socio-economic circumstances and place of residence impact an adult’s weight status after controlling other risk factors? Evidence on these might help designing multidimensional health programs that will control adults’ weight status and prevent higher BMI problems in Australia.
2. Methods
2.1. Data Sources
This study was conducted through 14 waves (waves 6 to 19) from the Household, Income, and Labour Dynamics in Australia (HILDA) survey spanning 2006 to 2019. It is a nationally representative household-based longitudinal survey of Australia covering a wide range of information about family, income, and the labour market. The survey was initiated with a large household sample in 2001 through a multistage sampling approach and re-sampled in 2011. The primary sampling unit, collection districts, was sampled by probability proportional to size. In the survey, adults aged ≥15 years have attended the face-to-face interviews and provided data by filling self-completed questionnaires. More about the data collection methodology has been mentioned elsewhere [30].
2.2. Sample Size
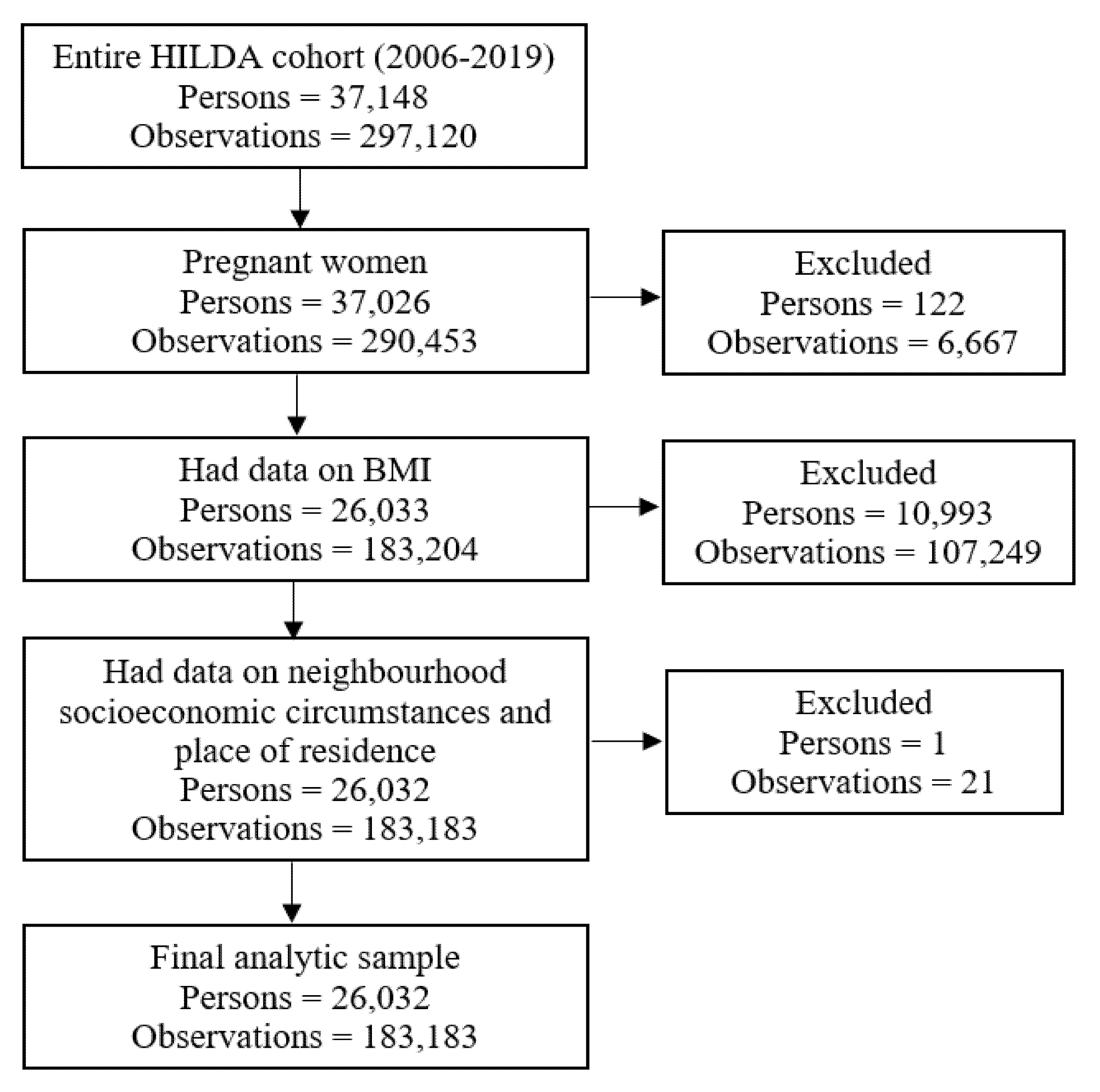
Figure 1 displays the steps for obtaining the final analytic data. Individual data points were excluded using the following criteria: pregnant women during the survey, missing data on body mass index (BMI) and primary exposures (neighbourhood socio-economic circumstances and place of residence). Utilising the exclusion criteria, this study included 183,183 yearly observations from 26,032 unique adults for the sub-sample analyses.
