Abstract
Aim: Class II Division I malocclusion poses significant challenges in orthodontics. The combination of a Herbst appliance and miniscrew anchorage emerged as a practical solution to improve skeletal and dental outcomes. This study employed finite element analysis to evaluate the biomechanical effects of a miniscrew-supported Herbst appliance on mandibular advancement and dentition movement. Methods: High-definition CBCT scans captured the maxilla and mandible’s detailed dental anatomy. The scans were stored in DICOM format for seamless integration with Mimics software (Mimics Innovation Suite research version 21.0, Materialise NV, Leuven, Belgium) for 3D reconstruction and model refinement. The appliance, designed with a maxillary fixed palatal arch and mandibular acrylic splint connected by telescoping rods, incorporated titanium TADs and elastic chains. STL models were optimized in Geomagic x Design for finite element analysis in Abaqus, assigning validated mechanical properties for materials. Tetrahedral meshing and realistic boundary conditions simulated biomechanical interactions. Tetrahedral C3D4 elements were used for meshing, ensuring a balance between computational efficiency and detailed anatomical representation. Tetrahedral meshing and realistic boundary conditions simulated biomechanical interactions. Dynamic simulations in CATIA evaluated mandibular movement. FEA analyzed displacement across dentoalveolar structures along the X, Y, and Z axes to assess treatment efficacy and biomechanical stability. Results: The Z displacement analysis revealed that the incisal edges of the lower central, lateral, and canines shifted lingually by 0.41, 0.4, and 0.47 mm, respectively. Additionally, the apices of the lower central, lateral, and canines displaced backwards by 0.05 mm, 0.05 mm, and 0.07 mm, respectively. Conclusions: The appliance facilitated mandibular advancement, bodily retracted the lower incisors, well-controlled the upper ones, and mesial-tipped the upper posterior teeth. In contrast with traditional functional appliances, it caused the lower anterior teeth to move backwards, while skeletal anchorage overcame some shortcomings of nonsurgical treatments. This method might be a good treatment option for growing skeletal Class II patients.
1. Introduction
Class II Division I malocclusion management presents persistent challenges within orthodontics, often necessitating innovative solutions to achieve optimal outcomes [1]. Many therapeutic appliances are available for treating patients with Class II malocclusion [2]. Removable functional appliances (such as Twin Block, Frankel, Activator, and myofunctional appliances) and fixed functional appliances (such as multibracket appliances combined with elastics, Carriere Motion, Forsus, and the Mandibular Anterior Repositioning Appliance (MARA)) are aimed at correcting the intermaxillary relationship and the overjet [3,4,5,6]. Fixed functional devices include Herbst appliances, which are noncompliance appliances used for the correction of skeletal Class II malocclusions, first proposed by Emily Herbst and developed by Hans Pancherz [7,8].
This device determines both skeletal and dental effects, including forward displacement of the mandible, reduction in sagittal growth of the maxilla, forward displacement of the mandibular arch, and distalization of the upper maxillary arch [8].
While skeletal results are favorable, dental effects such as palatal tipping of upper incisors and labial flaring of lower ones, as well as uncontrolled movement of posterior teeth, could reduce the mandibular growth response due to an excessive reduction in the overjet [9]. Therefore, several modifications of the original design have been proposed.
The MTH (Manni Telescopic Herbst) appliance (American Orthodontics, Sheboygan, WI) is particularly characterized by the presence of a lower acrylic splint, which prevents the flaring of the lower incisors [10]. To prevent anchorage loss, some studies proposed to combine Temporary Anchorage Devices (TADs) with functional appliances, reducing unwanted dental effects [11,12,13].
In the orthodontics field, finite element analysis (FEA) was widely used for evaluating the stress and deformation of complex structures. It is a useful tool for predicting tissue responses through the observation of areas of stress created by force systems. This non-invasive and accurate method provides detailed data on the physiological reactions potentially occurring in tissues. In the specific case, finite element analysis can be suitable for evaluating the effects of combining functional appliances and miniscrews to increase control in orthodontic treatments [14].
It is known that miniscrews provide a stable anchorage system that enhances biomechanical improvements in tooth and skeletal movement and ensures more predictable outcomes in complex orthodontic cases [15]. In this context, FEA plays a crucial role, offering detailed simulations of the mechanical interactions between the appliance, the screws, and the craniofacial structure, thus informing safer and more effective treatment plans [16]. Some studies have highlighted the potential of using FEA to evaluate orthodontic devices’ material properties and biomechanical performance under various loading conditions. These analyses aid in understanding the distribution of stresses and strains that affect the appliance and the surrounding biological structures, ensuring that the devices are both practical and minimally invasive [17,18].
