The Role of Platelet Molecules in Risk Stratification of Patients with COVID-19
Abstract
:1. Introduction
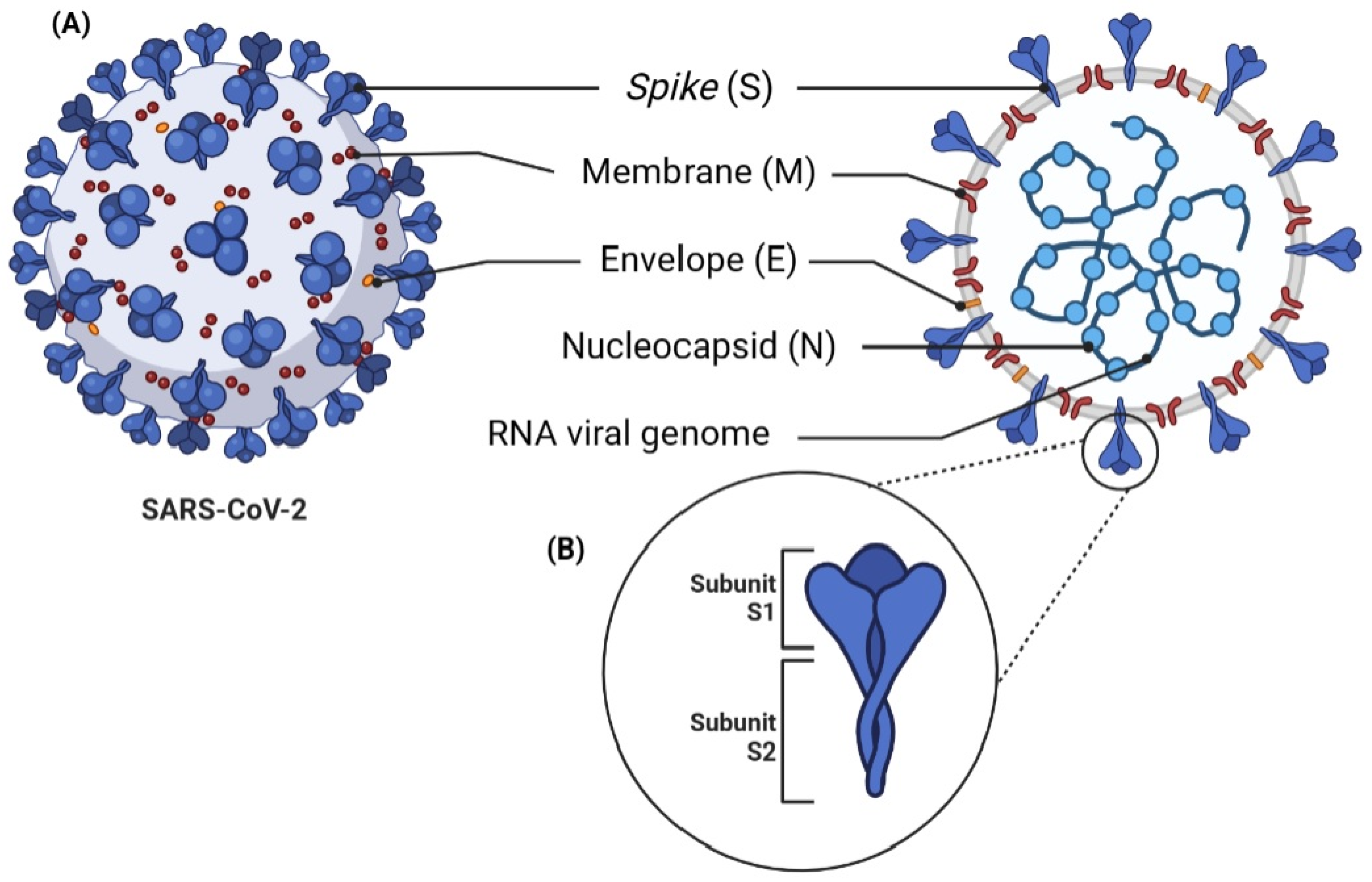
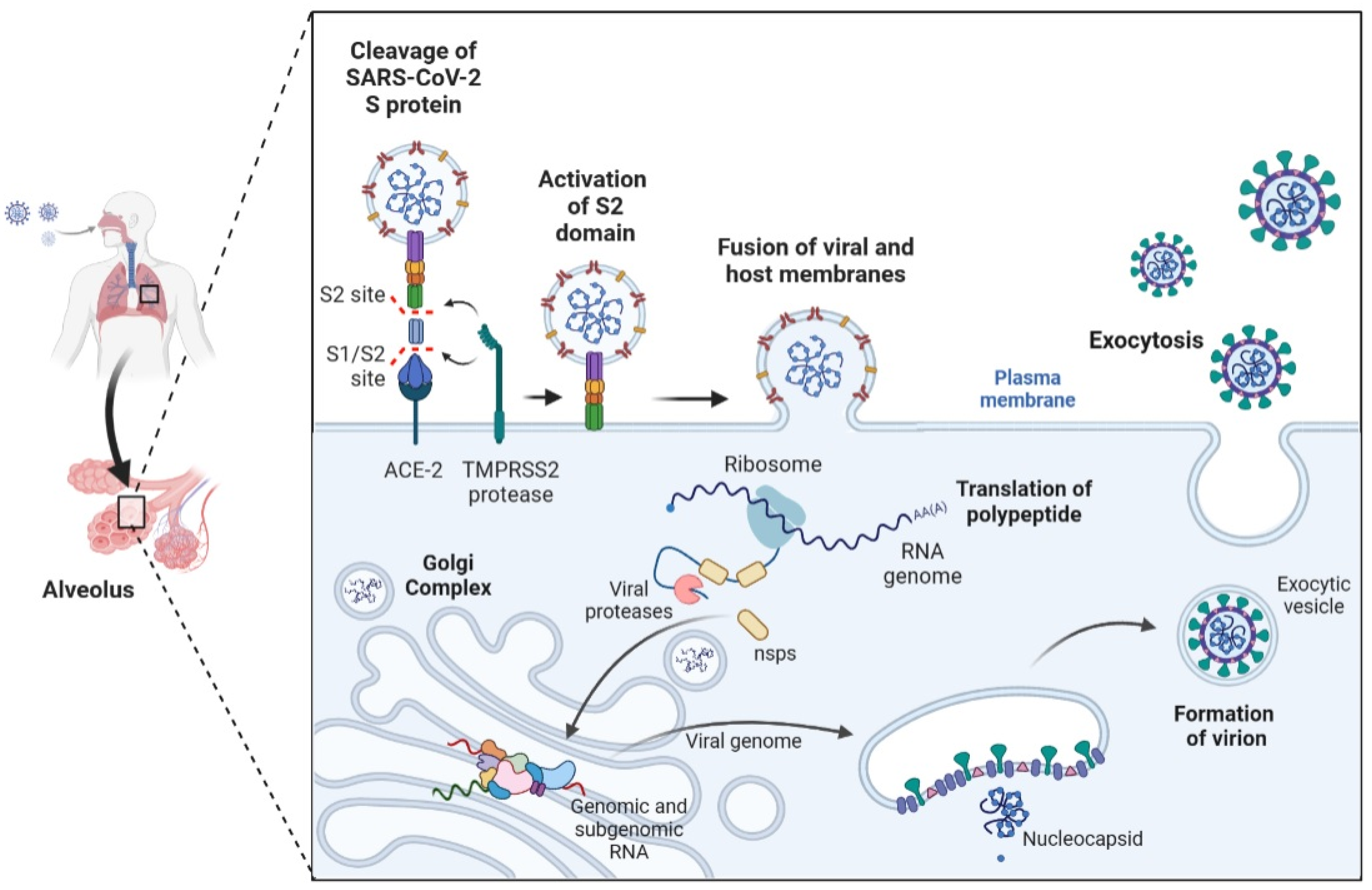
2. Pathophysiology and Pathogenesis of SARS-CoV-2
3. Immunothrombosis and SARS-CoV-2 Infection
4. Viral Infections, including SARS-CoV-2 and Its Interaction with Platelets
5. Platelet Markers and COVID-19
5.1. P-Selectin
5.2. Von Willebrand Factor (VWF)
5.3. Plasminogen Activator Inhibitor (PAI-1)
5.4. Platelet Factor 4 (PF4)
5.5. Transforming Growth Factor-Beta (TGF-β)
5.6. Platelet-Activating Factor (PAF)
5.7. MMP-2, MMP-9
5.8. Platelet-Derived Growth Factor (PDGF)
5.9. RANTES (CCL5)
5.10. Glutamate
5.11. Serotonin (5-HT)
5.12. C-Type Lectin-like Receptor 2 (CLEC-2)
5.13. Microparticles (MPs)
6. Treatment and Thromboprophylaxis in COVID-19
7. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Hartenian, E.; Nandakumar, D.; Lari, A.; Ly, M.; Tucker, J.M.; Glaunsinger, B.A. The Molecular Virology of Coronaviruses. J. Biol. Chem. 2020, 295, 12910–12934. [Google Scholar] [CrossRef]
- Gu, S.X.; Tyagi, T.; Jain, K.; Gu, V.W.; Lee, S.H.; Hwa, J.M.; Kwan, J.M.; Krause, D.S.; Lee, A.I.; Halene, S.; et al. Thrombocytopathy and Endotheliopathy: Crucial Contributors to COVID-19 Thromboinflammation. Nat. Rev. Cardiol. 2021, 18, 194–209. [Google Scholar] [CrossRef]
- Kang, S.; Yang, M.; Hong, Z.; Zhang, L.; Huang, Z.; Chen, X.; He, S.; Zhou, Z.; Zhou, Z.; Chen, Q.; et al. Crystal Structure of SARS-CoV-2 Nucleocapsid Protein RNA Binding Domain Reveals Potential Unique Drug Targeting Sites. Acta Pharm. Sin. B 2020, 10, 1228–1238. [Google Scholar] [CrossRef] [PubMed]
- Manne, B.K.; Denorme, F.; Middleton, E.A.; Portier, I.; Rowley, J.W.; Stubben, C.; Petrey, A.C.; Tolley, N.D.; Guo, L.; Cody, M.; et al. Platelet Gene Expression and Function in Patients with COVID-19. Blood 2020, 136, 1317–1329. [Google Scholar] [CrossRef] [PubMed]
- Chilamakuri, R.; Agarwal, S. COVID-19: Characteristics and Therapeutics. Cells 2021, 10, 206. [Google Scholar] [CrossRef] [PubMed]
- Machhi, J.; Herskovitz, J.; Senan, A.M.; Dutta, D.; Nath, B.; Oleynikov, M.D.; Blomberg, W.R.; Meigs, D.D.; Hasan, M.; Patel, M.; et al. The Natural History, Pathobiology, and Clinical Manifestations of SARS-CoV-2 Infections. J. Neuroimmune Pharmacol. 2020, 15, 359–386. [Google Scholar] [CrossRef]
- Pillalamarri, N.; Abdullah; Ren, G.; Khan, L.; Ullah, A.; Jonnakuti, S.; Ullah, M. Exploring the Utility of Extracellular Vesicles in Ameliorating Viral Infection-Associated Inflammation, Cytokine Storm and Tissue Damage. Transl. Oncol. 2021, 14, 101095. [Google Scholar] [CrossRef]
- Dhama, K.; Khan, S.; Tiwari, R.; Sircar, S.; Bhat, S.; Malik, Y.S.; Singh, K.P.; Chaicumpa, W.; Bonilla-Aldana, D.K.; Rodriguez-Morales, A.J. Coronavirus Disease 2019-COVID-19. Clin. Microbiol. Rev. 2020, 33, e00028-20. [Google Scholar] [CrossRef]
- Zhang, S.; Liu, Y.; Wang, X.; Yang, L.; Li, H.; Wang, Y.; Liu, M.; Zhao, X.; Xie, Y.; Yang, Y.; et al. SARS-CoV-2 Binds Platelet ACE2 to Enhance Thrombosis in COVID-19. J. Hematol. Oncol. 2020, 13, 120. [Google Scholar] [CrossRef]
- Connors, J.M.; Levy, J.H. COVID-19 and Its Implications for Thrombosis and Anticoagulation. Blood 2020, 135, 2033–2040. [Google Scholar] [CrossRef]
- Middleton, E.A.; Weyrich, A.S.; Zimmerman, G.A. Platelets in Pulmonary Immune Responses and Inflammatory Lung Diseases. Physiol. Rev. 2016, 96, 1211–1259. [Google Scholar] [CrossRef]
- Koupenova, M.; Clancy, L.; Corkrey, H.A.; Freedman, J.E. Circulating Platelets as Mediators of Immunity, Inflammation, and Thrombosis. Circ. Res. 2018, 122, 337–351. [Google Scholar] [CrossRef]
- Chaipan, C.; Soilleux, E.; Simpson, P.; Hofmann, H.; Gramberg, T.; Marzi, A.; Geier, M.; Stewart, E.; Eisemann, J.; Steinkasserer, A.; et al. DC-SIGN and CLEC-2 Mediate Human Immunodeficiency Virus Type 1 Capture by Platelets. J. Virol. 2006, 80, 8951–8960. [Google Scholar] [CrossRef] [PubMed]
- Solomon Tsegaye, T.; Gnirß, K.; Rahe-Meyer, N.; Kiene, M.; Krämer-Kühl, A.; Behrens, G.; Münch, J.; Pöhlmann, S. Platelet Activation Suppresses HIV-1 Infection of T Cells. Retrovirology 2013, 10, 48. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.; Feng, K.; Wang, Y.C.; Mei, J.J.; Ning, R.T.; Zheng, H.W.; Wang, J.J.; Worthen, G.S.; Wang, X.; Song, J.; et al. Critical Role of CXCL4 in the Lung Pathogenesis of Influenza (H1N1) Respiratory Infection. Mucosal Immunol. 2017, 10, 1529–1541. [Google Scholar] [CrossRef]
- Simon, A.Y.; Sutherland, M.R.; Pryzdial, E.L.G. Dengue Virus Binding and Replication by Platelets. Blood 2015, 126, 378–385. [Google Scholar] [CrossRef] [PubMed]
- Ojha, A.; Bhasym, A.; Mukherjee, S.; Annarapu, G.K.; Bhakuni, T.; Akbar, I.; Seth, T.; Vikram, N.K.; Vrati, S.; Basu, A.; et al. Platelet Factor 4 Promotes Rapid Replication and Propagation of Dengue and Japanese Encephalitis Viruses. EBioMedicine 2019, 39, 332–347. [Google Scholar] [CrossRef]
- Assinger, A.; Kral, J.B.; Yaiw, K.C.; Schrottmaier, W.C.; Kurzejamska, E.; Wang, Y.; Mohammad, A.-A.; Religa, P.; Rahbar, A.; Schabbauer, G.; et al. Human Cytomegalovirus-Platelet Interaction Triggers Toll-like Receptor 2-Dependent Proinflammatory and Proangiogenic Responses. Arterioscler. Thromb. Vasc. Biol. 2014, 34, 801–809. [Google Scholar] [CrossRef]
- Barrett, T.J.; Bilaloglu, S.; Cornwell, M.; Burgess, H.M.; Virginio, V.W.; Drenkova, K.; Ibrahim, H.; Yuriditsky, E.; Aphinyanaphongs, Y.; Lifshitz, M.; et al. Platelets Contribute to Disease Severity in COVID-19. J. Thromb. Haemost. 2021, 19, 3139–3153. [Google Scholar] [CrossRef]
- Hoffmann, M.; Kleine-Weber, H.; Schroeder, S.; Krüger, N.; Herrler, T.; Erichsen, S.; Schiergens, T.S.; Herrler, G.; Wu, N.-H.; Nitsche, A.; et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 2020, 181, 271–280. [Google Scholar] [CrossRef]
- Sungnak, W.; Huang, N.; Bécavin, C.; Berg, M.; Queen, R.; Litvinukova, M.; Talavera-López, C.; Maatz, H.; Reichart, D.; Sampaziotis, F.; et al. SARS-CoV-2 Entry Factors Are Highly Expressed in Nasal Epithelial Cells Together with Innate Immune Genes. Nat. Med. 2020, 26, 681–687. [Google Scholar] [CrossRef]
- Xu, H.; Zhong, L.; Deng, J.; Peng, J.; Dan, H.; Zeng, X.; Li, T.; Chen, Q. High Expression of ACE2 Receptor of 2019-NCoV on the Epithelial Cells of Oral Mucosa. Int. J. Oral. Sci. 2020, 12, 8. [Google Scholar] [CrossRef] [PubMed]
- Zumla, A.; Chan, J.F.W.; Azhar, E.I.; Hui, D.S.C.; Yuen, K.-Y. Coronaviruses—Drug Discovery and Therapeutic Options. Nat. Rev. Drug Discov. 2016, 15, 327–347. [Google Scholar] [CrossRef]