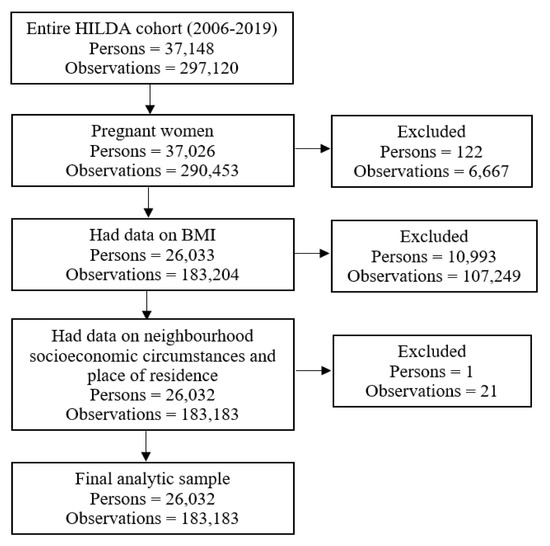
Figure 1.
Sample selection procedure.
2.3. Outcome Measurement
Body mass index (BMI) is the primary outcome variable of the present study. It was calculated using self-reported height and weight using the following formula: weight (in kilograms) divided by height (in metres squared). For the analysis purpose, BMI was categorised into four groups following World Health Organization recommended BMI cut-off points: <18.50 (underweight), 18.50–24.99 (normal/healthy weight), 25.00–29.99 (overweight), and ≥30 (obese) [2]. Overweight and obesity prevalence were calculated for the population aged 15 years and over living in Australia from 2006–2019.
2.4. Exposure Variables
The key exposures of the present study are neighbourhood socio-economic circumstances and place of residence. This study used the Index of Economic Resources as the proxy of neighbourhood socio-economic circumstances that was derived from Socio-economic Indexes for Areas (SEIFA). The SEIFA measure estimates the definite value and ranks it from socio-economic disadvantaged to advantaged areas [31]. Financial variables, mainly income and wealth, are considered in this regard to determine relative socio-economic advantage and disadvantage [31]. Thus, low index scores indicate most or more disadvantaged areas, and high index scores indicate more or most advantaged areas. More specifically, a low index score suggests that an individual living in a particular place has a comparative lack of access to economic resources and vice versa.
The other exposure, place of residence, was categorised as major cities of Australia, regional cities (inner regional Australia and outer regional Australia), and remote areas (remote or very remote areas of Australia).
2.5. Explanatory Variables
Authors selected risk factors associated with overweight and obesity based on existing evidence [5,25,26,28,32,33]. Demographic variables include age (15–24, 25–34, 35–44, 45–54, 55–64, and ≥65 years); gender (male and female); marital status (cohabitating and non-cohabitating) and ethnic origin (not of Indigenous origin; and Aboriginal, or Torres Strait Islander or both). Socio-economic variables include education (year 12 and below, professional qualifications, and university qualifications), household yearly disposable income (Quantile 1 [lowest], Quantile 2, Quantile 3, Quantile 4, and Quantile 5 [highest]), and labour force status (employed, unemployed, and not in the labour force).
Behavioural variables were smoking status (never smoked, ex-smoker, and current smoker), alcohol consumption (never drank, ex-drinker, only rarely to 4 days per week, and over four days per week), and physical activity (below the recommended level and recommended level).
2.6. Statistical Analyses
The study outlined participants’ characteristics in frequency (n) and percentages (%). Following this, the Chi-square test was deployed to examine the bivariate relationship between obesity and particular covariates (results were not reported). Finally, the study adopted the longitudinal random-effects logistic regression technique to identify the between-person effects in the relationship between neighbourhood socio-economic circumstance and place of residence with overweight and obesity. Central to the analyses reported in this study is the estimation of the random-effects logistic regression model in the following format:
Here, BMI is a categorical variable wherein healthy weight individual is the reference group, and overweight and obese adults are the counterparts. X is a vector of explanatory variables that might influence the weight status of the adults. This study includes neighbourhood socio-economic circumstances, place of residence, age, gender, civil status, education, household yearly disposable income, ethnicity, smoking status, alcohol consumption, and physical activity as explanatory variables. Covariates having a p-value of ≤0.05 in the bivariate logistic regression were entered into the longitudinal random-effects logistic regression model. Finally, the adjusted odds ratio (AOR) was reported to interpret the findings of the study. STATA version 17.0 (Stata SE 17, College Station, TX: StataCorp LLC, USA) was used to accomplish the analysis of this study.
