Abstract
Epilepsy is a critical neurological condition characterized by the disturbance of the excitatory neuron network, resulting in recurrent seizures. It is a serious health problem requiring intensive attention. The present study was designed to use bibliometric analysis to assess scientific research output on pharmacogenetics in epilepsy and drug-resistant epilepsy in Morocco during 1969–2024. The main objective of this study was to analyze scientific production and research development and to introduce available solutions to manage the elevating burden of epilepsy. The strategy approach comprised a suitable search scheme to collect publications related to epilepsy using the Scopus database. All the documents retrieved were analyzed to determine several parameters, including the number of publications annually, type of documents, institution and author productivity, and relevant sources. Studies on pharmacogenetics and drug-resistant epilepsy in Morocco are limited. The findings revealed that the number of articles has increased during the last decade. Publications remain scarce, especially on pharmacogenetics and drug-resistant epilepsy, and the most widely available publications include articles on epilepsy, seizures, mental illness, and anticonvulsant agents. Based on the search strategy, a bibliometric analysis identified potential subjects for further study. Consequently, research on epilepsy is essential to fully understand the condition, but it remains insufficient, and further studies are required, particularly on the pharmacogenetics of epilepsy.
1. Introduction
Epilepsy is a major neurological disorder that affects several millions of people worldwide. It is characterized by recurrent and unpredictable seizures caused by disturbed excitatory and inhibitory neuronal discharges with multiple etiologies [1,2]. The number of people suffering from epilepsy expands daily to reach almost 65 million worldwide [3]. This neurological disorder can be divided into three categories according to a consortium of researchers composing the International League against Epilepsy: generalized seizures, focal seizures, and seizures of undetermined onset [4,5,6]. At present, there are no effective medications for achieving free seizures in patients with epilepsy or preventing disease development. Many treatment methods have been used to treat epilepsy, including antiseizure drugs (ASDs), diet, neurostimulation, and palliative surgery [7]. ASDs are the first-line treatment for epilepsy. However, ASDs treat seizures without an underlying epileptic disorder or behavioral abnormalities in epileptic patients, and they often induce serious deleterious effects [8]. Furthermore, it has been reported that approximately 30% of patients treated with ASDs develop drug-resistant epilepsy [9]. Robust evidence has shown that different patients diagnosed with the same type of epilepsy react differently to medications, leading to different consequences [10]. This phenomenon can be explained by the impact of genetic factors that are implicated in the pharmacodynamics and pharmacokinetics of antiseizure drugs [11]. Numerous factors have been identified, including drug transport proteins, enzymes that metabolize drugs, and the modification of receptors and ion channel structures [9].
Bibliometric analysis is an excellent tool for identifying scientific trends in a field [12]. It is widely used to measure the impact of scientific research and establish the structures of research fields [13]. This analysis helps create new research directions and provides more information about the state of knowledge in specific fields [12]. Using this approach, researchers can shed light on emerging topics while dissecting their evolutionary characteristics. In addition, the emphasis on empirical contributions has given rise to other research areas. This makes it more difficult to actively gather accurate data from databases to improve our understanding [14]. Recently, bibliometric analyses of pharmacogenetic and drug-resistant epilepsy have been reported in some countries, including Pakistan, Latin America, and Turkey [15,16,17]. This is the first report on the pharmacogenetics of epilepsy and drug-resistant epilepsy in Morocco between 1969 and 2024. This study was conducted to analyze scientific production and trends in pharmacogenetics and drug-resistant epilepsy in Morocco using the VOSviewer and Scopus databases to build a network of authors, affiliations, and citations. Furthermore, this study analyzed pharmacogenetics in the context of epilepsy and drug-resistant epilepsy research, with the goal of creating new directions and recommendations for future research.
2. Materials and Methods
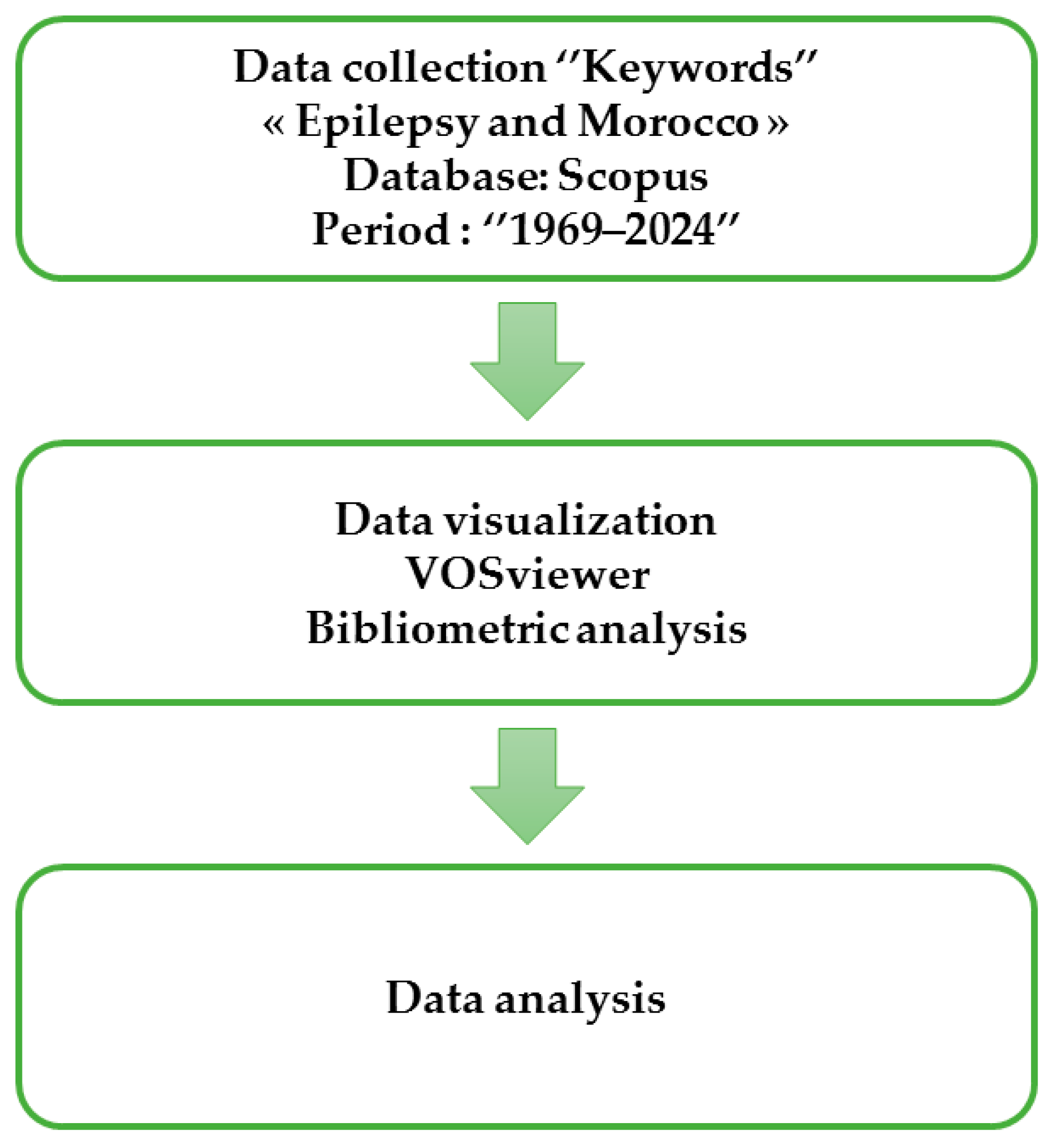
The bibliometric analysis was performed using the available articles in the Scopus database during the period between 1969 and 2024, following four steps as follows: the conceptualization of the study, data collection, data analysis and interpretation. To this end, the keywords “epilepsy” and “Morocco” were used. The Scopus database covers the most comprehensive catalog of publications, including books, conferences, and articles [18]. It also supports various software programs for retrieving bibliometric data, including authors, titles, dates of publications, countries, and institutions [19].
The process of evaluating data extracted from the Scopus database consists of the following steps: the data were collected using search keywords to choose the relevant literature based on the Scopus database criteria, the data were exported to VOSviewer for a bibliometric analysis and presentation of the findings, and outcomes were analyzed to determine the most important themes discussed and studied (Figure 1).
Figure 1.
Methodology procedure adopted to perform bibliometric analysis.
For the bibliometric analysis, we used VOSviewer and Graph Pad Prism 5 software to analyze data extracted from the Scopus database. VOSviewer is a tool widely used to create and present network data, including authorship, co-authorship, countries, citations, co-citations, and bibliographic coupling relationships, that can be used to build an author’s network. Additionally, field trends can be discovered using bibliometric analysis.
