Journal Description
Diabetology
Diabetology
is an international, peer-reviewed, open access journal on diabetes research published monthly online by MDPI.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within ESCI (Web of Science), Scopus, EBSCO, and other databases.
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 26.3 days after submission; acceptance to publication is undertaken in 5.8 days (median values for papers published in this journal in the first half of 2025).
- Journal Rank: CiteScore - Q2 (Medicine (miscellaneous))
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
Impact Factor:
2.2 (2024);
5-Year Impact Factor:
2.5 (2024)
Latest Articles
Barriers and Facilitators to Mental Health Treatment Among Adults with Type 1 Diabetes: Patient Perspectives on Access, Trust, and Care Gaps
Diabetology 2025, 6(10), 118; https://doi.org/10.3390/diabetology6100118 - 10 Oct 2025
Abstract
►
Show Figures
Background/Objectives: Adults with type 1 diabetes (T1D) experience disproportionately high rates of depression, anxiety, and psychological distress, yet integration of behavioral health into diabetes care remains limited. The objective of this study was to identify barriers and facilitators to mental health treatment
[...] Read more.
Background/Objectives: Adults with type 1 diabetes (T1D) experience disproportionately high rates of depression, anxiety, and psychological distress, yet integration of behavioral health into diabetes care remains limited. The objective of this study was to identify barriers and facilitators to mental health treatment among adults with T1D, using the Behavior Change Wheel as a framework to inform future integrated care strategies. Methods: We conducted five online focus groups with 21 adults with T1D. Discussions were guided by a semi-structured guide, with questions on lived experience, accessibility of mental health treatment, and integrated service delivery informed by the COM-B model domains. Transcripts were analyzed using qualitative content analysis, whereby meaning units were open-coded and then deductively categorized into COM-B constructs of capability, opportunity, and motivation. Results: Participants described limited psychological capability to address mental health due to the heavy self-management burden of T1D, lack of knowledge about navigating care, and uncertainty about treatment interactions. Physical opportunities were constrained by fragmented systems, high costs, and competing responsibilities. However, co-located services and telehealth were viewed as facilitators. Social opportunity was shaped by stigma, isolation, and feeling burdensome, with peer communities providing critical support. Motivation was undermined by past traumatic encounters with psychiatric care and the burden of educating providers about diabetes, contributing to mistrust and avoidance of treatment. Conclusions: Findings highlight how capability, opportunity, and motivation interact to influence engagement with mental health care among adults with T1D. Addressing these barriers through tailored, integrated models of care may strengthen access, trust, and long-term treatment engagement.
Full article
Open AccessReview
Ocular Effects of GLP-1 Receptor Agonists: A Review of Current Evidence and Safety Concerns
by
Giuseppe Maria Albanese, Giacomo Visioli, Ludovico Alisi, Francesca Giovannetti, Luca Lucchino, Marta Armentano, Fiammetta Catania, Marco Marenco and Magda Gharbiya
Diabetology 2025, 6(10), 117; https://doi.org/10.3390/diabetology6100117 - 10 Oct 2025
Abstract
►▼
Show Figures
Glucagon-like peptide-1 receptor agonists (GLP-1RAs) have emerged as cornerstone therapies for type 2 diabetes mellitus and obesity, offering significant cardiovascular and renal protection. However, recent evidence has sparked interest and concern regarding their potential ocular effects. This review critically synthesizes current data on
[...] Read more.
Glucagon-like peptide-1 receptor agonists (GLP-1RAs) have emerged as cornerstone therapies for type 2 diabetes mellitus and obesity, offering significant cardiovascular and renal protection. However, recent evidence has sparked interest and concern regarding their potential ocular effects. This review critically synthesizes current data on the impact of GLP-1RAs on diabetic retinopathy (DR), nonarteritic anterior ischemic optic neuropathy (NAION), age-related macular degeneration (AMD), and glaucoma or ocular hypertension. While preclinical studies suggest GLP-1RAs exert anti-inflammatory and neuroprotective effects in retinal tissues, clinical data remain mixed. Several large observational studies suggest a protective role against DR and glaucoma, while others raise safety concerns, particularly regarding semaglutide and NAION. Evidence on AMD is conflicting, with signals of both benefit and risk. We also discuss plausible pathophysiological mechanisms and the relevance of metabolic modulation on retinal perfusion. Overall, while GLP-1RAs hold promise for ocular protection in some contexts, vigilance is warranted, especially in patients with pre-existing eye disease. Further ophthalmology-focused prospective trials are essential to clarify long-term safety and guide clinical decision making.
Full article

Figure 1
Open AccessArticle
Are There Mental Health Benefits for Those Who Deliver Peer Support? A Mobile App Intervention for Adults with Type 1 Diabetes
by
Debbie Lam, Diana Sherifali, Frances S. Chen and Tricia S. Tang
Diabetology 2025, 6(10), 116; https://doi.org/10.3390/diabetology6100116 - 9 Oct 2025
Abstract
Background/Objectives: Peer support offers a promising approach for improving psychosocial outcomes among adults with type 1 diabetes (T1D). However, research has focused largely on the recipients of peer support rather than the individuals who provide support. This pilot study investigates the impact of
[...] Read more.
Background/Objectives: Peer support offers a promising approach for improving psychosocial outcomes among adults with type 1 diabetes (T1D). However, research has focused largely on the recipients of peer support rather than the individuals who provide support. This pilot study investigates the impact of delivering support on diabetes distress and other secondary mental health outcomes (e.g., depressive symptoms, resilience, and perceived social support). Methods: This pre–post single-cohort study recruited 44 adults with T1D who underwent a six-hour Zoom-based peer supporter training program designed to equip them with support-related skills (asking open-ended questions, making reflections, expressing empathy). Of this group, 36 served as peer supporters for REACHOUT, a six-month mental health support intervention delivered via mobile app. Assessments were conducted at baseline and after six months and measured diabetes distress (Type 1 Diabetes Distress Scale), depressive symptomatology (Patient Health Questionnaire-8), resilience (Diabetes Strengths and Resilience Measure), and perceived social support. Unadjusted and adjusted linear mixed models were performed for each outcome measure of interest. Results: Peer supporters had a mean age of 41 ± 16 years, with a majority identifying as female (75%). At baseline, peer supporters had little to no diabetes distress (50%) and no to mild depressive symptomatology (72%). Mean scores at baseline for diabetes distress, depressive symptoms, resilience, and perceived social support were sustained at 6 months post-intervention. Conclusions: Among peer supporters whose diabetes distress scores start around the target range, ongoing maintenance of these levels may reflect a favorable outcome associated with delivering mental health support.
Full article
(This article belongs to the Special Issue Lifestyle Behavior Intervention for Diabetes Prevention and Management: 2nd Edition)
►▼
Show Figures