3. Results
The characteristics of the study participants in the baseline and final waves and the pooled characteristics of all waves are demonstrated in Table 1. The results report Australian adults’ obesity, economic resources and residence, and socio-economic and lifestyle characteristics of the 183,183 yearly observations from 26,032 unique respondents. The proportion of obese people reported in the baseline and final waves were around 21% and 27%, respectively. Table 1 also demonstrates that of the pooled sample of all waves, there was an equal distribution in all age groups, more than half were female (53%), almost 59% were cohabitating, approximately one-fourth had university qualifications (25%), nearly two-thirds were employed (64%), most were not of indigenous origin (97%) and were living in major cities (66%). Of the lifestyle characteristics, 18% were current smokers, 15% drank alcohol over four days a week, and 66% performed physical activity below the recommended level.

Table 1.
Distribution of the analytic sample: baseline, final and pooled across all waves (person = 26,032, observation = 183,183).
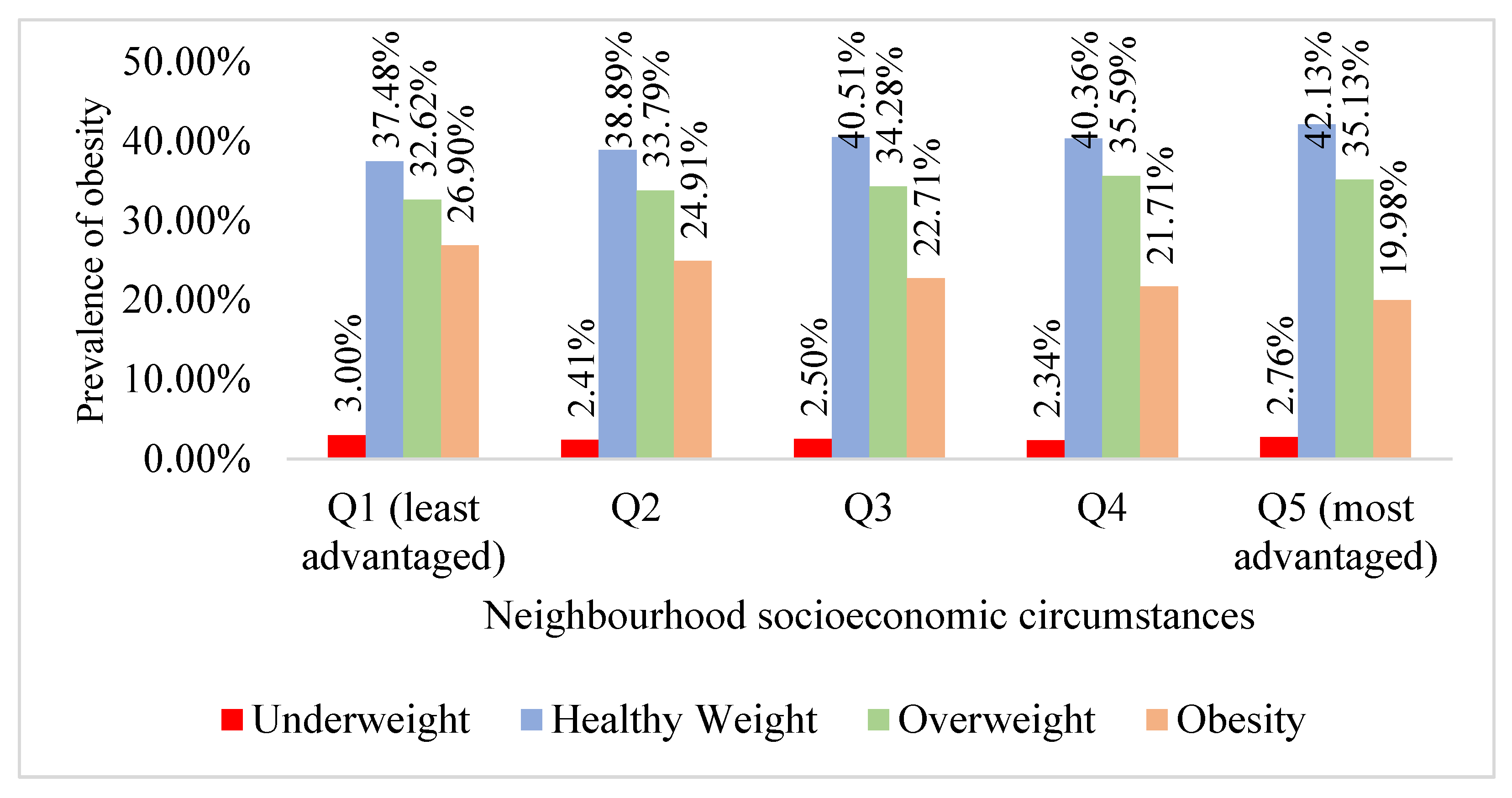
Figure 2 illustrates the distribution of weight status by neighbourhood socio-economic circumstances. The highest (27%) and second-highest (25%) prevalence of obesity were among the most deprived quartiles, Q1 and Q2, respectively. In reverse, healthy weight adults were more prevalent among more affluent populations, 40% in Q4 and 42% in Q5 socio-economic groups.
