Predicting Artificial Intelligence Acceptance in Dental Treatments Among Patients in Saudi Arabia: A Perceived Risks and Benefits Perspective
Abstract
1. Introduction
2. Materials and Methods
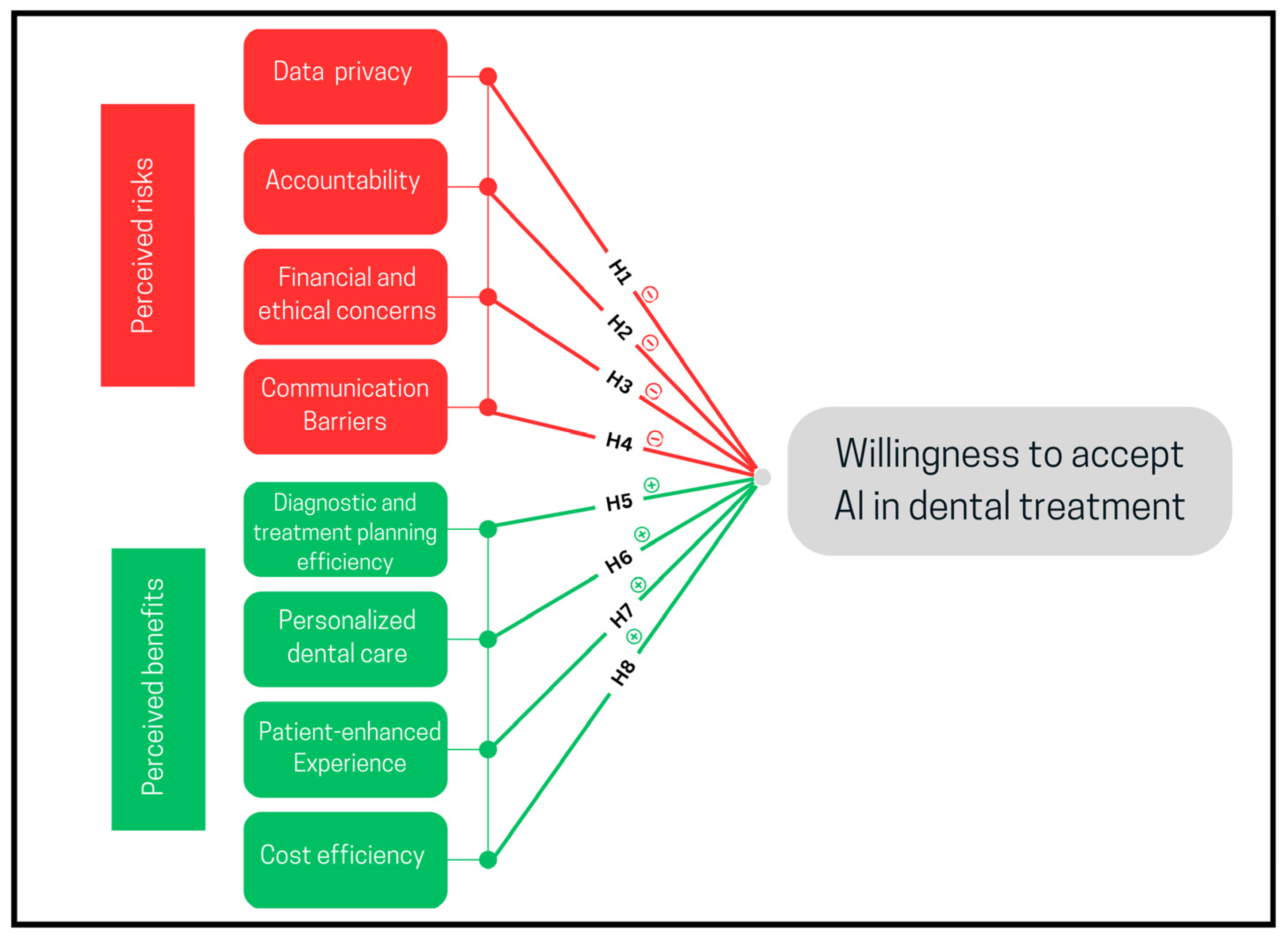
2.1. Research Model
2.1.1. Perceived Risks
Data Privacy
Accountability
Financial and Ethical Concerns
Communication Barriers
2.1.2. Perceived Benefits
Diagnostic and Treatment Planning Efficiency
Personalized Dental Care
Patient-Enhanced Experience
Cost Efficiency
2.2. Ethical Consideration
2.3. Study Setting and Subjects
2.4. Questionnaire Development and Procedure
2.5. Data Analysis
3. Results
3.1. Subjects Characteristics
3.2. Descriptive and Reliability Statistics
3.3. Testing of Assumptions
3.4. Hypothesis Testing
4. Discussion
Limitations and Future Research Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AI | Artificial Intelligence |
| CNN | Convolutional Neural Networks |
| VIF | Variance Inflation Factor |
References
- Secinaro, S.; Calandra, D.; Secinaro, A.; Muthurangu, V.; Biancone, P. The role of artificial intelligence in healthcare: A structured literature review. BMC Med. Inform. Decis. Mak. 2021, 21, 125. [Google Scholar] [CrossRef] [PubMed]
- Lekadir, K.; Frangi, A.F.; Porras, A.R.; Glocker, B.; Cintas, C.; Langlotz, C.P.; Starmans, M.P. FUTURE-AI: International consensus guideline for trustworthy and deployable artificial intelligence in healthcare. BMJ 2025, 388, 59–63. [Google Scholar] [CrossRef] [PubMed]
- Këpuska, V.; Bohouta, G. Next-generation of virtual personal assistants (Microsoft Cortana, Apple Siri, Amazon Alexa and Google Home). In Proceedings of the 2018 IEEE 8th Annual Computing and Communication Workshop and Conference (CCWC), Las Vegas, NV, USA, 8–10 January 2018; pp. 99–103. [Google Scholar]
- Kulkarni, M.M.D. Applications and Impact of Artificial intelligence in manufacturing: A review. IRJET 2024, 11, 59–63. [Google Scholar]
- Chemnad, K.; Othman, A. Digital accessibility in the era of artificial intelligence—Bibliometric analysis and systematic review. Front. Artif. Intell. 2024, 7, 1349668. [Google Scholar] [CrossRef]
- Santamato, V.; Tricase, C.; Faccilongo, N.; Iacoviello, M.; Marengo, A. Exploring the Impact of Artificial Intelligence on Healthcare Management: A Combined Systematic Review and Machine-Learning Approach. Appl. Sci. 2024, 14, 10144. [Google Scholar] [CrossRef]
- Semerci, Z.M.; Yardımcı, S. Empowering Modern Dentistry: The Impact of Artificial Intelligence on Patient Care and Clinical Decision Making. Diagnostics 2024, 14, 1260. [Google Scholar] [CrossRef]
- Ding, H.; Wu, J.; Zhao, W.; Matinlinna, J.P.; Burrow, M.F.; Tsoi, J.K.H. Artificial intelligence in dentistry—A review. Front. Dent. Med. 2023, 4, 1085251. [Google Scholar] [CrossRef]
