Lipodystrophies from Insulin Injection: An Update of the Italian Consensus Statement of AMD-OSDI Study Group on Injection Technique
Abstract
:1. Introduction
- A preventive search for LH to avoid injecting insulin into them;
- Constant injection site rotation ensuring a distance of at least 1 cm between two successive injections and utilization of the entire surface of injection areas identified in the abdomen, external and rear sides of the arms, upper external side of the thighs and buttocks;
- Single use of each pen needle (1 needle = 1 injection);
- Choice of 32 G × 4 mm needles even in overweight and obese subjects;
- Proper insulin storage;
- Ice-cold insulin avoidance;
- No skin massage after the injection;
- No injection through clothing;
- Thorough hand and skin hygiene;
- No pinch maneuver or acute angle needle inclination at the time of injection.
- Are you sure the explanations you gave to your patient when prescribing insulin were exhaustive and sufficiently clear to let him/her understand how to correctly perform injections?
- Did you explain to him/her how the insulin pen works?
- Did you show him/her how to insert the needle on top of the pen?
- Did you show him/her how to hold the pen at the time of injection?
- Did you provide him/her a chart or cartoon displaying clear indications of the best injection site selection?
- Did you give him/her clear information concerning the importance of selecting the correct needle length and inserting it onto the skin surface at a correct angle?
- Did you tell him/her how to store insulin and avoid ice-cold insulin injections?
- Did you tell him/her that too long needles pose him/her a risk of reaching the muscle tissue below the subcutaneous layer in the case of thin areas, and intramuscular injections make insulin absorption faster, thus often causing unexpected hypoglycemia?
- Did you take enough time to show him/her the best way to perform injection site rotation within separate skin areas?
- Did you explain to him/her the appropriate distance to keep among injection sites?
- Did you stress the importance of pressing the pen button for at least 10 s before taking the pen out of the skin enough?
- Did you repeatedly mention that disposable needles are to be used only once and then discarded?
- Did you remind him/her that, when repeatedly using the same injection site, he/she might give rise to skin nodules causing insulin absorption abnormalities with consequent large blood glucose variability, poor diabetes control, and ever-increasing insulin?
- Did you explain to him/her, especially when insulin-treated for a long time, that it is necessary to self-palpate the skin area in search of nodules and to avoid them if present?
- Did you make sure that, besides understanding all the information pills provided, he/she has taken the habit of correctly putting into practice the teachings you have told and shown so far?
2. Summary Points
- Lipohypertrophy (LH) due to incorrect injection technique is widespread, underdiagnosed, and mainly ignored by clinicians.
- We have national and international recommendations on correct injection techniques, but LH is, nevertheless, ubiquitous.
- A call to action is needed to implement the culture of LH and its complications.
- Recommendations must take into account advances in technology, and new research is needed to prove the usefulness of the new devices.
- It is necessary to implement structured clinical diagnostic paths for the identification of LH, especially in care settings without ultrasonography, an unsuitable and expensive method for population and screening studies.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gentile, S.; Guarino, G.; Satta, E.; Romano, C.; Strollo, F. Why 100-years after the discovery of insulin and the appearance of insulin-induced lipodystrophy: Are we still struggling with this nasty complication? Diabetes Res. Open. J. 2022, 8, 23–29. [Google Scholar] [CrossRef]
- Blanco, M.; Hernández, M.T.; Strauss, K.W.; Amaya, M. Prevalence and risk factors of lipohypertrophy in insulin-injecting patients with diabetes. Diabetes Metab. 2013, 39, 445–453. [Google Scholar] [CrossRef]
- Gentile, S.; Strollo, F.; De Rosa, N. Injection-Related Local Side Effects in the Treatment of Diabetes Mellitus: A Methodological Approach and Possible Solutions. Consensus Statement of AMD-OSDI Study Group on Injection Technique. In e-Book Diabetes Complications. 2016. Available online: https://www.semanticscholar.org/paper/Gr-upSM-Injection-Related-Local-Side-Effects-in-the-Sandro-Felice/d29d49e463d1dbe98bde0089177870f2080bc46c (accessed on 3 February 2023).