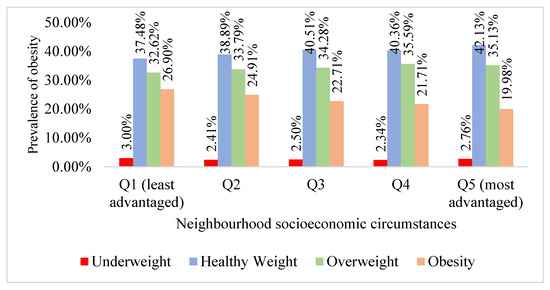
Figure 2.
Distribution of weight status by neighbourhood socio-economic circumstances, 26,032 persons, 183,183 observations.
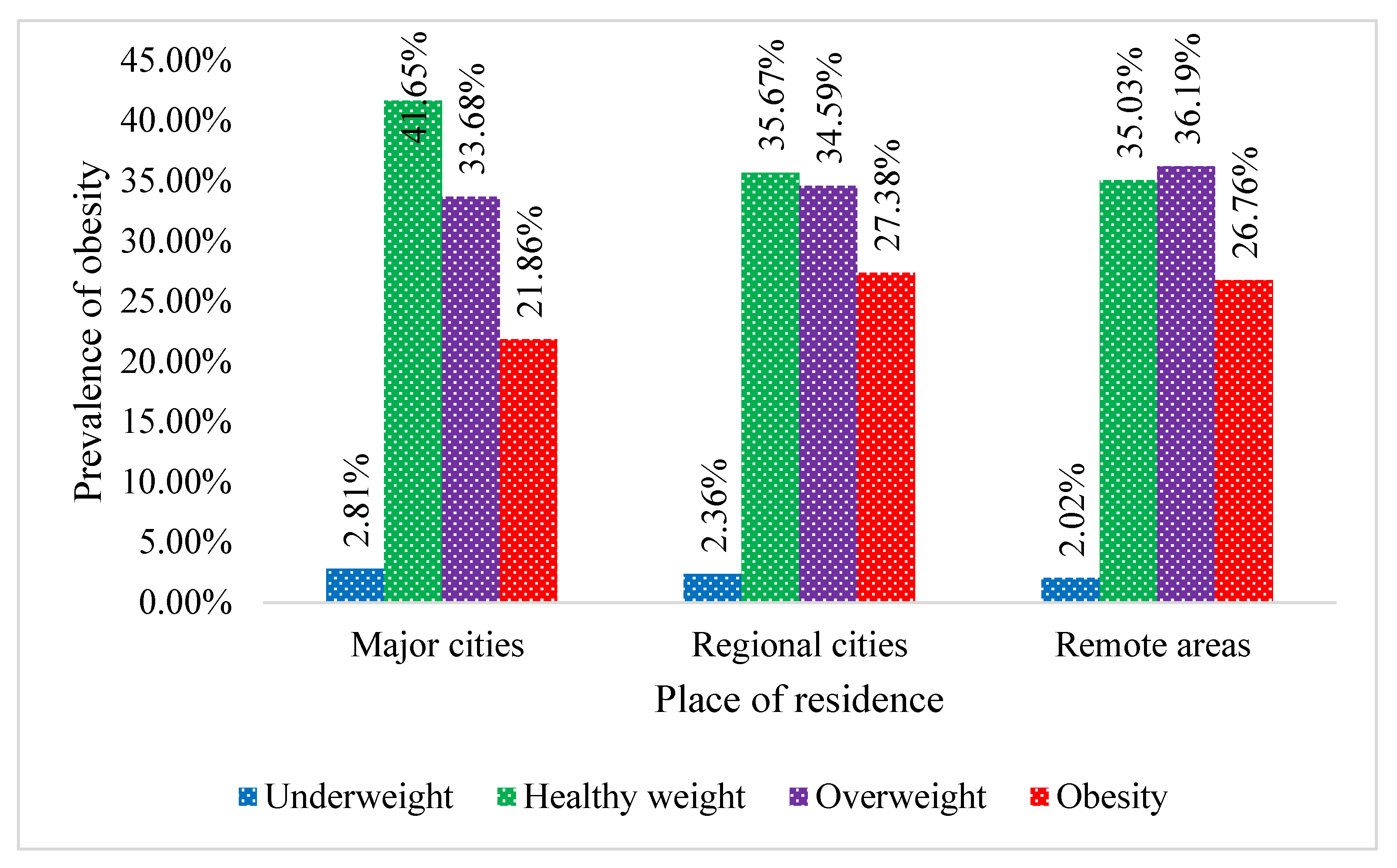
Figure 3 also presents the distribution of obesity status by place of residence. The prevalence of both overweight and obesity was found higher among inhabitants living in regional cities and remote areas than the residents of major cities. The highest prevalence of obesity (27%) was among peoples of regional cities, while the highest prevalence of overweight was (36%) observed among the residents of remote areas.