- Sharka, R.; Sedayo, L.; Morad, M.; Abuljadayel, J. Measuring the impact of dental service quality on revisit intention using an extended SERVQUAL model. Front. Oral. Health. 2024, 5, 1362659. [Google Scholar] [CrossRef]
- Alotaibi, G.; Awawdeh, M.; Farook, F.F.; Aljohani, M.; Aldhafiri, R.M.; Aldhoayan, M. Artificial intelligence (AI) diagnostic tools: Utilizing a convolutional neural network (CNN) to assess periodontal bone level radiographically—A retrospective study. BMC Oral Health 2022, 22, 399. [Google Scholar] [CrossRef]
- Lai, G.; Dunlap, C.; Gluskin, A.; Nehme, W.B.; Azim, A.A. Artificial Intelligence in Endodontics. J. Calif. Dent. Assoc. 2023, 51, 2199933. [Google Scholar] [CrossRef]
- Kühnisch, J.; Meyer, O.; Hesenius, M.; Hickel, R.; Gruhn, V. Caries Detection on Intraoral Images Using Artificial Intelligence. J. Dent. Res. 2022, 101, 158–165. [Google Scholar] [CrossRef]
- Al-Dabbagh, N.; Alnowailaty, Y.; Abed, H.; Sharka, R.; Alhilou, A.; Almarghlani, A. Patients’ Perception of using Robotics and Artificial Intelligence in Dentistry: A Cross-sectional Study. Open Dent. J. 2024, 18, e18742106339605. [Google Scholar] [CrossRef]
- Thorat, V.; Rao, P.; Joshi, N.; Talreja, P.; Shetty, A.R. Role of Artificial Intelligence (AI) in Patient Education and Communication in Dentistry. Cureus 2024, 16, e59799. [Google Scholar] [CrossRef]
- Ayad, N.; Schwendicke, F.; Krois, J.; van den Bosch, S.; Bergé, S.; Bohner, L.; Vinayahalingam, S. Patients’ perspectives on the use of artificial intelligence in dentistry: A regional survey. Head. Face Med. 2023, 19, 23. [Google Scholar] [CrossRef]
- Khalid, N.; Qayyum, A.; Bilal, M.; Al-Fuqaha, A.; Qadir, J. Privacy-preserving artificial intelligence in healthcare: Techniques and applications. Comput. Biol. Med. 2023, 158, 106848. [Google Scholar] [CrossRef]
- Chustecki, M. Benefits and Risks of AI in Health Care: Narrative Review. Interact. J. Med. Res. 2024, 13, e53616. [Google Scholar] [CrossRef]
- Murdoch, B. Privacy and artificial intelligence: Challenges for protecting health information in a new era. BMC Med. Ethics. 2021, 22, 122. [Google Scholar] [CrossRef]
- Williamson, S.M.; Prybutok, V. Balancing Privacy and Progress: A Review of Privacy Challenges, Systemic Oversight, and Patient Perceptions in AI-Driven Healthcare. Appl. Sci. 2024, 14, 675. [Google Scholar] [CrossRef]
- Schwendicke, F.; Samek, W.; Krois, J. Artificial Intelligence in Dentistry: Chances and Challenges. J. Dent. Res. 2020, 99, 769–774. [Google Scholar] [CrossRef]
- Ranjan, P.; Kumari, A.; Chakrawarty, A. How can Doctors Improve their Communication Skills? J. Clin. Diagn. Res. JCDR 2015, 9, JE01. [Google Scholar] [CrossRef]