- Gentile, S.; Guarino, G.; Della Corte, T.; Marino, G.; Satta, E.; Pasquarella, M.; Romano, C.; Alfrone, C.; Strollo, F.; AMD-OSDI Study Group on Injection Technique, Nefrocenter Research and Nyx Start-Up. Role of structured education in reducing lypodistrophy and its metabolic complications in insulin-treated people with type 2 diabetes: A randomized multicenter case-control study. Diabetes Ther. 2021, 12, 1379–1398. [Google Scholar] [CrossRef] [PubMed]
- Shen, M.; Shi, Y.; Zheng, S.; Fan, H.; Xu, J.; Yang, T. A systematic survey of physicians’ insights into lipohypertrophy. Front. Public Health 2021, 9, 738179. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Lin, L.; Wang, W.; Hong, J.; Zeng, H. Insulin-related lipohypertrophy: Ultrasound characteristics, risk factors, and impact of glucose fluctuations. Endocrine 2022, 75, 768–775. [Google Scholar] [CrossRef] [PubMed]
- Deng, N.; Zhang, X.; Zhao, F.; Wang, Y.; He, H. Prevalence of lipohypertrophy in insulin-treated diabetes patients: A systematic review and meta-analysis. J. Diabetes Investig. 2017, 9, 536–543. [Google Scholar] [CrossRef]
- Gentile, S.; Guarino, G.; Della Corte, T.; Marino, G.; Satta, E.; Pasquarella, M.; Romano, C.; Alfrone, C.; Giordano, L.; Loiacono, F.; et al. The Durability of an Intensive, Structured Education-Based Rehabilitation Protocol for Best Insulin Injection Practice: The ISTERP-2 Study. Diabetes Ther. 2021, 12, 2557–2569. [Google Scholar] [CrossRef]
- Gentile, S.; Guarino, G.; Marino, G.; Strollo, F. Risk factors for severe hypoglycemia in people with insulin-treated diabetes: Are we sure we took into account all variables involved? Nutr. Metab. Cardiovasc. Dis. 2017, 27, 415–416. [Google Scholar] [CrossRef]
- Gentile, S.; Satta, E.; Guarino, G.; Romano, C.; Maffettone, A.; Heinke, E.E.; Donnarumma, E.; Castellano, R.; Izzo, S.; Manzo, I.; et al. A Journey Through Guidelines, Consensus, Curriculum of Educators and Clinical Practice on Insulin-Induced Skin Lipohypertrophy: From the Earth to the Moons. Med. Res. Arch. 2022, 10. [Google Scholar] [CrossRef]
- Gentile, S.; Strollo, F.; Guarino, G. Why are so huge differences reported in the occurrence rate of skin lipohypertrophy? Does it depend on method defects or on lack of interest? Diabetes Metab. Syndr. 2019, 13, 682–686. [Google Scholar] [CrossRef]
- Strollo, F.; Satta, E.; Gentile, S. Insulin Injection-Related Skin Lipodystrophies: Blemish or Pathology? Diabetology 2022, 3, 615–619. [Google Scholar] [CrossRef]
- Gentile, S.; Guarino, G.; Giancaterini, A.; Guida, P.; Strollo, F.; AMD-OSDI Italian Injection Technique Study Group. A suitable palpation technique allows to identify skin lipohypertrophic lesions in insulin-treated people with diabetes. Springerplus 2016, 5, 563. [Google Scholar] [CrossRef] [Green Version]
