The Role and Future Directions of 3D Printing in Custom Prosthetic Design †
Abstract
1. Introduction
2. Traditional Prosthetic Manufacturing Processes

| Feature | Stereolithography (SL) | Fused Deposition Modeling (FDM) | Selective Laser Sintering (SLS) |
|---|---|---|---|
| Process Overview | Uses a UV laser to cure liquid resin layer by layer into a solid object. | Melts and extrudes thermoplastic filament through a nozzle, depositing it layer by layer. | Uses a laser to sinter powdered material into a solid structure layer by layer without requiring a support structure. |
| Material Options | Photopolymers (resins), limited to liquid state materials. | Wide range of thermoplastics (PLA, ABS, PETG, TPU, etc.). | Nylon, polyamide, and composites (e.g., nylon with carbon fiber or glass-filled materials). |
| Surface Finish | Produces smooth, high-resolution surfaces ideal for aesthetic prosthetic components. | Surfaces can be rough or require post-processing to smooth, depending on layer thickness and nozzle quality. | Excellent surface quality with minimal post-processing required, suitable for complex designs. |
| Strength and Durability | High resolution but less durable than thermoplastics; resins may be brittle and prone to cracking under stress. | Durable and flexible thermoplastics offer strong performance; however, strength depends on filament quality and print settings. | Produces durable and functional parts with good mechanical properties, including resistance to wear and impact. |
| Precision and Accuracy | Extremely precise, with high levels of detail, making it ideal for intricate designs. | Moderately precise; precision depends on nozzle size and printer calibration. | Highly precise, with the ability to handle complex geometries and fine details. |
| Speed | Slower than other methods due to the curing process; ideal for small, detailed parts but not for large-scale production. | Generally faster, particularly for simpler designs; ideal for prototyping. | Moderate speed; faster than SL for large builds but slower than FDM for simple parts. |
| Cost of Equipment | High initial costs due to advanced hardware and the need for specific materials (resins). | Low to moderate; affordable entry-level printers are widely available. | Expensive, with industrial-grade machines dominating the market. |
| Material Cost | High; specialized resins are more expensive than thermoplastics. | Low to moderate; thermoplastic filaments are widely available and affordable. | Moderate to high; powdered materials can be more costly, especially for specialized applications. |
| Ease of Use | Requires expertise to handle resins safely and operate the machine; post-curing is also necessary. | User-friendly and widely accessible; ideal for beginners and low-tech environments. | Requires technical expertise for setup and operation; safety precautions are needed for handling powders. |