- Nair, M.; Svedberg, P.; Larsson, I.; Nygren, J.M. A comprehensive overview of barriers and strategies for AI implementation in healthcare: Mixed-method design. PLoS ONE 2024, 19, e0305949. [Google Scholar] [CrossRef] [PubMed]
- Sun, G.; Zhou, Y.H. AI in healthcare: Navigating opportunities and challenges in digital communication. Front. Digit. Health 2023, 5, 1291132. [Google Scholar] [CrossRef]
- Rokaya, D.; Jaghsi, A.A.; Jagtap, R.; Srimaneepong, V. Artificial intelligence in dentistry and dental biomaterials. Front. Dent. Med. 2024, 5, 1525505. [Google Scholar] [CrossRef] [PubMed]
- Bapuji, R.; Devi, S.; Sangeeta Devi, M.; Priya, W. The Transformative Power of Artificial Intelligence in Dentistry. Int. J. Multidiscip. Res. 2023, 5, 1–6. [Google Scholar]
- Surdilovic, D.; Ille, T.; D’Souza, J. Artificial Intelligence and Dental Practice Management. Eur. J. Artif. Intell. Mach. Learn. 2022, 1, 11–14. [Google Scholar] [CrossRef]
- Knight, D.R.T.; Aakre, C.A.; Anstine, C.V.; Munipalli, B.; Biazar, P.; Mitri, G.; Dabrh, A.M.A. Artificial intelligence for patient scheduling in the real-world health care setting: A metanarrative review. Health Policy Technol. 2023, 12, 100824. [Google Scholar] [CrossRef]
- Valenzuela-Núñez, C.; Latorre-Núñez, G.; Troncoso-Espinosa, F. Smart Medical Appointment Scheduling: Optimization, Machine Learning, and Overbooking to Enhance Resource Utilization. IEEE Access 2024, 12, 7551–7562. [Google Scholar] [CrossRef]
- Singhal, S. Cost optimization and affordable health care using AI. Int. Mach. Learn. J. Comput. Eng. 2023, 6, 1–12. [Google Scholar]
- Hossain, S.; Ahmed, A.; Khadka, U.; Sarkar, S.; Khan, N. AI-driven Predictive Analytics, Healthcare Outcomes, Cost Reduction, Machine Learning, Patient Monitoring. Adv. Int. J. Multidiscip. Res. 2024, 2, 1–20. [Google Scholar]
- Esmaeilzadeh, P.; Mirzaei, T.; Dharanikota, S. Patients’ Perceptions Toward Human–Artificial Intelligence Interaction in Health Care: Experimental Study. J. Med. Internet Res. 2021, 23, e25856. [Google Scholar] [CrossRef]
- Zeb, S.; Fnu, N.; Abbasi, N.; Fahad, M. AI in Healthcare: Revolutionizing Diagnosis and Therapy. Int. J. Multidiscip. Sci. Arts 2024, 3, 118–128. [Google Scholar] [CrossRef]
- Fritsch, S.J.; Blankenheim, A.; Wahl, A.; Hetfeld, P.; Maassen, O.; Deffge, S.; Bickenbach, J. Attitudes and perception of artificial intelligence in healthcare: A cross-sectional survey among patients. Digit. Health 2022, 8, 20552076221116772. [Google Scholar] [CrossRef] [PubMed]
- Vayena, E.; Blasimme, A.; Cohen, I.G. Machine learning in medicine: Addressing ethical challenges. PLoS Med. 2018, 15, e1002689. [Google Scholar] [CrossRef]