- Cao, X. COVID-19: Immunopathology and Its Implications for Therapy. Nat. Rev. Immunol. 2020, 20, 269–270. [Google Scholar] [CrossRef]
- Shi, Y.; Wang, Y.; Shao, C.; Huang, J.; Gan, J.; Huang, X.; Bucci, E.; Piacentini, M.; Ippolito, G.; Melino, G. COVID-19 Infection: The Perspectives on Immune Responses. Cell Death Differ. 2020, 27, 1451–1454. [Google Scholar] [CrossRef] [PubMed]
- Henry, B.M.; de Oliveira, M.H.S.; Benoit, S.; Plebani, M.; Lippi, G. Hematologic, Biochemical and Immune Biomarker Abnormalities Associated with Severe Illness and Mortality in Coronavirus Disease 2019 (COVID-19): A Meta-Analysis. Clin. Chem. Lab. Med. 2020, 58, 1021–1028. [Google Scholar] [CrossRef] [PubMed]
- Zeng, F.; Huang, Y.; Guo, Y.; Yin, M.; Chen, X.; Xiao, L.; Deng, G. Association of Inflammatory Markers with the Severity of COVID-19: A Meta-Analysis. Int. J. Infect. Dis. 2020, 96, 467–474. [Google Scholar] [CrossRef]
- Bao, C.; Tao, X.; Cui, W.; Yi, B.; Pan, T.; Young, K.H.; Qian, W. SARS-CoV-2 Induced Thrombocytopenia as an Important Biomarker Significantly Correlated with Abnormal Coagulation Function, Increased Intravascular Blood Clot Risk and Mortality in COVID-19 Patients. Exp. Hematol. Oncol. 2020, 9, 16. [Google Scholar] [CrossRef]
- Goshua, G.; Pine, A.B.; Meizlish, M.L.; Chang, C.-H.; Zhang, H.; Bahel, P.; Baluha, A.; Bar, N.; Bona, R.D.; Burns, A.J.; et al. Endotheliopathy in COVID-19-Associated Coagulopathy: Evidence from a Single-Centre, Cross-Sectional Study. Lancet Haematol. 2020, 7, e575–e582. [Google Scholar] [CrossRef]
- Safiabadi Tali, S.H.; LeBlanc, J.J.; Sadiq, Z.; Oyewunmi, O.D.; Camargo, C.; Nikpour, B.; Armanfard, N.; Sagan, S.M.; Jahanshahi-Anbuhi, S. Tools and Techniques for Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2)/COVID-19 Detection. Clin. Microbiol. Rev. 2021, 34, e00228-20. [Google Scholar] [CrossRef]
- Zhang, Y.; Xiao, M.; Zhang, S.; Xia, P.; Cao, W.; Jiang, W.; Chen, H.; Ding, X.; Zhao, H.; Zhang, H.; et al. Coagulopathy and Antiphospholipid Antibodies in Patients with COVID-19. N. Engl. J. Med. 2020, 382, e38. [Google Scholar] [CrossRef] [PubMed]
- Iba, T.; Levy, J.H.; Levi, M.; Connors, J.M.; Thachil, J. Coagulopathy of Coronavirus Disease 2019. Crit. Care Med. 2020, 48, 1358–1364. [Google Scholar] [CrossRef] [PubMed]
- Peyvandi, F.; Artoni, A.; Novembrino, C.; Aliberti, S.; Panigada, M.; Boscarino, M.; Gualtierotti, R.; Rossi, F.; Palla, R.; Martinelli, I.; et al. Hemostatic Alterations in COVID-19. Haematologica 2021, 106, 1472–1475. [Google Scholar] [CrossRef]
- Lodigiani, C.; Iapichino, G.; Carenzo, L.; Cecconi, M.; Ferrazzi, P.; Sebastian, T.; Kucher, N.; Studt, J.-D.; Sacco, C.; Bertuzzi, A.; et al. Venous and Arterial Thromboembolic Complications in COVID-19 Patients Admitted to an Academic Hospital in Milan, Italy. Thromb. Res. 2020, 191, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Poissy, J.; Goutay, J.; Caplan, M.; Parmentier, E.; Duburcq, T.; Lassalle, F.; Jeanpierre, E.; Rauch, A.; Labreuche, J.; Susen, S.; et al. Pulmonary Embolism in Patients With COVID-19: Awareness of an Increased Prevalence. Circulation 2020, 142, 184–186. [Google Scholar] [CrossRef] [PubMed]
- Klok, F.A.; Kruip, M.J.H.A.; van der Meer, N.J.M.; Arbous, M.S.; Gommers, D.; Kant, K.M.; Kaptein, F.H.J.; van Paassen, J.; Stals, M.a.M.; Huisman, M.V.; et al. Confirmation of the High Cumulative Incidence of Thrombotic Complications in Critically Ill ICU Patients with COVID-19: An Updated Analysis. Thromb. Res. 2020, 191, 148–150. [Google Scholar] [CrossRef]
- Darif, D.; Hammi, I.; Kihel, A.; El Idrissi Saik, I.; Guessous, F.; Akarid, K. The Pro-Inflammatory Cytokines in COVID-19 Pathogenesis: What Goes Wrong? Microb. Pathog. 2021, 153, 104799. [Google Scholar] [CrossRef] [PubMed]
- Delabranche, X.; Helms, J.; Meziani, F. Immunohaemostasis: A New View on Haemostasis during Sepsis. Ann. Intensive Care 2017, 7, 117. [Google Scholar] [CrossRef]
- Hottz, E.D.; Azevedo-Quintanilha, I.G.; Palhinha, L.; Teixeira, L.; Barreto, E.A.; Pão, C.R.R.; Righy, C.; Franco, S.; Souza, T.M.L.; Kurtz, P.; et al. Platelet Activation and Platelet-Monocyte Aggregate Formation Trigger Tissue Factor Expression in Patients with Severe COVID-19. Blood 2020, 136, 1330–1341. [Google Scholar] [CrossRef]
- Hottz, E.D.; Bozza, P.T. Platelet-Leukocyte Interactions in COVID-19: Contributions to Hypercoagulability, Inflammation, and Disease Severity. Res. Pract. Thromb. Haemost. 2022, 6, e12709. [Google Scholar] [CrossRef] [PubMed]
- Xu, P.; Zhou, Q.; Xu, J. Mechanism of Thrombocytopenia in COVID-19 Patients. Ann. Hematol. 2020, 99, 1205–1208. [Google Scholar] [CrossRef] [PubMed]
- Hottz, E.D.; Medeiros-de-Moraes, I.M.; Vieira-de-Abreu, A.; de Assis, E.F.; Vals-de-Souza, R.; Castro-Faria-Neto, H.C.; Weyrich, A.S.; Zimmerman, G.A.; Bozza, F.A.; Bozza, P.T. Platelet Activation and Apoptosis Modulate Monocyte Inflammatory Responses in Dengue. J. Immunol. 2014, 193, 1864–1872. [Google Scholar] [CrossRef] [PubMed]
- Koupenova, M.; Corkrey, H.A.; Vitseva, O.; Manni, G.; Pang, C.J.; Clancy, L.; Yao, C.; Rade, J.; Levy, D.; Wang, J.P.; et al. The Role of Platelets in Mediating a Response to Human Influenza Infection. Nat. Commun. 2019, 10, 1780. [Google Scholar] [CrossRef] [PubMed]
- Dib, P.R.B.; Quirino-Teixeira, A.C.; Merij, L.B.; Pinheiro, M.B.M.; Rozini, S.V.; Andrade, F.B.; Hottz, E.D. Innate Immune Receptors in Platelets and Platelet-Leukocyte Interactions. J. Leukoc. Biol. 2020, 108, 1157–1182. [Google Scholar] [CrossRef] [PubMed]
- Maouia, A.; Rebetz, J.; Kapur, R.; Semple, J.W. The Immune Nature of Platelets Revisited. Transfus. Med. Rev. 2020, 34, 209–220. [Google Scholar] [CrossRef]
- Antoniak, S.; Mackman, N. Platelets and Viruses. Platelets 2021, 32, 325–330. [Google Scholar] [CrossRef]
- Zhang, W.; Nardi, M.A.; Borkowsky, W.; Li, Z.; Karpatkin, S. Role of Molecular Mimicry of Hepatitis C Virus Protein with Platelet GPIIIa in Hepatitis C–Related Immunologic Thrombocytopenia. Blood 2009, 113, 4086–4093. [Google Scholar] [CrossRef]
- Pugliese, A.; Gennero, L.; Cutufia, M.; Enrietto, M.; Morra, E.; Pescarmona, P.; Ponzetto, A. HCV Infective Virions Can Be Carried by Human Platelets. Cell Biochem. Funct. 2004, 22, 353–358. [Google Scholar] [CrossRef] [PubMed]
- Forghani, B.; Schmidt, N.J. Association of Herpes Simplex Virus with Platelets of Experimentally Infected Mice. Arch. Virol. 1983, 76, 269–274. [Google Scholar] [CrossRef]
- Koupenova, M.; Freedman, J.E. Platelets and Immunity: Going Viral. Arterioscler. Thromb. Vasc. Biol. 2020, 40, 1605–1607. [Google Scholar] [CrossRef]