3. Results
3.1. Publication Trend and Historical Background
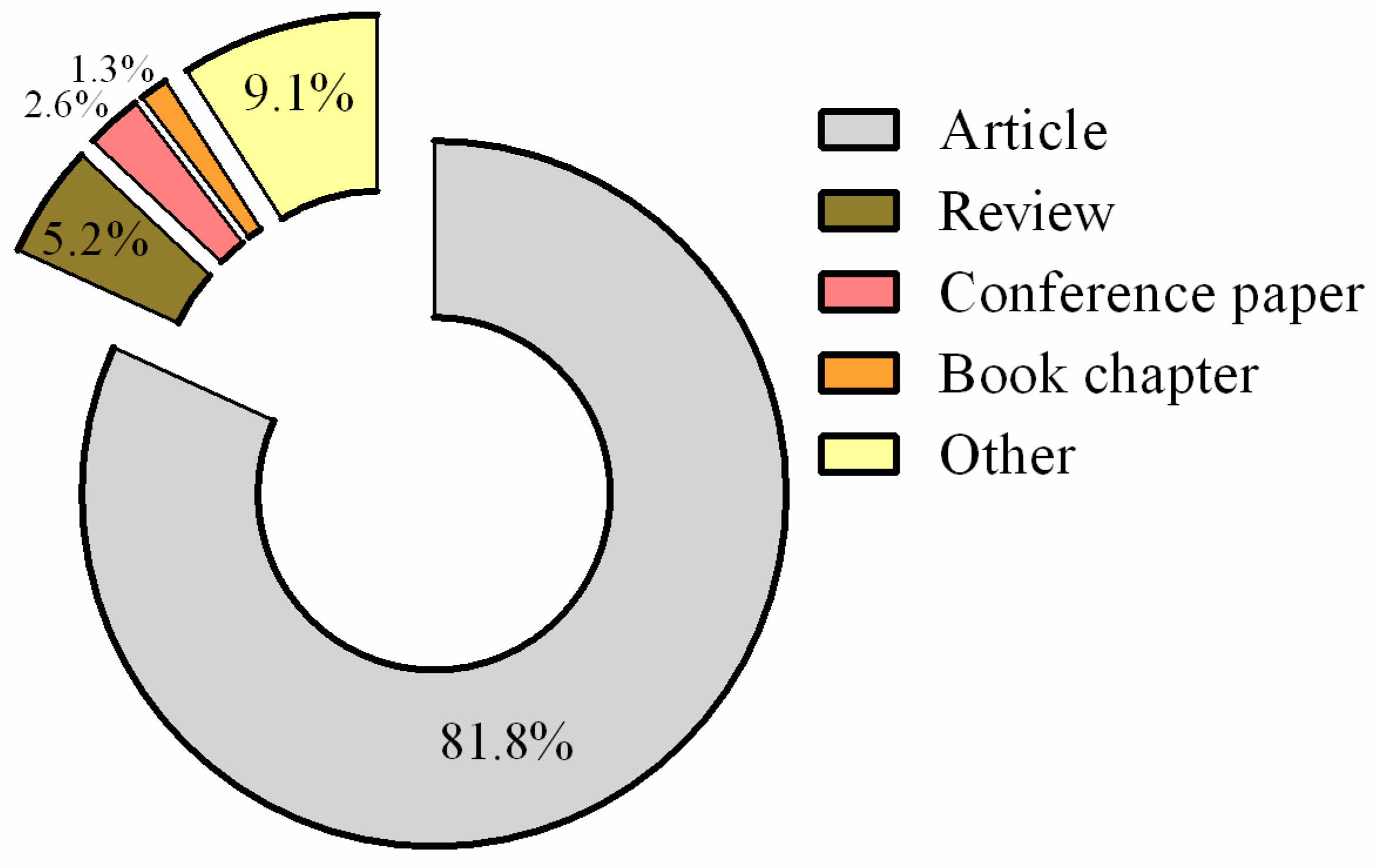
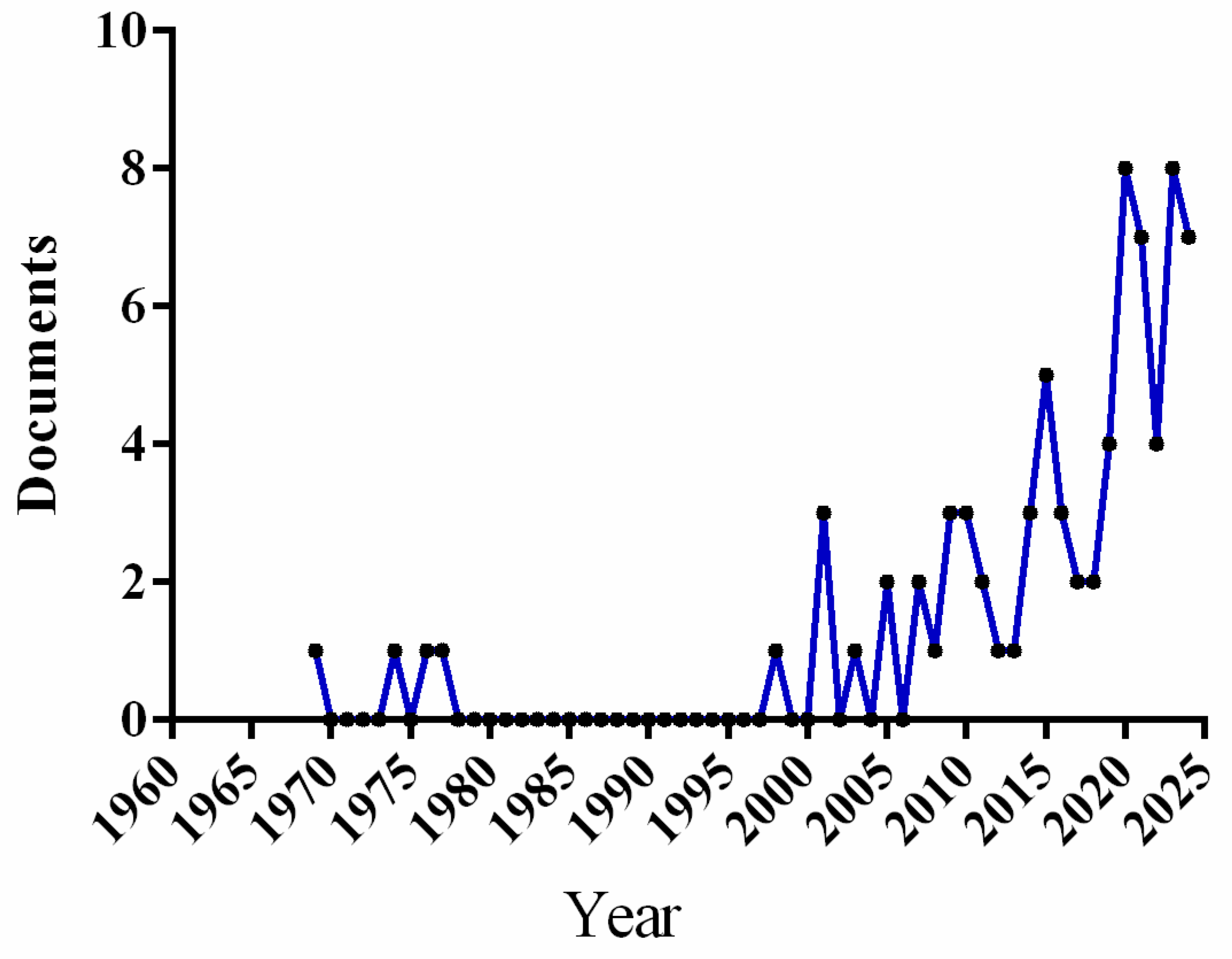
A total of 77 articles were found in the Scopus database and were published during the study period between 1969 and 2024, mostly articles (81.8%), reviews (5.2%), conference papers (3.9%), and book chapters (1.3%) (Figure 2). The findings revealed that the first document was published in 1969. The number of publications recorded in the Scopus database has progressively increased, with the exception of 1977 and 1997, which are characterized by 0 publications. Figure 3 provides robust evidence that the scientific community’s interest in this field of research has increased since 2007. This progression could be explained by the development of technology, a better understanding of the pathology, the development of a search for safer and effective medications, and the appearance of drug-resistant epilepsy.
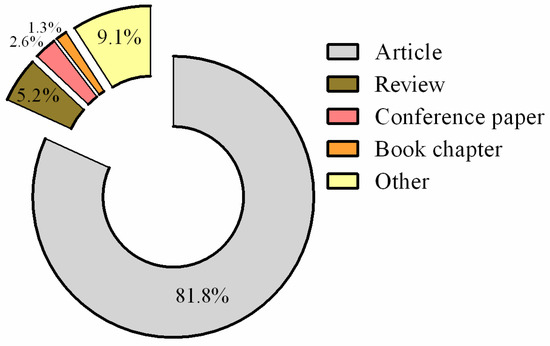
Figure 2.