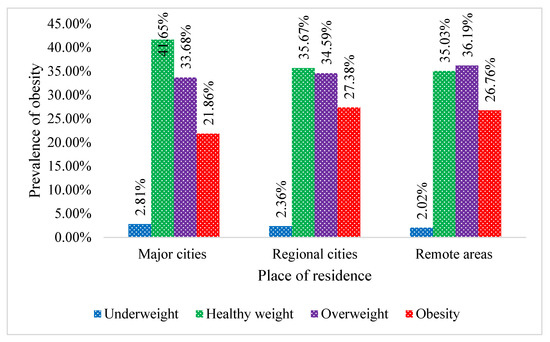
Figure 3.
Distribution of weight status by place of residence, 26,032 persons, 183,183 observations.
Table 2 presents the multivariate models that explored the association between neighbourhood socio-economic circumstances, place of residence, and obesity after adjusting for confounders. The results showed that compared to the respondents of affluent socio-economic status (Q5), the odds of being obese were higher among the participant of less affluent or most deprived groups, that is, the adults belonged to Q3, Q2 and Q1 of the socio-economic groups. The probability of being obese was 2.04 times higher (OR: 2.04, 95% CI: 1.57–2.65) among the participants of the most deprived adults (Q1), compared to the wealthiest adults (Q5) in the Australian society. The results from the random-effects logistic models also represent that the odds of being obese were 1.71 times higher (OR: 1.71, 95% CI: 1.34–2.19) among the participants inhabiting the regional cities compared to the inhabitants of major cities.

Table 2.
Adjusted random-effect logistic regression results for the between-person difference in obesity due to neighbourhood socio-economic circumstances and place of residence.
4. Discussion
The current study demonstrates the prevalence of overweight and obesity and its association with the neighbourhood socio-economic circumstances and place of residence among Australian adults. This study has been undertaken through the longitudinal random-effect logistic regression technique and the most recently available longitudinal data from the HILDA survey. This study found that the prevalence of overweight and obesity is very high among Australian adults, especially those living in disadvantaged neighbourhoods and the regional cities. The results also showed that neighbourhood socio-economic circumstances and place of residence are significantly associated with obesity.
The present study found that disadvantaged neighbourhood is a statistically significant risk factor of being obese. It indicates that adults from most disadvantaged neighbourhoods are more likely to be obese than their peers living in the most advantaged areas. This finding is consistent with existing evidence on the association between disadvantaged neighbourhoods and obesity [32,34]. Many studies have also reported that the prevalence of higher BMI is extensive amongst low-income groups in developed countries [32,35,36,37]. The possible reason for the socio-economic disparity in weight status is that low-income people usually reside in disadvantaged areas and cannot afford healthier diets. Besides, people from disadvantaged neighbourhoods generally lead an unhealthy lifestyle, such as eating non-nutrient and energy deficient foods [38]. Another possible reason could be that people from disadvantaged neighbourhoods perform lower levels of physical activity [32].
Place of residence is another crucial variable that is associated with increased levels of obesity. In this study, adults residing in regional (inner and outer) or remote areas had a higher risk of being overweight or obese compared to adults living in major cities in Australia. This finding aligns with previous evidence suggesting that adults living in regional and rural areas are more likely to be obese [5,39]. An earlier study from developing countries contexts also reported that place of residence is positively associated with obesity [40]. Higher BMI among adults in rural or remote territories might be due to deprivation related to education, income, and health services [5,41].
The present study findings emphasised diverse strategies to control the rapidly growing overweight and obesity prevalence in Australia. This study suggests forming healthier places to ensure healthy weight status for adults living in socioeconomically disadvantaged, rural, and remote areas. The current study also emphasises implementing a primary care program to reduce weight gain risk by increasing activity levels and consuming healthy diets (increasing fruit and vegetable intake and minimising alcohol consumption). These suggestions are identical with the goals of the Australian Health and Wellbeing Strategic Framework 2017–2026, which has also recommended constructing a healthy environment for individuals to stay healthy.
This study contributes to the literature in several ways. This study first outlined the distribution of Australia’s adult overweight and obesity across different neighbourhoods and place of residence. The study’s major strength is that it offered an assembled update on the impact of neighbourhood socio-economic circumstances and place of residence on higher BMI in Australian adults after adjusting for demographic, socio-economic circumstances, and health-related behaviour. Further, this study used the most recent available data from an extensive, nationally representative longitudinal survey (Wave 6–19 of the HILDA survey) to determine the association.
This study has some drawbacks that should be mentioned. Firstly, this study has used self-reported BMI, which may underestimate or overestimate the results. Secondly, causality cannot be drawn since this study performed analyses on unbalanced longitudinal data. Thirdly, the actual distribution of overweight and obesity might be underestimated in the total population since a large portion of the study participants were from major cities. However, the study findings are in line with other survey findings of Australia.