- Yeaman, M.R. 29—The Role of Platelets in Antimicrobial Host Defense. In Platelets, 4th ed.; Michelson, A.D., Ed.; Academic Press: Cambridge, MA, USA, 2019; pp. 523–546. ISBN 978-0-12-813456-6. [Google Scholar]
- Rayes, J.; Bourne, J.H.; Brill, A.; Watson, S.P. The Dual Role of Platelet-Innate Immune Cell Interactions in Thrombo-Inflammation. Res. Pract. Thromb. Haemost. 2020, 4, 23–35. [Google Scholar] [CrossRef] [PubMed]
- Maynard, D.M.; Heijnen, H.F.G.; Horne, M.K.; White, J.G.; Gahl, W.A. Proteomic Analysis of Platelet α-Granules Using Mass Spectrometry. J. Thromb. Haemost. 2007, 5, 1945–1955. [Google Scholar] [CrossRef] [PubMed]
- Lemons, P.P.; Chen, D.; Bernstein, A.M.; Bennett, M.K.; Whiteheart, S.W. Regulated Secretion in Platelets: Identification of Elements of the Platelet Exocytosis Machinery. Blood 1997, 90, 1490–1500. [Google Scholar] [CrossRef]
- Morrell, C.N.; Aggrey, A.A.; Chapman, L.M.; Modjeski, K.L. Emerging Roles for Platelets as Immune and Inflammatory Cells. Blood 2014, 123, 2759–2767. [Google Scholar] [CrossRef]
- Wang, Y.; Ouyang, Y.; Liu, B.; Ma, X.; Ding, R. Platelet Activation and Antiplatelet Therapy in Sepsis: A Narrative Review. Thromb. Res. 2018, 166, 28–36. [Google Scholar] [CrossRef] [PubMed]
- McFadyen, J.D.; Stevens, H.; Peter, K. The Emerging Threat of (Micro)Thrombosis in COVID-19 and Its Therapeutic Implications. Circ. Res. 2020, 127, 571–587. [Google Scholar] [CrossRef]
- Tang, N.; Li, D.; Wang, X.; Sun, Z. Abnormal Coagulation Parameters Are Associated with Poor Prognosis in Patients with Novel Coronavirus Pneumonia. J. Thromb. Haemost. 2020, 18, 844–847. [Google Scholar] [CrossRef]
- Zhang, L.; Feng, X.; Zhang, D.; Jiang, C.; Mei, H.; Wang, J.; Zhang, C.; Li, H.; Xia, X.; Kong, S.; et al. Deep Vein Thrombosis in Hospitalized Patients With COVID-19 in Wuhan, China: Prevalence, Risk Factors, and Outcome. Circulation 2020, 142, 114–128. [Google Scholar] [CrossRef]
- Gorog, D.A.; Storey, R.F.; Gurbel, P.A.; Tantry, U.S.; Berger, J.S.; Chan, M.Y.; Duerschmied, D.; Smyth, S.S.; Parker, W.A.E.; Ajjan, R.A.; et al. Current and Novel Biomarkers of Thrombotic Risk in COVID-19: A Consensus Statement from the International COVID-19 Thrombosis Biomarkers Colloquium. Nat. Rev. Cardiol. 2022, 19, 475–495. [Google Scholar] [CrossRef]
- Blann, A.D.; Nadar, S.K.; Lip, G.Y.H. The Adhesion Molecule P-Selectin and Cardiovascular Disease. Eur. Heart J. 2003, 24, 2166–2179. [Google Scholar] [CrossRef]
- Cambien, B.; Wagner, D.D. A New Role in Hemostasis for the Adhesion Receptor P-Selectin. Trends Mol. Med. 2004, 10, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Watany, M.M.; Abdou, S.; Elkolaly, R.; Elgharbawy, N.; Hodeib, H. Correction to: Evaluation of Admission Levels of P, E and L Selectins as Predictors for Thrombosis in Hospitalized COVID-19 Patients. Clin. Exp. Med. 2023, 23, 163. [Google Scholar] [CrossRef]
- Sadler, J.E. Biochemistry and Genetics of von Willebrand Factor. Annu. Rev. Biochem. 1998, 67, 395–424. [Google Scholar] [CrossRef]
- Chen, P.-C.; Kutzki, F.; Mojzisch, A.; Simon, B.; Xu, E.-R.; Aponte-Santamaría, C.; Horny, K.; Jeffries, C.; Schneppenheim, R.; Wilmanns, M.; et al. Structure and Dynamics of the von Willebrand Factor C6 Domain. J. Struct. Biol. 2022, 214, 107923. [Google Scholar] [CrossRef]
- Edvardsen, M.S.; Hindberg, K.; Hansen, E.-S.; Morelli, V.M.; Ueland, T.; Aukrust, P.; Brækkan, S.K.; Evensen, L.H.; Hansen, J.-B. Plasma Levels of von Willebrand Factor and Future Risk of Incident Venous Thromboembolism. Blood Adv. 2021, 5, 224–232. [Google Scholar] [CrossRef]
- Sadler, J.E.; Budde, U.; Eikenboom, J.C.J.; Favaloro, E.J.; Hill, F.G.H.; Holmberg, L.; Ingerslev, J.; Lee, C.A.; Lillicrap, D.; Mannucci, P.M.; et al. Update on the Pathophysiology and Classification of von Willebrand Disease: A Report of the Subcommittee on von Willebrand Factor. J. Thromb. Haemost. 2006, 4, 2103–2114. [Google Scholar] [CrossRef]
- Babkina, A.S.; Ostrova, I.V.; Yadgarov, M.Y.; Kuzovlev, A.N.; Grechko, A.V.; Volkov, A.V.; Golubev, A.M. The Role of Von Willebrand Factor in the Pathogenesis of Pulmonary Vascular Thrombosis in COVID-19. Viruses 2022, 14, 211. [Google Scholar] [CrossRef]
- Philippe, A.; Chocron, R.; Gendron, N.; Bory, O.; Beauvais, A.; Peron, N.; Khider, L.; Guerin, C.L.; Goudot, G.; Levasseur, F.; et al. Circulating Von Willebrand Factor and High Molecular Weight Multimers as Markers of Endothelial Injury Predict COVID-19 in-Hospital Mortality. Angiogenesis 2021, 24, 505–517. [Google Scholar] [CrossRef]
- Doevelaar, A.A.N.; Bachmann, M.; Hölzer, B.; Seibert, F.S.; Rohn, B.J.; Bauer, F.; Witzke, O.; Dittmer, U.; Bachmann, M.; Yilmaz, S.; et al. Von Willebrand Factor Multimer Formation Contributes to Immunothrombosis in Coronavirus Disease 2019. Crit. Care Med. 2021, 49, e512–e520. [Google Scholar] [CrossRef]
- Ladikou, E.E.; Sivaloganathan, H.; Milne, K.M.; Arter, W.E.; Ramasamy, R.; Saad, R.; Stoneham, S.M.; Philips, B.; Eziefula, A.C.; Chevassut, T. Von Willebrand Factor (VWF): Marker of Endothelial Damage and Thrombotic Risk in COVID-19? Clin. Med. 2020, 20, e178–e182. [Google Scholar] [CrossRef]
- Li, K.; Yao, L.; Wang, J.; Song, H.; Zhang, Y.-H.; Bai, X.; Zhang, K.; Zhou, D.-M.; Ai, D.; Zhu, Y. SARS-CoV-2 Spike Protein Promotes VWF Secretion and Thrombosis via Endothelial Cytoskeleton-Associated Protein 4 (CKAP4). Signal Transduct. Target. Ther. 2022, 7, 332. [Google Scholar] [CrossRef] [PubMed]
- Longstaff, C.; Kolev, K. Basic Mechanisms and Regulation of Fibrinolysis. J. Thromb. Haemost. 2015, 13 (Suppl. 1), S98–S105. [Google Scholar] [CrossRef]
- Wright, F.L.; Vogler, T.O.; Moore, E.E.; Moore, H.B.; Wohlauer, M.V.; Urban, S.; Nydam, T.L.; Moore, P.K.; McIntyre, R.C. Fibrinolysis Shutdown Correlation with Thromboembolic Events in Severe COVID-19 Infection. J. Am. Coll. Surg. 2020, 231, 193–203.e1. [Google Scholar] [CrossRef] [PubMed]
- Meltzer, M.E.; Lisman, T.; de Groot, P.G.; Meijers, J.C.M.; le Cessie, S.; Doggen, C.J.M.; Rosendaal, F.R. Venous Thrombosis Risk Associated with Plasma Hypofibrinolysis Is Explained by Elevated Plasma Levels of TAFI and PAI-1. Blood 2010, 116, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Zuo, Y.; Warnock, M.; Harbaugh, A.; Yalavarthi, S.; Gockman, K.; Zuo, M.; Madison, J.A.; Knight, J.S.; Kanthi, Y.; Lawrence, D.A. Plasma Tissue Plasminogen Activator and Plasminogen Activator Inhibitor-1 in Hospitalized COVID-19 Patients. Sci. Rep. 2021, 11, 1580. [Google Scholar] [CrossRef] [PubMed]