Distribution of documents published during 1969–2024 according their type.
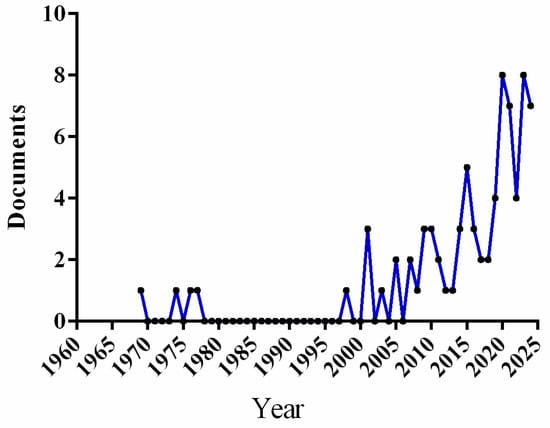
Figure 3.
Articles published on epilepsy in Morocco during 1969–2024.
The first publication on epilepsy in the Scopus database was a 1969 paper entitled “Epilepsy in North Africa” [20]. This paper is the first to report the evolution of epilepsy in North Africa.
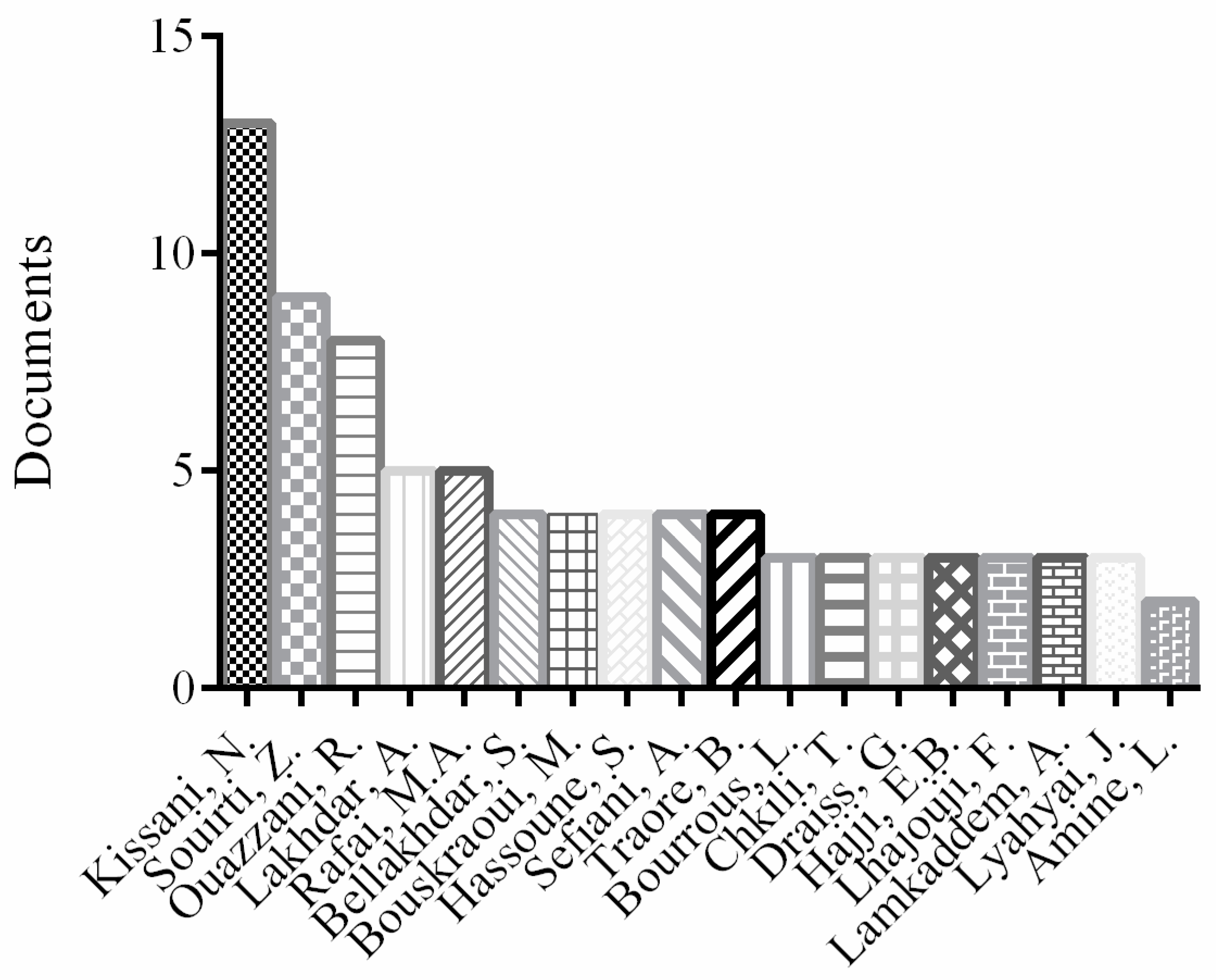
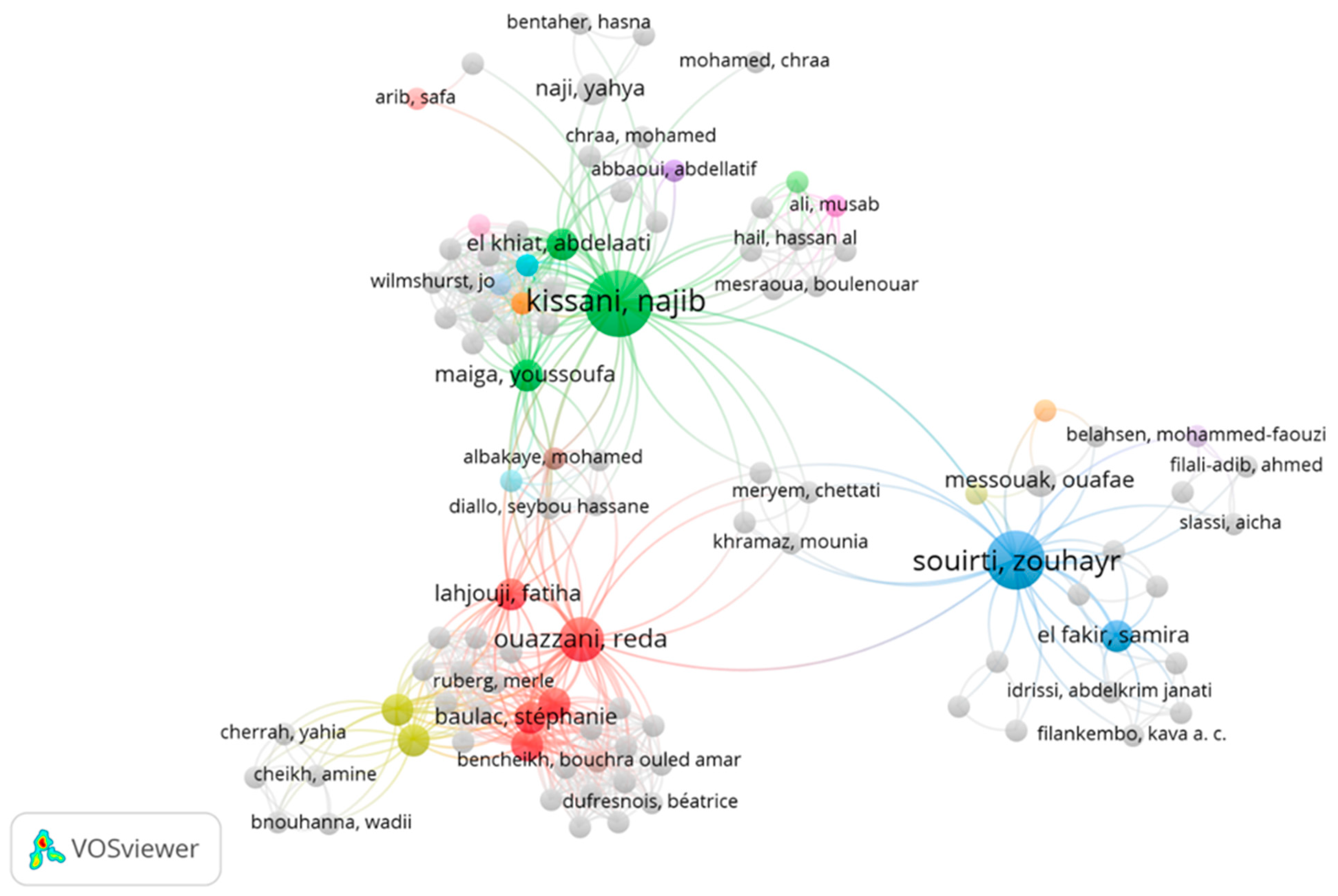
3.2. Contributing Authors
Based on the available data extracted from the Scopus database, the most contributing author was Kissani, N from University Hospital Mohamed VI, Marrakech, Morocco, with the highest article number of 11 articles and a total of 1646 citations. These findings demonstrate the paramount impact of the research conducted by Kissani, N on the scientific community, which marks their position as a leader in the field in Morocco. One of his most highly cited articles was “Telemedicine in epilepsy: How can we improve care, teaching, and awareness?” [21] with 59 citations, whereas his most recent publication was “Prevalence of epilepsy in Morocco: A population-based study” [22]. Souirti, Z and Ouazzani, R also significantly contributed to the enrichment of scientific databases on epilepsy, with eight and seven articles, respectively. Furthermore, other authors have participated deeply in the understanding of its pathology with variable article numbers, such as Lakhdar, A; Rafai, M.A; Bellakhder, S; Bouskraoui, M; and so on (Figure 4). More information about the authors’ publications during the study period is presented in Figure 4.
