Neurological and Psychiatric Symptoms of COVID-19: A Narrative Review
Abstract
:1. Introduction
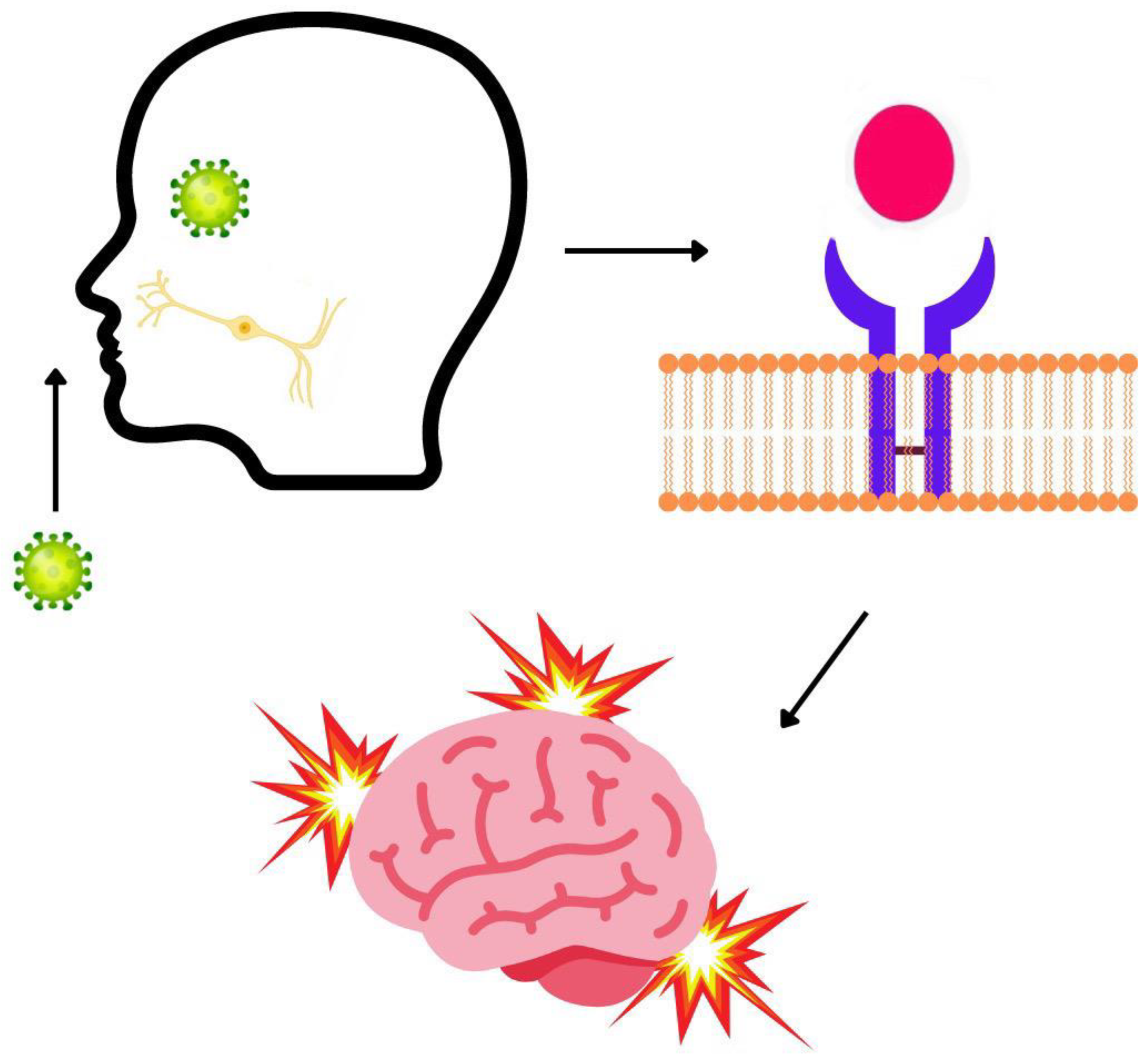
2. Neurological and Neuropsychiatric Symptoms of COVID-19
3. Daily Persistent Headache: Treatment and COVID-19 Relation
3.1. New Daily Persistent Headache
3.2. Proposed Pathophysiology
3.3. Treatment
3.4. Fatigue
3.5. Proposed Treatment of Fatigue
4. Psychiatric Symptoms and COVID-19 Relation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lopez-Leon, S.; Wegman-Ostrosky, T.; Perelman, C.; Sepulveda, R.; Rebolledo, P.A.; Cuapio, A.; Villapol, S. More than 50 long-term effects of COVID-19: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 16144. [Google Scholar] [CrossRef] [PubMed]
- Carod-Artal, F.J. Post-COVID-19 syndrome: Epidemiology, diagnostic criteria and pathogenic mechanisms involved. Rev. Neurol. 2021, 72, 384–396. [Google Scholar]
- Neuropsychiatric Aspects of COVID-19 Pandemic: A Selective Review. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7261092/ (accessed on 16 January 2022).