- Kosan, E.; Krois, J.; Wingenfeld, K.; Deuter, C.E.; Gaudin, R.; Schwendicke, F. Patients’ Perspectives on Artificial Intelligence in Dentistry: A Controlled Study. J. Clin. Med. 2022, 11, 2143. [Google Scholar] [CrossRef] [PubMed]
- Hair, J.; Black, W.; Anderson, R.; Babin, B. Multivariate Data Analysis, 7th ed.; Edinburgh Gate Harlow, CM20 2JE; Pearson Education Limited: Essex, UK, 2014; p. 832. [Google Scholar]
- Field, A. Discovering Statistics Using IBM SPSS Statistics; SAGE Publications Ltd.: Thousand Oaks, CA, USA, 2017; p. 1104. [Google Scholar]
- Kolarkodi, S.H.; Alotaibi, K.Z. Artificial Intelligence in Diagnosis of Oral Diseases: A Systematic Review. J. Contemp. Dent. Pract. 2023, 24, 61–68. [Google Scholar] [CrossRef]
- Younus, D.A.; Aleem, D.A.; Waqar, D.Z.; Bokhari, D.S.; Islam, D.S.A.; Khan, D.N. Investigating the role of artificial intelligence in dental diagnostics and treatment planning—A comparative study. J. Popul. Ther. Clin. Pharmacol. 2024, 31, 2362–2372. [Google Scholar]
- Inani, H.; Mehta, V.; Bhavsar, D.; Gupta, R.K.; Jain, A.; Akhtar, Z. AI-enabled dental caries detection using transfer learning and gradient-based class activation mapping. J. Ambient. Intell. Humaniz. Comput. 2024, 15, 3009–3033. [Google Scholar] [CrossRef]
- Musri, N.; Christie, B.; Ichwan, S.J.A.; Cahyanto, A. Deep learning convolutional neural network algorithms for the early detection and diagnosis of dental caries on periapical radiographs: A systematic review. Imaging Sci. Dent. 2021, 51, 237–242. [Google Scholar] [CrossRef]
- Turosz, N.; Chęcińska, K.; Chęciński, M.; Sielski, M.; Sikora, M. Evaluation of Dental Panoramic Radiographs by Artificial Intelligence Compared to Human Reference: A Diagnostic Accuracy Study. J. Clin. Med. 2024, 13, 6859. [Google Scholar] [CrossRef]
- Pauwels, R. A brief introduction to concepts and applications of artificial intelligence in dental imaging. Oral. Radiol. 2021, 37, 153–160. [Google Scholar] [CrossRef]
- Li, P.; Kong, D.; Tang, T.; Su, D.; Yang, P.; Wang, H.; Liu, Y. Orthodontic Treatment Planning based on Artificial Neural Networks. Sci. Rep. 2019, 9, 2037. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.J.; Lee, S.J.; Yong, T.H.; Shin, N.Y.; Jang, B.G.; Kim, J.E.; Yi, W.J. Deep Learning Hybrid Method to Automatically Diagnose Periodontal Bone Loss and Stage Periodontitis. Sci. Rep. 2020, 10, 7531. [Google Scholar] [CrossRef] [PubMed]
- Sharka, R.; San Diego, J.; Nasseripour, M.; Banerjee, A. Factor analysis of risk perceptions of using digital and social media in dental education and profession. J. Dent. Educ. 2023, 87, 118–129. [Google Scholar] [CrossRef] [PubMed]
