Additive Manufacturing of a Customized Printed Ankle–Foot Orthosis: Design, Manufacturing, and Mechanical Evaluation †
Abstract
:1. Introduction
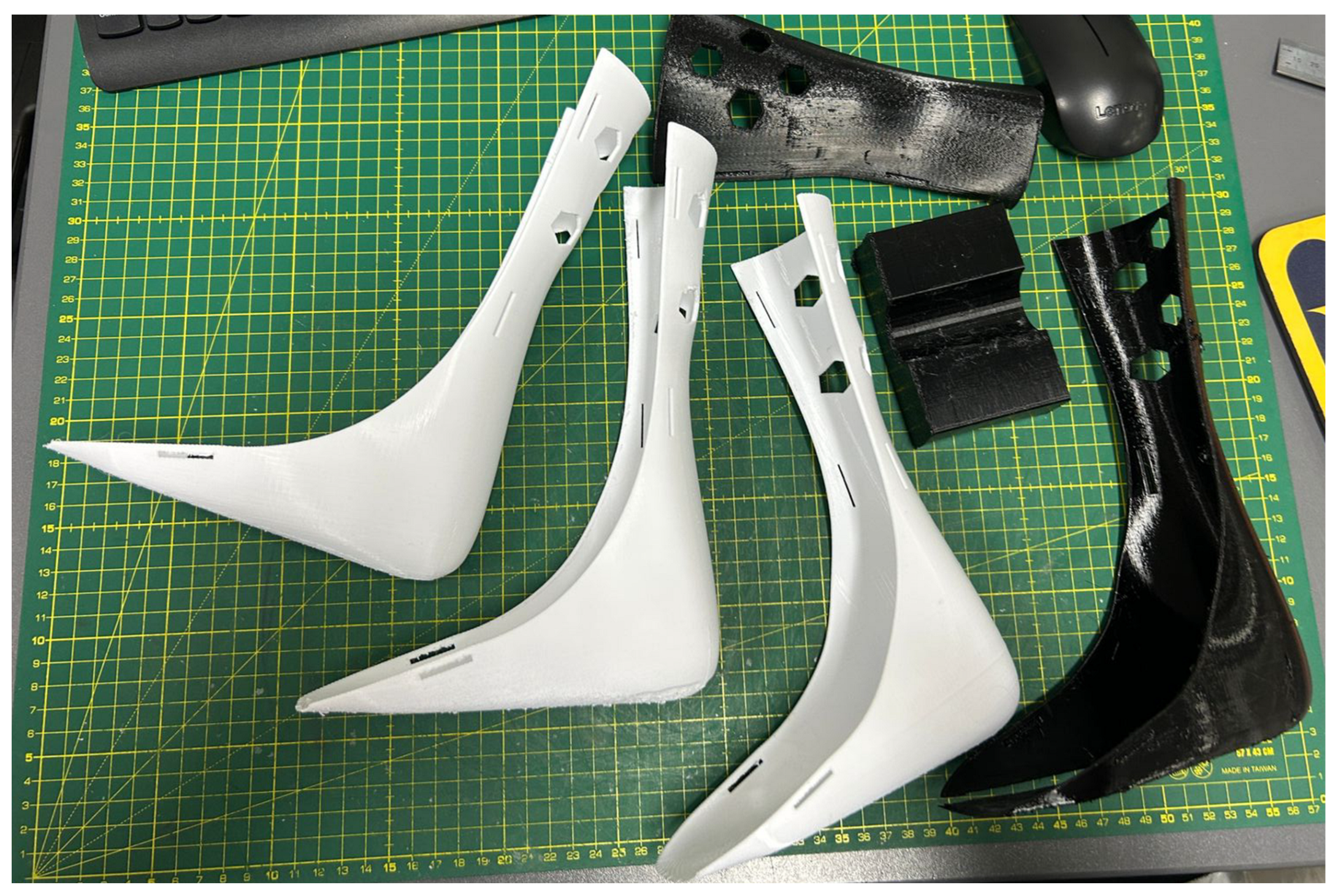
2. Materials and Methods
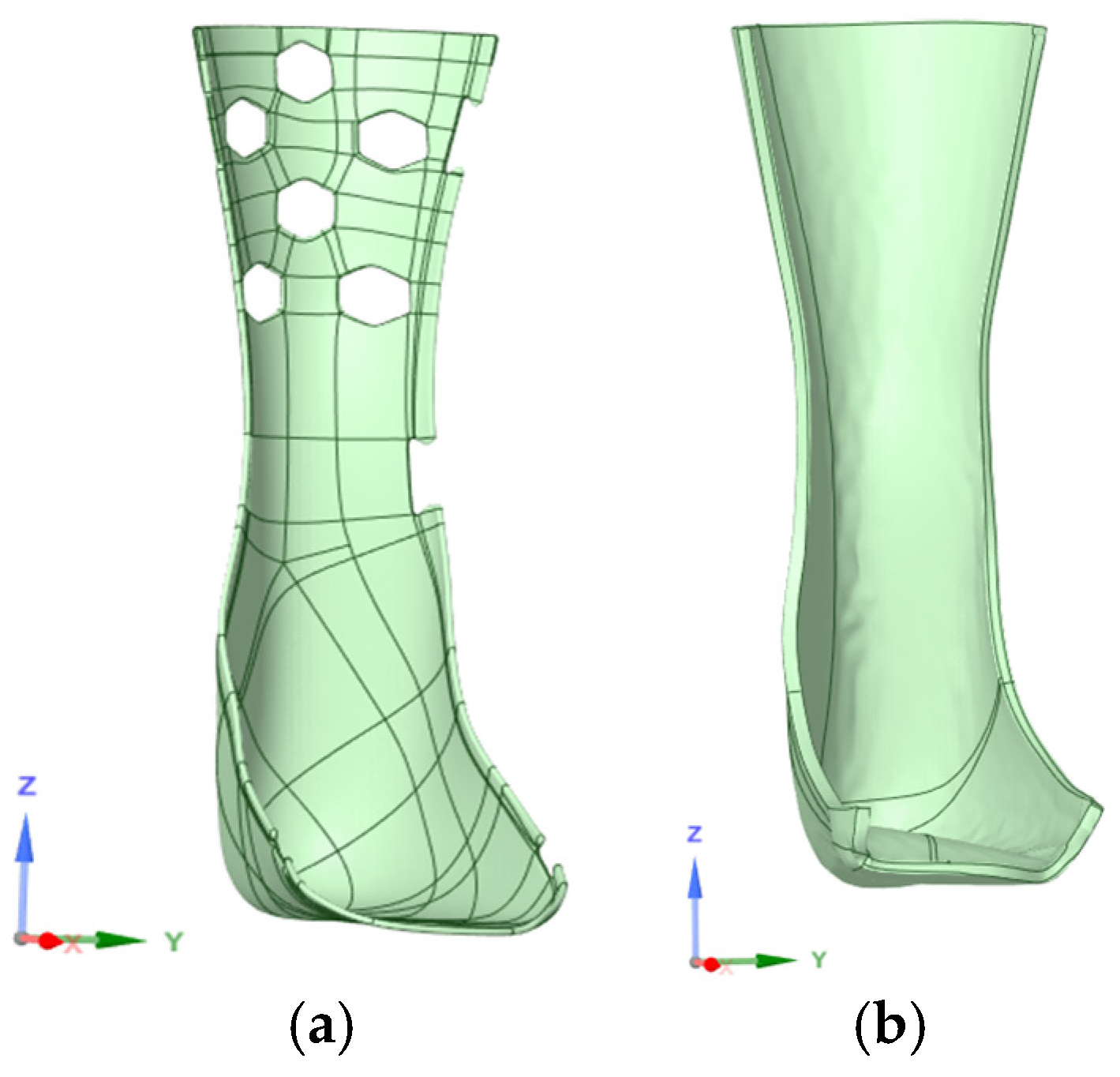
2.1. Fabrication and Modeling
2.2. Evaluation Protocols