- Bougakov, D.; Podell, K.; Goldberg, E. Multiple Neuroinvasive Pathways in COVID-19. Mol. Neurobiol. 2020, 58, 564–575. [Google Scholar] [CrossRef] [PubMed]
- Roy, D.; Ghosh, R.; Dubey, S.; Dubey, M.J.; Benito-León, J.; Ray, B.K. Neurological and Neuropsychiatric Impacts of COVID-19 Pandemic. Can. J. Neurol. Sci. 2020, 48, 9–24. [Google Scholar] [CrossRef] [PubMed]
- Frontiers|Cognitive and Neuropsychiatric Manifestations of COVID-19 and Effects on Elderly Individuals with Dementia|Aging Neuroscience. Available online: https://www.frontiersin.org/articles/10.3389/fnagi.2020.588872/full (accessed on 16 January 2022).
- Kumar, S.; Veldhuis, A.; Malhotra, T. Neuropsychiatric and Cognitive Sequelae of COVID-19. Front. Psychol. 2021, 12, 577529. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.-H.; Chen, Y.; Wang, Q.-H.; Wang, L.-R.; Jiang, L.; Yang, Y.; Chen, X.; Li, Y.; Cen, Y.; Xu, C.; et al. One-Year Trajectory of Cognitive Changes in Older Survivors of COVID-19 in Wuhan, China. JAMA Neurol. 2022, e220461. [Google Scholar] [CrossRef]
- Kang, Y.; Xu, S. Comprehensive overview of COVID-19 based on current evidence. Dermatol. Ther. 2020, 33, e13525. [Google Scholar] [CrossRef]
- Higgins, V.; Sohaei, D.; Diamandis, E.P.; Prassas, I. COVID-19: From an acute to chronic disease? Potential long-term health consequences. Crit. Rev. Clin. Lab. Sci. 2020, 58, 297–310. [Google Scholar] [CrossRef]
- Wang, F.; Kream, R.M.; Stefano, G.B. Long-Term Respiratory and Neurological Sequelae of COVID-19. Med. Sci. Monit. 2020, 26, e928996. [Google Scholar] [CrossRef]
- Barrantes, F.J. Central Nervous System Targets and Routes for SARS-CoV-2: Current Views and New Hypotheses. ACS Chem. Neurosci. 2020, 11, 2793–2803. [Google Scholar] [CrossRef]
- Mahalakshmi, A.M.; Ray, B.; Tuladhar, S.; Bhat, A.; Paneyala, S.; Patteswari, D.; Sakharkar, M.K.; Hamdan, H.; Ojcius, D.M.; Bolla, S.R.; et al. Does COVID-19 contribute to development of neurological disease? Immun. Inflamm. Dis. 2020, 9, 48–58. [Google Scholar] [CrossRef] [PubMed]
- Baig, A.M. Deleterious Outcomes in Long-Hauler COVID-19: The Effects of SARS-CoV-2 on the CNS in Chronic COVID Syndrome. ACS Chem. Neurosci. 2020, 11, 4017–4020. [Google Scholar] [CrossRef] [PubMed]
- Immediate and Long-Term Consequences of COVID-19 Infections for the Development of Neurological Disease. Available online: https://pubmed.ncbi.nlm.nih.gov/32498691/ (accessed on 21 February 2022).