- Gentile, S.; Strollo, F.; Guarino, G.; Giancaterini, A.; Ames, P.R.J.; Speese, K.; Guida, P.; Strauss, K. Factors hindering correct identification of unapparent lipohypertrophy. J. Diabetes Metab. Disord. Control 2016, 3, 42–47. [Google Scholar] [CrossRef]
- Kapeluto, J.E.; Paty, B.W.; Chang, S.D.; Meneilly, G.S. Ultrasound detection of insulin-induced lipohypertrophy in Type 1 and Type 2 diabetes. Diabet. Med. 2018, 35, 1383–1390. [Google Scholar] [CrossRef] [PubMed]
- Gentile, S.; Guarino, G.; Corte, T.D.; Marino, G.; Fusco, A.; Corigliano, G.; Colarusso, S.; Piscopo, M.; Improta, M.R.; Corigliano, M.; et al. Insulin-induced skin lipohypertrophy in Type 2 diabetes: A multicenter regional survey in Southern Italy. Diabetes Ther. 2020, 11, 2001–2017. [Google Scholar] [CrossRef]
- American Diabetes Association Professional Practice Committee. 9. Pharmacologic approaches to glycemic treatment: Standards of Medical Care in Diabetes—2022. Diabetes Care 2022, 45 (Suppl. 1), S125–S143. [Google Scholar] [CrossRef]
- Gentile, S.; Guarino, G.; Della Corte, T.; Marino, G.; Satta, E.; Pasquarella, M.; Romano, C.; Alfrone, C.; Giordano, L.; Loiacono, F.; et al. AMD-OSDI Study Group on Injection Techniques, and ANIAD. The Economic Burden of Insulin Injection-Induced Lipohypertophy. Role of Education: The ISTERP-3 Study. Adv. Ther. 2022, 39, 2192–2207, Erratum in Adv. Ther. 2022, 39, 3058. [Google Scholar] [CrossRef]
- Gentile, S.; Grassi, G.; Armentano, V.; Botta, A.; Cucco, L.; De Riu, S.; De Rosa, N.; Garrapa, G.; Gentile, L.; Giancaterini, A.; et al. AMD-OSDI consensus on injection techniques for people with diabetes mellitus. Med. Clin. Rev. 2016, 2, 3. [Google Scholar] [CrossRef]
- Frid, A.H.; Kreugel, G.; Grassi, G.; Halimi, S.; Hicks, D.; Hirsch, L.J.; Smith, M.J.; Wellhoener, R.; Bode, B.W.; Hirsch, I.B.; et al. New insulin delivery recommendations. Mayo Clin. Proc. 2016, 91, 1231–1255. [Google Scholar] [CrossRef] [Green Version]
- Consensus Document on the Italian Transposition of Forum for Injection Technique and Therapy Expert Recommendations 2015. Update and Integrations by the AMD-Osdi Inter-Corporate Group on Injective Techniques. 16 May 2017. Available online: https://aemmedi.it/wp-content/uploads/2016/09/FITTER2017.pdf (accessed on 13 February 2023).
- Valentini, M.; Scardapane, M.; Bondanini, F.; Bossi, A.; Colatrella, A.; Girelli, A.; Ciucci, A.; Leotta, S.; Minotti, E.; Pasotti, F.; et al. Efficacy, safety and acceptability of the new pen needle 33G × 4 mm. AGO 01 study. Curr. Med. Res. Opin. 2015, 31, 487–492. [Google Scholar] [CrossRef]