Figure 1
Open AccessArticle
Data-Efficiency with Comparable Accuracy: Personalized LSTM Neural Network Training for Blood Glucose Prediction in Type 1 Diabetes Management
by
Esha Manchanda, Jialiu Zeng and Chih Hung Lo
Diabetology 2025, 6(10), 115; https://doi.org/10.3390/diabetology6100115 - 9 Oct 2025
Abstract
►▼
Show Figures
Background/Objectives: Accurate blood glucose forecasting is critical for closed-loop insulin delivery systems to support effective disease management in people with type 1 diabetes (T1D). While long short-term memory (LSTM) neural networks have shown strong performance in glucose prediction tasks, the relative performance of
[...] Read more.
Background/Objectives: Accurate blood glucose forecasting is critical for closed-loop insulin delivery systems to support effective disease management in people with type 1 diabetes (T1D). While long short-term memory (LSTM) neural networks have shown strong performance in glucose prediction tasks, the relative performance of individualized versus aggregated training remains underexplored. Methods: In this study, we compared LSTM models trained on individual-specific data to those trained on aggregated data from 25 T1D subjects using the HUPA UCM dataset. Results: Despite having access to substantially less training data, individualized models achieved comparable prediction accuracy to aggregated models, with mean root mean squared error across 25 subjects of 22.52 ± 6.38 mg/dL for the individualized models, 20.50 ± 5.66 mg/dL for the aggregated models, and Clarke error grid Zone A accuracy of 84.07 ± 6.66% vs. 85.09 ± 5.34%, respectively. Subject-level analyses revealed only modest differences between the two approaches, with some individuals benefiting more from personalized training. Conclusions: These findings suggest that accurate and clinically reliable glucose prediction is achievable using personalized models trained on limited individual data, with important implications for adaptive, on-device training, and privacy-preserving applications.
Full article

Figure 1
Open AccessReview
Factors Influencing the Prescription of First-Line Treatment for Type 2 Diabetes Mellitus: A Systematic Review
by
Helena Silva-Moreira, Fernando Moreira, Ângelo Jesus, Matilde Monteiro-Soares and Paulo Santos
Diabetology 2025, 6(10), 114; https://doi.org/10.3390/diabetology6100114 - 9 Oct 2025
Abstract
Background/Objectives: Understanding prescribing patterns for type 2 diabetes mellitus, a complex condition affecting over 10% of the global adult population, can optimise prescribing practices, guide policymakers in promoting evidence-based medicine, and help tailor first-line treatments to individual characteristics or specific subgroups, improving patient
[...] Read more.
Background/Objectives: Understanding prescribing patterns for type 2 diabetes mellitus, a complex condition affecting over 10% of the global adult population, can optimise prescribing practices, guide policymakers in promoting evidence-based medicine, and help tailor first-line treatments to individual characteristics or specific subgroups, improving patient outcomes. This study aimed to identify factors influencing the prescription and non-prescription of metformin, the recommended first-line therapy in Western guidelines, and to evaluate whether these prescribing patterns align with evidence-based recommendations. It also explores factors associated with initial combination therapy, a more recent and controversial approach compared to stepwise therapy. Methods: We conducted a systematic search in PubMed, Scopus, and Web of Science on 25 August 2023, without language or time restrictions, to identify observational analytical studies assessing factors associated with the initiation of metformin or combination therapy in adults with type 2 diabetes mellitus who were naïve to antidiabetic medications. Studies involving pregnant or breastfeeding women were excluded. A narrative synthesis was conducted. Study quality was assessed using the Joanna Briggs Institute critical appraisal checklists (PROSPERO registration number CRD42023438313). Results: Thirty studies were included, evaluating 105 variables, most of which (62%) were assessed in one study. The 25 variables using combination therapy as the outcome were mostly (72%) evaluated also in one study. Initial metformin prescription was strongly and positively associated with younger age, lower glycated haemoglobin levels, higher body mass index, and absence of renal impairment. Initial combination therapy was associated with higher HbA1c levels and a lower burden of comorbidities. Findings also highlighted a discrepancy between clinical practice and evidence-based recommendations. However, concerns were raised regarding both the internal and external validity of the included studies. Conclusions: Our systematic review, which offers insights into real-world clinical practices, indicated that there is a misalignment between clinical practices and evidence-based recommendations, supporting the need for interventions in this field.
Full article
(This article belongs to the Special Issue Early Intervention and Treatment Strategies for Diabetes)
►▼
Show Figures

Figure 1
Open AccessArticle
Enhancing Diabetes Screening Among Oral Healthcare Professionals: A COM-B Model and a Theoretical Domains Framework Approach
by
André Priede, Phyllis Lau, Rodrigo Mariño and Ivan Darby
Diabetology 2025, 6(10), 113; https://doi.org/10.3390/diabetology6100113 - 5 Oct 2025
Abstract
►▼
Show Figures
Background/Objectives: Early detection of undiagnosed prediabetes (PD) and type 2 diabetes (T2D) could prevent or delay the onset of diabetes and its complications. The dental setting has been suggested as a location for expanding diabetes screening in primary care. This study aimed to
[...] Read more.
Background/Objectives: Early detection of undiagnosed prediabetes (PD) and type 2 diabetes (T2D) could prevent or delay the onset of diabetes and its complications. The dental setting has been suggested as a location for expanding diabetes screening in primary care. This study aimed to investigate behavioural factors that influence an oral healthcare professional’s (OHP) participation in diabetes screening and their decision to refer individuals at a high risk of diabetes for medical follow-up and confirmatory diagnosis. These factors provide targets for future interventions to encourage screening implementation and increase referral guideline compliance. Methods: This qualitative study utilised OHPs who had participated in a diabetes screening trial in Victoria, Australia. Qualitative, semi-structured interviews were conducted by telephone or videoconferencing and transcribed and analysed thematically. The themes identified were deductively mapped onto the Capability, Opportunity, Motivation, and Behaviour (COM-B) model and the Theoretical Domains Framework (TDF). Results: In total, eight interviews were conducted (seven dentists and one oral health therapist). Five COM-B domains were identified: reflective motivation, automatic motivation, social opportunity, physical opportunity, and psychological capability. Nine TDF domains were associated with issues related to knowledge, the environmental context and resources, memory, attention and decision processes, skills, social influences, beliefs about consequences, emotion, beliefs about capability, and social influence. Conclusions: This is the first study to investigate the factors influencing an OHP’s participation and decision making in diabetes screening and referral processes in the dental setting. The results demonstrate that OHPs need more education and training to screen for diabetes in dental clinics. This study represents the first step in developing interventions to target these factors and improve the effectiveness of diabetes screening in the dental setting.
Full article