- Porta-Etessam, J.; Matías-Guiu, J.A.; González-García, N.; Iglesias, P.G.; Santos-Bueso, E.; Arriola-Villalobos, P.; García-Azorín, D.; Matías-Guiu, J. Spectrum of Headaches Associated With SARS-CoV-2 Infection: Study of Healthcare Professionals. Headache 2020, 60, 1697–1704. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.; Gu, J.; Hou, P.; Zhang, L.; Bai, Y.; Guo, Z.; Wu, H.; Zhang, B.; Li, P.; Zhao, X. Incidence, clinical characteristics and prognostic factor of patients with COVID-19: A systematic review and meta-analysis. medRxiv 2020. [Google Scholar] [CrossRef]
- Chan, C.; Wei, D.Y.; Goadsby, P.J. Biochemical Modulation and Pathophysiology of Migraine. J. Neuro-Ophthalmol. Off. J. N. Am. Neuro-Ophthalmol. Soc. 2019, 39, 470–479. [Google Scholar] [CrossRef]
- COVID-19: Consider Cytokine Storm Syndromes and Immunosuppression—The Lancet. Available online: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30628-0/fulltext (accessed on 16 January 2022).
- Caronna, E.; Alpuente, A.; Torres-Ferrus, M.; Pozo-Rosich, P. Toward a better understanding of persistent headache after mild COVID-19: Three migraine-like yet distinct scenarios. Headache 2021, 61, 1277–1280. [Google Scholar] [CrossRef]
- Yamani, N.; Olesen, J. New daily persistent headache: A systematic review on an enigmatic disorder. J. Headache Pain 2019, 20, 80. [Google Scholar] [CrossRef] [Green Version]
- Prakash, S.; Patel, N.; Golwala, P.; Patell, R. Post-infectious headache: A reactive headache? J. Headache Pain 2011, 12, 467–473. [Google Scholar] [CrossRef] [Green Version]
- Rehberger, O. What Is the Difference between Chronic Migraine and NDPH? Available online: https://www.migraineagain.com/difference-ndph-chronic-migraine/ (accessed on 16 November 2021).
- Caronna, E.; Ballvé, A.; Llauradó, A.; Gallardo, V.J.; Ariton, D.M.; Lallana, S.; López Maza, S.; Olivé Gadea, M.; Quibus, L.; Restrepo, J.L.; et al. Headache: A striking prodromal and persistent symptom, predictive of COVID-19 clinical evolution. Cephalalgia 2020, 40, 1410–1421. [Google Scholar] [CrossRef]
- Mutiawati, E.; Syahrul, S.; Fahriani, M.; Fajar, J.K.; Mamada, S.S.; Maliga, H.A.; Samsu, N.; Ilmawan, M.; Purnamasari, Y.; Asmiragani, A.A.; et al. Global prevalence and pathogenesis of headache in COVID-19: A systematic review and meta-analysis. F1000Research 2020, 9, 1316. [Google Scholar] [CrossRef]
- Dono, F.; Consoli, S.; Evangelista, G.; D’Apolito, M.; Russo, M.; Carrarini, C.; Calisi, D.; De Rosa, M.; Di Pietro, M.; De Angelis, M.V.; et al. New daily persistent headache after SARS-CoV-2 infection: A report of two cases. Neurol. Sci. 2021, 42, 3965–3968. [Google Scholar] [CrossRef] [PubMed]
- Takase, Y.; Nakano, M.; Tatsumi, C.; Matsuyama, T. Clinical Features, Effectiveness Of Drug-Based Treatment, and Prognosis of New Daily Persistent Headache (NDPH): 30 Cases in Japan. Cephalalgia 2004, 24, 955–959. [Google Scholar] [CrossRef] [PubMed]
- Prakash, S.; Shah, N.D. Post-infectious new daily persistent headache may respond to intravenous methylprednisolone. J. Headache Pain 2010, 11, 59–66. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ali, A.; Kriegler, J.; Tepper, S.; Vij, B. New Daily Persistent Headache (NDPH) & OnabotulinumtoxinA Therapy (P3.114). Neurology 2018, 90. Available online: https://n.neurology.org/content/90/15_Supplement/P3.114 (accessed on 16 November 2021).
- Townsend, L.; Dyer, A.H.; Jones, K.; Dunne, J.; Mooney, A.; Gaffney, F.; O’Connor, L.; Leavy, D.; O’Brien, K.; Dowds, J.; et al. Persistent fatigue following SARS-CoV-2 infection is common and independent of severity of initial infection. PLoS ONE 2020, 15, e0240784. [Google Scholar] [CrossRef]
- Feasibility of Vitamin C in the Treatment of Post Viral Fatigue with Focus on Long COVID, Based on a Systematic Review of IV Vitamin C on Fatigue. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8066596/ (accessed on 16 January 2022).