- De Berardis, G.; Scardapane, M.; Lucisano, G.; Abbruzzese, S.; Bossi, A.C.; Cipponeri, E.; D’Angelo, P.; Fontana, L.; Lancione, R.; Marelli, G.; et al. Efficacy, safety and acceptability of the new pen needle 34 G × 3.5 mm: A crossover randomized non-inferiority trial; AGO 02 study. Curr. Med. Res. Opin. 2018, 34, 1699–1704. [Google Scholar] [CrossRef]
- Gentile, S.; Strollo, F.; Satta, E.; Della Corte, T.; Romano, C.; Guarino, G.; Nefrocenter Research Study Group: Nephrologists, Diabetologists, Nurses. Insulin-Related Lipohypertrophy in Hemodialyzed Diabetic People: A Multicenter Observational Study and a Methodological Approach. Diabetes Ther. 2019, 10, 1423–1433. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aronson, R. The role of comfort and discomfort in insulin therapy. Diabetes Technol. Ther. 2012, 14, 741–747. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bergenstal, R.M.; Strock, E.S.; Peremislov, D.; Gibney, M.A.; Parvu, V.; Hirsch, L.J. Safety and efficacy of insulin therapy delivered via a 4mm pen needle in obese patients with diabetes. Mayo Clin. Proc. 2015, 90, 329–338. [Google Scholar] [CrossRef] [PubMed]
- Rubino, F.; Amiel, S.A.; Zimmet, P.; Alberti, G.; Bornstein, S.; Eckel, R.H.; Mingrone, G.; Boehm, B.; Cooper, M.E.; Del Prato, S.; et al. New-Onset Diabetes in COVID-19. N. Engl. J. Med. 2020, 383, 789–790. [Google Scholar] [CrossRef]
- Di Bartolo, P.; Eckel, R.H.; Strollo, S.; Gentile, S. Hundred-year experience with insulin and lipohypertrophy: An unresolved issue. Diabetes Res. Clin. Pract. 2021, 178, 108924. [Google Scholar] [CrossRef]
- Gentle, S.; Strollo, F. Subcutaneous Nodules during Treatment with an Exenatide Long-Acting Once-Weekly Formulation: An Ultrasound Evaluation. Divers. Equal. Health Care 2016, 13, 313–318. [Google Scholar]

| CORRECT LH SEARCH SEQUENCE | |
|---|---|
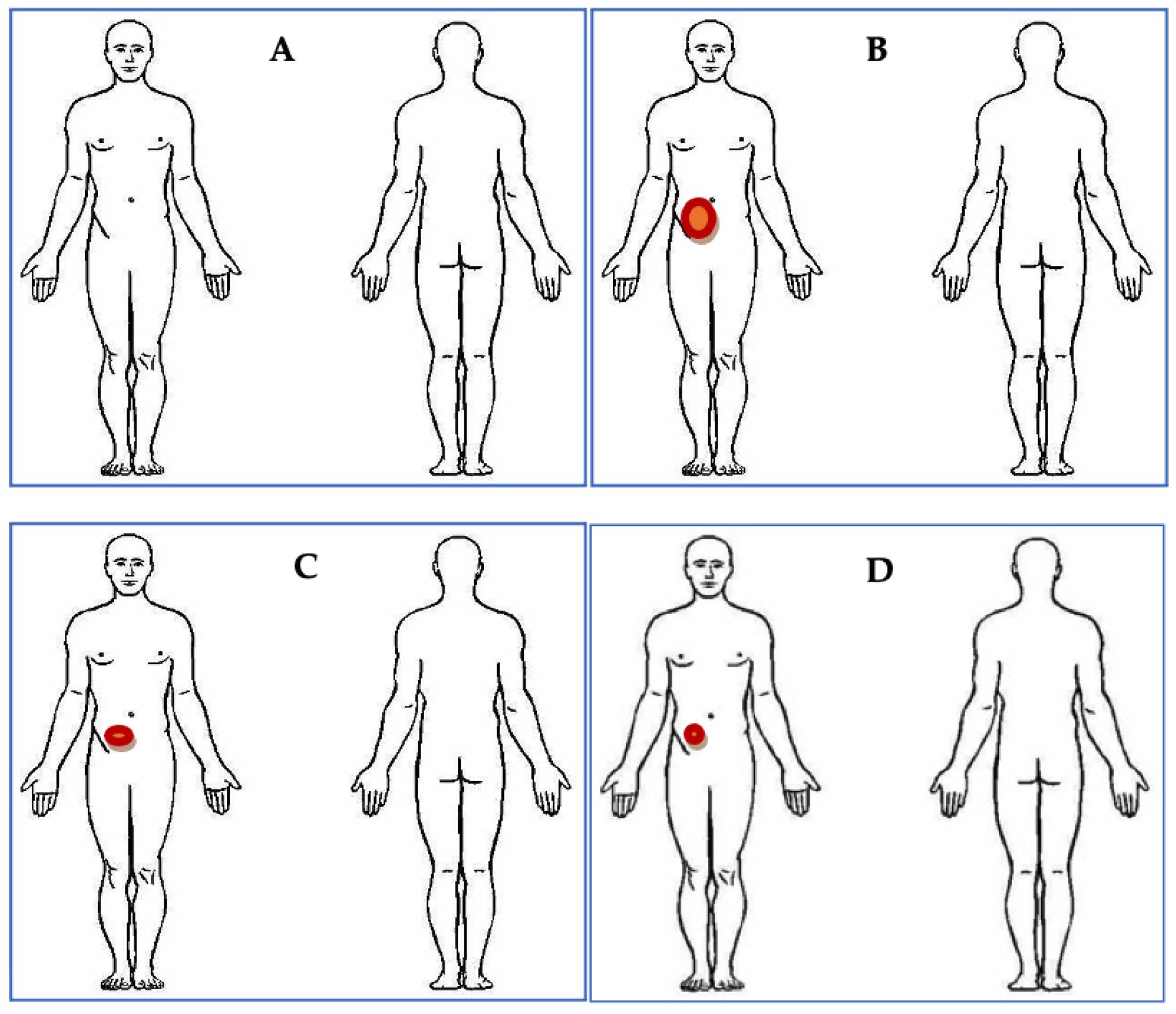
| 1 | Have the patient indicate all skin areas where he or she injects the insulin and examine all of them |
| 2 | Conduct the exam in a well-lit environment, preferably with natural light |
| 3 | Examine the patient supine without clothing and then in a standing position |
| 4 | Rotate the standing patient to take advantage of the incidence of light bringing out LH profile and elevation |
| 5 | Ask the patient to get muscles relaxed during the examination |
| 6 | Perform superficial palpation of the injection sites, passing the examining hand over and over again, looking for nodules or pasty areas of greater consistency than the surrounding skin |
| 7 | Repeat the palpation as described above, with more force to sense any deeper LH |