- Pandey, A.; Sureja, D.; Kaldate, S. The Implications of AI in Dentistry: Revolutionizing Patient Care and Clinical Precision. Mathews J. Dent. 2024, 8, 1–2. [Google Scholar] [CrossRef]
- Karimian, G.; Petelos, E.; Evers, S.M.A.A. The ethical issues of the application of artificial intelligence in healthcare: A systematic scoping review. AI Ethics 2022, 2, 539–551. [Google Scholar] [CrossRef]
| Dimensions | Items Label | Mean (SD) | Cronbach’s Alpha (α) |
|---|---|---|---|
| Data privacy | Confidentiality | 3.04 (1.13) | 0.73 |
| Misuse | 3.03 (1.12) | ||
| Privacy | 3.04 (1.13) | ||
| Average scores | 3.05 (2.72) | ||
| Accountability | Incorrect diagnoses | 3.19 (1.04) | 0.71 |
| Trust AI recommendations | 3.08 (1.04) | ||
| AI reliability | 3.07 (1.04) | ||
| Responsibility for AI errors | 3.68 (1.1) | ||
| Average scores | 3.19 (1.04) | ||
| Financial and ethical concerns | High cost | 3.51 (1.11) | 0.60 |
| Inequitable access | 2.97 (1.07) | ||
| Ethical issues | 2.94 (1.05) | ||
| Average scores | 3.14 (2.38) | ||
| Communication barriers | Personal interaction | 3.46 (1.09) | 0.60 |
| Preference for human treatment | 3.36 (1.09) | ||
| Communication difficulty | 3.7 (1.11) | ||
| Average scores | 3.51 (2.41) | ||
| Diagnostic and treatment planning efficiency | AI-Assisted treatment planning | 3.96 (0.91) | 0.75 |
| Early Detection | 3.89 (0.91) | ||
| Reduction of human errors | 3.65 (0.96) | ||
| Average scores | 3.84 (2.280) | ||
| Personalized dental care | Access to advanced treatments | 3.86 (0.91) | 0.77 |
| Innovative treatment options | 3.82 (0.92) | ||
| Personalized dental care | 3.70 (0.94) | ||
| Average scores | 3.79 (2.30) | ||
| Patient-enhanced experience | Confidence in treatment | 3.48 (1.02) | 0.79 |
| Better health outcomes | 3.63 (0.93) | ||
| Improved experience | 3.73 (0.91) | ||
| Average scores | 3.61 (2.41) | ||
| Cost efficiency | Cost reduction | 3.28 (1.08) | 0.70 |
| Informed decision-making | 3.86 (0.90) | ||
| Consistency and reliability | 3.56 (0.9 | ||
| Average scores | 3.57 (2.33) | ||
| Willingness to accept AI in dental treatment | Acceptance of AI technology | 3.60 (1.03) | 0.91 |
| Acceptance of AI diagnosis | 3.56 (0.99) | ||
| Acceptance of AI treatment plans | 3.59 (1.00) | ||
| Average scores | 3.59 (2.81) |
| Model | R | R Square | Adjusted R Square | Std. Error of the Estimate | Change Statistics | ||||
|---|---|---|---|---|---|---|---|---|---|
| R Square Change | F Change | df1 | df2 | Sig. F Change | |||||
| 1 | 0.081 | 0.007 | 0.001 | 0.934 | 0.007 | 1.107 | 3 | 507 | 0.346 |
| 2 | 0.821 | 0.673 | 0.666 | 0.540 | 0.667 | 127.270 | 8 | 499 | <0.001 |
| Predictor Variables | Unstandardized Coefficients | Standardized Coefficients | t | p-Value | Collinearity Statistics | ||