Despite promising clinical results [10,11,12,13], no previous finite element analysis was performed simulating the combination of an Acrylic Splint Herbst Appliance and skeletal anchorage in both the upper and lower arch.
Therefore, this study aims to contribute to the growing evidence supporting advanced anchorage and assessment techniques in orthodontics, where miniscrews and functional appliances are used together, providing a comprehensive overview of the technologies’ potential benefits and applications in clinical practice.
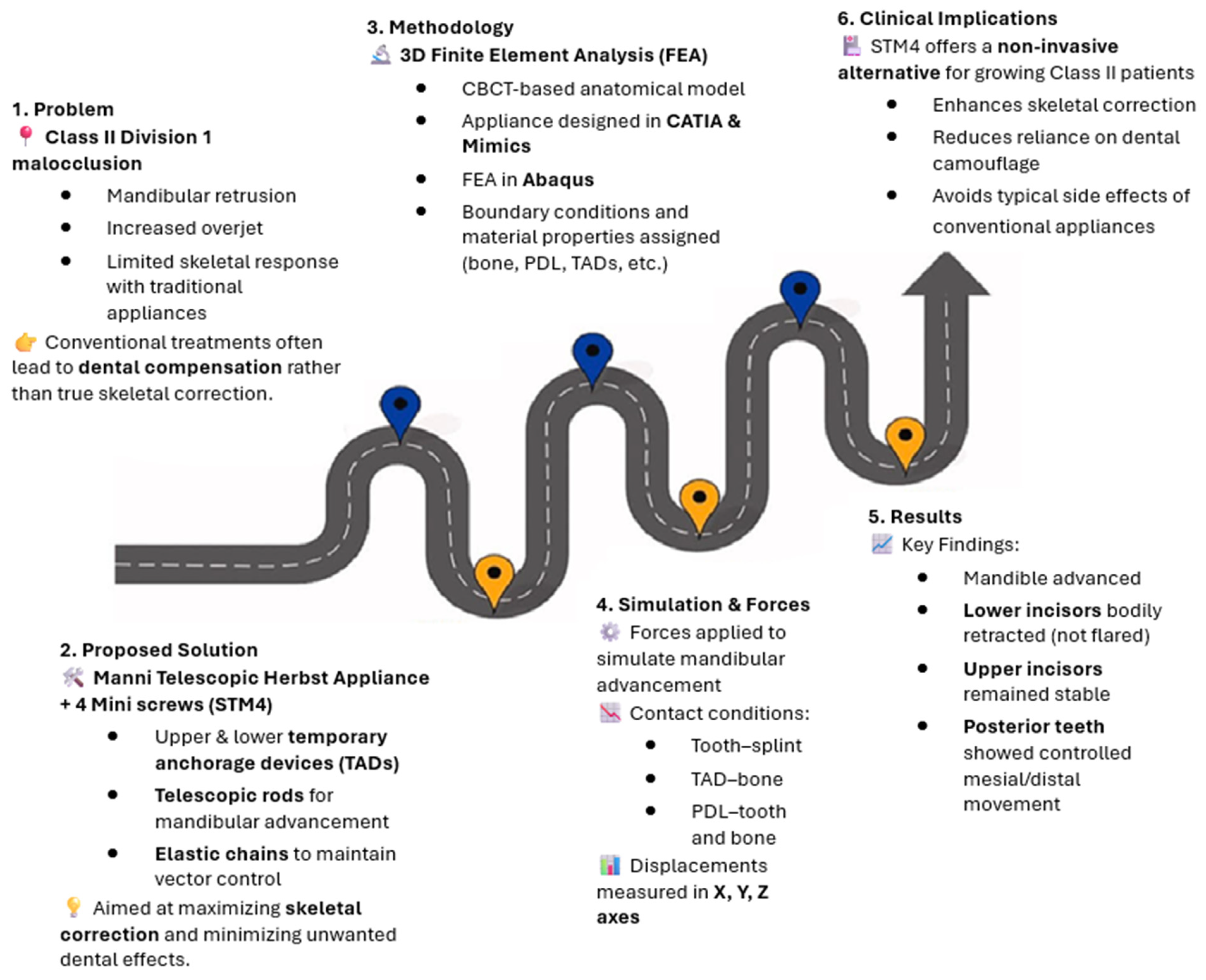
Moreover, this design introduces a novel approach that integrates functional appliances and miniscrews with elastic chains in both the arches. It leverages the precision of finite element analysis (FEA) to evaluate the appliance’s effects on the skeletal structure. In particular, this research aims to assess the position of the upper and lower dentition, especially the lower and upper incisors. Using FEA, the study quantifies the changes induced by this appliance along the X, Y, and Z axes, providing a three-dimensional view of the resulting orthodontic movements. Figure 1 provides a graphical abstract of this article.