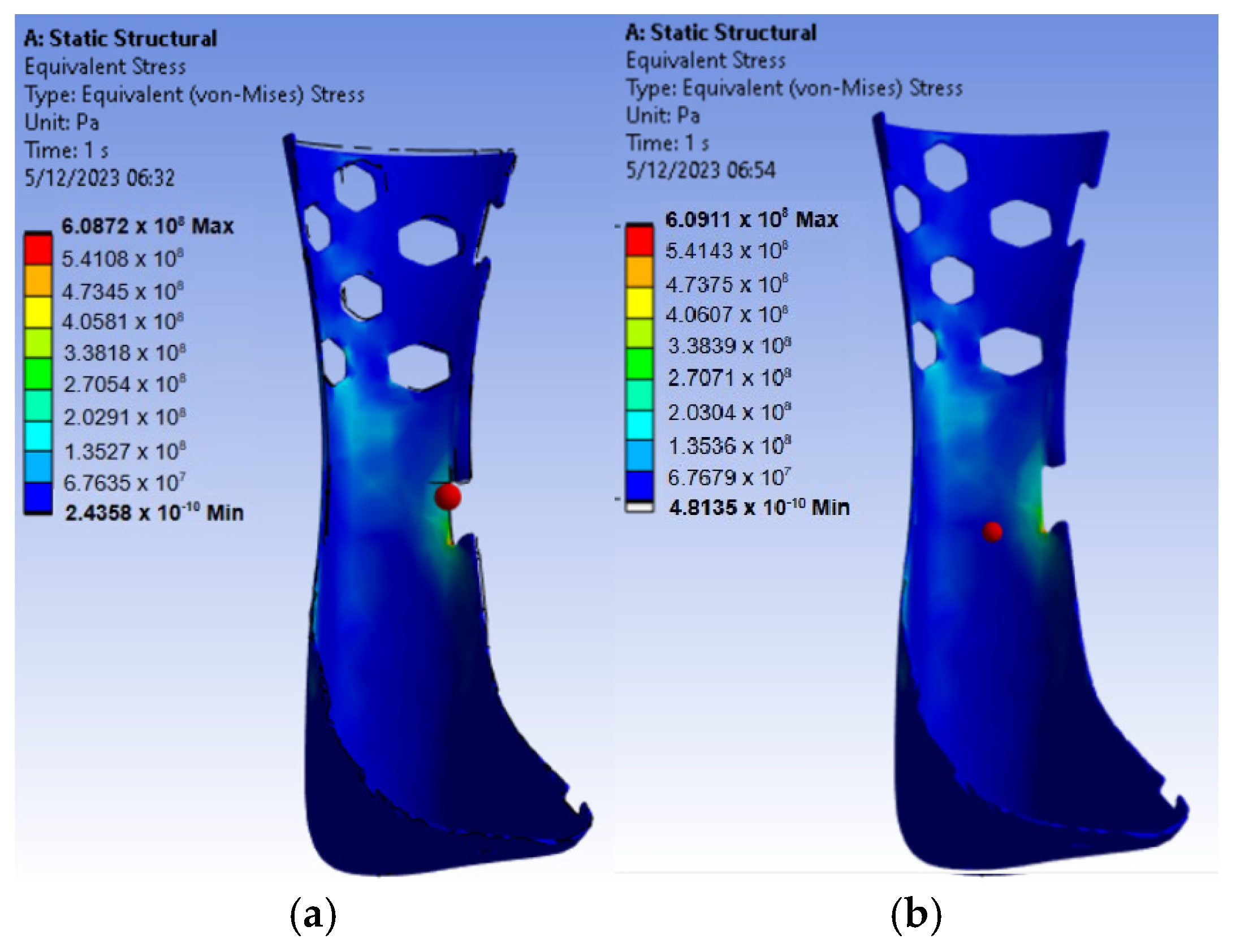
2.2.1. Computer Simulation
2.2.2. Mechanical Testing
3. Results and Discussion
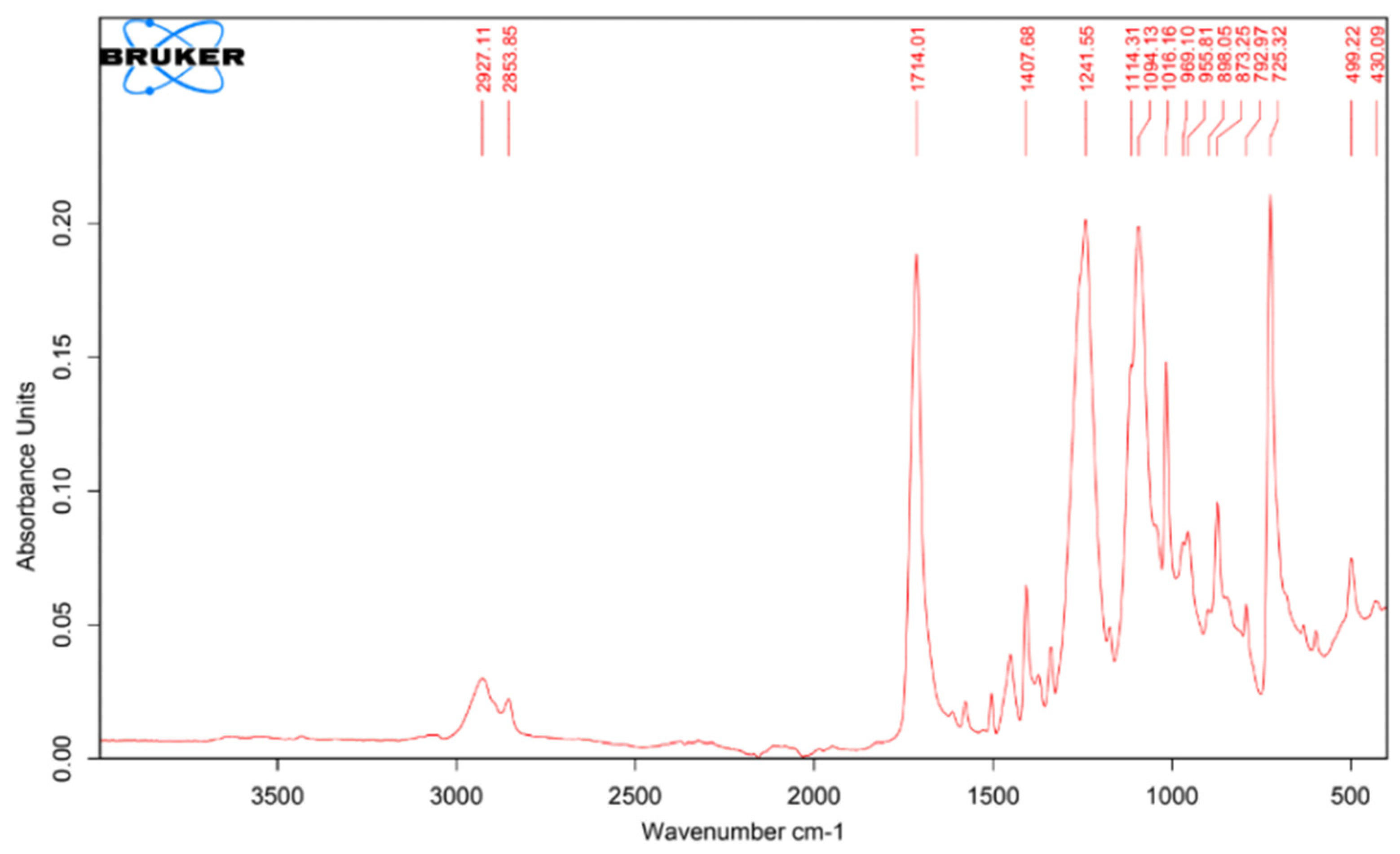
3.1. Material Characterization
3.1.1. Tensile Testing
3.1.2. Melt Flow Index
3.1.3. Fourier-Transform Infrared Spectrophotometry
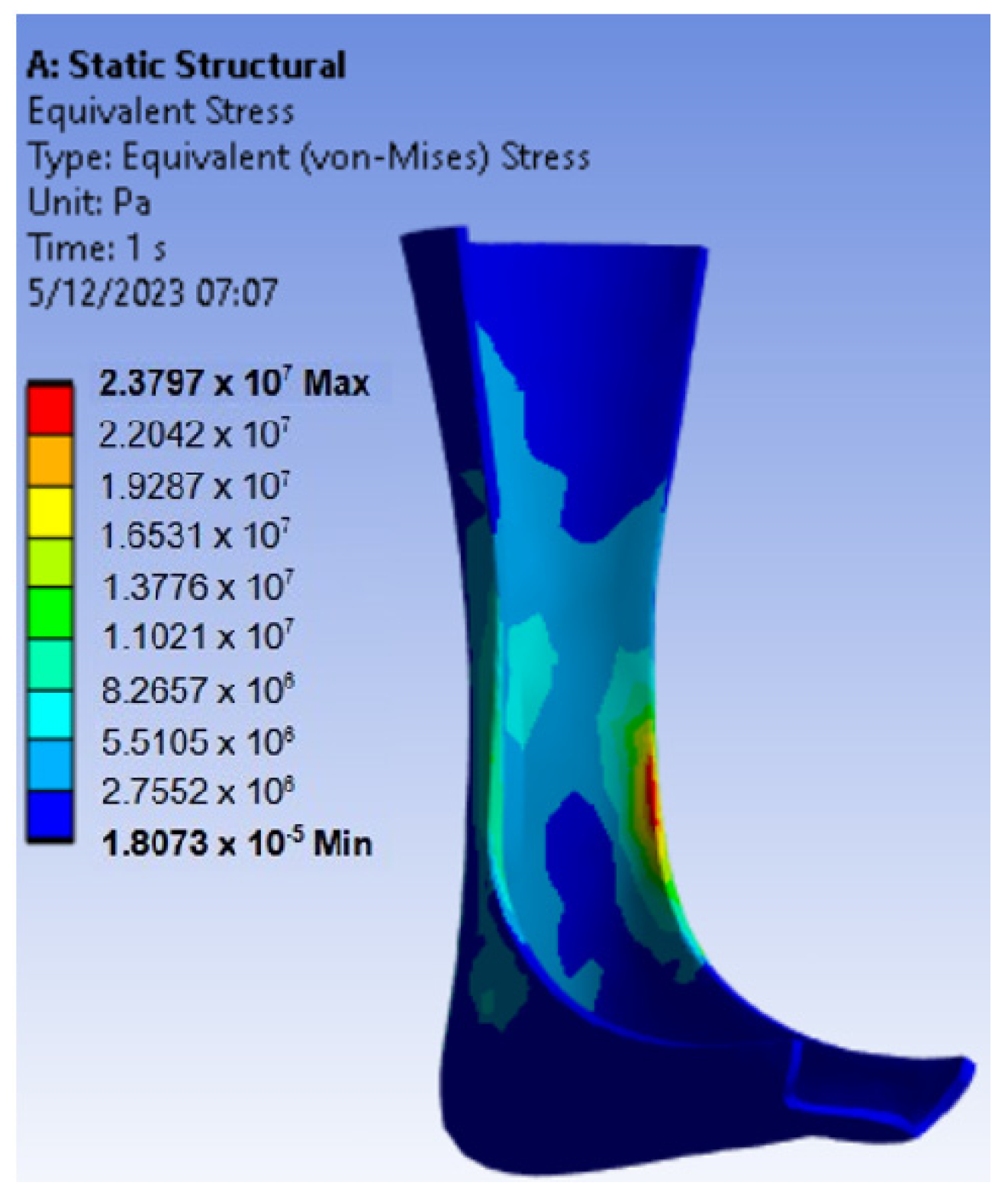
3.2. Mechanical Simulation
3.3. Results of Mechanical Testing on 3D-Printed AFOs
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Catalán, E.; Sierra, M.; Ceballos, J.; Rendón, M. Tratamiento de esguince de tobillo grado II en adultos laboralmente activos: Inmovilización contra vendaje funcional. Rev. De Sanid. Mil. 2018, 72, 240–245. [Google Scholar]
- Esguince de Tobillo—Mayo Clinic. Available online: https://www.mayoclinic.org/es/diseases-conditions/sprained-ankle/symptoms-causes/syc-20353225 (accessed on 14 September 2023).
- Rincón Cardozo, D.F.; Camacho Casas, J.A.; Sauza Rodríguez, N.; Rincón Cardozo, P.A. Abordaje del esguince de tobillo para el médico general. Rev. De La Univ. Ind. De Santander 2015, 47, 85–92. [Google Scholar]
- Tratamiento con Cirugía en el Esguince de Tobillo—Cirugía Pie y Tobillo por Dr. Ballester. Available online: https://www.cirugiapie.com/blog/cirugia-en-esguince-de-tobillo (accessed on 15 September 2023).