5. Conclusions
This study revealed the prevalence of overweight and obesity by the respondents’ neighbourhoods socio-economic circumstances and type of residence, along with the respective contribution of these risk factors to individuals exposed to weight gain. The results showed that the prevalence of overweight and obesity is higher among adults living in regional cities or remote areas and people living in disadvantaged neighbourhoods. The high prevalence of obesity imposes a substantial cost to the individuals involved and the Australian healthcare system. Increased prevalence of overweight and obesity may worsen if no policy interventions can be implemented to reverse the trend and overcome the situation. Implementing strategies and interventions to reduce the prevalence of overweight and obesity requires evidence to make it fruitful. This study may provide evidence to health system decision-makers in Australia to identify the “hot spots” and the related risk factors of overweight and obesity. The authors suggest that interventions should be tailored to consider the needs of socioeconomically and geographically disadvantaged adults who are at the most significant risk of excessive weight gain. The authors envisage that the study findings may contribute to the formulation of context-specific interventions or preventive efforts to reduce the current levels of weight gain and reduce the burden of obesity in the future in Australian society.
Author Contributions
Conceptualization, S.A.K., R.C. and R.H. (Rubayyat Hashmi); Data curation, S.A.K. and B.A.; Formal analysis, S.A.K. and K.A.; Funding acquisition, R.H. (Rubayyat Hashmi); Investigation, S.A.K., R.H. (Rezwanul Haque) and B.A.; Methodology, S.A.K., B.A. and K.A.; Resources, R.H. (Rezwanul Haque) and B.A.; Software, R.H. (Rubayyat Hashmi); Supervision, R.H. (Rezwanul Haque) and R.H. (Rubayyat Hashmi); Validation, R.C.; Visualization, N.J.S., R.H. (Rezwanul Haque) and R.C.; Writing—original draft, N.J.S. and K.A.; Writing—review & editing, N.J.S., R.H. (Rezwanul Haque), B.A., R.C., R.H. (Rubayyat Hashmi) and K.A. All authors have read and agreed to the published version of the manuscript.
Funding
The authors received no specific funding for this work.
Institutional Review Board Statement
The HILDA survey commenced in 2001 and since then has been conducted annually following the University of Melbourne’s ethical guidelines. This research project has been approved by the Human Research Ethics Committee of The University of Melbourne. The ethics ID number of the research project (HILDA Survey) is 1647030. This paper uses unit record data from the HILDA conducted by the Australian Government Department of Social Services (DSS). This study did not require ethical approval as the analysis used only de-identified existing unit record data from the HILDA survey.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data used for the study were collected from the Melbourne Institute of Applied Economic and Social Research. There are some restrictions on this data, and it is not available to the public. Those interested in accessing this data should contact the Melbourne Institute of Applied Economic and Social Research, the University of Melbourne, VIC 3010, Australia.
Acknowledgments
The authors wish to thank the Melbourne Institute of Applied Economic and Social Research for providing the HILDA data set. This paper uses unit record data from the HILDA conducted by the Australian Government Department of Social Services (DSS). The findings and views reported in this paper, however, are those of the authors and should not be attributed to the Australian Government, DSS, or any of DSS contractors or partners. DOI:10.26193/OFRKRH, ADA Dataverse, V2.
Conflicts of Interest
The authors declare that they have no conflict of interest.
Abbreviations
| BMI | Body Mass Index |
| OR | Odds Ratio |
| CI | Confidence Interval |
| HILDA | Household, Income and Labour Dynamics in Australia |
| SEIFA | Socio-Economic Indexes for Areas |
References
- Jaacks, L.M.; Vandevijvere, S.; Pan, A.; McGowan, C.J.; Wallace, C.; Imamura, F.; Mozaffarian, D.; Swinburn, B.; Ezzati, M. The obesity transition: Stages of the global epidemic. Lancet Diabetes Endocrinol. 2019, 7, 231–240. [Google Scholar] [CrossRef]
- World Health Organization Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 18 April 2021).
- OECD Obesity Update 2017. OECD Updat. Rep. 2017, 13, 331–341.