|---|---|---|---|---|---|---|---|
| B | Std. Error | β | Tolerance | VIF | |||
| Model 1 | |||||||
| (Constant) | 3.696 | 0.095 | 39.012 | <0.001 | |||
| Gender | −0.164 | 0.091 | −0.088 | −1.794 | 0.073 | 0.822 | 1.216 |
| Age | −0.048 | 0.092 | −0.026 | −0.530 | 0.597 | 0.827 | 1.210 |
| Education level | 0.012 | 0.149 | 0.003 | 0.077 | 0.938 | 0.993 | 1.007 |
| Model 2 | |||||||
| (Constant) | 0.093 | 0.200 | 0.463 | 0.644 | |||
| Gender | 0.048 | 0.054 | 0.026 | 0.889 | 0.374 | 0.796 | 1.256 |
| Age | −0.022 | 0.054 | −0.012 | −0.402 | 0.688 | 0.792 | 1.263 |
| Education level | −0.138 | 0.087 | −0.041 | −1.584 | 0.114 | 0.978 | 1.023 |
| Data privacy concerns | −0.046 | 0.038 | −0.044 | −1.211 | 0.226 | 0.491 | 2.038 |
| Accountability Concerns | −0.007 | 0.048 | −0.006 | −0.145 | 0.885 | 0.434 | 2.302 |
| Communication barriers | −0.030 | 0.038 | −0.026 | −0.790 | 0.430 | 0.605 | 1.652 |
| Financial and ethical concerns | −0.045 | 0.042 | −0.038 | −1.063 | 0.288 | 0.512 | 1.952 |
| Diagnostic and treatment planning efficiency | 0.060 | 0.058 | 0.049 | 1.024 | 0.306 | 0.291 | 3.436 |
| Personalized dental care | 0.271 | 0.050 | 0.222 | 5.375 | <0.001 | 0.383 | 2.610 |
| Patient enhanced experience | 0.548 | 0.050 | 0.471 | 10.951 | <0.001 | 0.354 | 2.824 |
| Cost efficiency | 0.184 | 0.051 | 0.153 | 3.606 | <0.001 | 0.363 | 2.754 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sharka, R.; Skatawi, B.; Sayyam, G.; Abutaleb, M.; Alshareef, M.; Alamar, M.; Abualkhair, L.; Ezzat, Y. Predicting Artificial Intelligence Acceptance in Dental Treatments Among Patients in Saudi Arabia: A Perceived Risks and Benefits Perspective. Oral 2025, 5, 28. https://doi.org/10.3390/oral5020028
Sharka R, Skatawi B, Sayyam G, Abutaleb M, Alshareef M, Alamar M, Abualkhair L, Ezzat Y. Predicting Artificial Intelligence Acceptance in Dental Treatments Among Patients in Saudi Arabia: A Perceived Risks and Benefits Perspective. Oral. 2025; 5(2):28. https://doi.org/10.3390/oral5020028
Chicago/Turabian StyleSharka, Rayan, Bayan Skatawi, Ghaday Sayyam, Maya Abutaleb, Mawadah Alshareef, Mohammed Alamar, Lujain Abualkhair, and Yousef Ezzat. 2025. "Predicting Artificial Intelligence Acceptance in Dental Treatments Among Patients in Saudi Arabia: A Perceived Risks and Benefits Perspective" Oral 5, no. 2: 28. https://doi.org/10.3390/oral5020028
APA StyleSharka, R., Skatawi, B., Sayyam, G., Abutaleb, M., Alshareef, M., Alamar, M., Abualkhair, L., & Ezzat, Y. (2025). Predicting Artificial Intelligence Acceptance in Dental Treatments Among Patients in Saudi Arabia: A Perceived Risks and Benefits Perspective. Oral, 5(2), 28. https://doi.org/10.3390/oral5020028