- Nougier, C.; Benoit, R.; Simon, M.; Desmurs-Clavel, H.; Marcotte, G.; Argaud, L.; David, J.S.; Bonnet, A.; Negrier, C.; Dargaud, Y. Hypofibrinolytic State and High Thrombin Generation May Play a Major Role in SARS-COV2 Associated Thrombosis. J. Thromb. Haemost. 2020, 18, 2215–2219. [Google Scholar] [CrossRef]
- Chen, R.; Yan, J.; Liu, P.; Wang, Z.; Wang, C. Plasminogen Activator Inhibitor Links Obesity and Thrombotic Cerebrovascular Diseases: The Roles of PAI-1 and Obesity on Stroke. Metab. Brain Dis. 2017, 32, 667–673. [Google Scholar] [CrossRef]
- Kowalska, M.A.; Rauova, L.; Poncz, M. Role of the Platelet Chemokine Platelet Factor 4 (PF4) in Hemostasis and Thrombosis. Thromb. Res. 2010, 125, 292–296. [Google Scholar] [CrossRef]
- Liu, Z.-Y.; Sun, M.-X.; Hua, M.-Q.; Zhang, H.-X.; Mu, G.-Y.; Zhou, S.; Wang, Z.; Xiang, Q.; Cui, Y.-M. New Perspectives on the Induction and Acceleration of Immune-Associated Thrombosis by PF4 and VWF. Front. Immunol. 2023, 14, 1098665. [Google Scholar] [CrossRef]
- Scheuerer, B.; Ernst, M.; Dürrbaum-Landmann, I.; Fleischer, J.; Grage-Griebenow, E.; Brandt, E.; Flad, H.-D.; Petersen, F. The CXC-Chemokine Platelet Factor 4 Promotes Monocyte Survival and Induces Monocyte Differentiation into Macrophages. Blood 2000, 95, 1158–1166. [Google Scholar] [CrossRef]
- Kasper, B.; Brandt, E.; Brandau, S.; Petersen, F. Platelet Factor 4 (CXC Chemokine Ligand 4) Differentially Regulates Respiratory Burst, Survival, and Cytokine Expression of Human Monocytes by Using Distinct Signaling Pathways. J. Immunol. 2007, 179, 2584–2591. [Google Scholar] [CrossRef] [PubMed]
- Eslin, D.E.; Zhang, C.; Samuels, K.J.; Rauova, L.; Zhai, L.; Niewiarowski, S.; Cines, D.B.; Poncz, M.; Kowalska, M.A. Transgenic Mice Studies Demonstrate a Role for Platelet Factor 4 in Thrombosis: Dissociation between Anticoagulant and Antithrombotic Effect of Heparin. Blood 2004, 104, 3173–3180. [Google Scholar] [CrossRef] [PubMed]
- Ebeyer-Masotta, M.; Eichhorn, T.; Weiss, R.; Lauková, L.; Weber, V. Activated Platelets and Platelet-Derived Extracellular Vesicles Mediate COVID-19-Associated Immunothrombosis. Front. Cell Dev. Biol. 2022, 10, 914891. [Google Scholar] [CrossRef] [PubMed]
- Middleton, E.A.; He, X.-Y.; Denorme, F.; Campbell, R.A.; Ng, D.; Salvatore, S.P.; Mostyka, M.; Baxter-Stoltzfus, A.; Borczuk, A.C.; Loda, M.; et al. Neutrophil Extracellular Traps Contribute to Immunothrombosis in COVID-19 Acute Respiratory Distress Syndrome. Blood 2020, 136, 1169–1179. [Google Scholar] [CrossRef] [PubMed]
- Comer, S.P.; Cullivan, S.; Szklanna, P.B.; Weiss, L.; Cullen, S.; Kelliher, S.; Smolenski, A.; Murphy, C.; Altaie, H.; Curran, J.; et al. COVID-19 Induces a Hyperactive Phenotype in Circulating Platelets. PLoS Biol. 2021, 19, e3001109. [Google Scholar] [CrossRef]
- Dragonetti, D.; Guarini, G.; Pizzuti, M. Detection of Anti-Heparin-PF4 Complex Antibodies in COVID-19 Patients on Heparin Therapy. Blood Transfus. 2020, 18, 328. [Google Scholar] [CrossRef]
- Brodard, J.; Kremer Hovinga, J.A.; Fontana, P.; Studt, J.-D.; Gruel, Y.; Greinacher, A. COVID-19 Patients Often Show High-Titer Non-Platelet-Activating Anti-PF4/Heparin IgG Antibodies. J. Thromb. Haemost. 2021, 19, 1294–1298. [Google Scholar] [CrossRef]
- Rauova, L.; Zhai, L.; Kowalska, M.A.; Arepally, G.M.; Cines, D.B.; Poncz, M. Role of Platelet Surface PF4 Antigenic Complexes in Heparin-Induced Thrombocytopenia Pathogenesis: Diagnostic and Therapeutic Implications. Blood 2006, 107, 2346–2353. [Google Scholar] [CrossRef]
- Warkentin, T.E.; Levine, M.N.; Hirsh, J.; Horsewood, P.; Roberts, R.S.; Gent, M.; Kelton, J.G. Heparin-Induced Thrombocytopenia in Patients Treated with Low-Molecular-Weight Heparin or Unfractionated Heparin. N. Engl. J. Med. 1995, 332, 1330–1336. [Google Scholar] [CrossRef]
- Liu, X.; Zhang, X.; Xiao, Y.; Gao, T.; Wang, G.; Wang, Z.; Zhang, Z.; Hu, Y.; Dong, Q.; Zhao, S.; et al. Heparin-Induced Thrombocytopenia Is Associated with a High Risk of Mortality in Critical COVID-19 Patients Receiving Heparin-Involved Treatment. medRxiv 2020. [Google Scholar] [CrossRef]
- Arguinchona, L.M.; Zagona-Prizio, C.; Joyce, M.E.; Chan, E.D.; Maloney, J.P. Microvascular Significance of TGF-β Axis Activation in COVID-19. Front. Cardiovasc. Med. 2022, 9, 1054690. [Google Scholar] [CrossRef] [PubMed]
- Hoying, J.B.; Yin, M.; Diebold, R.; Ormsby, I.; Becker, A.; Doetschman, T. Transforming Growth Factor Β1 Enhances Platelet Aggregation through a Non-Transcriptional Effect on the Fibrinogen Receptor. J. Biol. Chem. 1999, 274, 31008–31013. [Google Scholar] [CrossRef]
- Ghazavi, A.; Ganji, A.; Keshavarzian, N.; Rabiemajd, S.; Mosayebi, G. Cytokine Profile and Disease Severity in Patients with COVID-19. Cytokine 2021, 137, 155323. [Google Scholar] [CrossRef] [PubMed]
- Colarusso, C.; Maglio, A.; Terlizzi, M.; Vitale, C.; Molino, A.; Pinto, A.; Vatrella, A.; Sorrentino, R. Post-COVID-19 Patients Who Develop Lung Fibrotic-like Changes Have Lower Circulating Levels of IFN-β but Higher Levels of IL-1α and TGF-β. Biomedicines 2021, 9, 1931. [Google Scholar] [CrossRef] [PubMed]
- Ferreira-Gomes, M.; Kruglov, A.; Durek, P.; Heinrich, F.; Tizian, C.; Heinz, G.A.; Pascual-Reguant, A.; Du, W.; Mothes, R.; Fan, C.; et al. SARS-CoV-2 in Severe COVID-19 Induces a TGF-β-Dominated Chronic Immune Response That Does Not Target Itself. Nat. Commun. 2021, 12, 1961. [Google Scholar] [CrossRef]
- Witkowski, M.; Tizian, C.; Ferreira-Gomes, M.; Niemeyer, D.; Jones, T.C.; Heinrich, F.; Frischbutter, S.; Angermair, S.; Hohnstein, T.; Mattiola, I.; et al. Untimely TGFβ Responses in COVID-19 Limit Antiviral Functions of NK Cells. Nature 2021, 600, 295–301. [Google Scholar] [CrossRef]
- Prescott, S.M.; Zimmerman, G.A.; Stafforini, D.M.; McIntyre, T.M. Platelet-Activating Factor and Related Lipid Mediators. Annu. Rev. Biochem. 2000, 69, 419–445. [Google Scholar] [CrossRef]
- Zimmerman, G.A.; McIntyre, T.M.; Prescott, S.M.; Stafforini, D.M. The Platelet-Activating Factor Signaling System and Its Regulators in Syndromes of Inflammation and Thrombosis. Crit. Care Med. 2002, 30, S294–S301. [Google Scholar] [CrossRef]
- Kelesidis, T.; Papakonstantinou, V.; Detopoulou, P.; Fragopoulou, E.; Chini, M.; Lazanas, M.C.; Antonopoulou, S. The Role of Platelet-Activating Factor in Chronic Inflammation, Immune Activation, and Comorbidities Associated with HIV Infection. AIDS Rev. 2015, 17, 191–201. [Google Scholar]
- Detopoulou, P.; Nomikos, T.; Fragopoulou, E.; Chrysohoou, C.; Antonopoulou, S. Platelet Activating Factor in Heart Failure: Potential Role in Disease Progression and Novel Target for Therapy. Curr. Heart Fail. Rep. 2013, 10, 122–129. [Google Scholar] [CrossRef]