- Cameron, A.J.; Welborn, T.A.; Zimmet, P.Z. Overweight and obesity in Australia: The 1999–2000 Australian Diabetes, Obesity and Lifestyle Study (AusDiab). Med. J. Aust. 2004, 180, 418. [Google Scholar] [CrossRef] [PubMed]
- Keramat, S.A.; Alam, K.; Al-Hanawi, M.K.; Gow, J.; Biddle, S.J.H.; Hashmi, R. Trends in the prevalence of adult overweight and obesity in Australia, and its association with geographic remoteness. Sci. Rep. 2021, 11, 11320. [Google Scholar] [CrossRef]
- Walls, H.L.; Magliano, D.J.; Stevenson, C.E.; Backholer, K.; Mannan, H.R.; Shaw, J.E.; Peeters, A. Projected progression of the prevalence of obesity in Australia. Obesity 2012, 20, 872–878. [Google Scholar] [CrossRef] [PubMed]
- Keramat, S.A.; Alam, K.; Rana, R.H.; Chowdhury, R.; Farjana, F.; Hashmi, R.; Gow, J.; Biddle, S.J.H. Obesity and the risk of developing chronic diseases in middle-aged and older adults: Findings from an Australian longitudinal population survey, 2009–2017. PLoS ONE 2021, 16, e0260158. [Google Scholar] [CrossRef]
- Keramat, S.A.; Alam, K.; Sathi, N.J.; Gow, J.; Biddle, S.J.H.; Al-Hanawi, M.K. Self-reported disability and its association with obesity and physical activity in Australian adults: Results from a longitudinal study. SSM-Popul. Health 2021, 14, 100765. [Google Scholar] [CrossRef]
- Keramat, S.A.; Alam, K.; Ahinkorah, B.O.; Islam, M.S.; Islam, M.I.; Hossain, M.Z.; Ahmed, S.; Gow, J.; Biddle, S.J. Obesity, Disability and Self-Perceived Health Outcomes in Australian Adults: A Longitudinal Analysis Using 14 Annual Waves of the HILDA Cohort. Clin. Outcomes Res. 2021, 13, 777–788. [Google Scholar] [CrossRef]
- Keramat, S.A.; Alam, K.; Rana, R.H.; Shuvo, S.D.; Gow, J.; Biddle, S.J.H.; Keating, B. Age and gender differences in the relationship between obesity and disability with self-perceived employment discrimination: Results from a retrospective study of an Australian national sample. SSM-Popul. Health 2021, 16, 100923. [Google Scholar] [CrossRef]
- Keramat, S.A.; Alam, K.; Gow, J.; Biddle, S.J.H. Obesity, Long-Term Health Problems, and Workplace Satisfaction: A Longitudinal Study of Australian Workers. J. Community Health 2020, 45, 288–300. [Google Scholar] [CrossRef]
- Keramat, S.A.; Alam, K.; Gow, J.; Biddle, S.J.H. Gender differences in the longitudinal association between obesity, and disability with workplace absenteeism in the Australian working population. PLoS ONE 2020, 15, e0233512. [Google Scholar] [CrossRef]
- Keramat, S.A.; Alam, K.; Gow, J.; Biddle, S.J.H. A longitudinal exploration of the relationship between obesity, and long term health condition with presenteeism in Australian workplaces, 2006–2018. PLoS ONE 2020, 15, e0238260. [Google Scholar] [CrossRef] [PubMed]
- Mayosi, B.M.; Flisher, A.J.; Lalloo, U.G.; Sitas, F.; Tollman, S.M.; Bradshaw, D. The burden of non-communicable diseases in South Africa. Lancet 2009, 374, 934–947. [Google Scholar] [CrossRef]
- Goettler, A.; Grosse, A.; Sonntag, D. Productivity loss due to overweight and obesity: A systematic review of indirect costs. BMJ Open 2017, 7, e014632. [Google Scholar] [CrossRef] [Green Version]
- Haque, R.; Keramat, S.A.; Rahman, S.M.; Mustafa, M.U.R.; Alam, K. Association of maternal obesity with fetal and neonatal death: Evidence from South and South-East Asian countries. PLoS ONE 2021, 16, e0256725. [Google Scholar] [CrossRef]
- Tucker, C.M.; Butler, A.; Kaye, L.B.; Nolan, S.E.M.; Flenar, D.J.; Marsiske, M.; Bragg, M.; Hoover, E.; Daly, K. Impact of a Culturally Sensitive Health Self-Empowerment Workshop Series on Health Behaviors/Lifestyles, Body Mass Index, and Blood Pressure of Culturally Diverse Overweight/Obese Adults. Am. J. Lifestyle Med. 2014, 8, 122–132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haby, M.M.; Markwick, A.; Peeters, A.; Shaw, J.; Vos, T. Future predictions of body mass index and overweight prevalence in Australia, 2005–2025. Health Promot. Int. 2012, 27, 250–260. [Google Scholar] [CrossRef] [Green Version]
- Hayes, A.J.; Lung, T.W.C.; Bauman, A.; Howard, K. Modelling obesity trends in Australia: Unravelling the past and predicting the future. Int. J. Obes. 2017, 41, 178–185. [Google Scholar] [CrossRef]
- van Baal, P.H.M.; Polder, J.J.; de Wit, G.A.; Hoogenveen, R.T.; Feenstra, T.L.; Boshuizen, H.C.; Engelfriet, P.M.; Brouwer, W.B.F. Lifetime Medical Costs of Obesity: Prevention No Cure for Increasing Health Expenditure. PLoS Med. 2008, 5, e29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olds, T.S.; Tomkinson, G.R.; Ferrar, K.E.; Maher, C.A. Trends in the prevalence of childhood overweight and obesity in Australia between 1985 and 2008. Int. J. Obes. 2010, 34, 57–66. [Google Scholar] [CrossRef] [Green Version]