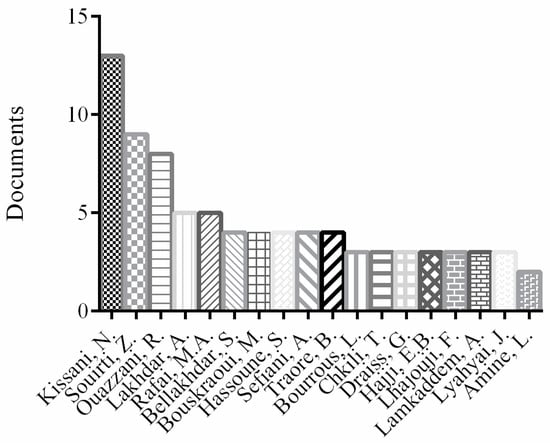
Figure 4.
Author productivity.
Figure 5 displays the bibliometric analysis of the authors’ distribution. It is clearly seen that the top three prolific authors were Kissani, N, Ouazzani, R, and Souirti, Z from University Hospital Mohammed VI, Marrakech, Morocco, Clinical Neurosciences Laboratory, the Faculty of Medicine and Pharmacy, the University of Sidi Mohammed Ben Abdellah, Fez, Morocco, and the Department of Clinical Neurophysiology, the Faculty of Medicine and Pharmacy of Rabat, Avicenne Hospital, the Mohammed V University of Rabat, Rabat, Morocco, respectively. Kissani, N focuses on knowledge on and attitudes and traditional practices toward epilepsy among relatives of PWEs (patients with epilepsy) in Marrakesh, Morocco. Kissani, N was at the top of the list of authors who contributed considerably in the field, with 11 articles cited 68 times. Conversely, Souirti Z has eight publications, which have been cited 44 times. Furthermore, Ouazzani Rida was classified as third with seven publications, which had more citations (122) (Table 1).
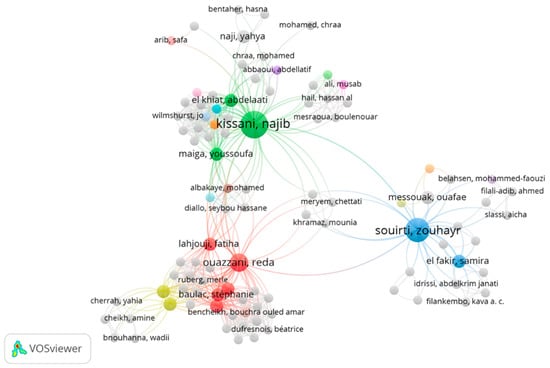
Figure 5.
Bibliometric analysis of the authors of publications on epilepsy in Morocco.

Table 1.
Top three prolific authors contributing towards epilepsy research in Morocco.
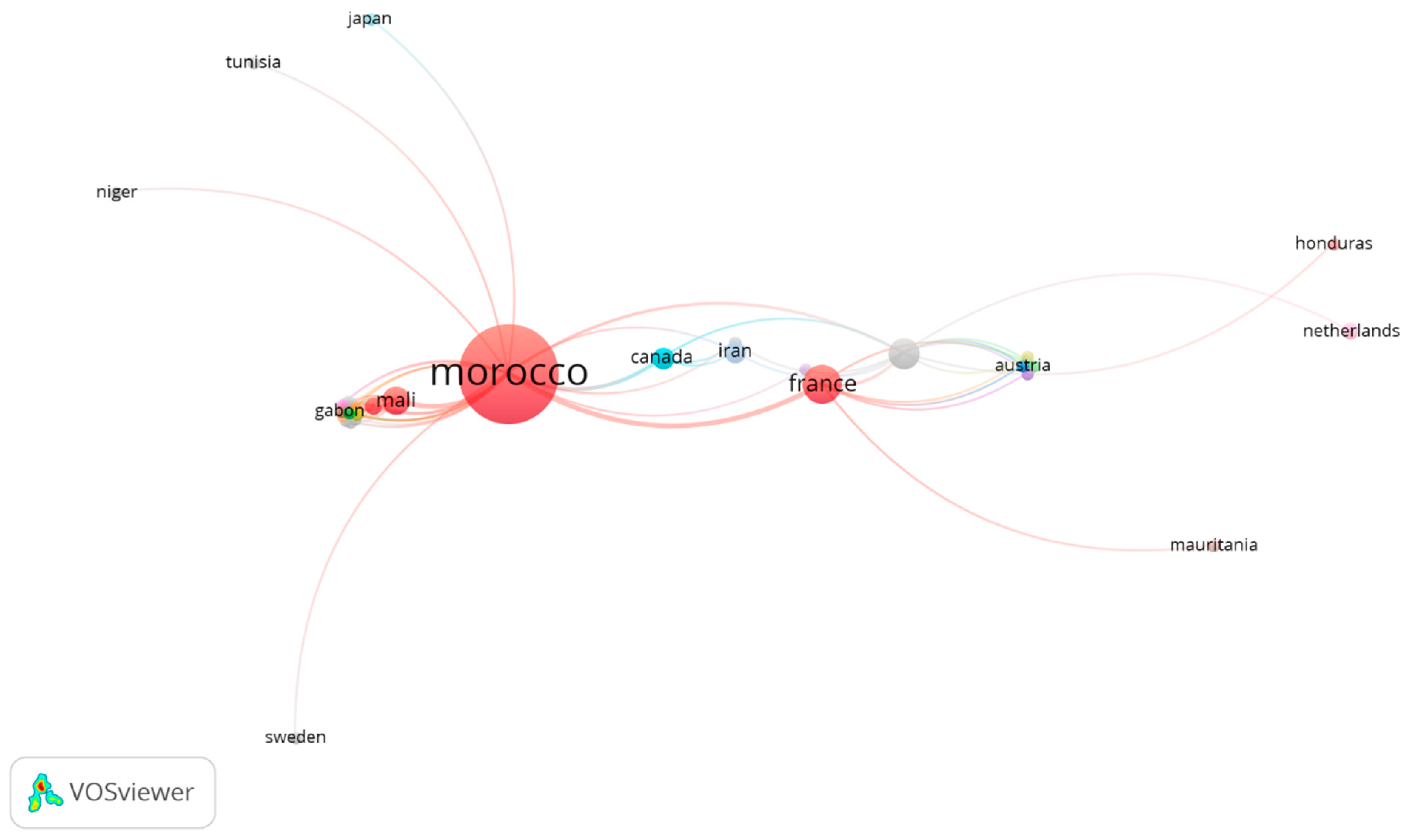
3.3. Country-Wise Mapping
A country-wise analysis revealed that 55 articles were published in Morocco, followed by France with 9 publications, and the United States with 5 publications. In the bibliometric analysis of countries, 13 countries contributed to epilepsy research in collaboration with Morocco (Figure 6). This analysis provided important insights into collaborations between Morocco and other countries. The dispersion of research activities among countries illuminates the global reach and cooperation in this field. France and the United States are significantly involved in pathology research, and they are dedicated to increasing knowledge of epilepsy’s pathology and developing efficient treatment strategies. Furthermore, France is positioned as one of the most prolific countries in terms of research output, with nine documents available in the Scopus database. This suggests a gap in the area’s research output, which offers potential expansion and cooperation in the future, especially regarding pharmacogenetics in epilepsy and drug-resistant epilepsy.
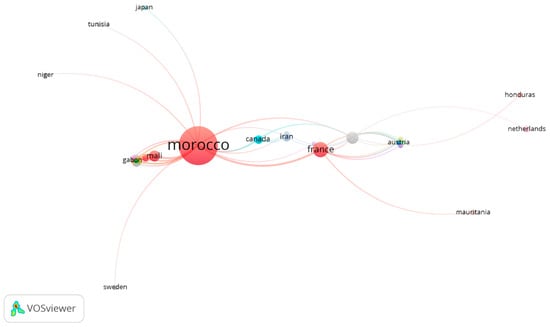
Figure 6.