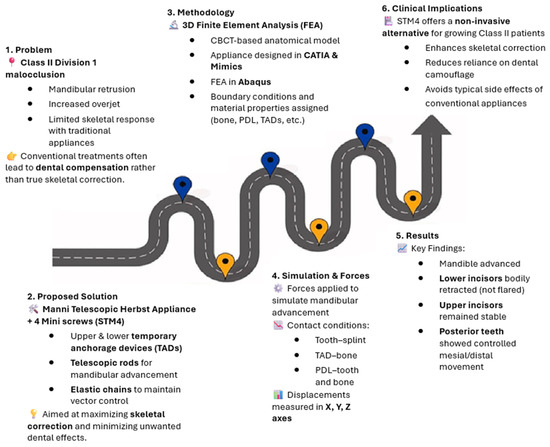
Figure 1.
Schematic diagram of the main contents of the present study.
2. Materials and Methods
This study is a computational analysis conducted using archived Cone Beam Computed Tomography (CBCT) data. Ethical approval was not required since no direct patient involvement occurred and all data were anonymized before analysis. This approach aligns with institutional and ethical guidelines for retrospective studies using previously recorded imaging data.
To perform FEA analysis, the following procedure was applied.
2.1. Imaging
High-definition CBCT scans of a skeletal Class II patient with permanent dentition were acquired to accurately capture the patient’s maxilla and mandible’s intricate bony and dental anatomy. The scans were taken with a 0.25 mm slice thickness to optimize detail resolution. The DICOM format was used for image storage, ensuring seamless integration with 3D modeling software for further processing.
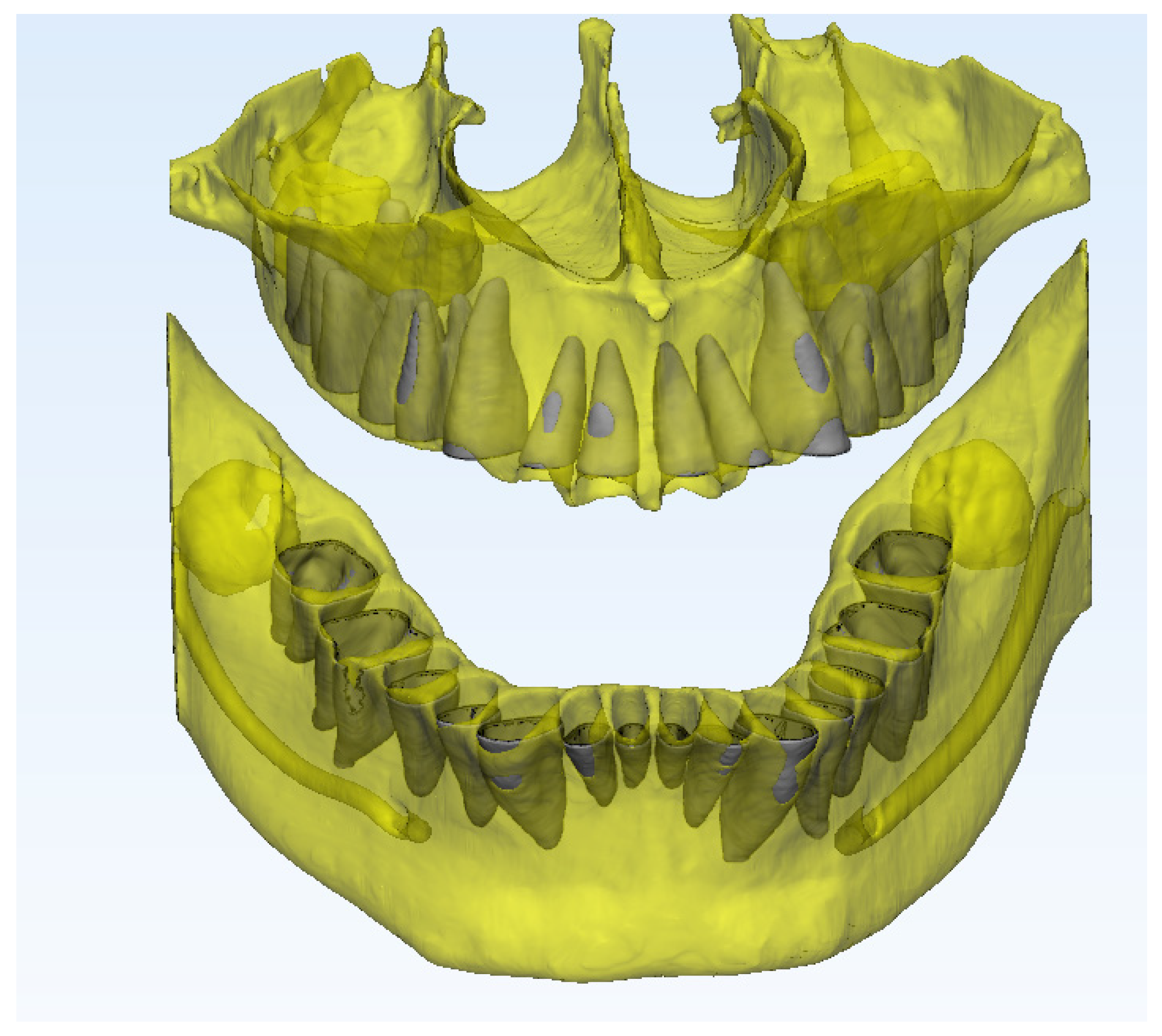
2.2. Three-Dimensional Reconstruction and Model Preparation
The DICOM data were imported into Mimics software for precise 3D reconstruction of dental and maxillofacial structures. The software used in this study includes Mimics 21 (Materialise, Leuven, Belgium), CATIA V5R21 (Dassault Systèmes, Vélizy-Villacoublay, France), and Abaqus 2024 (Dassault Systèmes, Vélizy-Villacoublay, France). These software packages were utilized for image processing, 3D modeling, and finite element analysis, respectively.
