1. Introduction
Skin is our largest organ, with a surface area of 1.8–2 m
2 and an approximate weight of 9 kg. The skin serves as a processor of sensory, thermoregulatory, metabolic, and immunological contact between the body’s internal milieu and the external environment. Skin has the potential to easily become injured by sharp objects as it is a delicate organ. Wounds are injuries that damage or result in openings in the skin or other body tissues with multiple causes, such as sutures, stitches, and surgeries. Wounds initiate a complex healing process [
1,
2].
Wound dressing is utilized in order to aid the healing process [
3]. There are two types of wound dressing, which are traditional and advanced wound dressing [
4]. Wounds are a global health concern, yet technological advancements have not fully addressed wound management [
5]. This study aims to fabricate a self-healing bioabsorbable polymeric base with antibacterial and improved wound healing properties.
2. Materials
After optimizing the morphological conditions and accurately determining the essential standards for the design, the base materials were selected to be polyvinyl alcohol (PVA) and chitosan. These two polymers were chosen because of the characteristics and features mentioned in
Table 1. Furthermore, combining synthetic and natural polymers will enhance the dressing properties.
Table 2 shows some possible additives that could be added to the polymer to enhance the quality of the dressing. The selection from the additives will be based on their efficacy during the practical trials.
3. Method
Two mixtures were prepared for testing: a pure mixture consisting only of polymers, and an additive mixture containing additives.
The PVA mixture was prepared by heating distilled water to 90 °C, then adding 22.5 g of PVA to the water and stirring until completely dissolved. The final volume was 100 mL, with a 15% PVA concentration. To prepare the chitosan, 150 mL of distilled water was stirred with 7.5 g of chitosan, 5% Acetic acid, and 5% Acetic acid for 24 h. The final volume was 150 mL, with a 5% chitosan concentration. This mixture was blended with heat to create a gel-based texture. The additive mixture was prepared by adding frankincense, myrrh, alum stone, and rose water to 500 mL of rose water. This solution was finalized using a double filtration method, resulting in 400 mL of the additive solution. A blend of 50% pure chitosan and 50% PVA was combined with the additive solution, creating a gel-based texture. The gel was poured into an acrylic mold, covered with non-stick and non-woven paper, and left to solidify for two to three days. The adhesive gel was then applied to a DAMA transparent adhesive dressing.
A bacterial growth test was conducted using a development buffer (DB) made of 8 mL PBS, 24 mL distilled water, 4 mL MgCl2, and 4 mL CaCl2. Agar powder was added to the DB to provide a stable growth surface for bacteria to form colonies. The mixture was sterilized by being holed for 15 min at 121 °C in an autoclave. The initial investigative test involved wiping three sample plates with a pre-sterilized DB mixture, pure mixed polymers, and composite polymers and additives, then adding 4 ml of a media buffer (MB) under UV light for 20 min, which enhanced the growth of microorganisms and the fermentation of the environment. As a second investigative test, the MB solution was separated from the sample plates and poured into two bottles with a small amount of distilled water and 0.5 mL iodine. This solution was centrifuged for four minutes to separate the particles, creating a strong bacterial environment for the testing operation. Then, three sample plates were wiped with a pre-sterilized DB mixture, pure mixed polymers, and composite polymers and additives. A total of 4 mL of mononuclear and iodine agent solution was added to each plate and kept at room temperature for four days.