| Environmental Impact | Resins are less eco-friendly and can be hazardous if not disposed of properly. | Filaments, like PLA, are biodegradable and more eco-friendly; however, others, like ABS, produce fumes during printing. | Powder waste can be recycled to an extent, but the overall environmental impact depends on the material usage and disposal practices. |
| Applications in Prosthetics | Excellent for creating aesthetic components, such as cosmetic covers and lightweight decorations. | Ideal for rapid prototyping, preliminary designs, and the cost-effective production of simple prosthetic parts. | Well-suited for functional and structural components, such as load-bearing prosthetic frames or complex joints. |
| Advantages | - High resolution and detail for intricate designs.- Smooth surface finish reduces post-processing. - Ideal for small, detailed, and aesthetic components. | - Cost-effective and accessible. - Wide material availability. - Flexible design options for prototypes and low-stress parts. | - Superior mechanical properties. - No need for support structures, enabling complex geometries. - Durable, functional parts suitable for long-term use. |
| Disadvantages | - High material and equipment costs. - Limited material strength and durability. - Requires expertise in handling and post-curing. | - Limited surface finish quality; often requires post-processing. - Less suitable for high-stress or complex load-bearing parts. | - High equipment and material costs. - Requires technical expertise and industrial setup. - Not as accessible for small-scale or individual users. |
| Future Potential | Advancements in resin materials to improve durability and reduce costs may expand its applications in prosthetics. | Continuous improvements in filament quality and printer precision could make FDM more suitable for functional prosthetic components. | Expanding material options and reducing machine costs could make SLS more accessible, enabling the widespread use of both functional and aesthetic prosthetic components. |
3. Advantages of 3D Printing in Prosthetic Design
3.1. Rapid Production
3.2. Cost-Effectiveness
3.3. Customization and Personalization
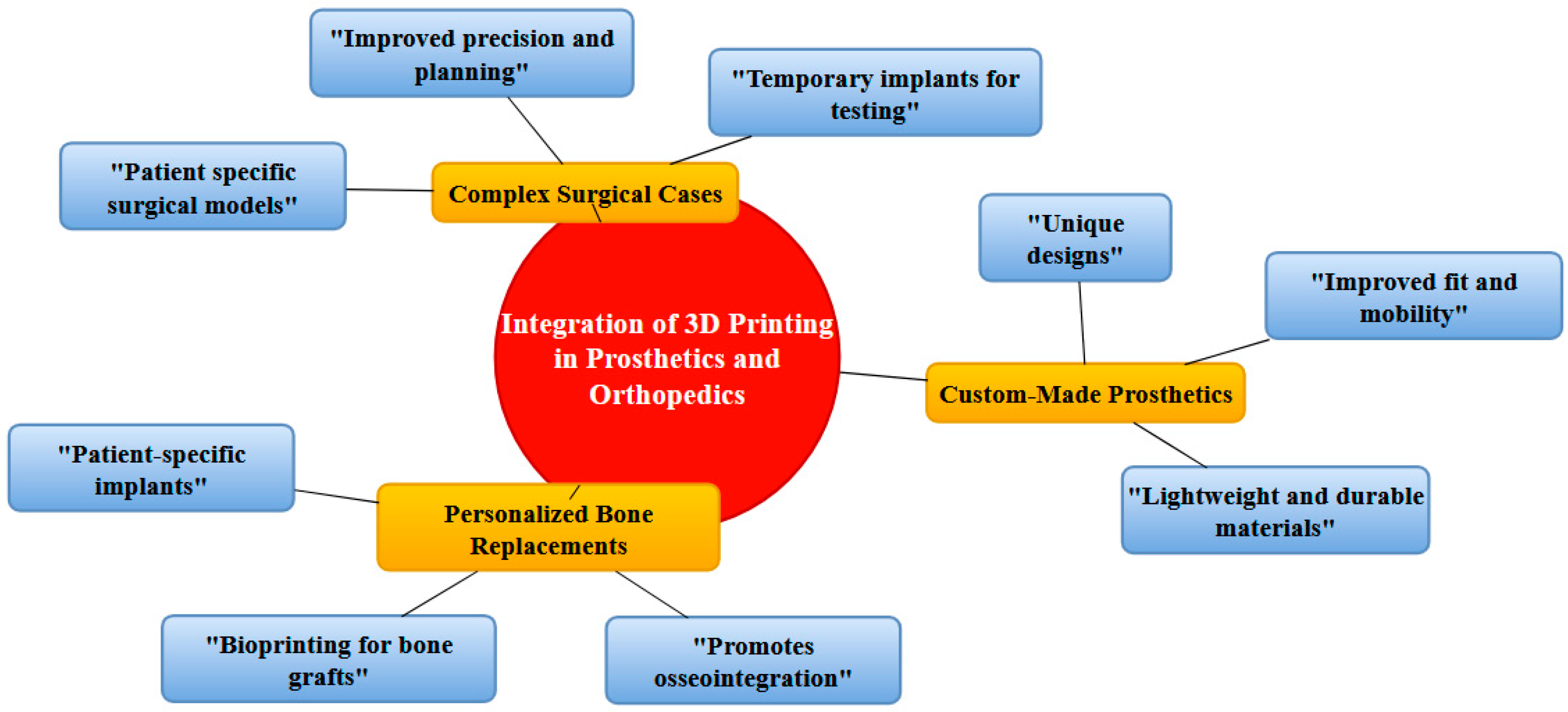
4. Integration of 3D Printing in Prosthetics and Orthopedics
4.1. Custom-Made Prosthetics
4.2. Personalized Bone Replacements
4.3. Use in Complex Surgical Cases
5. Technological Advancements
5.1. Material and Design Flexibility
5.2. Durability and Performance
6. The Evolution of Materials in Prosthetics
7. Design Considerations for 3D-Printed Prosthetic and Orthopedic Solutions
7.1. Customization and Personalization
7.2. Material Selection
7.3. Structural and Functional Design
7.4. Integration with Advanced Technologies
8. Some Recent Case Studies on 3D-Printed Prosthetics
9. Current Limitations, Material Constraints, and Regulatory Hurdles of 3D Printing in Prosthetics
9.1. Material Constraints
9.2. Regulatory Hurdles
10. Affordability and Accessibility of 3D Printers
11. Transformative Impact on the Prosthetics Industry
12. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wolfe, R.A.; Roys, E.C.; Merion, R.M. Trends in Organ Donation and Transplantation in the United States, 1999–2008. Am. J. Transplant. 2010, 10 Pt 2, 961–962. [Google Scholar] [CrossRef]
- Yeong, W.Y.; Chua, C.K.; Leong, K.F.; Chandrasekaran, M.; Lee, M.W. Indirect fabrication of collagen scaffold based on inkjet printing technique. Rapid Prototyp. J. 2006, 12, 229–237. [Google Scholar] [CrossRef]
- Butscher, A.; Bohner, M.; Doebelin, N.; Hofmann, S.; Müller, R. New depowderingfriendly designs for three-dimensional printing of calcium phosphate bone substitutes. Acta Biomater. 2013, 9, 9149–9158. [Google Scholar] [CrossRef] [PubMed]
- Saunders, R.E.; Gough, J.E.; Derby, B. Delivery of human fibroblast cells by piezoelectric drop-on-demand inkjet printing. Biomaterials 2008, 29, 193–203. [Google Scholar] [CrossRef]
- Pathak, K.; Saikia, R.; Das, A.; Das, D.; Islam, A.; Pramanik, P.; Parasar, A.; Borthakur, P.P.; Sarmah, P.; Saikia, M.; et al. 3D printing in biomedicine: Advancing personalized care through additive manufacturing. Explor. Med. 2023, 4, 1135–1167. [Google Scholar] [CrossRef]
- Xu, T.; Zhao, W.; Zhu, J.M.; Albanna, M.Z.; Yoo, J.J.; Atala, A. Complex heterogeneous tissue constructs containing multiple cell types prepared by inkjet printing technology. Biomaterials 2013, 34, 130–139. [Google Scholar] [CrossRef]
- Derby, B. Printing and prototyping of tissues and scaffolds. Science 2012, 338, 921–926. [Google Scholar] [CrossRef]
- Wang, K.; Ho, C.C.; Zhang, C.; Wang, B. A review on the 3D printing of functional structures for medical phantoms and regenerated tissue and organ applications. Engineering 2017, 3, 653–662. [Google Scholar] [CrossRef]
- Zhao, Y.; Yao, R.; Ouyang, L.; Ding, H.; Zhang, T.; Zhang, K.; Cheng, S.; Sun, W. Three-dimensional printing of Hela cells for cervical tumor model in vitro. Biofabrication 2014, 6, 035001. [Google Scholar] [CrossRef]
- Wang, Y.; Tan, Q.; Pu, F.; Boone, D.; Zhang, M. A Review of the Application of Additive Manufacturing in Prosthetic and Orthotic Clinics from a Biomechanical Perspective. Engineering 2020, 6, 1258–1266. [Google Scholar] [CrossRef]
- Totah, D.; Kovalenko, I.; Saez, M.; Barton, K. Manufacturing Choices for Ankle-Foot Orthoses: A Multi-Objective Optimization. Procedia CIRP 2017, 65, 145–150. [Google Scholar] [CrossRef]
- Jiang, R.; Kleer, R.; Piller, F.T. Predicting the Future of Additive Manufacturing: A Delphi Study on Economic and Societal Implications of 3D Printing for 2030. Technol. Forecast. Soc. 2017, 117, 84–97. [Google Scholar] [CrossRef]
- Baumers, M.; Dickens, P.; Tuck, C.; Hague, R. The Cost of Additive Manufacturing: Machine Productivity, Economies of Scale, and Technology-Push. Technol. Forecast. Soc. 2016, 102, 193–201. [Google Scholar] [CrossRef]
- Kurfess, T.; Cass, W.J. Rethinking Additive Manufacturing and Intellectual Property Protection. Res. Technol. Manag. 2014, 57, 35–42. [Google Scholar] [CrossRef]