A robust segmentation process enabled the isolation of individual anatomical features, followed by advanced 3D reconstruction. Post-reconstruction refinements, such as smoothing and defect correction, were conducted to enhance model fidelity.
2.3. Appliance Design
- ○
- The appliance comprises a maxillary fixed palatal arch connected by two telescoping rods to a mandibular acrylic splint. The rods permit forward mandibular movement along with a lower splint. The trans palatal arch is bonded onto the upper first molars. A second trans palatal arch, not connected to the first one, is placed onto two miniscrews inserted in the T-zone between the upper canine and the first upper premolar teeth. The upper TADs were titanium, with a length of 11 mm and a diameter of 2 mm (TAD for expanders, D2 L11 mm; Leone, Sesto Fiorentino, Italy). Bilateral elastic chains (Memory Chain, 150/200 g for each side; American Orthodontics, Sheboygan, Wis) connect the two palatal arches. The applied forces were derived from established biomechanical studies and validated clinical protocols to ensure physiologically relevant load distribution [10].
- ○
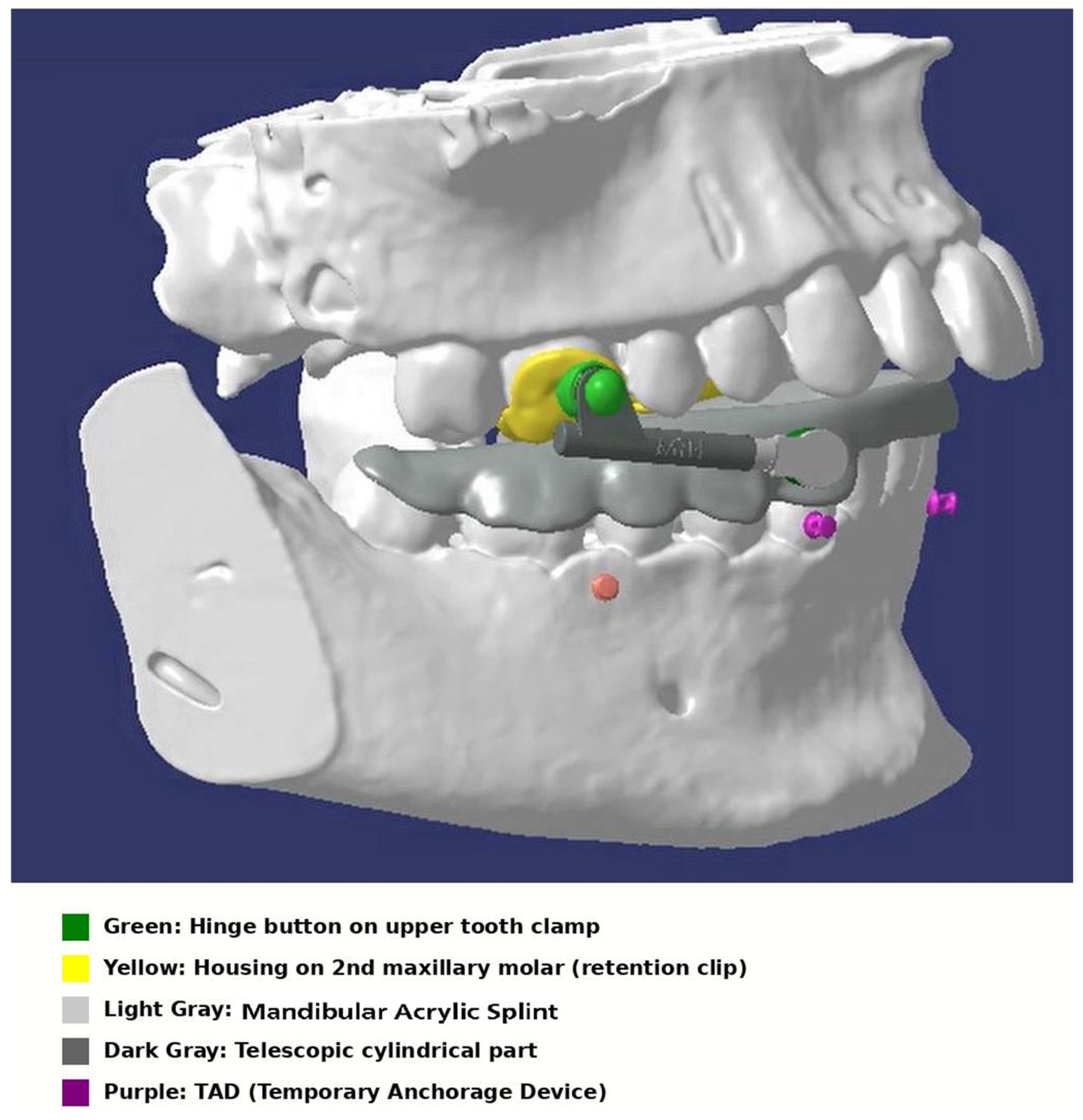
