Class-Switching of B Lymphocytes by DNA and Cell Immunization for Stereospecific Monoclonal Antibodies against Native GPCR
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Mice
2.3. Cell Culture
2.4. Recombinant Plasmid Vectors
2.5. Recombinant Cells
2.6. Immunization
2.7. Optimized Stereospecific Targeting (SST) Technique
2.8. Cell-Based Enzyme-Linked Immunosorbent Assay (Cell-ELISA)
2.9. Isotype of Antibodies
3. Results and Discussion
3.1. DNA and Cell Immunization for Optimized Stereospecific Targeting (SST)
3.2. Effect of the Number of DNA Immunizations and the Sensitization Period on Class-Switching
3.3. IgG and IgM Production of Stereospecific Monoclonal Antibodies by DNA Immunization and Cell Immunization
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Liu, M.A. A comparison of plasmid DNA and mRNA as vaccine technologies. Vaccines 2019, 7, 37. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Petrovsky, N. Molecular mechanisms for enhanced DNA vaccine immunogenicity. Expert Rev. Vaccines 2016, 15, 313–329. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.A. DNA vaccines: An historical perspective and view to the future. Immunol. Rev. 2011, 239, 62–84. [Google Scholar] [CrossRef] [PubMed]
- Pardi, N.; Hogan, M.J.; Porter, F.W.; Weissman, D. mRNA vaccines—A new era in vaccinology. Nat. Rev. Drug Discov. 2018, 17, 261–279. [Google Scholar] [CrossRef] [PubMed]
- Kaplon, H.; Reichert, J.M. Antibodies to watch in 2019. MAbs 2019, 11, 219–238. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Song, Y.; Tian, W. How to select IgG subclasses in developing anti-tumor therapeutic antibodies. J. Hematol. Oncol. 2020, 13, 45. [Google Scholar] [CrossRef]
- Thomas, A.; Teicher, B.A.; Hassan, R. Antibody-drug conjugates for cancer therapy. Lancet Oncol. 2016, 17, e254–e262. [Google Scholar] [CrossRef]
- Tsumoto, K.; Isozaki, Y.; Tomita, M. Production of monoclonal antibodies. In Culture of Animal Cells: A Manual of Basic Technique and Specialized Applications, 7th ed.; Freshney, R.I., Ed.; Wiley-Blackwell: Hoboken, NJ, USA, 2016; pp. 544–545. [Google Scholar]
- Yamasaki, Y.; Miyamae, C.; Isozaki, Y.; Ichikawa, K.; Kaneko, Y.; Oda, Y.; Murayama, T.; Sakurai, T.; Tamai, K.; Tsumoto, K.; et al. Optimization of stereospecific targeting technique for selective production of monoclonal antibodies against native ephrin type-A receptor 2. J. Immunol. Methods 2020, 484–485, 112813. [Google Scholar] [CrossRef]
- Isozaki, Y.; Tsumoto, K.; Tomita, M. Conformation-specific monoclonal antibodies recognizing the native structure of G protein-coupled receptor (GPCR). Int. Immunopharmacol. 2021, 98, 107872. [Google Scholar] [CrossRef]
- Stavnezer, J.; Schrader, C.E. IgH chain class switch recombination: Mechanism and regulation. J. Immunol. 2014, 193, 5370–5378. [Google Scholar] [CrossRef]