- Yan, Q.; Dong, H.; Su, J.; Han, J.; Song, B.; Wei, Q.; Shi, Y. A Review of 3D Printing Technology for Medical Applications. Engineering 2018, 4, 729–742. [Google Scholar] [CrossRef]
- Weller, C.; Kleer, R.; Piller, F.T. Economic Implications of 3D Printing: Market Structure Models in Light of Additive Manufacturing Revisited. Int. J. Prod. Econ. 2015, 164, 43–56. [Google Scholar] [CrossRef]
- Petrick, I.J.; Simpson, T.W. 3D Printing Disrupts Manufacturing: How Economies of One Create New Rules of Competition. Res. Technol. Manag. 2013, 56, 12–16. [Google Scholar] [CrossRef]
- Patel, P.; Gohil, P. Custom orthotics development process based on additive manufacturing. Mater. Today Proc. 2022, 59, A52–A63. [Google Scholar] [CrossRef]
- Pallari, J.H.P.; Dalgarno, K.W.; Munguia, J.; Muraru, L.; Peeraer, L.; Telfer, S.; Woodburn, J. Design and Additive Fabrication of Foot and Ankle-Foot Orthoses. In Proceedings of the 21st Annual International Solid Freeform Fabrication Symposium—An Additive Manufacturing Conference, Austin, TX, USA, 9–11 August 2010. [Google Scholar]
- Boschetto, A.; Giordano, V.; Veniali, F. Modelling Micro Geometrical Profiles in Fused Deposition Process. Int. J. Adv. Manuf. Tech. 2012, 61, 945–956. [Google Scholar] [CrossRef]
- Boschetto, A.; Bottini, L.; Veniali, F. Finishing of Fused Deposition Modeling Parts by CNC Machining. Robot. CIM Int. Manuf. 2016, 41, 92–101. [Google Scholar] [CrossRef]
- Al-Masa’fah, W.; Abushaikha, I.; Bwaliez, O.M. Exploring the role of additive manufacturing in the prosthetic supply chain: Qualitative evidence. TQM J. 2024. [Google Scholar] [CrossRef]
- Chopra, T. Application of artificial intelligence and 3D printing in prosthetics: A review. NeuroQuantology 2022, 20, 2691–2694. [Google Scholar]
- Mobarak, M.H.; Islam, M.A.; Hossain, N.; Mahmud, M.Z.A.; Rayhan, M.T.; Nishi, N.J.; Chowdhury, M.A. Recent Advances of Additive Manufacturing in Implant Fabrication—A Review. Appl. Surf. Sci. Adv. 2023, 18, 100462. [Google Scholar] [CrossRef]
- Park, J.W.; Kang, H.G. Application of 3-dimensional printing implants for bone tumors. Clin. Exp. Pediatr. 2022, 65, 476–482. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Patel, P.; Gohil, P. Design, Analysis and Development of Prosthetic and Orthotic Elements by Additive Manufacturing Process. Int. J. Lightweight Mater. Manuf. 2024, 8, 205–227. [Google Scholar] [CrossRef]
- Smith, D.G.; Burgess, E.M. The use of CAD/CAM technology in prosthetics and orthotics--current clinical models and a view to the future. J. Rehabil. Res. Dev. 2001, 38, 327–334. [Google Scholar] [PubMed]
- Ciobanu, O. Utilizarea tehnologiilor de tip CAD/CAM şi de fabricare rapidă în producerea protezelor şi ortezelor [The use of CAD/CAM and rapid fabrication technologies in prosthesis and orthotics manufacturing]. Rev. Med.-Chir. Soc. Medici Nat. Iasi 2012, 116, 642–648. [Google Scholar]
- Lemaire, E. A CAD analysis programme for prosthetics and orthotics. Prosthet. Orthot. Int. 1994, 18, 112–117. [Google Scholar] [CrossRef] [PubMed]