- Klein, M.; Dao, V.; Khan, F. A Review of Platelet-Activating Factor As a Potential Contributor to Morbidity and Mortality Associated with Severe COVID-19. Clin. Appl. Thromb. Hemost. 2021, 27, 10760296211051764. [Google Scholar] [CrossRef] [PubMed]
- Theoharides, T.C.; Antonopoulou, S.; Demopoulos, C.A. Coronavirus 2019, Microthromboses, and Platelet Activating Factor. Clin. Ther. 2020, 42, 1850–1852. [Google Scholar] [CrossRef] [PubMed]
- Demopoulos, C.; Antonopoulou, S.; Theoharides, T.C. COVID-19, Microthromboses, Inflammation, and Platelet Activating Factor. Biofactors 2020, 46, 927–933. [Google Scholar] [CrossRef] [PubMed]
- Karhausen, J.; Choi, H.W.; Maddipati, K.R.; Mathew, J.P.; Ma, Q.; Boulaftali, Y.; Lee, R.H.; Bergmeier, W.; Abraham, S.N. Platelets Trigger Perivascular Mast Cell Degranulation to Cause Inflammatory Responses and Tissue Injury. Sci. Adv. 2020, 6, eaay6314. [Google Scholar] [CrossRef]
- Motta Junior, J.d.S.; Miggiolaro, A.F.R.D.S.; Nagashima, S.; de Paula, C.B.V.; Baena, C.P.; Scharfstein, J.; de Noronha, L. Mast Cells in Alveolar Septa of COVID-19 Patients: A Pathogenic Pathway That May Link Interstitial Edema to Immunothrombosis. Front. Immunol. 2020, 11, 574862. [Google Scholar] [CrossRef]
- de Carvalho, J.C.S.; da Silva-Neto, P.V.; Toro, D.M.; Fuzo, C.A.; Nardini, V.; Pimentel, V.E.; Pérez, M.M.; Fraga-Silva, T.F.C.; Oliveira, C.N.S.; Degiovani, A.M.; et al. The Interplay among Glucocorticoid Therapy, Platelet-Activating Factor and Endocannabinoid Release Influences the Inflammatory Response to COVID-19. Viruses 2023, 15, 573. [Google Scholar] [CrossRef]
- Santos-Martínez, M.J.; Medina, C.; Jurasz, P.; Radomski, M.W. Role of Metalloproteinases in Platelet Function. Thromb. Res. 2008, 121, 535–542. [Google Scholar] [CrossRef]
- Parks, W.; Wilson, C.; López-Boado, Y. Parks WC, Wilson CL, Lopez-Boado YSMatrix Metalloproteinases as Modulators of Inflammation and Innate Immunity. Nat. Rev. Immunol. 2004, 4, 617–629. [Google Scholar] [CrossRef]
- Chung, A.W.Y.; Radomski, A.; Alonso-Escolano, D.; Jurasz, P.; Stewart, M.W.; Malinski, T.; Radomski, M.W. Platelet–Leukocyte Aggregation Induced by PAR Agonists: Regulation by Nitric Oxide and Matrix Metalloproteinases. Br. J. Pharmacol. 2004, 143, 845–855. [Google Scholar] [CrossRef]
- Unal, R.; Yao-Borengasser, A.; Varma, V.; Rasouli, N.; Labbate, C.; Kern, P.A.; Ranganathan, G. Matrix Metalloproteinase-9 Is Increased in Obese Subjects and Decreases in Response to Pioglitazone. J. Clin. Endocrinol. Metab. 2010, 95, 2993–3001. [Google Scholar] [CrossRef]
- Marchesi, C.; Dentali, F.; Nicolini, E.; Maresca, A.M.; Tayebjee, M.H.; Franz, M.; Guasti, L.; Venco, A.; Schiffrin, E.L.; Lip, G.Y.H.; et al. Plasma Levels of Matrix Metalloproteinases and Their Inhibitors in Hypertension: A Systematic Review and Meta-Analysis. J. Hypertens. 2012, 30, 3–16. [Google Scholar] [CrossRef]
- Kapoor, C.; Vaidya, S.; Wadhwan, V.; Hitesh; Kaur, G.; Pathak, A. Seesaw of Matrix Metalloproteinases (MMPs). J. Cancer Res. Ther. 2016, 12, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Carolina, D.; Couto, A.E.; Campos, L.C.; Vasconcelos, T.F.; Michelon-Barbosa, J.; Corsi, C.A.; Mestriner, F.; Petroski-Moraes, B.C.; Garbellini-Diab, M.J.; Couto, D.M.; et al. MMP-2 and MMP-9 Levels in Plasma Are Altered and Associated with Mortality in COVID-19 Patients. Biomed. Pharmacother. 2021, 142, 112067. [Google Scholar] [CrossRef]
- Zingaropoli, M.A.; Latronico, T.; Pasculli, P.; Masci, G.M.; Merz, R.; Ciccone, F.; Dominelli, F.; Del Borgo, C.; Lichtner, M.; Iafrate, F.; et al. Tissue Inhibitor of Matrix Metalloproteinases-1 (TIMP-1) and Pulmonary Involvement in COVID-19 Pneumonia. Biomolecules 2023, 13, 1040. [Google Scholar] [CrossRef] [PubMed]
- Mohammadhosayni, M.; Sadat Mohammadi, F.; Ezzatifar, F.; Mahdavi Gorabi, A.; Khosrojerdi, A.; Aslani, S.; Hemmatzadeh, M.; Yazdani, S.; Arabi, M.; Marofi, F.; et al. Matrix Metalloproteinases Are Involved in the Development of Neurological Complications in Patients with Coronavirus Disease 2019. Int. Immunopharmacol. 2021, 100, 108076. [Google Scholar] [CrossRef]
- Razmi, N.; Baradaran, B.; Hejazi, M.; Hasanzadeh, M.; Mosafer, J.; Mokhtarzadeh, A.; de la Guardia, M. Recent Advances on Aptamer-Based Biosensors to Detection of Platelet-Derived Growth Factor. Biosens. Bioelectron. 2018, 113, 58–71. [Google Scholar] [CrossRef]
- Nasr El-Din, A.; Ata, K.A.E.-S.; Abdel-Gawad, A.R.; Fahmy, N.F. Impact of High Serum Levels of MMP-7, MMP-9, TGF-β and PDGF Macrophage Activation Markers on Severity of COVID-19 in Obese-Diabetic Patients. Infect. Drug Resist. 2021, 14, 4015–4025. [Google Scholar] [CrossRef]
- Petrey, A.C.; Qeadan, F.; Middleton, E.A.; Pinchuk, I.V.; Campbell, R.A.; Beswick, E.J. Cytokine Release Syndrome in COVID-19: Innate Immune, Vascular, and Platelet Pathogenic Factors Differ in Severity of Disease and Sex. J. Leukoc. Biol. 2021, 109, 55–66. [Google Scholar] [CrossRef]
- Marino, A.P.M.P.; da Silva, A.; dos Santos, P.; Pinto, L.M.d.O.; Gazzinelli, R.T.; Teixeira, M.M.; Lannes-Vieira, J. Regulated on Activation, Normal T Cell Expressed and Secreted (RANTES) Antagonist (Met-RANTES) Controls the Early Phase of Trypanosoma Cruzi-Elicited Myocarditis. Circulation 2004, 110, 1443–1449. [Google Scholar] [CrossRef]
- Alard, J.-E.; Ortega-Gomez, A.; Wichapong, K.; Bongiovanni, D.; Horckmans, M.; Megens, R.T.A.; Leoni, G.; Ferraro, B.; Rossaint, J.; Paulin, N.; et al. Recruitment of Classical Monocytes Can Be Inhibited by Disturbing Heteromers of Neutrophil HNP1 and Platelet CCL5. Sci. Transl. Med. 2015, 7, 317ra196. [Google Scholar] [CrossRef]
- Crawford, A.; Angelosanto, J.M.; Nadwodny, K.L.; Blackburn, S.D.; Wherry, E.J. A Role for the Chemokine RANTES in Regulating CD8 T Cell Responses during Chronic Viral Infection. PLoS Pathog. 2011, 7, e1002098. [Google Scholar] [CrossRef]
- Alam, R.; York, J.; Boyars, M.; Stafford, S.; Grant, J.A.; Lee, J.; Forsythe, P.; Sim, T.; Ida, N. Increased MCP-1, RANTES, and MIP-1alpha in Bronchoalveolar Lavage Fluid of Allergic Asthmatic Patients. Am. J. Respir. Crit. Care Med. 1996, 153, 1398–1404. [Google Scholar] [CrossRef]
- Olszewska-Pazdrak, B.; Casola, A.; Saito, T.; Alam, R.; Crowe, S.E.; Mei, F.; Ogra, P.L.; Garofalo, R.P. Cell-Specific Expression of RANTES, MCP-1, and MIP-1alpha by Lower Airway Epithelial Cells and Eosinophils Infected with Respiratory Syncytial Virus. J. Virol. 1998, 72, 4756–4764. [Google Scholar] [CrossRef] [PubMed]