- Yewdell, W.T.; Chaudhuri, J. A transcriptional serenAID: The role of noncoding RNAs in class switch recombination. Int. Immunol. 2017, 29, 183–196. [Google Scholar] [CrossRef]
- Muramatsu, M.; Kinoshita, K.; Fagarasan, S.; Yamada, S.; Shinkai, Y.; Honjo, T. Class switch recombination and hypermutation require activation-induced cytidine deaminase (AID), a potential RNA editing enzyme. Cell 2000, 102, 553–563. [Google Scholar] [CrossRef]
- Stavnezer, J.; Guikema, J.E.; Schrader, C.E. Mechanism and regulation of class switch recombination. Annu. Rev. Immunol. 2008, 26, 261–292. [Google Scholar] [CrossRef] [PubMed]
- Pioszak, A.A.; Parker, N.R.; Suino-Powell, K.; Xu, H.E. Molecular recognition of corticotropin-releasing factor by its G-protein-coupled receptor CRFR1. J. Biol. Chem. 2008, 283, 32900–32912. [Google Scholar] [CrossRef] [PubMed]
- Stocker, J.W.; Forster, H.K.; Miggiano, V.; Stahli, C.; Staehelin, T. Generation of two new myeloma cell lines ‘PAI’ and ‘PAI-O’ for hybridoma production. Res. Discolsure 1982, 21, 7155–7157. [Google Scholar]
- Lo, M.M.S.; Tsong, T.Y.; Conrad, M.K.; Strittmatter, S.M.; Hester, L.D.; Snyder, S.H. Monoclonal antibody production by receptor-mediated electrically induced cell fusion. Nature 1984, 310, 792–794. [Google Scholar] [CrossRef]
- Costagliola, S.; Rodien, P.; Many, M.C.; Ludgate, M.; Vassart, G. Genetic immunization against the human thyrotropin receptor causes thyroiditis and allows production of monoclonal antibodies recognizing the native receptor. J. Immunol. 1998, 160, 1458–1465. [Google Scholar]
- Costagliola, S.; Franssen, J.D.; Bonomi, M.; Urizar, E.; Willnich, M.; Bergmann, A.; Vassart, G. Generation of a mouse monoclonal TSH receptor antibody with stimulating activity. Biochem. Biophys. Res. Commun. 2002, 299, 891–896. [Google Scholar] [CrossRef]
- Takatsuka, S.; Sekiguchi, A.; Tokunaga, M.; Fujimoto, A.; Chiba, J. Generation of a panel of monoclonal antibodies against atypical chemokine receptor CCX-CKR by DNA immunization. J. Pharmacol. Toxicol. Methods 2011, 63, 250–257. [Google Scholar] [CrossRef]
- Koch-Nolte, F.; Glowacki, G.; Bannas, P.; Braasch, F.; Dubberke, G.; Ortolan, E.; Funaro, A.; Malavasi, F.; Haag, F. Use of genetic immunization to raise antibodies recognizing toxin-related cell surface ADP-ribosyltransferases in native conformation. Cell Immunol. 2005, 236, 66–71. [Google Scholar] [CrossRef]
- Øynebråten, I.; Løvås, T.O.; Thompson, K.; Bogen, B. Generation of antibody-producing hybridomas following one single immunization with a targeted DNA vaccine. Scand. J. Immunol. 2012, 75, 379–388. [Google Scholar] [CrossRef] [PubMed]
- Tan, G.S.; Krammer, F.; Eggink, D.; Kongchanagul, A.; Moran, T.M.; Palese, P. A pan-H1 anti-hemagglutinin monoclonal antibody with potent broad-spectrum efficacy in vivo. J. Virol. 2012, 86, 6179–6188. [Google Scholar] [CrossRef]