- SStavem, K.; Ghanima, W.; Olsen, M.; Gilboe, H.; Einvik, G. Prevalence and Determinants of Fatigue after COVID-19 in Non-Hospitalized Subjects: A Population-Based Study. Int. J. Environ. Res. Public Health 2021, 18, 2030. [Google Scholar] [CrossRef]
- Journal of Medical Internet Research—Severe Fatigue in Long COVID: Web-Based Quantitative Follow-up Study in Members of Online Long COVID Support Groups. Available online: https://www.jmir.org/2021/9/e30274 (accessed on 16 January 2022).
- Tejera, D.; Mercan, D.; Sanchez-Caro, J.M.; Hanan, M.; Greenberg, D.; Soreq, H.; Latz, E.; Golenbock, D.; Heneka, M.T. Systemic inflammation impairs microglial Aβ clearance through NLRP 3 inflammasome. EMBO J. 2019, 38, e101064. [Google Scholar] [CrossRef]
- Miners, S.; Kehoe, P.G.; Love, S. Cognitive impact of COVID-19: Looking beyond the short term. Alzheimer’s Res. Ther. 2020, 12, 170. [Google Scholar] [CrossRef]
- Lamontagne, S.J.; Winters, M.F.; Pizzagalli, D.A.; Olmstead, M.C. Post-acute sequelae of COVID-19: Evidence of mood & cognitive impairment. Brain Behav. Immun.-Health 2021, 17, 100347. [Google Scholar] [CrossRef]
- Ardila, A.; Lahiri, D. Executive dysfunction in COVID-19 patients. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 1377–1378. [Google Scholar] [CrossRef]
- Chacko, M.; Job, A.; Caston, F.; George, P.; Yacoub, A.; Cáceda, R. COVID-19-Induced Psychosis and Suicidal Behavior: Case Report. SN Compr. Clin. Med. 2020, 2, 2391–2395. [Google Scholar] [CrossRef] [PubMed]
- Brown, E.; Gray, R.; Lo Monaco, S.; O’Donoghue, B.; Nelson, B.; Thompson, A.; Francey, S.; McGorry, P. The potential impact of COVID-19 on psychosis: A rapid review of contemporary epidemic and pandemic research. Schizophr Res. 2020, 222, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.M.; Komisar, J.R.; Mourad, A.; Kincaid, B.R. COVID-19-associated brief psychotic disorder. BMJ Case Rep. 2020, 13, e236940. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Edinoff, A.N.; Chappidi, M.; Alpaugh, E.S.; Turbeville, B.C.; Falgoust, E.P.; Cornett, E.M.; Murnane, K.S.; Kaye, A.M.; Kaye, A.D. Neurological and Psychiatric Symptoms of COVID-19: A Narrative Review. Psychiatry Int. 2022, 3, 158-168. https://doi.org/10.3390/psychiatryint3020013
Edinoff AN, Chappidi M, Alpaugh ES, Turbeville BC, Falgoust EP, Cornett EM, Murnane KS, Kaye AM, Kaye AD. Neurological and Psychiatric Symptoms of COVID-19: A Narrative Review. Psychiatry International. 2022; 3(2):158-168. https://doi.org/10.3390/psychiatryint3020013
Chicago/Turabian StyleEdinoff, Amber N., Maithreyi Chappidi, E. Saunders Alpaugh, Bailey C. Turbeville, Evan P. Falgoust, Elyse M. Cornett, Kevin S. Murnane, Adam M. Kaye, and Alan D. Kaye. 2022. "Neurological and Psychiatric Symptoms of COVID-19: A Narrative Review" Psychiatry International 3, no. 2: 158-168. https://doi.org/10.3390/psychiatryint3020013
APA StyleEdinoff, A. N., Chappidi, M., Alpaugh, E. S., Turbeville, B. C., Falgoust, E. P., Cornett, E. M., Murnane, K. S., Kaye, A. M., & Kaye, A. D. (2022). Neurological and Psychiatric Symptoms of COVID-19: A Narrative Review. Psychiatry International, 3(2), 158-168. https://doi.org/10.3390/psychiatryint3020013