- Martin, L.; Blanpain, C.; Garnier, P.; Wittamer, V.; Parmentier, M.; Vita, C. Structural and Functional Analysis of the RANTES-Glycosaminoglycans Interactions. Biochemistry 2001, 40, 6303–6318. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Jiang, L.; Li, X.; Lin, F.; Wang, Y.; Li, B.; Jiang, T.; An, W.; Liu, S.; Liu, H.; et al. Clinical and Pathological Investigation of Patients with Severe COVID-19. JCI Insight 2020, 5, e138070. [Google Scholar] [CrossRef]
- Patterson, B.K.; Seethamraju, H.; Dhody, K.; Corley, M.J.; Kazempour, K.; Lalezari, J.P.; Pang, A.P.; Sugai, C.; Francisco, E.B.; Pise, A.; et al. Disruption of the CCL5/RANTES-CCR5 Pathway Restores Immune Homeostasis and Reduces Plasma Viral Load in Critical COVID-19. medRxiv 2020. [Google Scholar] [CrossRef]
- Morrell, C.N.; Sun, H.; Ikeda, M.; Beique, J.-C.; Swaim, A.M.; Mason, E.; Martin, T.V.; Thompson, L.E.; Gozen, O.; Ampagoomian, D.; et al. Glutamate Mediates Platelet Activation through the AMPA Receptor. J. Exp. Med. 2008, 205, 575–584. [Google Scholar] [CrossRef]
- Curi, R.; Lagranha, C.J.; Doi, S.Q.; Sellitti, D.F.; Procopio, J.; Pithon-Curi, T.C.; Corless, M.; Newsholme, P. Molecular Mechanisms of Glutamine Action. J. Cell Physiol. 2005, 204, 392–401. [Google Scholar] [CrossRef] [PubMed]
- Mallolas, J.; Hurtado, O.; Castellanos, M.; Blanco, M.; Sobrino, T.; Serena, J.; Vivancos, J.; Castillo, J.; Lizasoain, I.; Moro, M.A.; et al. A Polymorphism in the EAAT2 Promoter Is Associated with Higher Glutamate Concentrations and Higher Frequency of Progressing Stroke. J. Exp. Med. 2006, 203, 711–717. [Google Scholar] [CrossRef]
- Ferrarese, C.; Sala, G.; Riva, R.; Begni, B.; Zoia, C.; Tremolizzo, L.; Galimberti, G.; Millul, A.; Bastone, A.; Mennini, T.; et al. Decreased Platelet Glutamate Uptake in Patients with Amyotrophic Lateral Sclerosis. Neurology 2001, 56, 270–272. [Google Scholar] [CrossRef]
- Zhu, Y.; Li, T.; Ramos da Silva, S.; Lee, J.-J.; Lu, C.; Eoh, H.; Jung, J.U.; Gao, S.-J. A Critical Role of Glutamine and Asparagine γ-Nitrogen in Nucleotide Biosynthesis in Cancer Cells Hijacked by an Oncogenic Virus. mBio 2017, 8, e01179-17. [Google Scholar] [CrossRef]
- Vastag, L.; Koyuncu, E.; Grady, S.L.; Shenk, T.E.; Rabinowitz, J.D. Divergent Effects of Human Cytomegalovirus and Herpes Simplex Virus-1 on Cellular Metabolism. PLoS Pathog. 2011, 7, e1002124. [Google Scholar] [CrossRef]
- Li, X.-K.; Tu, B.; Zhang, X.-A.; Xu, W.; Chen, J.-H.; Zhao, G.-Y.; Xu, B.; Zheng, J.-J.; Yan, Y.-F.; Hao, P.-F.; et al. Dysregulation of Glutamine/Glutamate Metabolism in COVID-19 Patients: A Metabolism Study in African Population and Mini Meta-Analysis. J. Med. Virol. 2023, 95, e28150. [Google Scholar] [CrossRef] [PubMed]
- Páez-Franco, J.C.; Torres-Ruiz, J.; Sosa-Hernández, V.A.; Cervantes-Díaz, R.; Romero-Ramírez, S.; Pérez-Fragoso, A.; Meza-Sánchez, D.E.; Germán-Acacio, J.M.; Maravillas-Montero, J.L.; Mejía-Domínguez, N.R.; et al. Metabolomics Analysis Reveals a Modified Amino Acid Metabolism That Correlates with Altered Oxygen Homeostasis in COVID-19 Patients. Sci. Rep. 2021, 11, 6350. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Yang, G.; Wang, X.; Wen, Z.; Shuai, L.; Luo, J.; Wang, C.; Sun, Z.; Liu, R.; Ge, J.; et al. SARS-CoV-2 Uses Metabotropic Glutamate Receptor Subtype 2 as an Internalization Factor to Infect Cells. Cell Discov. 2021, 7, 119. [Google Scholar] [CrossRef] [PubMed]
- Eteraf-Oskouei, T.; Najafi, M. The Relationship between the Serotonergic System and COVID-19 Disease: A Review. Heliyon 2022, 8, e09544. [Google Scholar] [CrossRef]
- Adnot, S.; Houssaini, A.; Abid, S.; Marcos, E.; Amsellem, V. Serotonin Transporter and Serotonin Receptors. Handb. Exp. Pharmacol. 2013, 218, 365–380. [Google Scholar] [CrossRef]
- O’Connell, P.J.; Wang, X.; Leon-Ponte, M.; Griffiths, C.; Pingle, S.C.; Ahern, G.P. A Novel Form of Immune Signaling Revealed by Transmission of the Inflammatory Mediator Serotonin between Dendritic Cells and T Cells. Blood 2006, 107, 1010–1017. [Google Scholar] [CrossRef]
- León-Ponte, M.; Ahern, G.P.; O’Connell, P.J. Serotonin Provides an Accessory Signal to Enhance T-Cell Activation by Signaling through the 5-HT7 Receptor. Blood 2007, 109, 3139–3146. [Google Scholar] [CrossRef]
- Mikulski, Z.; Zaslona, Z.; Cakarova, L.; Hartmann, P.; Wilhelm, J.; Tecott, L.H.; Lohmeyer, J.; Kummer, W. Serotonin Activates Murine Alveolar Macrophages through 5-HT2C Receptors. Am. J. Physiol. Lung Cell Mol. Physiol. 2010, 299, L272–L280. [Google Scholar] [CrossRef]
- Cloutier, N.; Allaeys, I.; Marcoux, G.; Machlus, K.R.; Mailhot, B.; Zufferey, A.; Levesque, T.; Becker, Y.; Tessandier, N.; Melki, I.; et al. Platelets Release Pathogenic Serotonin and Return to Circulation after Immune Complex-Mediated Sequestration. Proc. Natl. Acad. Sci. USA 2018, 115, E1550–E1559. [Google Scholar] [CrossRef]
- Kumar, D.; Jahan, S.; Khan, A.; Siddiqui, A.J.; Redhu, N.S.; Wahajuddin; Khan, J.; Banwas, S.; Alshehri, B.; Alaidarous, M. Neurological Manifestation of SARS-CoV-2 Induced Inflammation and Possible Therapeutic Strategies Against COVID-19. Mol. Neurobiol. 2021, 58, 3417–3434. [Google Scholar] [CrossRef]
- Attademo, L.; Bernardini, F. Are Dopamine and Serotonin Involved in COVID-19 Pathophysiology? Eur. J. Psychiatry 2021, 35, 62–63. [Google Scholar] [CrossRef] [PubMed]
- Keith, P.; Saint-Jour, M.; Pusey, F.; Hodges, J.; Jalali, F.; Scott, L.K. Unprovoked Serotonin Syndrome-like Presentation of SARS-CoV-2 Infection: A Small Case Series. SAGE Open Med. Case Rep. 2021, 9, 2050313X211032089. [Google Scholar] [CrossRef] [PubMed]
- Zaid, Y.; Puhm, F.; Allaeys, I.; Naya, A.; Oudghiri, M.; Khalki, L.; Limami, Y.; Zaid, N.; Sadki, K.; Ben El Haj, R.; et al. Platelets Can Associate with SARS-Cov-2 RNA and Are Hyperactivated in COVID-19. Circ. Res. 2020, 127, 1404–1418. [Google Scholar] [CrossRef] [PubMed]
- Duerschmied, D.; Suidan, G.L.; Demers, M.; Herr, N.; Carbo, C.; Brill, A.; Cifuni, S.M.; Mauler, M.; Cicko, S.; Bader, M.; et al. Platelet Serotonin Promotes the Recruitment of Neutrophils to Sites of Acute Inflammation in Mice. Blood 2013, 121, 1008–1015. [Google Scholar] [CrossRef] [PubMed]
- Ishikura, H.; Irie, Y.; Kawamura, M.; Hoshino, K.; Nakamura, Y.; Mizunuma, M.; Maruyama, J.; Nakashio, M.; Suzuki-Inoue, K.; Kitamura, T. Early Recognition of Sepsis-Induced Coagulopathy Using the C2PAC Index: A Ratio of Soluble Type C Lectin-like Receptor 2 (SCLEC-2) Level and Platelet Count. Platelets 2022, 33, 935–944. [Google Scholar] [CrossRef]
- Suzuki-Inoue, K.; Tsukiji, N.; Shirai, T.; Osada, M.; Inoue, O.; Ozaki, Y. Platelet CLEC-2: Roles Beyond Hemostasis. Semin. Thromb. Hemost. 2018, 44, 126–134. [Google Scholar] [CrossRef]