Bibliometric analysis of countries in collaboration with Morocco.
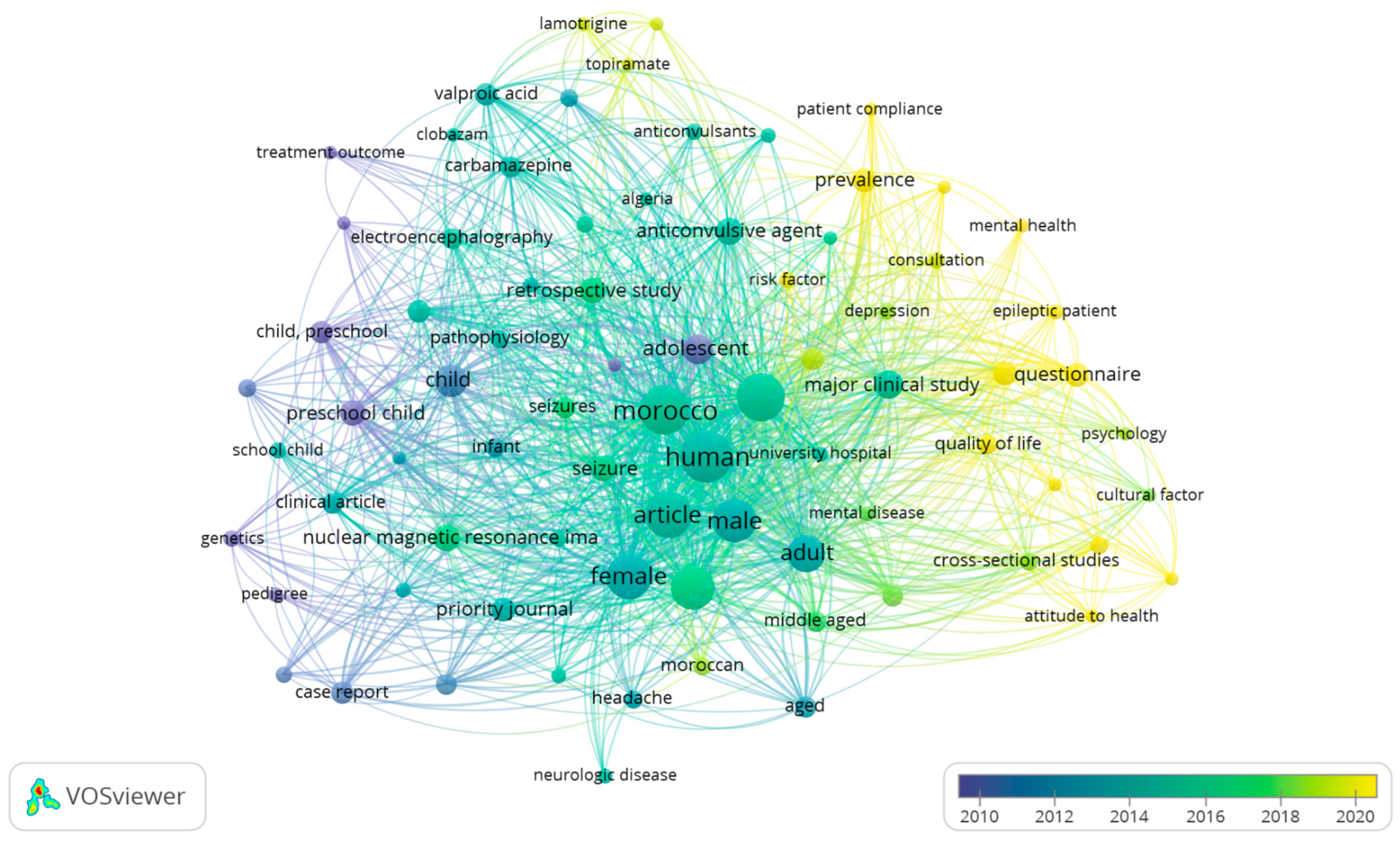
3.4. Bibliometric Analysis of Co-Occurring Keywords
A bibliometric analysis of co-occurring keywords was performed using all keywords. The treatment of data extracted from Scopus revealed that 1306 keywords were identified. For network analysis, the selected keywords that occurred at least 5 times (78 keywords) were used (Figure 7). The keywords “Epilepsy” and “Morocco” were the most frequent keywords in the scheme for obvious reasons, as we limited our search to Morocco. Figure 7 shows different nodes representing an entity. The size of each entity denotes how frequently a keyword appears, and the co-occurrence of a keyword is represented by the association between different generated nodes. Four clusters of keywords with varying colors were produced by the bibliometric study (blue, green, and yellow). The green cluster consists of the main words centered on epilepsy, seizures, mental illness, and anticonvulsant agents. The yellow cluster comprises the most widely used keywords after 2020, including quality of life, epileptic patient, questionnaire, and mental health (Figure 7). Notably, there is a scarcity of keywords related to pharmacogenetics in epilepsy and drug-resistant epilepsy, which presents a potential opportunity for future growth and collaboration with international institutions.
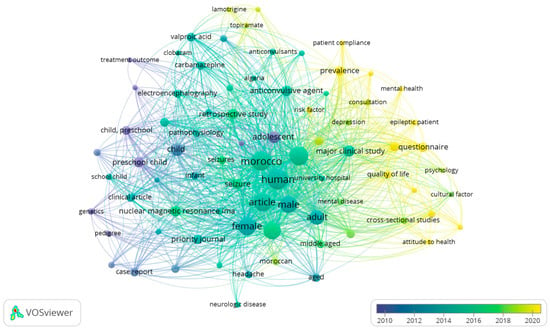
Figure 7.
Co-occurrence of important keywords according to papers on VOSviewer-based major theme visualization.
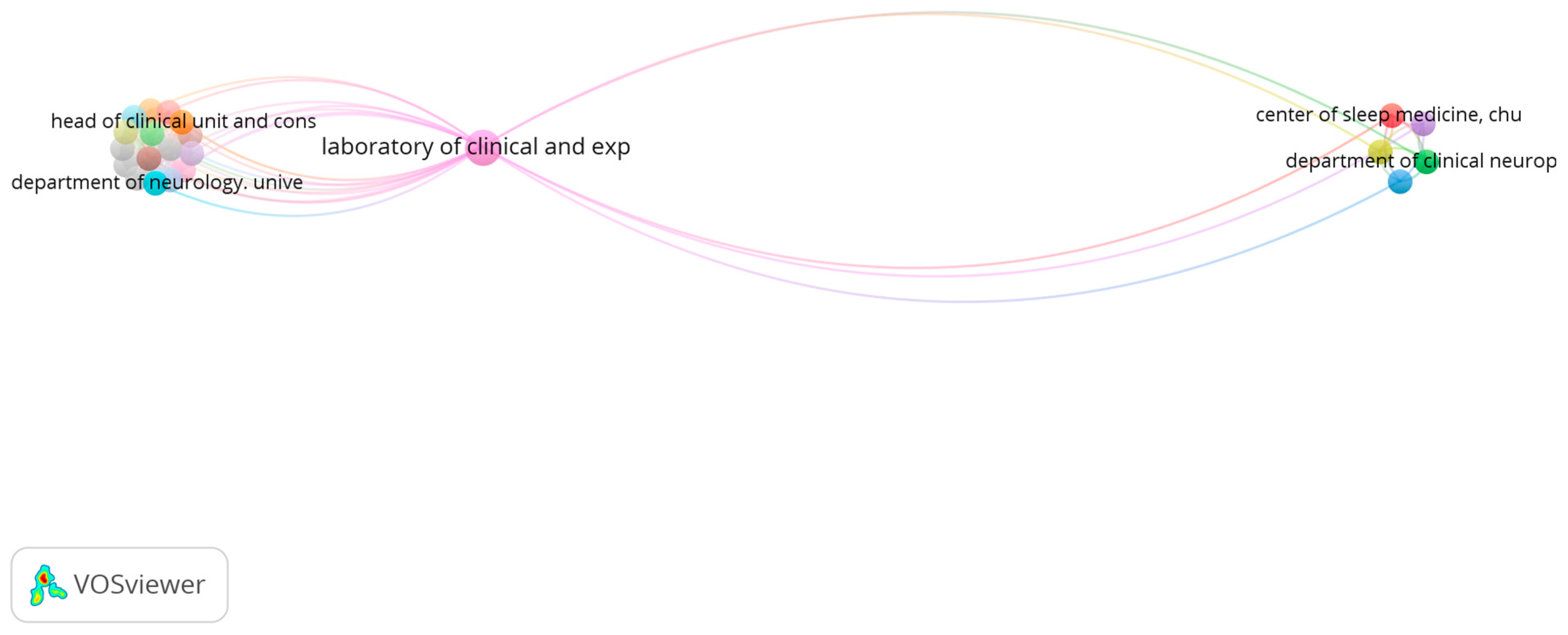
3.5. Institutions Contributing
In Morocco, we found 22 institutions contributing to epilepsy, which were classified into two clusters (Cluster 1 and Cluster 2). The first item comprises 16 items, including the Department of Neurology, University Teaching, Hospital Mohammed VI, Marrakesh, Morocco, and the second cluster includes 6 items, such as the Center of Sleep Medicine, CHU Hassan II, Fez, Morocco; the Department of Clinical Neurophysiology, Specialty Hospital Ono CHU Ibn Sina Rabat, Morocco; the Department of Neurology, CHU Hassan II, Fez, Morocco; the Department of Neurology, Mohammed VI Oujda University Hospital Morocco; the Department of Neurology, Mohammed VI University Hospital, Marrakesh, Morocco; and the Laboratory of Clinical and Experimental Neuroscience, the Faculty of Medicine, Cadi Ayyad University, Marrakesh, Morocco (Figure 8).