- Hassan, B.B.; Wong, M.S. Contemporary and Future Development of 3D Printing Technology in the Field of Assistive Technology, Orthotics and Prosthetics. Can. Prosthet. Ortho. J. 2023, 6, 42225. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Daniele, B. Evolution of prosthetic feet and design based on gait analysis data. In Clinical Engineering Handbook, 2nd ed.; Elsevier: Amsterdam, The Netherlands, 2019; pp. 458–468. [Google Scholar] [CrossRef]
- Powell, S.K.; Cruz, R.L.J.; Ross, M.T.; Woodruff, M.A. Past, present, and future of soft-tissue prosthetics: Advanced polymers and advanced manufacturing. Adv. Mater. 2020, 32, 2001122. [Google Scholar] [CrossRef]
- Fiorillo, L.; D’amico, C.; Turkina, A.Y.; Nicita, F.; Amoroso, G.; Risitano, G. Endo and exoskeleton: New technologies on composite materials. Prosthesis 2020, 2, 1. [Google Scholar] [CrossRef]
- Young, K.J.; Pierce, J.E.; Zuniga, J.M. Assessment of body-powered 3D printed partial finger prostheses: A case study. 3D Print. Med. 2019, 5, 7. [Google Scholar] [CrossRef]
- Delgado, A.E.; Contreras, G.G.M.; Espinosa, W.J.M. Implementation of mechanical elements and materials for knee joint prostheses. ARPN J. Eng. Appl. Sci. 2021, 16, 2589–2593. [Google Scholar]
- Lascano, S.; Estay, D. Biomedical devices: Materials, fabrication and control. In Intelligent Systems 2022, Control and Automation: Science and Engineering; Springer: Berlin/Heidelberg, Germany, 2022; Volume 82, pp. 195–219. [Google Scholar] [CrossRef]
- Vedi, H.; Bhaiswar, V.; Walke, P. Design, analysis and development of low-cost 3D printed prosthetic hand. AIP Conf. Proc. 2024, 3139, 030007. [Google Scholar] [CrossRef]
- Varaganti, P.; Seo, S. Recent advances in biomimetics for the development of bio-inspired prosthetic limbs. Biomimetics 2024, 9, 273. [Google Scholar] [CrossRef]
- D’Alessio, J.; Christensen, A. 3D printing for commercial orthopedic applications: Advances and challenges. In 3D Printing in Orthopaedic Surgery; Elsevier: Amsterdam, The Netherlands, 2018; pp. 65–83. [Google Scholar] [CrossRef]
- Ribeiro, D.; Cimino, S.R.; Mayo, A.L.; Ratto, M.; Hitzig, S.L. 3D printing and amputation: A scoping review. Disabil. Rehabil. Assist. Technol. 2021, 16, 221–240. [Google Scholar] [CrossRef] [PubMed]
- Oladapo, B.I.; Olawumi, M.A.; Omigbodun, F.T. Advancements and future prospects of additive manufacturing in orthopedics. In Medical Additive Manufacturing: Concepts and Fundamentals; Elsevier: Amsterdam, The Netherlands, 2024; pp. 443–473. [Google Scholar] [CrossRef]
- Oladapo, B.I.; Omigbodun, F.T.; Olawumi, M.A. Medical additive manufacturing then, now, and will. In Medical Additive Manufacturing: Concepts and Fundamentals; Elsevier: Amsterdam, The Netherlands, 2024; pp. 381–400. [Google Scholar] [CrossRef]
- Kelly, C.; Adams, S.B. 3D printing materials and technologies for orthopaedic applications. J. Orthop. Trauma. 2024, 38, S9–S12. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.B.; Chen, S.; Sun, X. Advancements in polymer nanocomposite manufacturing: Revolutionizing medical breakthroughs via additive manufacturing. Polym. Bull. 2024, 81, 9465–9517. [Google Scholar] [CrossRef]