Figure 1
Open AccessArticle
Serum Sphingolipid and Glycerophospholipid Synthesis, Especially Phosphatidylinositol/Lysophosphatidylinositol, Phosphatidylglycerol/Lysophosphatidylglycerol, and Ceramides, Are Significantly Influenced by Diabetes Mellitus and Associated with Its Complications
by
Hideyuki Takizawa, Baasanjav Uranbileg, Yatomi Yutaka and Makoto Kurano
Diabetology 2025, 6(10), 112; https://doi.org/10.3390/diabetology6100112 - 3 Oct 2025
Abstract
►▼
Show Figures
Background/Objectives: Diabetes mellitus, a prevalent metabolic disorder, causes severe complications and economic burden, requiring effective therapeutic strategies. While triglycerides and low-density lipoproteins (LDLs) have been widely studied in type 2 diabetes mellitus (T2DM) and related cardiovascular risks, the roles of other lipids, such
[...] Read more.
Background/Objectives: Diabetes mellitus, a prevalent metabolic disorder, causes severe complications and economic burden, requiring effective therapeutic strategies. While triglycerides and low-density lipoproteins (LDLs) have been widely studied in type 2 diabetes mellitus (T2DM) and related cardiovascular risks, the roles of other lipids, such as sphingolipids and glycerophospholipids, remain unclear. This study aimed to investigate their involvement in T2DM and its complications. Methods: We examined sphingolipid and glycerophospholipid profiles in T2DM patients to assess alterations associated with diabetes mellitus and its related complications. Results: Patients with T2DM showed significant modulations in sphingolipid and glycerophospholipid levels, suggesting these lipids contribute to metabolic dysregulation and progression of diabetes-related complications. Conclusions: Alterations in sphingolipids and glycerophospholipids play a critical role in T2DM, indicating their potential as novel targets for therapeutic intervention and risk mitigation in patients with diabetes and its complications.
Full article

Figure 1
Open AccessReview
Redox Balance, Mitohormesis, and Organ Stress in Type 2 Diabetes Mellitus: Mechanistic Insights and the Therapeutic Role of SGLT2 Inhibitors
by
Toshiki Otoda, Ken-ichi Aihara and Tadateru Takayama
Diabetology 2025, 6(10), 111; https://doi.org/10.3390/diabetology6100111 - 3 Oct 2025
Abstract
►▼
Show Figures
Oxidative stress and chronic low-grade inflammation are recognized key drivers of diabetic complications. Lysosomal dysfunction, cellular senescence, and inter-organ stress signaling further aggravate the Redox–Inflammation–Organ Stress Axis in type 2 diabetes mellitus (T2DM). Recent studies suggest that reactive oxygen species (ROS) are not
[...] Read more.
Oxidative stress and chronic low-grade inflammation are recognized key drivers of diabetic complications. Lysosomal dysfunction, cellular senescence, and inter-organ stress signaling further aggravate the Redox–Inflammation–Organ Stress Axis in type 2 diabetes mellitus (T2DM). Recent studies suggest that reactive oxygen species (ROS) are not always harmful. Through mitohormesis, mild and transient increases in ROS levels can trigger antioxidant defenses, strengthen mitochondrial function, and limit chronic inflammation. Evidence from caloric restriction, exercise, and ketone body studies supports this adaptive redox balance, underscoring the importance of maintaining a “hormetic window” rather than indiscriminate antioxidant supplementation. In our prospective study, sodium-glucose cotransporter 2 inhibitor treatment significantly reduced albuminuria and serum levels of inflammatory markers, e.g., tumor necrosis factor receptors 1 and 2, while paradoxically increasing urinary 8-hydroxy-2′-deoxyguanosine levels and biological antioxidant potential (BAP), suggestive of adaptive ROS responses consistent with mitohormesis. Concomitant glucagon-like peptide-1 receptor agonist use emerged as an independent explanatory factor for increased urinary levels of oxidative stress markers, suggesting that multiple metabolic therapies converge on shared hormetic pathways. Emerging evidence that stressed adipocytes can communicate mild ROS signals via extracellular vesicles expands this paradigm to inter-organ mitohormesis. Collectively, these insights caution against indiscriminate antioxidant use and underscore the therapeutic potential of controlled redox modulation to disrupt the vicious cycle of senescence, inflammation, and organ stress. Incorporating redox biomarkers like urinary 8-hydroxy-2′-deoxyguanosine, reactive oxygen metabolite derivatives, and BAP into clinical monitoring, alongside pharmacological and lifestyle interventions, may facilitate the realization of precision metabolic medicine for multi-organ protection in T2DM.
Full article