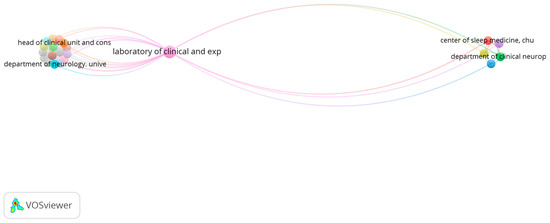
Figure 8.
Leading institutions’ publications on epilepsy.
The Laboratory of Clinical and Experimental Neuroscience, the Faculty of Medicine, Cadi Ayyad University, Marrakesh, Morocco, was on the top of the institution list working on epilepsy in Morocco, with more than seven papers published on epilepsy, which confirmed the interest shown in this subject by epilepsy research structures in Morocco.
Laboratory of clinical and exp: the Laboratory of Clinical and Experimental Neuroscience, the Faculty of Medicine, Cadi Ay-yad University, Marrakesh, Morocco.
Head of clinical unit and cons: The Head of the Clinical Unit and Consultant Neurologist.
Department of neurology unive: the Department of Neurology, Mohammed VI University Hospital, Marrakesh, Morocco.
Department of clinical neurop: the Department of Clinical Neurophysiology, Specialty Hospital Ono CHU Ibn Sina Rabat, Morocco.
Center of sleep medicine, chu: the Center of Sleep Medicine, CHU Hassan II, Fez.
3.6. Influential Articles
Concerning influential articles, Chaachouay et al.’s article entitled “Ethnobotanical Study Aimed at Investigating the Use of Medicinal Plants to Treat Nervous System Diseases in the Rif of Morocco” [23], which has been cited 39 times, plays an important role in experimental studies that document different natural remedies widely used in the Rif region, Morocco. It was also found that Bakhchane et al. published an article under the title “Recessive TBC1D24 mutations are frequent in Moroccan non-syndromic hearing loss pedigrees”, published in 2015 [24]. This article was cited 29 times and constitutes the first report of recessive TBC1D24 mutations in Moroccan non-syndromic hearing loss pedigrees with four neurological presentations (infantile epileptic encephalopathy, infantile myoclonic epilepsy, DOORS, and NSHL [24]. Pharmacogenetics in epilepsy has served as a foundation for researchers and clinicians investigating various therapeutic approaches.
4. Discussion
Several reports have discussed epilepsy in Morocco, although the number of reports is limited. This could be explained by the fact that only 77 studies have been found in the Scopus database since the first publication in 1969 (an average of 1.4 documents per year and only 0.03% (77/250929) of all articles on epilepsy found in the Scopus database). Despite a considerable increase in recent scientific trends, considerable gaps remain. More precisely, there are still many published works in the fields of the pharmacogenetics of epilepsy, drug-resistant epilepsy, and personalized medication.
Epilepsy is a common neurological disorder that affects people of all ages. Numerous etiologies of this disease exist, and its global burden lowers patient quality of life. A cross-sectional and descriptive study on the knowledge, attitudes, and traditional practices of the outpatient neurology clinic at Mohammed 6 University Hospital in the Marrakesh region was conducted. The findings showed that most recruited patients were ignorant of the condition, held false beliefs about it, and thought that witchcraft was the primary cause of their seizures [25]. In other regions, including the United Arab Emirates (UAE) and Jordan, 13% and 16% of patients attributed their ailment to a supernatural cause or demonic possession [26,27]. Moreover, the extremely high incidence of epilepsy in rural areas may be explained by a lack of education, greater dependence on traditional healers, and environmental exposure. Ancient civilizations have developed considerable knowledge of epilepsy management, dating back to at least four millennia [28]. Most previous epilepsy treatments were empirical and based on the clinical observations of traditional physicians or even beliefs. Among other treatments, these therapies include diet, herbal remedies, and sometimes even surgery like skull trephination [28]. In fact, approximately 30 chemical agents have been released to the pharmaceutical market to treat epilepsy, and medication therapy has become the basis of treatment for neurological disorders in recent times [29,30]. Even with adequate therapies, 30% of patients develop resistance despite recent technological advancements [29]. Given the higher risks of morbidity and health issues associated with drug-resistant epileptic convulsions, many individuals with epilepsy frequently search for assistance using unconventional approaches [31]. A retrospective study on focal drug-resistant epilepsy was conducted in the epileptology department of the University Hospital of Fez, Morocco. Primary causes of complication appearance were a known delay between the onset of seizures and epilepsy surgery, a restricted number of epilepsy centers, and a scarcity of invasive testing [32]. Hajji et al. first described the prevalence and predictive factors of drug-resistant epilepsy in the Casablanca-Settat region. The authors found that the prevalence of drug-resistant epilepsy was 29.4%, and for pseudo-resistant epilepsy, it was 18%, and the most predictive factors of drug-resistant epilepsy were allopathic treatment use, interictal EEG abnormalities, preictal auras, comorbidities, and concomitant affections [33]. Recently, drug-resistant epilepsy has been revealed to involve genetic factors implicated in the process. The same treatment administered to two patients with the same kind of disease showed different degrees of effectiveness [10]. These factors include the polymorphism of microsomal enzymes (CYP2C19 and CYP1C9), multidrug resistance-associated proteins, P glycoproteins, ion channels, and the perturbation of the pharmacodynamic activity of neurotransmitter GABA receptors [9]. The genetic polymorphism of enzymes that metabolize antiseizure drugs influences how quickly drugs are metabolized, which can result in varying degrees of sensitivity to their concentrations and even toxic side effects [9]. It has been found that antiseizure drugs that enhance GABAergic transmission decrease neuronal oxidative stress in a dose-dependent manner [34]. A previous study investigated the effect of vigabatrin (VGB) on the oxidation of proteins and lipids in rats during various stages of pregnancy [35]. The authors found that VGB passes through the placenta and induces oxidative stress by reducing glutathione peroxidase, glutathione reductase, and glutathione-transferase levels in rats’ fetal liver [35].
Precision medicine has become a viable therapeutic option for epilepsy treatment recently. The most researched treatment modalities are gene therapy, deep brain stimulation, blood–brain targeting, and anti-inflammatory strategies [36]. Furthermore, multiple investigations into genetics are required to analyze other biomarkers for the implementation of predictive and preventive measures. Successful therapy for such diseases is highly impacted by individual characteristics, such as sex, age, health status, socioeconomic status, and diagnosis [37]. One of the most important aspects of personalized medicine is genomic medicine, which involves various omics approaches, including proteomics and metabolomics [37]. The use of pharmacogenomics biomarkers is of paramount importance to enhance treatment efficacy and prevent unfavorable drug responses. Medication efficacy is often polygenic; however, significant adverse effects are less common and more likely to be inherited [37]. These negative effects are considered by the WHO as the main causes of hospitalization and mortality [37]. Since the appearance of pharmacogenetics in 1959, which was coined by Friedrich Vogel, it has gained considerable attention from the scientific community [37]. Several studies have been conducted to identify the genetic factors implicated in ASD responses. It has been found that the expression of glycoprotein-P encoded by the multidrug resistance gene (MDR1) considerably affects the biological activities of several drugs, affecting their bioavailability, passage across tissues, and elimination from tissues. Previous studies have demonstrated that the overexpression of glycoprotein-P enhances the resistance of ASDs due to their ability to expulse drugs throughout the blood–brain barrier into the blood [38]. A study conducted on dogs revealed that prolonged seizures significantly enhanced glycoprotein-P overexpression. This could perhaps explain the decrease in anticonvulsant efficacy and the appearance of resistance [39]. Furthermore, MDR1 was expressed tenfold more in patients with drug-resistant epilepsy than in the control group [40]. Despite technological advancements, complementary and alternative medicine occupies an important position in the medical habits of several civilizations worldwide. An increasing number of scientific communities are becoming aware of the possible benefits of natural remedies that have fewer toxicity and adverse effects.