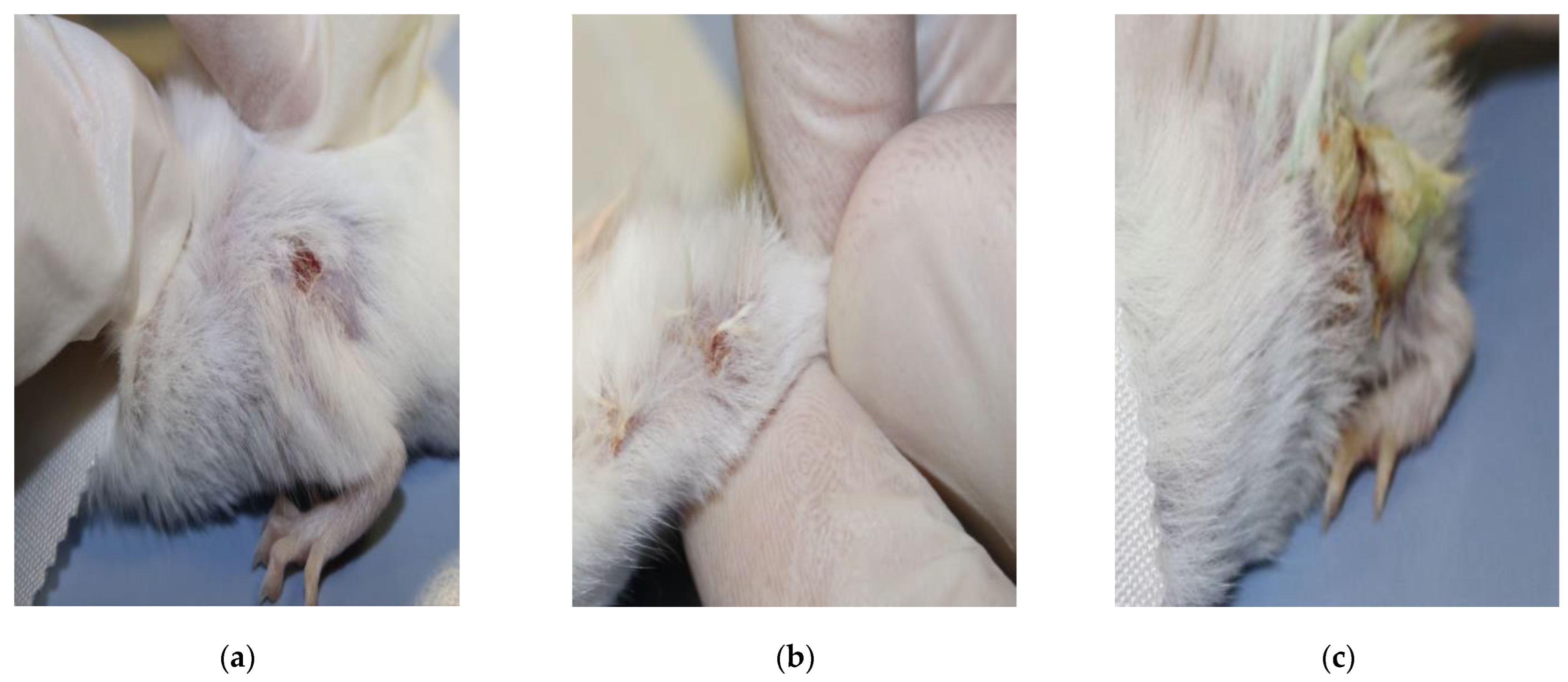
After obtaining ethical approval from the deanship of scientific research, we acquired three rats to evaluate their wound-healing process by making minor cuts (superficial wounds) on their body under local anesthetic. Then, we wiped the first rat’s wound with the pure mixture of polymers, the second one with the mixture of polymers and additives, and the third without any solution, to be considered a control sample. The wounds were monitored for four days.
The viscosity of a mixture was determined through four practical steps: determining the weight of the pure polymer mix and the composite polymer mix with additives; calculating the volume using normative beakers and calculating the density of both mixtures. These data were then applied to the mathematical formula to determine their viscosity.
4. Result
The effectiveness of each mixture was assessed in lab rats and the wound healing duration was monitored. The following figure shows the results once the lab rats had been monitored for four days, after applying the gel once, directly after incision.
After the fabrication, the first test performed was a physical properties test that included measuring the viscosities of the mixtures.
Table 3 shows the calculated viscosity results.
5. Discussion
The control plates showed clear and significant cell aggregation as well as a large number of fruiting bodies, indicating normal cell growth. The plates containing the pure gel mixture showed no aggregation or cell development on the growth plate and no fruiting bodies on the development plate. This indicates that the mixture had a strong inhibitory effect on microbial growth. The final two plates were used with the additive mixture: the growth plate showed some aggregation and fungi, but the aggregation was not as significant as the control; and the development plate showed some fruiting bodies, though most were dead. This indicates that the mixture had a partly inhibitory effect, but not as strong as the pure gel mixture.
The rats were monitored for four days after applying the gel once directly after incision. For the pure mixture, the results were promising compared to the control rat, showing a reduction in wound size. Meanwhile, the additive mixture did not show any enhancement of wound healing, and made the wound look inflamed.
When the gel made from chitosan and PVA was molded on a medical pad, it worked well for healing wounds. It helped wounds heal faster, initiated new skin growth, and stopped bacteria from growing. The pure gel showed the best results. This gel is affordable, easy to obtain, safe, and suitable for people with allergies.
6. Conclusions and Future Work
The chitosan and PVA polymer-based gel formed an effective wound dressing when applied to a medical pad. It showed promising results in accelerating wound healing, promoting new skin formation, and inhibiting bacterial growth. Testing showed that the pure polymer gel mixture was most effective, while the additive-containing mixture provided few benefits. This suggests that the chitosan–PVA base itself is what is effective. The polymer gel dressing’s affordability, accessibility, safety, and hypoallergenic properties make it a promising option. However, further research and optimization are still needed before commercializing this product. Future work could improve the prototype through advanced manufacturing techniques to make it suitable for post-surgical wounds instead of sutures. Additionally, incorporating local natural materials from Al-Ahsa could give the product a distinctive cultural theme while contributing to the development of national industries. While the initial results are promising, substantial research and development are still needed before this polymer dressing can be routinely used as an accepted treatment. Nevertheless,, with focused efforts and refinement, this novel dressing has the potential to become a valuable treatment option in the near future.