- Pérez-Caballer, A.J.; Sanz-Hospital, J.; Delgado, P. Tratamiento quirúrgico de la inestabilidad lateral crónica de tobillo. Rev. Española De Cirugía Ortopédica Y Traumatol. 2004, 48, 53–59. [Google Scholar]
- Castillo Gonzalez, S.A.; Pulido Talero, W.E.; Castañeda Jerez, C.E. Diseño e impresión 3D de órtesis para tratamiento de ligamento cruzado posterior/anterior como herramienta de aplicación en la industria 4.0. Av. Investig. En Ing. 2022, 19, 27–43. [Google Scholar] [CrossRef]
- Lin, Y.-C.; Huang, L.-Y.; Chen, C.-S. Strength Evaluation and Modification of a 3D Printed Anterior Ankle Foot Orthoses. Appl. Sci. 2020, 10, 7289. [Google Scholar] [CrossRef]
- Cha, Y.H.; Lee, K.H.; Ryu, H.J.; Joo, I.W.; Seo, A.; Kim, D.-H.; Kim, S.J. Ankle-Foot Orthosis Made by 3D Printing Technique and Automated Design Software. Appl. Bionics Biomech. 2017, 2017, 9610468. [Google Scholar] [CrossRef] [PubMed]
- Del Maso, A.; Cosmi, F. 3D-printed ankle-foot orthosis: A design method. Mater. Today Proc. 2019, 12, 252–261. [Google Scholar] [CrossRef]
- Lukaszewski, K.; Raj, R.; Karwasz, A. Mechanical Evaluation of PET-G 3D-Printed Wrist-Hand Orthosis: An Integrated Experimental and Numerical Approach. Materials 2023, 16, 6132. [Google Scholar] [CrossRef] [PubMed]
- Batista, M.; Lagomazzini, J.M.; Ramirez-Peña, M.; Vazquez-Martinez, J.M. Mechanical and Tribological Performance of Carbon Fiber-Reinforced PETG for FFF Applications. Appl. Sci. 2023, 13, 12701. [Google Scholar] [CrossRef]
- Máquina de Ensayos Universal ProLine. Available online: https://www.zwickroell.com/es/productos/maquinas-de-ensayos-de-materiales-estaticas/maquinas-de-ensayos-universales-para-aplicaciones-estaticas/proline/ (accessed on 12 October 2023).
- Doronin, F.; Rudakova, A.; Rytikov, G.; Nazarov, V. Simple Determination of the Melt Flow Index of Composite Polymer Filaments Used in Material Extrusion Additive Manufacturing. Coatings 2023, 13, 1592. [Google Scholar] [CrossRef]
- “Medidor del índice de fluidez Mflow”, ZwickRoell. Available online: https://www.zwickroell.com/es/productos/medidores-del-indice-de-fluidez/medidor-del-indice-de-fluidez-mflow/ (accessed on 18 October 2023).
- Latko-Durałek, P.; Dydek, K.; Boczkowska, A. Thermal, Rheological and Mechanical Properties of PETG/rPETG Blends. J. Polym. Environ. 2019, 27, 2600–2606. [Google Scholar] [CrossRef]
- “Espectrómetros FT-IR de Rutina”, Bruker. Available online: https://www.bruker.com/es/products-and-solutions/infrared-and-raman/ft-ir-routine-spectrometer.html (accessed on 8 November 2023).
- Sense Scanner. Available online: https://support.3dsystems.com/s/article/Sense-Scanner?language=en_US (accessed on 8 November 2023).
- Meshmixer. Available online: https://meshmixer.com/ (accessed on 15 November 2023).
- Peirone, M. Using Fusion 360 to Design Patient-Specific Prosthetic and Orthotic Devices. Autodesk. Available online: https://static.au-uw2-prd.autodesk.com/Class_Handout_SD500053_ClassHandout-SD500053-Peirone-AU2021.pdf (accessed on 15 November 2023).