- Sarah, R.; Woods, P.; Bae, J.; Goyal, K.; Habib, M.D.A. An effort to three-dimensionally fabricate finger prosthesis using hybrid materials with integrated tactile sensing. In Proceedings of the IISE Annual Conference and Expo 2024, Montreal, Canada, 18–21 May 2024. [Google Scholar]
- Habib, A.; Goyal, K.; Pervaiz, S.; Bae, J.H. Towards natural movement: Integrating sustainable materials with hybrid 3D printing techniques and in-house-developed smart sensors. In Proceedings of the ASME International Mechanical Engineering Congress and Exposition (IMECE), Portland, OR, USA, 17–21 November 2024; Volume 4, p. V004T06A020. [Google Scholar] [CrossRef]
- De Vivo Nicoloso, L.G.; Pelz, J.; Barrack, H.; Kuester, F. Towards 3D printing of a monocoque transtibial prosthesis using a bio-inspired design workflow. Rapid Prototyp. J. 2021, 27, 67–80. [Google Scholar] [CrossRef]
- Kalidindi, S. The role of three-dimensional (3D) printing in plastic and reconstructive surgery: Innovations and applications. Eur. J. Plast. Surg. 2024, 47, 96. [Google Scholar] [CrossRef]
- Maroti, P.; Schlegl, A.T.; Nagy, B.; Toth, L.; Bogar, P.; Jozsa, G.; Rendeki, S.; Mallakpour, S.; Hussain, C.M. Additive manufacturing in limb prosthetics and orthotics: The past, present and future of 3D printing orthopedic assistive devices. In Medical Additive Manufacturing: Concepts and Fundamentalsi; Elsevier: Amsterdam, The Netherlands, 2024; pp. 179–207. [Google Scholar] [CrossRef]
- Mordà, F.; Basile, G.; Villafañe, J.H.; Grassi, F.A.; Leigheb, M. 3D printing in orthopedic surgery. Chirurgia 2023, 36, 384–389. [Google Scholar] [CrossRef]
- Boffano, M.; Aprato, A.; Piana, R. Indications: Didactical use of 3D printing, surgical didactical use, surgical planning, patient information, custom-made prosthesis, spacer and template, external prosthesis, cast. In 3D Printing in Bone Surgery; Springer International Publishing: Cham, Switzerland, 2022; pp. 1–12. [Google Scholar] [CrossRef]
- Choy, W.J.; Mobbs, R.J.; Wilcox, B.; Phan, S.; Phan, K.; Sutterlin, C.E. III. Reconstruction of thoracic spine using a personalized 3D-printed vertebral body in adolescent. J. Orthop. Surg. 2024, 42, 546–552. [Google Scholar] [CrossRef]
- Pugliese, R.; Beltrami, B.; Regondi, S.; Lunetta, C. Polymeric biomaterials for 3D printing in medicine: An overview. Ann. 3D Print. Med. 2021, 2, 100011. [Google Scholar] [CrossRef]
- Qu, Z.; Yue, J.; Song, N.; Li, S. Innovations in three-dimensional-printed individualized bone prosthesis materials: Revolutionizing orthopedic surgery: A review. Int. J. Surg. 2024, 110, 6748–6762. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.S.; Beygi, B.H.; Zheng, Y. Materials for exoskeletal orthotic and prosthetic systems. In Encyclopedia of Biomedical Engineering; Elsevier: Amsterdam, The Netherlands, 2019; pp. 352–367. [Google Scholar] [CrossRef]