| 8 | Perform the pinching maneuver, taking a flap of skin between the index finger and thumb, to evaluate the thickness of the skin fold and compare it with nearby areas that are not affected by the injections: the LH is recognizable by a greater thickness of the fold |
| 9 | The set of previous findings allows us to describe an area of skin containing an LH |
| 10 | The LHs can be small or several centimeters large, protruding on the skin or flat; their recognition by sight alone risks not identify clear palpable LHs |
| 11 | Show identified LHs to the patient, explain why they form, what metabolic consequences they entail, and why the need to correctly perform the insulin injection |
| 12 | Give precise and motivated indications on how to correctly inject insulin (injection site rotation, no reuse of the same needle, insulin at room temperature, use of short and thin needles as recommended) |
| 13 | Skin examination (e.g., acanthosis nigricans, insulin injection or insertion sites, lipodystrophy) is a component of the comprehensive diabetes medical evaluation at initial and annual visits, besides every follow-up |
| LH Features | Right Arm | Left Arm | Right Thigh | Left Thigh | Right Hemi- Abdomen | Left Hemi- Abdomen | Right Buttock | Left Buttock |
|---|---|---|---|---|---|---|---|---|
| Present | ||||||||
| >4 cm | ||||||||
| <4 cm | ||||||||
| Protruding | ||||||||
| Flat | ||||||||
| Hard-elastic | ||||||||
| Soft |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gentile, S.; Satta, E.; Guarino, G.; Strollo, F., on behalf of the AMD-OSDI Study Group on Injection Technique. Lipodystrophies from Insulin Injection: An Update of the Italian Consensus Statement of AMD-OSDI Study Group on Injection Technique. Diabetology 2023, 4, 119-127. https://doi.org/10.3390/diabetology4010013
Gentile S, Satta E, Guarino G, Strollo F on behalf of the AMD-OSDI Study Group on Injection Technique. Lipodystrophies from Insulin Injection: An Update of the Italian Consensus Statement of AMD-OSDI Study Group on Injection Technique. Diabetology. 2023; 4(1):119-127. https://doi.org/10.3390/diabetology4010013
Chicago/Turabian StyleGentile, Sandro, Ersilia Satta, Giuseppina Guarino, and Felice Strollo on behalf of the AMD-OSDI Study Group on Injection Technique. 2023. "Lipodystrophies from Insulin Injection: An Update of the Italian Consensus Statement of AMD-OSDI Study Group on Injection Technique" Diabetology 4, no. 1: 119-127. https://doi.org/10.3390/diabetology4010013
APA StyleGentile, S., Satta, E., Guarino, G., & Strollo, F., on behalf of the AMD-OSDI Study Group on Injection Technique. (2023). Lipodystrophies from Insulin Injection: An Update of the Italian Consensus Statement of AMD-OSDI Study Group on Injection Technique. Diabetology, 4(1), 119-127. https://doi.org/10.3390/diabetology4010013