Graphical abstract
Open AccessArticle
Development and Content Validation of the Insulin Pump Infusion Sets Satisfaction Scale (IPISS): A Self-Reported Questionnaire for Patients with Type 1 Diabetes and Caregivers
by
Marco Del Monte, Giordano Spacco, Andrea Pintabona, Giulia Siri, Stefano Parodi, Filippo Gambarelli, Elena Poirè, Nicola Minuto and Marta Bassi
Diabetology 2025, 6(10), 110; https://doi.org/10.3390/diabetology6100110 - 3 Oct 2025
Abstract
Background: Patient satisfaction with diabetes technology is increasingly recognized as a key factor in therapeutic success. Patient-reported outcomes (PROs) are gaining importance in diabetes care and in the evaluation of advanced insulin delivery systems. Objectives: This study aimed to design and validate a
[...] Read more.
Background: Patient satisfaction with diabetes technology is increasingly recognized as a key factor in therapeutic success. Patient-reported outcomes (PROs) are gaining importance in diabetes care and in the evaluation of advanced insulin delivery systems. Objectives: This study aimed to design and validate a new questionnaire, the Insulin Pump Infusion Sets Satisfaction Scale (IPISS), to assess satisfaction with insulin infusion sets among individuals with type 1 diabetes. Methods: The questionnaire was developed by our Diabetology Unit in two versions: one for patient self-reporting and one for caregivers when the patient is too young to complete it autonomously. Content validity was assessed by six healthcare professionals (three diabetologists and three nurses) based on Polit and Beck’s methodology. The Item Content Validity Index (I-CVI) was calculated for both relevance and comprehensibility and was considered satisfactory if expert agreement reached ≥83%. The Scale Content Validity Index (S-CVI) was computed as the average of I-CVIs, with a cut-off value > 90% deemed acceptable. Results: Almost all items achieved 100% positive agreement for both relevance and comprehensibility, except one item in the caregiver version, for which one rater did not provide a rating for comprehensibility (I-CVI = 83.3%). The S-CVI was 100% for relevance in both versions, 99.24% for comprehensibility in the caregiver version, and 100% in the patient version. Conclusions: The IPISS is a content-validated, self-reported tool, suitable for evaluating satisfaction with infusion sets in individuals using insulin pumps, with versions adapted for both patients and caregivers.
Full article
(This article belongs to the Special Issue Insulin Injection Techniques and Skin Lipodystrophy)
Open AccessArticle
Validated Diabetes Risk Scores and Their Associations with Lifestyle and Quality of Life in Spanish Workers
by
María Dolores Marzoa Jansana, Pedro Juan Tárraga López, Juan José Guarro Miquel, Ángel Arturo López-González, Pere Riutord Sbert, Carla Busquets-Cortés and José Ignacio Ramírez-Manent
Diabetology 2025, 6(10), 109; https://doi.org/10.3390/diabetology6100109 - 2 Oct 2025
Abstract
►▼
Show Figures
Background: Type 2 diabetes mellitus (T2DM) is a global health concern driven by aging, lifestyle, and socio-economic disparities. Early detection is key, with tools like FINDRISC, QDScore, and CANRISK providing non-invasive screening. Yet, the combined effects of sociodemographic factors, healthy habits, and perceived
[...] Read more.
Background: Type 2 diabetes mellitus (T2DM) is a global health concern driven by aging, lifestyle, and socio-economic disparities. Early detection is key, with tools like FINDRISC, QDScore, and CANRISK providing non-invasive screening. Yet, the combined effects of sociodemographic factors, healthy habits, and perceived quality of life on diabetes risk remain insufficiently studied in working populations. Objectives: To evaluate the association between sociodemographic variables, lifestyle habits (smoking, physical activity, adherence to the Mediterranean diet), and health-related quality of life (HRQoL) with the risk of developing type 2 diabetes, using three validated screening tools in a large cohort of Spanish workers. Methods: A cross-sectional study was conducted among 100,014 Spanish workers aged 18 to 69 years who underwent standardized medical evaluations between January 2021 and December 2023. Diabetes risk was assessed using the FINDRISC, QDScore, and CANRISK tools. Lifestyle variables and HRQoL (measured via the SF-12 questionnaire) were evaluated through validated instruments. Multivariate logistic regression models were used to examine the association of independent variables with moderate-to-high diabetes risk according to each score. Results: Among the strongest predictors, poor adherence to a Mediterranean diet (OR = 1.45, 95% CI: 1.32–1.58) and low physical activity (OR = 1.39, 95% CI: 1.27–1.52) were independently associated with higher diabetes risk. Poor HRQoL was also significant (OR = 1.33, 95% CI: 1.22–1.47). Conclusions: Sociodemographic factors, lifestyle behaviors, and perceived health status are independently associated with increased type 2 diabetes risk in Spanish workers. The integration of HRQoL assessments into occupational health surveillance may enhance early identification of at-risk individuals and guide tailored prevention strategies.
Full article

Figure 1
Open AccessArticle
Impact of Diabetes Mellitus, Its Duration, and Associated Complications on Nutritional Intake in Patients at Risk of Malnutrition: A Focused Nutritional Assessment
by
Paloma Pérez López, Jaime González Gutiérrez, Lucía Estévez Asensio, Olatz Izaola Jauregui, David Primo Martín, Beatriz Ramos Bachiller, Eva López Andrés, Daniel De Luis Román and Juan José López Gómez
Diabetology 2025, 6(10), 108; https://doi.org/10.3390/diabetology6100108 - 2 Oct 2025
Abstract
►▼
Show Figures
Background/Objectives: Diabetes mellitus (DM) is a disorder which affects carbohydrate metabolism and has been associated with other conditions such as disease-related malnutrition (DRM), leading to specific challenges in its management. This study aims to evaluate the implications of DM, its complications, and its
[...] Read more.
Background/Objectives: Diabetes mellitus (DM) is a disorder which affects carbohydrate metabolism and has been associated with other conditions such as disease-related malnutrition (DRM), leading to specific challenges in its management. This study aims to evaluate the implications of DM, its complications, and its duration on energy and protein intake in patients at high risk of malnutrition. Methods: Descriptive cross-sectional study in 179 patients with high risk of malnutrition. Patients were compared based on the presence or absence of DM, diabetes duration and the presence of complications. Age, gender, body mass index, bioimpedanciometry, ultrasonography and dynamometry parameters and the diagnosis of sarcopenia were recorded. Energy and protein requirements were calculated, and the composition of the patients’ three-day diet was analyzed. Results: DM was associated with lower weight-adjusted energy intake (Overall: 29.15 (9.99) vs. DM: 24.87 (8.28) vs. NoDM: 30.65 (10.13) kcal/kg/day; p < 0.01) and lower weight-adjusted protein intake (Overall: 1.29 (0.47) vs. DM: 1.18 (0.39) vs. NoDM: 1.33 (0.49) g of protein/kg/day; p < 0.05). DM was a risk factor for poorer compliance with energy requirements (OR: 2.38, 95% CI: 1.13–5.01, p < 0.05). Similarly, the occurrence of complications was identified as a risk factor associated with reduced adherence to energy intake requirements (OR: 1.78, 95% CI 1.06–2.98; p < 0.05), and a duration of diabetes mellitus exceeding 10 years was linked to lower adherence to protein intake requirements (OR 1.79, 95% CI 1.08–2.99; p < 0.05). Conclusions: Among patients at high risk of malnutrition, diabetes mellitus was associated with suboptimal adherence to both caloric and protein intake requirements. The presence of diabetes and its related complications emerged as risk factors for inadequate fulfillment of energy needs, while a longer disease duration was specifically linked to reduced compliance with protein requirements.
Full article