Mesraoua et al. found that complementary and alternative medicine for epilepsy, including religious and spiritual beliefs, has evolved to minimize treatment costs compared with conventional medication used to manage the illness [30]. Furthermore, due to the low availability of various antiseizure drugs, the prescription pattern of antiseizure drugs as monotherapy offers restricted solutions to the use of the oldest medications, with considerable side effects. In fact, the search for effective epilepsy medication approaches has focused on natural remedies because of their wide-spectrum neurobiological properties. This could explain the vast utility of complementary and alternative medicine for epilepsy treatment in North Africa. However, in some countries like Iran, complementary alternative medicine occupies an important position for some neurologists and is of paramount importance for treating epilepsy [41]. Various studies have been conducted to examine the antiseizure activity of different components extracted from natural resources, such as coumarin derivatives [42,43,44]. Furthermore, natural products contain a wide range of biologically active compounds, including alkaloids, phenolic acids, flavonoids, organic acids, vitamins, and minerals [41]. The pleiotropic effects of bioactive compounds found in several natural products make them potential candidates for treating various neurological disorders [45]. Li and colleagues summarized the different mechanisms of action of different alkaloids, including indole, quinolones, terpenoid, and pyridine. The authors mentioned that natural alkaloids enhance GABAergic neurotransmission, decrease excitatory glutamatergic activities, and downregulate pro-inflammatory pathways [45]. Phytoactive compounds exert synergistic effects by controlling synaptic interactions in neurons, mitigating neuro-inflammation, and restoring neuronal homeostasis [46]. Given its multiple etiologies, pathobiology and pharmacotherapy-resistant variants, epilepsy necessitates a specific therapeutic strategy. The combination of natural products and their phytoactive compounds with antiseizure drugs constitutes a promising approach via distinct mechanisms, such as a decrease in membrane excitability via the downregulation of cation channels, the amelioration of mitochondrial functions by controlling antioxidant status, an improvement in GABAa receptor functions, the control of immune reactions and inflammatory processes, and arrest protein synthesis and metabolism [47]. Robust experimental evidence demonstrated that the administration of classical Baijin Pills (BJPs) to mice with lithium–pilocarpine-induced epilepsy extended the latency of seizures and decreased the duration of epilepsy [48]. Additionally, BJP protects the hippocampus, downregulates pro-inflammatory marker expression, and improves the antioxidant status of animals [48]. Further experimental studies on plant-based extracts and natural remedies are required to develop safer and more effective antiepileptic therapies.
5. Conclusions
This study used quantitative and qualitative data extracted from the Scopus database to support and shift scientific attention towards epilepsy in Morocco. A bibliometric analysis was performed to review articles published on epilepsy in Morocco and analyze the current state of research in this field. The outcomes revealed scientific trends, authors, countries, institution contributions, research gaps, and leading research. This study showed that the number of articles published on epilepsy in Morocco is limited, particularly on pharmacogenetics and drug-resistant epilepsy. Most studies highlighted their interest in pathogenesis and conventional and traditional treatment strategies. Further analyses are required to enlarge the databases used to collect data, including the Web of Sciences, Springer, PubMed, and MDPI databases, to acquire more high-quality scientific contributions.
Author Contributions
Conceptualization, A.Z. and Y.K.; methodology, A.Z. and D.O.; writing—original draft preparation, A.Z.; writing—review and editing, D.O.; supervision, Y.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The dataset is available on request from the authors.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Thijs, R.D.; Surges, R.; O’Brien, T.J.; Sander, J.W. Epilepsy in Adults. Lancet 2019, 393, 689–701. [Google Scholar] [CrossRef] [PubMed]
- Beghi, E. The Epidemiology of Epilepsy. Neuroepidemiology 2020, 54, 185–191. [Google Scholar] [CrossRef] [PubMed]
- Farrelly, A.M.; Vlachou, S.; Grintzalis, K. Efficacy of Phytocannabinoids in Epilepsy Treatment: Novel Approaches and Recent Advances. Int. J. Environ. Res. Public Health 2021, 18, 3993. [Google Scholar] [CrossRef] [PubMed]
- Fisher, R.S. The New Classification of Seizures by the International League Against Epilepsy 2017. Curr. Neurol. Neurosci. Rep. 2017, 17, 48. [Google Scholar] [CrossRef] [PubMed]
- Fisher, R.S.; Acevedo, C.; Arzimanoglou, A.; Bogacz, A.; Cross, J.H.; Elger, C.E.; Engel, J.; Forsgren, L.; French, J.A.; Glynn, M.; et al. ILAE Official Report: A Practical Clinical Definition of Epilepsy. Epilepsia 2014, 55, 475–482. [Google Scholar] [CrossRef]
- Fisher, R.S.; Boas, W.V.E.; Blume, W.; Elger, C.; Genton, P.; Lee, P.; Engel, J. Epileptic Seizures and Epilepsy: Definitions Proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE). Epilepsia 2005, 46, 470–472. [Google Scholar] [CrossRef]
- Cho, S.-J.; Park, E.; Baker, A.; Reid, A.Y. Age Bias in Zebrafish Models of Epilepsy: What Can We Learn from Old Fish? Front. Cell Dev. Biol. 2020, 8, 573303. [Google Scholar] [CrossRef]
- Cano-López, I.; Hampel, K.G.; Garcés, M.; Villanueva, V.; González-Bono, E. Quality of Life in Drug-Resistant Epilepsy: Relationships with Negative Affectivity, Memory, Somatic Symptoms and Social Support. J. Psychosom. Res. 2018, 114, 31–37. [Google Scholar] [CrossRef]
- Smolarz, B.; Makowska, M.; Romanowicz, H. Pharmacogenetics of Drug-Resistant Epilepsy (Review of Literature). Int. J. Mol. Sci. 2021, 22, 11696. [Google Scholar] [CrossRef]
- Spear, B.B. Pharmacogenetics and Antiepileptic Drugs. Epilepsia 2001, 42, 31–34. [Google Scholar] [CrossRef]
- Hakami, T. Neuropharmacology of Antiseizure Drugs. Neuropsychopharm. Rep. 2021, 41, 336–351. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, K.H.; Roslan, M.F.; Ishak, N.S.; Ilias, M.; Dani, R. Unearthing Hidden Research Opportunities through Bibliometric Analysis: A Review. Asian J. Res. Educ. Soc. Sci. 2023, 5, 251–262. [Google Scholar]
- Rodrigues, M.; Daniel, A.D.; Franco, M. What Is Important to Know about Mumpreneurship? A Bibliometric Analysis. Int. J. Organ. Anal. 2023, 31, 3413–3435. [Google Scholar] [CrossRef]
- Lim, W.M.; Kumar, S. Guidelines for Interpreting the Results of Bibliometric Analysis: A Sensemaking Approach. Glob. Bus. Org. Excell. 2024, 43, 17–26. [Google Scholar] [CrossRef]
- Topal, Z.; Bahsi, I.; Tufan, A.E. Evaluation of the Psychiatric Research Output from Turkey via Web of Science Database: A Bibliometric Analysis. Psychiatry Clin. Psychopharmacol. 2020, 30, 1–33. [Google Scholar] [CrossRef]
- Morán-Mariños, C.; Pacheco-Mendoza, J.; Metcalf, T.; De la Cruz Ramirez, W.; Alva-Diaz, C. Collaborative Scientific Production of Epilepsy in Latin America from 1989 to 2018: A Bibliometric Analysis. Heliyon 2020, 6, e05493. [Google Scholar] [CrossRef]