- Kim, S.; Yalla, S.V.; Shetty, S.; Rosenblatt, N.J. Structural integrity of custom-designed additive manufactured prosthetic sockets compared to traditional sockets. Results Mater. 2024, 21, 100549. [Google Scholar] [CrossRef]
- Zahid, M.J.; Mavani, P.; Awuah, W.A.; Alabdulrahman, M.; Punukollu, R.; Kundu, A.; Mago, A.; Maher, K.; Adebusoye, F.T.; Khan, T.N. Sculpting the future: A narrative review of 3D printing in plastic surgery and prosthetic devices. Health Sci. Rep. 2024, 7, e2205. [Google Scholar] [CrossRef]
- Lee, J.; Nkama, C.; Yusuf, H.; Maina, J.; Ikuzwe, J.; Byiringiro, J.; Busogi, M.; Tucker, C. Increasing accessibility of 3D-printed customized prosthetics in resource-constrained communities. In Proceedings of the ASME Design Engineering Technical Conference 2024, Washington, DC, USA, 25–28 August 2024; Volume 3B-2024, p. v03bt00a024. [Google Scholar] [CrossRef]
- Francis, V.; Singh, S.K.; Bhonde, R.G.; Tichkule, Y.H.; Gupta, V.S.; Farande, S.P. Adaptation of 3D printing technology for fabrication of economical upper limb prostheses. In Advances in Industrial and Production Engineering: Select Proceedings of FLAME 2020; Springer: Singapore, 2021; pp. 861–868. [Google Scholar] [CrossRef]
- van der Stelt, M.; Verhulst, A.C.; Vas Nunes, J.H.; Koroma, T.A.R.; Nolet, W.W.E.; Slump, C.H.; Grobusch, M.P.; Maal, T.J.J.; Brouwers, L. Improving lives in three dimensions: The feasibility of 3D printing for creating personalized medical AIDS in a rural area of Sierra Leone. Am. J. Trop. Med. Hyg. 2020, 102, 905–909. [Google Scholar] [CrossRef]
- Hofmann, M.; Harris, J.; Hudson, S.E.; Mankoff, J. Helping hands: Requirements for a prototyping methodology for upper-limb prosthetics users. In Proceedings of the Conference on Human Factors in Computing Systems, San Jose, CA, USA, 7–12 May 2016; pp. 1769–1780. [Google Scholar] [CrossRef]
- Copeland, C.; Reyes, C.C.; Peck, J.L.; Srivastava, R.; Zuniga, J.M. Functional performance and patient satisfaction comparison between a 3D printed and a standard transradial prosthesis: A case report. BioMedical Eng. Online 2022, 21, 7. [Google Scholar] [CrossRef]
- Choonara, Y.E.; du Toit, L.C.; Kumar, P.; Kondiah, P.P.; Pillay, V. 3D-printing and the effect on medical costs: A new era? Expert Rev. Pharmacoecon. Outcomes Res. 2016, 16, 23–32. [Google Scholar] [CrossRef]
- Generalova, A.N.; Vikhrov, A.A.; Prostyakova, A.I.; Apresyan, S.V.; Stepanov, A.G.; Myasoedov, M.S.; Oleinikov, V.A. Polymers in 3D printing of external maxillofacial prostheses and in their retention systems. Int. J. Pharm. 2024, 657, 124181. [Google Scholar] [CrossRef]
- Das, A.; Awasthi, P.; Jain, V.; Banerjee, S.S. 3D printing of maxillofacial prosthesis materials: Challenges and opportunities. Bioprinting 2023, 32, e00282. [Google Scholar] [CrossRef]
- Amalraj, A.R.; Balasubramanium, M.; Reddy, V.; Chidambaranathan, A.S.; John, P. Digitally made nasal prosthesis: A new frontier in facial reconstruction—Case report. Oral. Oncol. Rep. 2024, 12, 100679. [Google Scholar] [CrossRef]