Graphical abstract
Open AccessArticle
Evaluation of Cardiovascular Risk Factor Control Among People with Diabetes in the Community Pharmacy Setting—A Descriptive Observational Study
by
Marian Zaki, Claire O’Sullivan, Ellen Barrett, Nasim Mirzai, Hazel Thornton, Yazid N. Al Hamarneh and Margaret Bermingham
Diabetology 2025, 6(10), 107; https://doi.org/10.3390/diabetology6100107 - 2 Oct 2025
Abstract
►▼
Show Figures
Background: In some countries, community pharmacists provide advanced services to people with diabetes that improve glycaemic control and cardiovascular risk. This study aims to describe the cardiovascular risk profile of people with diabetes attending community pharmacy in Ireland. Methods: Data collection for this
[...] Read more.
Background: In some countries, community pharmacists provide advanced services to people with diabetes that improve glycaemic control and cardiovascular risk. This study aims to describe the cardiovascular risk profile of people with diabetes attending community pharmacy in Ireland. Methods: Data collection for this descriptive, observational, cross-sectional study took place in 10 pharmacies, in four Irish counties between July 2018 and October 2019. Participants were aged ≥18 years, with type 1 or type 2 diabetes, attending a participating pharmacy and were dispensed oral diabetes medicines, insulin, or devices for monitoring glycaemic control. Participants were asked about their demographics, medical history, and cardiovascular risk factors. Current medications were identified from dispensing software. Results: Data were available for 106 participants; 70 (66.0%) were male and 36 (34.0%) were female. The median age was 66.0 [56.5: 72.0] years. Of these, 90 (84.9%) had type 2 diabetes. Hypertension and dyslipidaemia were reported by 60 (56.6%) and 59 (55.7%) participants, respectively. Twenty-one participants (19.8%) were current smokers, 31 (29.2%) followed no specific diet, and 44 (41.5%) did not undertake exercise. Oral diabetes medication was prescribed to 85 (80.2%) and insulin was prescribed to 29 (27.4%) participants. Where an antihypertensive was prescribed, 21 participants (19.8%) achieved the systolic blood pressure on-treatment goal of ≤130 mmHg and 34 (32.1%) achieved the diastolic blood pressure on-treatment goal of <80 mmHg. Conclusions: Study participants demonstrated a high rate of characteristics associated with increased cardiovascular risk, including non-achievement of target blood pressure, smoking, and lack of exercise. A community pharmacist-led intervention aimed at potentially improving cardiovascular risk factors in people with diabetes warrants further study in an Irish setting.
Full article

Figure 1
Open AccessArticle
Association Between Hypoglycaemia at the 24–28th-Week OGTT and Obstetric and Neonatal Outcomes in Women with Gestational Diabetes
by
Maria Luís Mazeda, Bruna Silva, Catarina Cidade-Rodrigues, Filipa Moreira, Vânia Benido-Silva, Vânia Gomes, Catarina Chaves, Catarina A. Pereira, Cláudia Machado, Odete Figueiredo, Anabela Melo, Mariana Martinho, Anabela Ferreira, Ana Morgado, Maria do Céu Almeida, Ana Saavedra, Margarida Almeida and Filipe M. Cunha
Diabetology 2025, 6(10), 106; https://doi.org/10.3390/diabetology6100106 - 2 Oct 2025
Abstract
►▼
Show Figures
Introduction: Women with gestational diabetes mellitus (GDM) can present with hypoglycaemia during the oral glucose tolerance test (OGTT), which has been associated with adverse perinatal outcomes. Objectives: We studied whether the presence of hypoglycaemia during the OGGT (HdOGTT) was associated with
[...] Read more.
Introduction: Women with gestational diabetes mellitus (GDM) can present with hypoglycaemia during the oral glucose tolerance test (OGTT), which has been associated with adverse perinatal outcomes. Objectives: We studied whether the presence of hypoglycaemia during the OGGT (HdOGTT) was associated with adverse perinatal outcomes. Methods: Retrospective study of a national database of women diagnosed with GDM in the 24–28th week OGTT. Excluded: women with missing OGTT or the primary outcomes data. HdOGGT: any glucose value < 70 mg/dL. Primary outcomes: hypertensive disease of pregnancy, preterm delivery, caesarean section (CSA), small-for-gestational-age, large-for-gestational-age, neonatal hypoglycaemia, respiratory distress syndrome, and intensive care unit admission. Women with and without hypoglycaemia were compared. Predictors of HdOGTT and the association between HdOGTT and the primary outcomes were studied using a multivariate logistic regression analysis. Results: We analysed 7704 women, 10.7% with HdOGTT. Most of them (94.8%) presented fasting hypoglycaemia, and 3.2% had blood glucose values < 54 mg/dL. There were no differences between groups regarding the primary outcomes, except for women with HdOGTT, who had a lower rate of CSA (34.1% vs. 29.0%, p = 0.001), large-for-gestational-age newborns (9.7% vs. 13.8%, p < 0.001), and a higher rate of small-for-gestational-age newborns (11.0% vs. 6.9%, p < 0.001) than those without HdOGTT. Age, BMI, previous miscarriage, and chronic hypertension were associated with lower risk of HdOGTT. HdOGTT was only associated with increased risk of SGA [OR (95% CI): 1.25 (1.00–1.56), p = 0.047] after adjustment for confounders. Conclusions: The prevalence of HdOGTT was 10.7%. Age, BMI, previous miscarriage, and chronic hypertension were associated with lower risk of HdOGTT. HdOGTT was associated with 25% higher risk of SGA newborns.
Full article