- Nagata, S.; Salvatore, G.; Pastan, I. DNA immunization followed by a single boost with cells: A protein-free immunization protocol for production of monoclonal antibodies against the native form of membrane proteins. J. Immunol. Methods 2003, 280, 59–72. [Google Scholar] [CrossRef]
- Schmidlin, H.; Diehl, S.A.; Blom, B. New insights into the regulation of human B-cell differentiation. Trends Immunol. 2009, 30, 277–285. [Google Scholar] [CrossRef] [PubMed]
- Tangye, S.G.; Tarlinton, D.M. Memory B cells: Effectors of long-lived immune responses. Eur. J. Immunol. 2009, 39, 2065–2075. [Google Scholar] [CrossRef]
- Nicholson, L.B. The immune system. Essays Biochem. 2016, 60, 275–301. [Google Scholar] [CrossRef] [PubMed]
- Yatim, K.M.; Lakkis, F.G. A brief journey through the immune system. Clin. J. Am. Soc. Nephrol. 2015, 10, 1274–1281. [Google Scholar] [CrossRef] [PubMed]

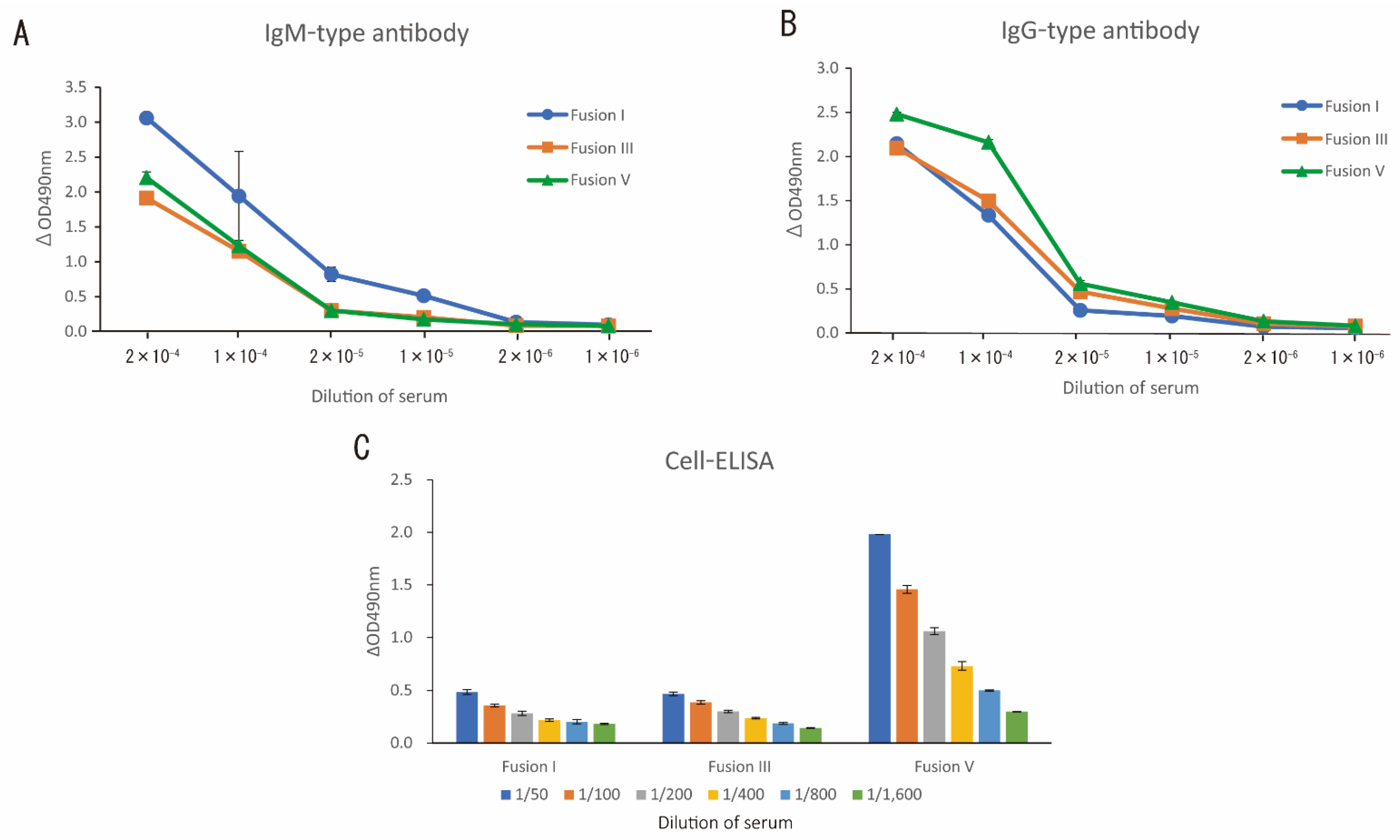

| Immunization Method | Number of DNA Immunization (Total Weeks for Immunization) a) | Fusion Day b | Number of Wells | Hybridoma Positive Wells | Cell-ELISA Positive Wells c | Isotype-Determined Wells (A) | Isotype | Rate of IgG Production (B)/(A) ×100 (%) | Rate of IgM Production (C)/(A) ×100 (%) | |
|---|---|---|---|---|---|---|---|---|---|---|
| IgG-Positive Wells d (B) | IgM-Positive Wells e (C) | |||||||||
| Fusion I | 3 (9) | 3 | 192 | 107 | 14 | 14 | 0 | 13 | 0 | 92.9 |
| Fusion II | 3 (8) | 5 | 288 | 29 | 8 | 8 | 4 | 8 | 50.0 | 100.0 |
| Fusion III | 3 (11) | 5 | 288 | 25 | 9 | 5 | 4 | 5 | 80.0 | 100.0 |
| Fusion IV | 4 (12) | 5 | 192 | 78 | 22 | 13 | 13 | 6 | 100.0 | 46.2 |
| Fusion V | 4 (15) | 5 | 192 | 22 | 3 | 3 | 3 | 0 | 100.0 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Isozaki, Y.; Tsumoto, K.; Tomita, M. Class-Switching of B Lymphocytes by DNA and Cell Immunization for Stereospecific Monoclonal Antibodies against Native GPCR. Immuno 2021, 1, 432-441. https://doi.org/10.3390/immuno1040031
Isozaki Y, Tsumoto K, Tomita M. Class-Switching of B Lymphocytes by DNA and Cell Immunization for Stereospecific Monoclonal Antibodies against Native GPCR. Immuno. 2021; 1(4):432-441. https://doi.org/10.3390/immuno1040031
Chicago/Turabian StyleIsozaki, Yushi, Kanta Tsumoto, and Masahiro Tomita. 2021. "Class-Switching of B Lymphocytes by DNA and Cell Immunization for Stereospecific Monoclonal Antibodies against Native GPCR" Immuno 1, no. 4: 432-441. https://doi.org/10.3390/immuno1040031
APA StyleIsozaki, Y., Tsumoto, K., & Tomita, M. (2021). Class-Switching of B Lymphocytes by DNA and Cell Immunization for Stereospecific Monoclonal Antibodies against Native GPCR. Immuno, 1(4), 432-441. https://doi.org/10.3390/immuno1040031