- Morrison, R.J.; Kashlan, K.N.; Flanagan, C.L.; Wright, J.K.; Green, G.E.; Hollister, S.J.; Weatherwax, K.J. Regulatory considerations in the design and manufacturing of implantable 3D-printed medical devices. Clin. Transl. Sci. 2015, 8, 594–600. [Google Scholar] [CrossRef]
- Elango, V.; Murugappan, M.; Vetrivel, K.; Yusuf, M.; Nikam, K.D. 3D printing in the pharmaceutical industry: A special consideration on medical device and its applications. Int. J. Appl. Pharm. 2025, 17, 1–11. [Google Scholar] [CrossRef]
- Hourd, P.; Medcalf, N.; Segal, J.; Williams, D.J. A 3D bioprinting exemplar of the consequences of the regulatory requirements on customized processes. Regen. Med. 2015, 10, 863–883. [Google Scholar] [CrossRef] [PubMed]
- Kırtaş, O.; Samur, E. Somatosensation in soft and anthropomorphic prosthetic hands and legs. In Somatosensory Feedback for Neuroprosthetics; Elsevier: Amsterdam, The Netherlands, 2021; pp. 561–588. [Google Scholar] [CrossRef]
- Jeong, M.; Radomski, K.; Lopez, D.; Liu, J.T.; Lee, J.D.; Lee, S.J. Materials and Applications of 3D Printing Technology in Dentistry: An Overview. Dent. J. 2024, 12, 1. [Google Scholar] [CrossRef]
- Borthakur, P.P.; Sarmah, R.R. An Introduction to Additive Manufacturing (3D Printing). In Advances in Engineering Technology; Singh, J., Ed.; Akinik Publishers: Delhi, India, 2021; Volume 1, pp. 1–11. [Google Scholar] [CrossRef]
- Tack, P.; Victor, J.; Gemmel, P.; Annemans, L. 3D-printing techniques in a medical setting: A systematic literature review. BioMed. Eng. OnLine 2016, 15, 115. [Google Scholar] [CrossRef]
- Gao, T.; Rivlin, M.; Abraham, J.A. Three-dimensional printing technology and role for custom implants in orthopedic oncology. Tech. Orthop. 2018, 33, 166–174. [Google Scholar] [CrossRef]
- Hermida-Ochoa, J.C.; Beltrán-Fernández, J.A.; Andrade, J.L.C.; Hernández-Gómez, L.H.; Uribe-Cortés, T.B.; Moreno-Garibaldi, P. Tridimensional design and printing techniques to obtain personalized prosthetic components for specific cases involving bone defects. In Advanced Structured Materials; Springer: Berlin/Heidelberg, Germany, 2021; Volume 146, pp. 181–191. [Google Scholar] [CrossRef]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Borthakur, P.P. The Role and Future Directions of 3D Printing in Custom Prosthetic Design. Eng. Proc. 2024, 81, 10. https://doi.org/10.3390/engproc2024081010
Borthakur PP. The Role and Future Directions of 3D Printing in Custom Prosthetic Design. Engineering Proceedings. 2024; 81(1):10. https://doi.org/10.3390/engproc2024081010
Chicago/Turabian StyleBorthakur, Partha Protim. 2024. "The Role and Future Directions of 3D Printing in Custom Prosthetic Design" Engineering Proceedings 81, no. 1: 10. https://doi.org/10.3390/engproc2024081010
APA StyleBorthakur, P. P. (2024). The Role and Future Directions of 3D Printing in Custom Prosthetic Design. Engineering Proceedings, 81(1), 10. https://doi.org/10.3390/engproc2024081010