Figure 1
Open AccessArticle
Program Evaluation of Do Well, Be Well with Diabetes: Promoting Healthy Living in Adults with Type 2 Diabetes
by
Sumathi Venkatesh, Katelin M. Alfaro Hudak, Morium B. Bably, Stephanie M. Rogus, Danielle Krueger, Heidi Fowler and Michael Laguros
Diabetology 2025, 6(10), 105; https://doi.org/10.3390/diabetology6100105 - 2 Oct 2025
Abstract
►▼
Show Figures
Background/Objectives: Type 2 diabetes (T2D) is a pressing public health challenge in the United States (U.S.). Community-based diabetes education programs equip individuals with T2D with the knowledge and skills to improve dietary behaviors, build confidence, and better manage their condition to reduce
[...] Read more.
Background/Objectives: Type 2 diabetes (T2D) is a pressing public health challenge in the United States (U.S.). Community-based diabetes education programs equip individuals with T2D with the knowledge and skills to improve dietary behaviors, build confidence, and better manage their condition to reduce complications. However, few studies evaluate self-care adherence and self-efficacy together. This study examined participant adherence to diabetes self-care practices and confidence in managing diabetes through a community-based education program. Methods: Do Well, Be Well with Diabetes (DWBWD) is a 5-week program focused on reinforcing the best practices in diabetes management through dietary practices, physical activity, and gaining self-confidence in managing T2D. The program was evaluated among 137 participants across 14 Texas counties using pre- and post-surveys that assessed the number of days per week participants engaged in diabetes self-care practices, as well as their confidence in performing these behaviors (rated on a scale from 1 = not at all confident to 5 = extremely confident). Results: Participants were mostly male (75.9%), White (60.6%), and over 65 years (58.4%). Most participants had T2D (57.7%) or prediabetes (27.0%). Compared to the program entry, participants reported improvements (p < 0.001) in self-care practices, as reflected by their mean differences (MD), including following a healthful eating plan (MD −1.46), consuming five servings of fruit and vegetables (MD −0.87), spacing carbohydrate intake evenly throughout the day (MD −1.64), engaging in at least 30 min of daily physical activity (MD −0.74), testing blood glucose (MD −1.08), and checking their feet (MD −1.09). Confidence in performing all self-care behaviors significantly improved (p < 0.001), with MDs between −0.53 and −1.13, indicating higher post-program scores. Conclusions: Participation in the DWBWD program increased confidence in diabetes management and enhanced engagement in key health behaviors associated with reducing diabetes complications.
Full article

Graphical abstract
Open AccessArticle
Dietary Behaviors and Psychosocial Factors of People Managing Diabetes During Fasting: A Qualitative Study from Five US Muslim Communities
by
Asma Mahd Ali, Olayinka O. Shiyanbola, Ejura Salihu, Salma Abdelwahab, James E. Bailey and Betty Chewning
Diabetology 2025, 6(10), 104; https://doi.org/10.3390/diabetology6100104 - 1 Oct 2025
Abstract
Objectives: This study sought to understand dietary behaviors among US Muslim people with Type 2 diabetes while managing diabetes and fasting during Ramadan, identify key psychosocial factors influencing behaviors, and examine how identified factors influence diet behaviors and health outcomes from the patient’s
[...] Read more.
Objectives: This study sought to understand dietary behaviors among US Muslim people with Type 2 diabetes while managing diabetes and fasting during Ramadan, identify key psychosocial factors influencing behaviors, and examine how identified factors influence diet behaviors and health outcomes from the patient’s perspective. Methods: The study employed community-engaged research principles and qualitative research design. Twenty-two adult Muslim adults living with Type 2 diabetes for over 6 months participated in semi-structured one-on-one interviews. Participants were recruited from five US communities using purposive sampling. Three trained researchers used abductive coding, combining deductive and inductive approaches, to analyze the data. Results: Six main themes emerged from the data: (1) changes in dietary habits during Ramadan; (2) strong influence of religious, cultural and social practices on dietary behaviors; (3) variable self-efficacy in managing dietary behaviors; (4) impact of prior habits and current blood glucose status; (5) decision-making based on diabetes-related health outcomes (e.g., experiencing low blood sugar); (6) participants’ perception of Ramadan as an opportunity for sustainable behavioral changes. Conclusions: This study is among the first to document the dietary behaviors and key psychosocial factors influencing dietary behaviors and health outcomes for US Muslim people with Type 2 diabetes during Ramadan. The study suggests that interventions to improve diabetes control and promote diabetes remission among Muslims can benefit from cultural tailoring that draws on Ramadan religious, cultural and social practices to encourage sustainable behavioral change.
Full article
(This article belongs to the Special Issue Lifestyle Behavior Intervention for Diabetes Prevention and Management: 2nd Edition)
►▼
Show Figures

Graphical abstract
Open AccessArticle
Increased Insulin Resistance in Roma Pregnancies
by
Christina Pagkaki, Ourania Christou, Dimitra Oikonomopoulou, Zoe Siateli, Sofia Kalantaridou, Emmanouil Zoumakis, Georgios Petrakos and Panagiotis Halvatsiotis
Diabetology 2025, 6(10), 103; https://doi.org/10.3390/diabetology6100103 - 30 Sep 2025
Abstract
►▼
Show Figures
Background: Reduced tissue sensitivity to insulin, as well as the associated increased risk of gestational diabetes mellitus is genetically controlled and often varies racially and geographically. Roma populations constitute a genetically autonomous society with particularities in their type of sociability, and they are
[...] Read more.
Background: Reduced tissue sensitivity to insulin, as well as the associated increased risk of gestational diabetes mellitus is genetically controlled and often varies racially and geographically. Roma populations constitute a genetically autonomous society with particularities in their type of sociability, and they are reported to have an increased prevalence of type 2 diabetes mellitus, which is pathophysiologically related to insulin resistance. Objectives: The aim of this study was to investigate the level of insulin sensitivity in pregnancies of Roma mothers compared to controls. Methods: A total of 65 pregnancies were studied during the third trimester, divided between 33 Roma mothers (RP) and 32 mothers of European descent to serve as control volunteers (CP). The presence of gestational diabetes was confirmed according to the WHO diagnostic criteria by a 75 mg oral glucose tolerance test and insulin resistance status by the means of HOMA-IR index. Results: The mean fasting insulin levels as well as the mean HOMA-IR index were statistically significantly higher in the Roma population (p = 0.0013) and (p < 0.001), respectively, regardless of the age and BMI of the participants. Gestational Diabetes Mellitus developed in seven women (10.7%), five of whom were Roma (15.1%) and in two controls (6.2%) (p = 0.247). Conclusions: Increased insulin resistance is observed in Roma pregnancies, so it would be beneficial to provide these women with appropriate counseling focused on healthy diet and lifestyle.
Full article