Author Contributions
Conceptualization, Z.A.A. and S.A.; methodology, H.A.; software, M.A.; validation, F.A. and W.A.; formal analysis, R.A. (Reem Alamer); investigation, G.A.S.; resources, M.A.; data curation, R.A. (Rayanah Aloudah); writing—original draft preparation, H.A., Alatafi, M., R.A. (Reem Alamer), R.A. (Rayanah Aloudah), F.A., G.A.S. and W.A.; writing—review and editing, Z.A.A. and S.A.; visualization, S.A.; supervision, Z.A.A.; project administration, M.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
With due consideration for animal welfare, animal testing must be conducted ethically and humanely. Our experiment was ethically conducted with the approval of King Faisal University, ensuring responsible and ethical conduct. The ethical approval number is KFU-REC-2023-JAN-ETHICS493.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Değim, Z. Use of microparticulate systems to accelerate skin wound healing. J. Drug Target. 2008, 16, 437–448. [Google Scholar] [CrossRef] [PubMed]
- Wounds and Injuries. Available online: https://medlineplus.gov/woundsandinjuries.html (accessed on 20 September 2023).
- Dreifke, M.B.; Jayasuriya, A.A.; Jayasuriya, A.C. Current wound healing procedures and potential care. Mater. Sci. Eng. C 2015, 48, 651–662. [Google Scholar] [CrossRef] [PubMed]
- Tottoli, E.M.; Dorati, R.; Genta, I.; Chiesa, E.; Pisani, S.; Conti, B. Skin Wound Healing Process and New Emerging Technologies for Skin Wound Care and Regeneration. Pharmaceutics 2020, 12, 735. [Google Scholar] [CrossRef] [PubMed]
- EL-Ghoul, Y.; Alminderej, F.M.; Alsubaie, F.M.; Alrasheed, R.; Almousa, N.H. Recent Advances in Functional Polymer Materials for Energy, Water, and Biomedical Applications: A Review. Polymers 2021, 13, 4327. [Google Scholar] [CrossRef] [PubMed]
- Matica, M.A.; Aachmann, F.L.; Tøndervik, A.; Sletta, H.; Ostafe, V. Chitosan as a Wound Dressing Starting Material: Antimicrobial Properties and Mode of Action. Int. J. Mol. Sci. 2019, 20, 5889. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.; Wu, P.; Cheng, Q.; He, C.; Chen, Y.; Zhou, J. Ultrafast Fabrication of Self-Healing and Injectable Carboxymethyl Chitosan Hydrogel Dressing for Wound Healing. ACS Appl. Mater. Interfaces 2021, 13, 24095–24105. [Google Scholar] [CrossRef] [PubMed]
- Gaaz, T.; Sulong, A.; Akhtar, M.; Kadhum, A.; Mohamad, A.; Al-Amiery, A. Properties and Applications of Polyvinyl Alcohol, Halloysite Nanotubes and Their Nanocomposites. Molecules 2015, 20, 22833–22847. [Google Scholar] [CrossRef] [PubMed]
- 15 Uses and Benefits of Frankincense Essential Oil. iLAVAHEMP. Available online: https://ilavahemp.com/frankincense-essential-oil/ (accessed on 23 September 2023).
- 5 Benefits and Uses of Frankincense—And 7 Myths. Available online: https://www.healthline.com/nutrition/frankincense# (accessed on 23 September 2023).
- Alum: Benefits, Precautions and Dosage. 1 mg. Available online: https://www.1mg.com/ayurveda/alum-143 (accessed on 23 September 2023).
- Pal, D.A. Alum: Uses, Benefits & Side Effects. PharmEasy Blog. 25 April 2022. Available online: https://pharmeasy.in/blog/ayurveda-uses-benefits-side-effects-of-alum/ (accessed on 23 September 2023).
- Rose Water: 10 Benefits and How to Use. Available online: https://www.healthline.com/health/rose-water-benefits (accessed on 23 September 2023).
- Suliman, R.S.; Alghamdi, S.S.; Ali, R.; Aljatli, D.; Aljammaz, N.A.; Huwaizi, S.; Suliman, R.; Kahtani, K.M.; Albadrani, G.M.; Barhoumi, T.; et al. The Role of Myrrh Metabolites in Cancer, Inflammation, and Wound Healing: Prospects for a Multi-Targeted Drug Therapy. Pharmaceuticals 2022, 15, 944. [Google Scholar] [CrossRef] [PubMed]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).