- Navarro-Núñez, L.; Langan, S.A.; Nash, G.B.; Watson, S.P. The Physiological and Pathophysiological Roles of Platelet CLEC-2. Thromb. Haemost. 2013, 109, 991–998. [Google Scholar] [CrossRef]
- Meng, D.; Luo, M.; Liu, B. The Role of CLEC-2 and Its Ligands in Thromboinflammation. Front. Immunol. 2021, 12, 688643. [Google Scholar] [CrossRef]
- Suzuki-Inoue, K.; Fuller, G.L.J.; García, Á.; Eble, J.A.; Pöhlmann, S.; Inoue, O.; Gartner, T.K.; Hughan, S.C.; Pearce, A.C.; Laing, G.D.; et al. A Novel Syk-Dependent Mechanism of Platelet Activation by the C-Type Lectin Receptor CLEC-2. Blood 2006, 107, 542–549. [Google Scholar] [CrossRef] [PubMed]
- Yamashita, Y.; Suzuki, K.; Mastumoto, T.; Ikejiri, M.; Ohishi, K.; Katayama, N.; Suzuki-Inoue, K.; Wada, H. Elevated Plasma Levels of Soluble C-Type Lectin-like Receptor 2 (CLEC2) in Patients with Thrombotic Microangiopathy. Thromb. Res. 2019, 178, 54–58. [Google Scholar] [CrossRef] [PubMed]
- Inoue, O.; Osada, M.; Nakamura, J.; Kazama, F.; Shirai, T.; Tsukiji, N.; Sasaki, T.; Yokomichi, H.; Dohi, T.; Kaneko, M.; et al. Soluble CLEC-2 Is Generated Independently of ADAM10 and Is Increased in Plasma in Acute Coronary Syndrome: Comparison with Soluble GPVI. Int. J. Hematol. 2019, 110, 285–294. [Google Scholar] [CrossRef] [PubMed]
- Fei, M.; Xiang, L.; Chai, X.; Jin, J.; You, T.; Zhao, Y.; Ruan, C.; Hao, Y.; Zhu, L. Plasma Soluble C-Type Lectin-like Receptor-2 Is Associated with the Risk of Coronary Artery Disease. Front. Med. 2020, 14, 81–90. [Google Scholar] [CrossRef]
- Zhang, X.; Zhang, W.; Wu, X.; Li, H.; Zhang, C.; Huang, Z.; Shi, R.; You, T.; Shi, J.; Cao, Y. Prognostic Significance of Plasma CLEC-2 (C-Type Lectin-Like Receptor 2) in Patients With Acute Ischemic Stroke. Stroke 2019, 50, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Nishigaki, A.; Ichikawa, Y.; Ezaki, M.; Yamamoto, A.; Suzuki, K.; Tachibana, K.; Kamon, T.; Horie, S.; Masuda, J.; Makino, K.; et al. Soluble C-Type Lectin-Like Receptor 2 Elevation in Patients with Acute Cerebral Infarction. J. Clin. Med. 2021, 10, 3408. [Google Scholar] [CrossRef] [PubMed]
- Guo, M.; Zhang, H.; Lv, Q.-W.; Huang, H.-B.; Shen, L.-J. Higher Plasma C-Type Lectin-like Receptor 2 Concentrations for Prediction of Higher Risk of 30-Day Mortality in Isolated Severe Blunt Traumatic Brain Injury. Clin. Chim. Acta 2019, 496, 1–6. [Google Scholar] [CrossRef]
- Yamamoto, A.; Wada, H.; Ichkawa, Y.; Tanaka, M.; Tashiro, H.; Shiraki, K.; Shimpo, H.; Yamashita, Y.; Mastumoto, T.; Shimaoka, M.; et al. Soluble C-Type Lectin-Like Receptor 2 Is a Biomarker for Disseminated Intravascular Coagulation. J. Clin. Med. 2021, 10, 2860. [Google Scholar] [CrossRef]
- Wada, H.; Ichikawa, Y.; Ezaki, M.; Yamamoto, A.; Tomida, M.; Yoshida, M.; Fukui, S.; Moritani, I.; Shiraki, K.; Shimaoka, M.; et al. Elevated Plasma Soluble C-Type Lectin-like Receptor 2 Is Associated with the Worsening of Coronavirus Disease 2019. J. Clin. Med. 2022, 11, 985. [Google Scholar] [CrossRef]
- Garnier, Y.; Claude, L.; Hermand, P.; Sachou, E.; Claes, A.; Desplan, K.; Chahim, B.; Roger, P.-M.; Martino, F.; Colin, Y.; et al. Plasma Microparticles of Intubated COVID-19 Patients Cause Endothelial Cell Death, Neutrophil Adhesion and Netosis, in a Phosphatidylserine-Dependent Manner. Br. J. Haematol. 2022, 196, 1159–1169. [Google Scholar] [CrossRef]
- Nomura, S.; Shimizu, M. Clinical Significance of Procoagulant Microparticles. J. Intensive Care 2015, 3, 2. [Google Scholar] [CrossRef]
- Nieri, D.; Neri, T.; Petrini, S.; Vagaggini, B.; Paggiaro, P.; Celi, A. Cell-Derived Microparticles and the Lung. Eur. Respir. Rev. 2016, 25, 266–277. [Google Scholar] [CrossRef] [PubMed]
- Morel, O.; Morel, N.; Freyssinet, J.-M.; Toti, F. Platelet Microparticles and Vascular Cells Interactions: A Checkpoint between the Haemostatic and Thrombotic Responses. Platelets 2008, 19, 9–23. [Google Scholar] [CrossRef] [PubMed]
- Théry, C.; Ostrowski, M.; Segura, E. Membrane Vesicles as Conveyors of Immune Responses. Nat. Rev. Immunol. 2009, 9, 581–593. [Google Scholar] [CrossRef]
- Hugel, B.; Martínez, M.C.; Kunzelmann, C.; Freyssinet, J.-M. Membrane Microparticles: Two Sides of the Coin. Physiology 2005, 20, 22–27. [Google Scholar] [CrossRef]
- Morel, O.; Toti, F.; Hugel, B.; Bakouboula, B.; Camoin-Jau, L.; Dignat-George, F.; Freyssinet, J.-M. Procoagulant Microparticles: Disrupting the Vascular Homeostasis Equation? Arterioscler. Thromb. Vasc. Biol. 2006, 26, 2594–2604. [Google Scholar] [CrossRef]
- Owens, A.P.; Mackman, N. Microparticles in Hemostasis and Thrombosis. Circ. Res. 2011, 108, 1284–1297. [Google Scholar] [CrossRef] [PubMed]
- Thachil, J.; Tang, N.; Gando, S.; Falanga, A.; Cattaneo, M.; Levi, M.; Clark, C.; Iba, T. ISTH Interim Guidance on Recognition and Management of Coagulopathy in COVID-19. J. Thromb. Haemost. 2020, 18, 1023–1026. [Google Scholar] [CrossRef]
- Kaur, S.; Singh, A.; Kaur, J.; Verma, N.; Pandey, A.K.; Das, S.; Bhattacharyya, S.; Guchhait, P. Upregulation of Cytokine Signalling in Platelets Increases Risk of Thrombophilia in Severe COVID-19 Patients. Blood Cells Mol. Dis. 2022, 94, 102653. [Google Scholar] [CrossRef]
- Morel, O.; Marchandot, B.; Jesel, L.; Sattler, L.; Trimaille, A.; Curtiaud, A.; Ohana, M.; Fafi-Kremer, S.; Schini-Kerth, V.; Grunebaum, L.; et al. Microparticles in COVID-19 as a Link between Lung Injury Extension and Thrombosis. ERJ Open Res. 2021, 7, 00954–02020. [Google Scholar] [CrossRef]
- Rausch, L.; Lutz, K.; Schifferer, M.; Winheim, E.; Gruber, R.; Oesterhaus, E.F.; Rinke, L.; Hellmuth, J.C.; Scherer, C.; Muenchhoff, M.; et al. Binding of Phosphatidylserine-Positive Microparticles by PBMCs Classifies Disease Severity in COVID-19 Patients. J. Extracell. Vesicles 2021, 10, e12173. [Google Scholar] [CrossRef]
- Barnes, G.D.; Burnett, A.; Allen, A.; Ansell, J.; Blumenstein, M.; Clark, N.P.; Crowther, M.; Dager, W.E.; Deitelzweig, S.B.; Ellsworth, S.; et al. Thromboembolic Prevention and Anticoagulant Therapy during the COVID-19 Pandemic: Updated Clinical Guidance from the Anticoagulation Forum. J. Thromb. Thrombolysis 2022, 54, 197–210. [Google Scholar] [CrossRef] [PubMed]
- Kyriakoulis, K.G.; Kollias, A.; Kyriakoulis, I.G.; Kyprianou, I.A.; Papachrysostomou, C.; Makaronis, P.; Kotronias, R.A.; Terentes-Printzios, D.; Toskas, I.; Mikhailidis, D.P. Thromboprophylaxis in Patients with COVID-19: Systematic Review of National and International Clinical Guidance Reports. Curr. Vasc. Pharmacol. 2022, 20, 96–110. [Google Scholar] [CrossRef]