Figure 1
Open AccessArticle
A Real-World Study of Electronic Prescriptions and Medication Adherence in Bulgaria
by
Nikol Georgieva, Nikolay Gerasimov, Vasil Madzharov and Guenka Petrova
Diabetology 2025, 6(10), 102; https://doi.org/10.3390/diabetology6100102 - 29 Sep 2025
Abstract
Background: The implementation of electronic prescriptions in Bulgaria since 2023 provides new opportunities for real-world data analysis of prescribing practices and medication adherence particularly for chronic diseases such as diabetes. Objective: To evaluate prescribing patterns medication adherence and National Health Insurance Fund (NHIF)
[...] Read more.
Background: The implementation of electronic prescriptions in Bulgaria since 2023 provides new opportunities for real-world data analysis of prescribing practices and medication adherence particularly for chronic diseases such as diabetes. Objective: To evaluate prescribing patterns medication adherence and National Health Insurance Fund (NHIF) coverage in patients with diabetes across three major Bulgarian regions using 6-month electronic prescription (e-prescription) data from January to June 2024. Materials and Methods: Data were collected from community pharmacies in Sofia, Plovdiv, and Dobrich and Stara Zagora. Prescriptions were categorized by diabetes type (type 1 or type 2), therapy class (traditional vs. innovative), refill frequency, and NHIF reimbursement. Adherence was estimated using refill frequency and the Proportion of Days Covered (PDC) method. Results: A total of 1071 prescriptions were analyzed. In Sofia, type 1 patients (n = 13) had high rates of adherence (mean: 6.5 refills; 54% refill-based adherence), while type 2 patients (n = 138) showed more variability (mean: 4.55 refills; 27.5% with PDC ≥ 80%). Innovative therapies (e.g., DPP-4, SGLT2 inhibitors) were more frequently used in Sofia, reflected by higher NHIF reimbursement costs. In contrast, Dobrich, Stara Zagora, and Plovdiv predominantly relied on traditional medications (e.g., metformin, sulfonylureas) with lower adherence and limited use of innovative therapies. Conclusions: E-prescription data provides valuable insights into real-world diabetes management and shows substantial regional differences in adherence and treatment intensity. In the bigger cities there is better adherence and access to modern therapies, while smaller regions are slower in adopting these treatments. These findings support the need for national policies to ensure equitable access to innovative therapies and enhanced digital support for chronic disease management. From clinical practice point of view adherence follow-up is a key for treatment success and healthcare decision-making.
Full article
Open AccessCase Report
A Case of Paradoxical Appetite Increase During Semaglutide Therapy
by
Edin Karisik, Zorica Stanojevic-Ristic, Slobodan Jankovic, Bojana Bozic Cvijan, Marija Djukanovic, Esin Halo and Mersiha Mulic
Diabetology 2025, 6(10), 101; https://doi.org/10.3390/diabetology6100101 - 25 Sep 2025
Abstract
►▼
Show Figures
Semaglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist, is widely used to reduce appetite and promote weight loss in patients with type 2 diabetes. However, individual variability may lead to paradoxical responses. We describe a 60-year-old woman with type 2 diabetes who experienced progressive
[...] Read more.
Semaglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist, is widely used to reduce appetite and promote weight loss in patients with type 2 diabetes. However, individual variability may lead to paradoxical responses. We describe a 60-year-old woman with type 2 diabetes who experienced progressive weight gain and increased appetite during 12 months of semaglutide therapy, despite previous successful weight loss with sodium-glucose cotransporter 2 (SGLT2) inhibitors. Her body mass index (BMI) rose from 31.6 to 34.6 kg/m2, accompanied by worsening glycemic control. Eating behavior assessment with the Dutch Eating Behavior Questionnaire revealed a maximum score for emotional eating, suggesting a strong psychological barrier to treatment efficacy. Genetic factors, such as GLP-1 receptor polymorphisms, may also contribute to reduced responsiveness. This case highlights the possible influence of both emotional and genetic factors on treatment outcomes and emphasizes the need for personalized approaches in the management of obesity and type 2 diabetes.
Full article