- Wolfenden, L.; Hardy, L.L.; Wiggers, J.; Milat, A.J.; Bell, C.; Sutherland, R. Prevalence and socio-demographic associations of overweight and obesity among children attending child-care services in rural and regional Australia. Nutr. Diet. 2011, 68, 15–20. [Google Scholar] [CrossRef]
- Sacks, G.; Veerman, J.L.; Moodie, M.; Swinburn, B. Traffic-light nutrition labelling and junk-food tax: A modelled comparison of cost-effectiveness for obesity prevention. Int. J. Obes. 2011, 35, 1001–1009. [Google Scholar] [CrossRef] [Green Version]
- Veerman, J.L.; Barendregt, J.J.; Forster, M.; Vos, T. Cost-Effectiveness of Pharmacotherapy to Reduce Obesity. PLoS ONE 2011, 6, e26051. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cois, A.; Day, C. Obesity trends and risk factors in the South African adult population. BMC Obes. 2015, 2, 42. [Google Scholar] [CrossRef] [Green Version]
- Gong, S.; Wang, K.; Li, Y.; Alamian, A. Geographic differences in obesity prevalence and its risk factors among Asian Americans: Findings from the 2013–2014 California Health Interview Survey. Sci. Rep. 2018, 8, 12510. [Google Scholar] [CrossRef]
- Hu, L.; Huang, X.; You, C.; Li, J.; Hong, K.; Li, P.; Wu, Y.; Wu, Q.; Wang, Z.; Gao, R.; et al. Prevalence of overweight, obesity, abdominal obesity and obesity-related risk factors in southern China. PLoS ONE 2017, 12, e0183934. [Google Scholar] [CrossRef] [PubMed]
- Samouda, H.; Ruiz-Castell, M.; Bocquet, V.; Kuemmerle, A.; Chioti, A.; Dadoun, F.; Kandala, N.B.; Stranges, S. Geographical variation of overweight, obesity and related risk factors: Findings from the European Health Examination Survey in Luxembourg, 2013–2015. PLoS ONE 2018, 13, e0197021. [Google Scholar] [CrossRef]
- He, Y.; Pan, A.; Wang, Y.; Yang, Y.; Xu, J.; Zhang, Y.; Liu, D.; Wang, Q.; Shen, H.; Zhang, Y.; et al. Prevalence of overweight and obesity in 15.8 million men aged 15–49 years in rural China from 2010 to 2014. Sci. Rep. 2017, 7, 5012. [Google Scholar] [CrossRef] [Green Version]
- Wooden, M.; Freidin, S.; Watson, N. The Household, Income and Labour Dynamics in Australia (HILDA) Survey: Wave 1. Aust. Econ. Rev. 2002, 35, 339–348. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. Socio-Economic Indexes for Areas (SEIFA)—2016; ABS: Canberra, Australia, 2018.
- Keramat, S.A.; Alam, K.; Gow, J.; Biddle, S.J.H. Impact of Disadvantaged Neighborhoods and Lifestyle Factors on Adult Obesity: Evidence From a 5-Year Cohort Study in Australia. Am. J. Health Promot. 2021, 35, 28–37. [Google Scholar] [CrossRef]
- Keramat, S.A.; Alam, K.; Gow, J.; Biddle, S.J.H. Job-Related Characteristics and Obesity in Australian Employees: Evidence From a Longitudinal Nationally Representative Sample. Am. J. Health Promot. 2020, 34, 729–739. [Google Scholar] [CrossRef]
- Menigoz, K.; Nathan, A.; Heesch, K.C.; Turrell, G. Neighbourhood disadvantage, geographic remoteness and body mass index among immigrants to Australia: A national cohort study 2006–2014. PLoS ONE 2018, 13, e0191729. [Google Scholar] [CrossRef] [Green Version]
- Kuntz, B.; Lampert, T. Socioeconomic Factors and Obesity. Dtsch. Aerzteblatt Online 2010, 107, 517–523. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, E.M. Why Do College Graduates Behave More Healthfully Than Those Who Are Less Educated? J. Health Soc. Behav. 2017, 58, 291–306. [Google Scholar] [CrossRef] [PubMed]
- Ogden, C.L.; Fakhouri, T.H.; Carroll, M.D.; Hales, C.M.; Fryar, C.D.; Li, X.; Freedman, D.S. Prevalence of Obesity Among Adults, by Household Income and Education—United States, 2011–2014. MMWR Morb. Mortal. Wkly. Rep. 2017, 66, 1369–1373. [Google Scholar] [CrossRef]
- Kalkunte, S.S.; Mselle, T.F.; Norris, W.E.; Wira, C.R.; Sentman, C.L.; Sharma, S. Vascular Endothelial Growth Factor C Facilitates Immune Tolerance and Endovascular Activity of Human Uterine NK Cells at the Maternal-Fetal Interface. J. Immunol. 2009, 182, 4085–4092. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Australian Institute of Health and Welfare. Australia’ s Health 2018; Cat. No. AUS 222; AIHW: Canberra, Australia, 2018.
- Ahmad, K.; Khanam, T.; Keramat, S.A.; Islam, M.I.; Kabir, E.; Khanam, R. Interaction between the place of residence and wealth on the risk of overweight and obesity in Bangladeshi women. PLoS ONE 2020, 15, e0243349. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. Rural & Remote Health; Cat. No: PHE 255; AIHW: Canberra, Australia, 2017.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).