- Song, P.; Qi, Y.M.; Cai, D.C. Research and Application of Autodesk Fusion 360 in Industrial Design. IOP Conf. Ser. Mater. Sci. Eng. 2018, 359, 012037. [Google Scholar] [CrossRef]
- Ultimaker Cura. Available online: https://ultimaker.com/software/ultimaker-cura/ (accessed on 5 December 2023).
- Filamento para Impresión 3d en PET-G Azul. Available online: https://bimek3d.com/filamentos-para-impresion-3d/pet-g/filamento-para-impresi%C3%B3n-3d-en-pet-g-azul-detail (accessed on 5 December 2023).
- Ielapi, A.; Forward, M.; De Beule, M. Computational and Experimental Evaluation of the Mechanical Properties of Ankle Foot Orthoses: A Literature Review. Prosthet. Orthot. Int. 2019, 43, 339–348. [Google Scholar] [CrossRef] [PubMed]
- Raj, R.; Dixit, A.R.; Łukaszewski, K.; Wichniarek, R.; Rybarczyk, J.; Kuczko, W.; Górski, F. Numerical and Experimental Mechanical Analysis of Additively Manufactured Ankle–Foot Orthoses. Materials 2022, 15, 6130. [Google Scholar] [CrossRef] [PubMed]
- Mansilla, P. Análisis de los Parámetros del Proceso de Impresión 3D FGF. Aplicación a la Fabricación de Mobiliario; Universidad de Valladolid: Valladolid, Spain, 2023. [Google Scholar]
- “Tablas de Espectroscopía”, Universidad de Granada. Available online: https://www.ugr.es/~quiored/lab/tablas_espec/ir.htm (accessed on 5 December 2023).


| Parameter | Value | Observations |
|---|---|---|
| Angle with respect to the base | −15° | - |
| Layer height | 0.28 mm | - |
| Line width | 0.44 mm | - |
| Wall thickness | 1.76 mm | 4 wall lines |
| Horizontal expansion | 1 mm | - |
| Top layers | 4 | - |
| Bottom layers | 3 | - |
| Infill density | 15% | Gyroid pattern |
| Printing temperature | 240 °C | According to the literature, an optimal temperature ranges from 230 °C to 250 °C [22] |
| Print speed | 65 m/s | |
| Support density | 6% | Zig Zag Pattern |
| Adhesion type | Brim | |
| Conical support | Enabled | 30° support angle and 5 mm minimum width |
| Material | Density (kg/m3) | Young’s Modulus (MPa) | Poisson Coefficient | Tensile Yield Strength (MPa) |
|---|---|---|---|---|
| PET | 1339 | 2898 | 0.38 | 52.4 |
| PETG | 1270 | 2035.81 | 0.35 | 51.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hernández, A.; Huarcaya, V.; Acuña, Í.; Marcos, G.; Ccama, G.; Ochoa, E.; Molina, A.R. Additive Manufacturing of a Customized Printed Ankle–Foot Orthosis: Design, Manufacturing, and Mechanical Evaluation. Eng. Proc. 2025, 83, 24. https://doi.org/10.3390/engproc2025083024
Hernández A, Huarcaya V, Acuña Í, Marcos G, Ccama G, Ochoa E, Molina AR. Additive Manufacturing of a Customized Printed Ankle–Foot Orthosis: Design, Manufacturing, and Mechanical Evaluation. Engineering Proceedings. 2025; 83(1):24. https://doi.org/10.3390/engproc2025083024
Chicago/Turabian StyleHernández, Adrián, Valery Huarcaya, Ítalo Acuña, Gabriel Marcos, Gianella Ccama, Emilio Ochoa, and Andoni R. Molina. 2025. "Additive Manufacturing of a Customized Printed Ankle–Foot Orthosis: Design, Manufacturing, and Mechanical Evaluation" Engineering Proceedings 83, no. 1: 24. https://doi.org/10.3390/engproc2025083024
APA StyleHernández, A., Huarcaya, V., Acuña, Í., Marcos, G., Ccama, G., Ochoa, E., & Molina, A. R. (2025). Additive Manufacturing of a Customized Printed Ankle–Foot Orthosis: Design, Manufacturing, and Mechanical Evaluation. Engineering Proceedings, 83(1), 24. https://doi.org/10.3390/engproc2025083024