Graphical abstract
Open AccessArticle
Therapeutic Adherence and Glycemic Control in the Population with Diabetes in Ceuta (Spain), a Multicultural City: A Cross-Sectional Study
by
Brieba del Río Pascual, Antolí Jover Ana María, Vázquez Lara Juana María, Ruger Navarrete Azahara, Vázquez Lara María Dolores, Palomo Gómez Rocio, Artero García Alejandro, Rodríguez Díaz Luciano and Fernández Carrasco Francisco Javier
Diabetology 2025, 6(9), 100; https://doi.org/10.3390/diabetology6090100 - 22 Sep 2025
Abstract
►▼
Show Figures
Diabetes mellitus constitutes a significant global public health problem. It is a chronic disease characterized by persistent hyperglycemia, which is a consequence of inadequate insulin secretion, deficient insulin action, or a combination of both factors. A crucial component in the effective management of
[...] Read more.
Diabetes mellitus constitutes a significant global public health problem. It is a chronic disease characterized by persistent hyperglycemia, which is a consequence of inadequate insulin secretion, deficient insulin action, or a combination of both factors. A crucial component in the effective management of this pathology is therapeutic adherence, as it helps prevent complications, improve patient quality of life, reduce associated mortality, and decrease the need for hospitalization. In this context, it is crucial to implement a comprehensive care model that offers continuous support and a multidisciplinary approach. Primary care should be central, coordinating the entire care process. Understanding the clinical and social characteristics of people with diabetes is key to guiding more effective interventions. Objective: The objective of this study was to describe the sociodemographic and anthropometric characteristics, degree of metabolic control, and treatment adherence in patients with diabetes mellitus enrolled in primary care programs in Ceuta. Materials and Methods: This was a descriptive, observational, and cross-sectional study conducted during the second half of 2024. The study population included individuals enrolled in the primary care diabetes program in Ceuta. We analyzed sociodemographic variables with a self-administered questionnaire, the level of therapeutic adherence using the MMAS-8 scale, and glycemic control through glycosylated hemoglobin (HbA1c) values. Results: The sample consisted of 370 individuals, with 50.3% being men. The average age was 62.82 years (SD = 13.46). A significant portion of participants, 61.07%, had no formal education or had only received primary education. Additionally, 84.9% of the participants had at least one other associated chronic pathology. Regarding adherence, 36.8% of the patients showed a high level, and for all patients, the mean HbA1c value was 7.5% (SD = 1.55). Furthermore, our analysis revealed statistically significant associations between cultural background and both therapeutic adherence (weak positive correlation: r = 0.213, p ≤ 0.001; multivariate significance: sig: <0.001; Exp(B) = 2.448) and glycemic control (multivariate significance: sig: <0.001; Exp(B) = 2.686). Conclusions: We observed high treatment adherence in the study population, with HbA1c values within the limits recommended by the World Health Organization for older adults. Furthermore, a relationship between cultural background and both treatment adherence and glycemic control was identified. This suggests a need for further research into these and other social determinants, like study level or monthly income, in future studies.
Full article
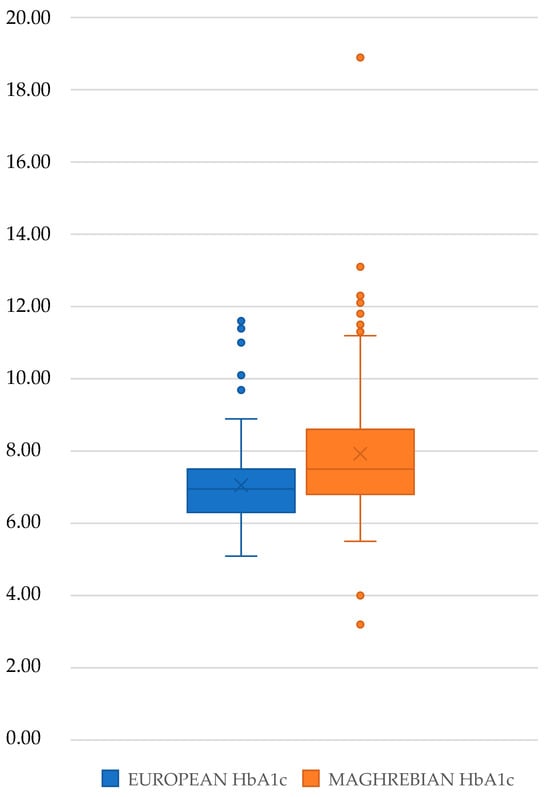
Figure 1
Open AccessArticle
Prevalence of Sarcopenia in Very Old Diabetic and Non-Diabetic Hospitalized Patients
by
Sandra De Breucker, Véronique Lachat, Emilia Frangos, Andrea Trombetti, Ulrich Vischer, Aline Mendes, François R. Herrmann and Christophe E. Graf
Diabetology 2025, 6(9), 99; https://doi.org/10.3390/diabetology6090099 - 11 Sep 2025
Abstract
Background/Objectives: The prevalence of diabetes in very old people is rising sharply worldwide, due not only to obesity, nutritional and sedentary lifestyles, but also to aging per se. Diabetes is associated with a higher incidence of sarcopenia, malnutrition and physical disabilities. However,
[...] Read more.
Background/Objectives: The prevalence of diabetes in very old people is rising sharply worldwide, due not only to obesity, nutritional and sedentary lifestyles, but also to aging per se. Diabetes is associated with a higher incidence of sarcopenia, malnutrition and physical disabilities. However, many age-specific issues in the clinical management of very old diabetic patients remain unstudied. Methods: This is a case–control prospective study including 162 very old hospitalized diabetic patients and 301 controls. We explored the impact of diabetes on the prevalence of sarcopenia according to the EWGSOP2 criteria, using Jamar handgrip to assess muscle strength, BIA-derived fat-free mass index to assess muscle mass, and the timed up and go test to assess physical performance. We also explored factors associated with sarcopenia in both groups in multiple logistic analysis. Results: Mean age was 84.8 ± 6.0 years. We found a prevalence of sarcopenia of 8.0% and 16.7% in the diabetic and the control groups, respectively (p = 0.010). BMI was independently associated with sarcopenia in both groups, explaining 25% of the model in the diabetic group and 33% of the model in the control group. Conclusions: Sarcopenia was less prevalent in diabetic hospitalized older patients than in other patients, indicating that old frail patients are not the same patients as those that are in epidemiological studies on sarcopenia in diabetes. These results should be confirmed in further studies.
Full article
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics

Conferences
Special Issues
Special Issue in
Diabetology
Innovations in the Identification, Prevention and Management of Diabetes-Related Foot Complications
Guest Editor: Aikaterini AndreadiDeadline: 31 October 2025
Special Issue in
Diabetology
Obesity and Diabetes: Healthy Lifestyle Choices
Guest Editors: Elena Gangitano, Maria Irene BelliniDeadline: 15 November 2025
Special Issue in
Diabetology
New Perspectives and Future Challenges in Diabetic Retinopathy
Guest Editor: Akifumi KushiyamaDeadline: 30 November 2025
Special Issue in
Diabetology
Current Understanding of Gender Differences in Diabetes and Rheumatological Diseases
Guest Editors: Giancarlo Tonolo, Daniela MarottoDeadline: 15 December 2025