- Baig, D.N.; Siddique, R.; Zafar, A.; Al Firdausi, M.; Shafiq, M.; Arain, O.Z.; Uzair, M.; Bashir, S.; Jannat, S.; Kaleem, I. Bibliometric Analysis of Epilepsy Research in Pakistan. J. Pharma Biomed. 2023, 1, 17–26. [Google Scholar]
- Zhao, X.; Wang, S.; Wang, X. Characteristics and Trends of Research on New Energy Vehicle Reliability Based on the Web of Science. Sustainability 2018, 10, 3560. [Google Scholar] [CrossRef]
- Baas, J.; Schotten, M.; Plume, A.; Côté, G.; Karimi, R. Scopus as a Curated, High-Quality Bibliometric Data Source for Academic Research in Quantitative Science Studies. Quant. Sci. Stud. 2020, 1, 377–386. [Google Scholar] [CrossRef]
- Christozov, C. Epilepsy in North Africa. Tunis. Medicale 1969, 47, 327–336. [Google Scholar]
- Kissani, N.; Lengané, Y.T.M.; Patterson, V.; Mesraoua, B.; Dawn, E.; Ozkara, C.; Shears, G.; Riphagen, H.; Asadi-Pooya, A.A.; Bogacz, A. Telemedicine in Epilepsy: How Can We Improve Care, Teaching, and Awareness? Epilepsy Behav. 2020, 103, 106854. [Google Scholar] [CrossRef] [PubMed]
- Souirti, Z.; Hmidani, M.; Lamkadddem, A.; Khabbach, K.; Belakhdar, S.; Charkani, D.; Mhandez Tlemcani, D.; Lahmadi, N.; El Akramine, M.; Erriouiche, S.; et al. Prevalence of Epilepsy in Morocco: A Population-based Study. Epilepsia Open 2023, 8, 1340–1349. [Google Scholar] [CrossRef] [PubMed]
- Chaachouay, N.; Benkhnigue, O.; Zidane, L. Ethnobotanical Study Aimed at Investigating the Use of Medicinal Plants to Treat Nervous System Diseases in the Rif of Morocco. J. Chiropr. Med. 2020, 19, 70–81. [Google Scholar] [CrossRef]
- Bakhchane, A.; Charif, M.; Salime, S.; Boulouiz, R.; Nahili, H.; Roky, R.; Lenaers, G.; Barakat, A. Recessive TBC1D24 Mutations Are Frequent in Moroccan Non-Syndromic Hearing Loss Pedigrees. PLoS ONE 2015, 10, e0138072. [Google Scholar] [CrossRef]
- Kissani, N.; Moro, M.; Arib, S. Knowledge, Attitude and Traditional Practices towards Epilepsy among Relatives of PWE (Patients with Epilepsy) in Marrakesh, Morocco. Epilepsy Behav. 2020, 111, 107257. [Google Scholar] [CrossRef]
- Bener, A.; Al-Marzooqi, F.H.; Sztriha, L. Public Awareness and Attitudes towards Epilepsy in the United Arab Emirates. Seizure 1998, 7, 219–222. [Google Scholar] [CrossRef]
- Daoud, A.; Al-Safi, S.; Otoom, S.; Wahba, L.; Alkofahi, A. Public Knowledge and Attitudes towards Epilepsy in Jordan. Seizure 2007, 16, 521–526. [Google Scholar] [CrossRef] [PubMed]
- Asadi-Pooya, A.A.; Nikseresht, A.R.; Yaghoubi, E. Old Remedies for Epilepsy: Avicenna’s Medicine. Iran. Red Crescent Med. J. 2012, 14, 174. [Google Scholar]
- Kwan, P.; Brodie, M.J. Early Identification of Refractory Epilepsy. N. Engl. J. Med. 2000, 342, 314–319. [Google Scholar] [CrossRef]
- Mesraoua, B.; Kissani, N.; Deleu, D.; Elsheikh, L.; Ali, M.; Melikyan, G.; Al Hail, H.; Wiebe, S.; Asadi-Pooya, A.A. Complementary and Alternative Medicine (CAM) for Epilepsy Treatment in the Middle East and North Africa (MENA) Region. Epilepsy Res. 2021, 170, 106538. [Google Scholar] [CrossRef]
- Sperling, M.R.; Barshow, S.; Nei, M.; Asadi-Pooya, A.A. A Reappraisal of Mortality after Epilepsy Surgery. Neurology 2016, 86, 1938–1944. [Google Scholar] [CrossRef]
- Souirti, Z.; Sghir, A.; Belfkih, R.; Messouak, O. Focal Drug-Resistant Epilepsy: Progress in Care and Barriers, a Morroccan Perspective. J. Clin. Neurosci. 2016, 34, 276–280. [Google Scholar] [CrossRef]
- Hajji, E.B.; Traore, B.; Hassoune, S.; Alahiane, Z.; Chahid, I.; Bellakhdar, S.; Rafai, M.A.; Lakhdar, A. Drug-Resistant Epilepsy in Morocco: Description, Prevalence and Predictive Factors in Casablanca-Settat Region. J. Clin. Neurosci. 2024, 126, 28–37. [Google Scholar] [CrossRef]
- Kośmider, K.; Kamieniak, M.; Czuczwar, S.J.; Miziak, B. Second Generation of Antiepileptic Drugs and Oxidative Stress. Int. J. Mol. Sci. 2023, 24, 3873. [Google Scholar] [CrossRef] [PubMed]
- Cengiz, M.; Yüksel, A.; Özaydın, A.; Özkılıç, A.; Çetinel, Ü.; Seven, M. The Effects of Vigabatrin on Rat Liver Antioxidant Status. Drug Metab. Drug Interact. 2005, 21, 109–116. [Google Scholar] [CrossRef]
- Riva, A.; Golda, A.; Balagura, G.; Amadori, E.; Vari, M.S.; Piccolo, G.; Iacomino, M.; Lattanzi, S.; Salpietro, V.; Minetti, C. New Trends and Most Promising Therapeutic Strategies for Epilepsy Treatment. Front. Neurol. 2021, 12, 753753. [Google Scholar] [CrossRef]
- Sadee, W.; Wang, D.; Hartmann, K.; Toland, A.E. Pharmacogenomics: Driving Personalized Medicine. Pharmacol. Rev. 2023, 75, 789–814. [Google Scholar] [CrossRef]
- Miller, D.S.; Bauer, B.; Hartz, A.M. Modulation of P-Glycoprotein at the Blood-Brain Barrier: Opportunities to Improve Central Nervous System Pharmacotherapy. Pharmacol. Rev. 2008, 60, 196–209. [Google Scholar] [CrossRef]
- Pekcec, A.; Unkrüer, B.; Stein, V.; Bankstahl, J.P.; Soerensen, J.; Tipold, A.; Baumgärtner, W.; Potschka, H. Over-Expression of P-Glycoprotein in the Canine Brain Following Spontaneous Status Epilepticus. Epilepsy Res. 2009, 83, 144–151. [Google Scholar] [CrossRef] [PubMed]
- Tishler, D.M.; Weinberg, K.I.; Hinton, D.R.; Barbaro, N.; Annett, G.M.; Raffel, C. MDR1 Gene Expression in Brain of Patients with Medically Intractable Epilepsy. Epilepsia 1995, 36, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Asadi-Pooya, A.A.; Emami, M. Perception and Use of Complementary and Alternative Medicine among Children and Adults with Epilepsy: The Importance of the Decision Makers. Acta Medica Iran. 2014, 52, 153–157. [Google Scholar]
- Kozioł, E.; Jóźwiak, K.; Budzyńska, B.; de Witte, P.A.; Copmans, D.; Skalicka-Woźniak, K. Comparative Antiseizure Analysis of Diverse Natural Coumarin Derivatives in Zebrafish. Int. J. Mol. Sci. 2021, 22, 11420. [Google Scholar] [CrossRef] [PubMed]
- Chipiti, T.; Viljoen, A.M.; Cordero-Maldonado, M.L.; Veale, C.G.; Van Heerden, F.R.; Sandasi, M.; Chen, W.; Crawford, A.D.; Enslin, G.M. Anti-Seizure Activity of African Medicinal Plants: The Identification of Bioactive Alkaloids from the Stem Bark of Rauvolfia Caffra Using an in Vivo Zebrafish Model. J. Ethnopharmacol. 2021, 279, 114282. [Google Scholar] [CrossRef]
- Zhu, H.; Wan, J.; Wang, Y.; Li, B.; Xiang, C.; He, J.; Li, P. Medicinal Compounds with Antiepileptic/Anticonvulsant Activities. Epilepsia 2014, 55, 3–16. [Google Scholar] [CrossRef]
- Li, S.; Lin, X.; Duan, L. Harnessing the Power of Natural Alkaloids: The Emergent Role in Epilepsy Therapy. Front. Pharmacol. 2024, 15, 1418555. [Google Scholar] [CrossRef]
- Ohanme, E.O.; Iganga, O.N.; Ofor, C.C.; Ofonakara, U.; Nwafor, A.V.; Eze, C.; Etu, K.E.; Nwakelu, B.N.; Unekwe, C.P. Pharmacological Review of Plants and Natural Products with Antiepileptic Effects. J. Complement. Altern. Med. Res. 2024, 25, 13–24. [Google Scholar] [CrossRef]
- Tabassum, S.; Shorter, S.; Ovsepian, S.V. Analysis of the Action Mechanisms and Targets of Herbal Anticonvulsants Highlights Opportunities for Therapeutic Engagement with Refractory Epilepsy. J. Mol. Med. 2024, 102, 761–771. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Cheng, X.; Xue, L.; Liu, H. Ameliorative Influence of Baijin Pills on Lithium-Pilocarpine-Induced Epilepsy in Mice: Role of Oxidative Stress, Neurotransmitters and Multidrug Resistant Transporters. Phytomed. Plus 2024, 4, 100555. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).