- Schulman, S.; Sholzberg, M.; Spyropoulos, A.C.; Zarychanski, R.; Resnick, H.E.; Bradbury, C.A.; Broxmeyer, L.; Connors, J.M.; Falanga, A.; Iba, T.; et al. ISTH Guidelines for Antithrombotic Treatment in COVID-19. J. Thromb. Haemost. 2022, 20, 2214–2225. [Google Scholar] [CrossRef] [PubMed]
- Bohula, E.A.; Berg, D.D.; Lopes, M.S.; Connors, J.M.; Babar, I.; Barnett, C.F.; Chaudhry, S.-P.; Chopra, A.; Ginete, W.; Ieong, M.H.; et al. Anticoagulation and Antiplatelet Therapy for Prevention of Venous and Arterial Thrombotic Events in Critically Ill Patients With COVID-19: COVID-PACT. Circulation 2022, 146, 1344–1356. [Google Scholar] [CrossRef] [PubMed]
- Cuker, A.; Tseng, E.K.; Nieuwlaat, R.; Angchaisuksiri, P.; Blair, C.; Dane, K.; DeSancho, M.T.; Diuguid, D.; Griffin, D.O.; Kahn, S.R.; et al. American Society of Hematology Living Guidelines on the Use of Anticoagulation for Thromboprophylaxis in Patients with COVID-19: January 2022 Update on the Use of Therapeutic-Intensity Anticoagulation in Acutely Ill Patients. Blood Adv. 2022, 6, 4915–4923. [Google Scholar] [CrossRef]
- Kollias, A.; Kyriakoulis, K.G.; Trontzas, I.P.; Rapti, V.; Kyriakoulis, I.G.; Theochari, C.A.; Dimakakos, E.; Poulakou, G.; Syrigos, K. High versus Standard Intensity of Thromboprophylaxis in Hospitalized Patients with COVID-19: A Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 5549. [Google Scholar] [CrossRef]
- Mohseni Afshar, Z.; Tavakoli Pirzaman, A.; Hosseinzadeh, R.; Babazadeh, A.; Taghizadeh Moghadam, M.A.; Miri, S.R.; Sio, T.T.; Sullman, M.J.M.; Barary, M.; Ebrahimpour, S. Anticoagulant Therapy in COVID-19: A Narrative Review. Clin. Transl. Sci. 2023, 16, 1510–1525. [Google Scholar] [CrossRef]

| Molecule | Biological Function | Methods | Pro-Infection Mechanism | Clinical Complications | Ref. |
|---|---|---|---|---|---|
| P-Selectin | Platelet activation; adhesion and modulation of platelet–leukocyte interaction. | Flowcytometry | Increased surface expression. | Platelet–leukocyte aggregates; increased platelet aggregation, adhesion and spread. | [39,61,62,63] |
| VWF | Recruitment of circulating platelets to the site of injury; platelet activation and aggregation. | LIA, ELISA, immunohistology | Increased plasma levels in patients on ITU support. | Thrombosis; vasculopathy; greater severity and in-hospital mortality. | [64,65,66,67,68,69,70,71,72] |
| PAI-1 | Fibrinolytic regulation. | ELISA | Significantly higher levels in ITU patients. | Predisposition to thrombotic events; associated with worse respiratory status and unfavorable clinical outcome. | [73,74,75,76,77,78] |
| PF4 | Coagulation; regulating angiogenesis and inflammatory and infectious responses. | ELISA | High expression in plasma and tracheal aspirate. | Platelet hyperactivation associated with immunothrombosis and the formation of PF4/heparin immune complexes. | [39,79,80,81,82,83,84,85,86,87,88,89,90,91] |
| TGF-β | Inflammatory regulation; coagulation; wound healing. | ELISA | High serum levels are associated with greater disease severity. | Increased coagulation; immune dysregulation; pulmonary fibrosis. | [92,93,94,95,96,97] |
| PAF | Leukocyte chemotaxis; platelet aggregation; inflammatory mediator in infectious processes. | ELISA | Increased levels were described in patients with moderate COVID-19. | Increased inflammation; interstitial edema; immunothrombosis. | [98,99,100,101,102,103,104,105,106,107] |
| MMP-2, MMP-9 | Degradation of extracellular matrix proteins; embryonic development and fibrinolysis. | Zymography, ELISA | Elevated levels of MMP-2 and MMP-9 in severe COVID-19 patients. | Increased mortality; respiratory complications; neurological syndrome. | [108,109,110,111,112,113,114,115,116] |
| PDGF | Cell differentiation, proliferation and chemotaxis. | ELISA | High levels were associated with greater disease severity. | Platelet activation; formation of platelet–leukocyte aggregates; lung damage. | [4,39,117,118,119] |
| RANTES (CCL5) | Monocyte recruitment; activation and differentiation of T cells. | ELISA | Increased plasma levels and activity in critically ill patients. | Lung damage; NETs; immunothrombosis. | [85,120,121,122,123,124,125,126,127] |
| Glutamate | Regulation of platelet production and activation. | Chromatography, mass spectrometry | Lower glutamine levels and higher glutamate levels in severe COVID-19. | Lung damage; hypoxia; neurological disability; thrombosis risk. | [128,129,130,131,132,133,134,135,136] |
| Serotonin | Vasoconstriction; T cell activation and differentiation; platelet aggregation. | ELISA | High serum levels in severe COVID-19. | Serotonergic toxicity; platelet degranulation; vascular injury. | [137,138,139,140,141,142,143,144,145,146,147] |
| CLEC-2 | Hemostasis; healing; maintenance of vascular integrity; platelet adhesion. | CLEIA | Elevated plasma levels in severe and critical COVID-19. | Platelet activation; thrombotic syndrome. | [13,148,149,150,151,152,153,154,155,156,157,158,159,160] |
| MPs | Regulation of inflammation; coagulation; cell proliferation and differentiation. | Flowcytometry, ELISA | High levels of circulating MPs in ITU patients. | Lung injury; increase in plateletleukocyte aggregates; worse clinical outcome. | [161,162,163,164,165,166,167,168,169,170,171,172] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Oliveira Sales, L.; de Oliveira, L.L.B.; da Silva, J.B.S.; de Moraes Filho, M.O.; de Moraes, M.E.A.; Montenegro, R.C.; Moreira-Nunes, C.A. The Role of Platelet Molecules in Risk Stratification of Patients with COVID-19. Hemato 2023, 4, 364-383. https://doi.org/10.3390/hemato4040029
de Oliveira Sales L, de Oliveira LLB, da Silva JBS, de Moraes Filho MO, de Moraes MEA, Montenegro RC, Moreira-Nunes CA. The Role of Platelet Molecules in Risk Stratification of Patients with COVID-19. Hemato. 2023; 4(4):364-383. https://doi.org/10.3390/hemato4040029
Chicago/Turabian Stylede Oliveira Sales, Lívia, Lais Lacerda Brasil de Oliveira, Jean Breno Silveira da Silva, Manoel Odorico de Moraes Filho, Maria Elisabete Amaral de Moraes, Raquel Carvalho Montenegro, and Caroline Aquino Moreira-Nunes. 2023. "The Role of Platelet Molecules in Risk Stratification of Patients with COVID-19" Hemato 4, no. 4: 364-383. https://doi.org/10.3390/hemato4040029
APA Stylede Oliveira Sales, L., de Oliveira, L. L. B., da Silva, J. B. S., de Moraes Filho, M. O., de Moraes, M. E. A., Montenegro, R. C., & Moreira-Nunes, C. A. (2023). The Role of Platelet Molecules in Risk Stratification of Patients with COVID-19. Hemato, 4(4), 364-383. https://doi.org/10.3390/hemato4040029