- In the mandible, auxiliary buttons were bonded on the buccal surface of the lower cuspids, and two 1.4 mm × 8 mm TADs (Osstem, Seoul, Republic of Korea) were placed bilaterally between the second premolar and first molar in the attached gingiva, with an insertion angle of about 45°. Elastic chains (Memory Chain, 150/200 g for each side; American Orthodontics, Sheboygan, Wis) were applied between the buttons and the lower miniscrews. The force provided by the elastic chains should be as parallel as possible to the occlusal plane (horizontal, depending on the bone availability). This protocol is defined as a Skeletal Therapy Manni Telescopic Herbst 4 TAD (STM4). Figure 2 shows the appliance design from a lateral perspective at baseline.
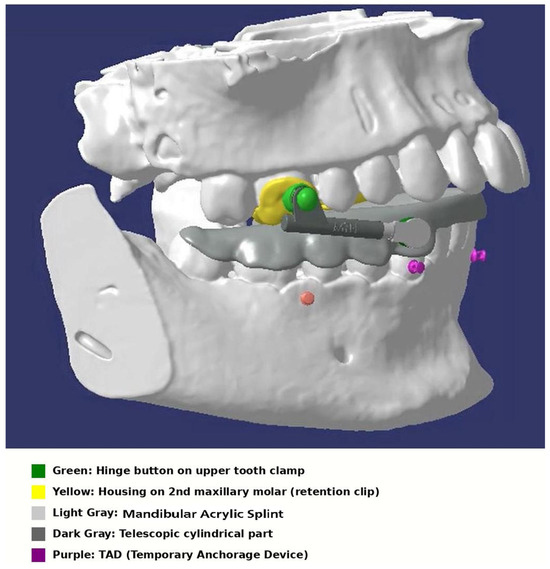 Figure 2. Lateral view of the appliance design before mandibular advancement.
Figure 2. Lateral view of the appliance design before mandibular advancement.
2.4. Boundary Conditions
In this study, the boundary conditions were defined to replicate real-world mechanical behavior as accurately as possible. The force was applied to the telescopic component, inducing its controlled expansion. This predefined displacement from the closed to the open position generated forces transmitted to the splints and subsequently to the teeth. By implementing this approach in the computational model, we ensured that the force application and system interactions closely mimicked clinical conditions. We will clarify this methodology in the revised manuscript for improved transparency.
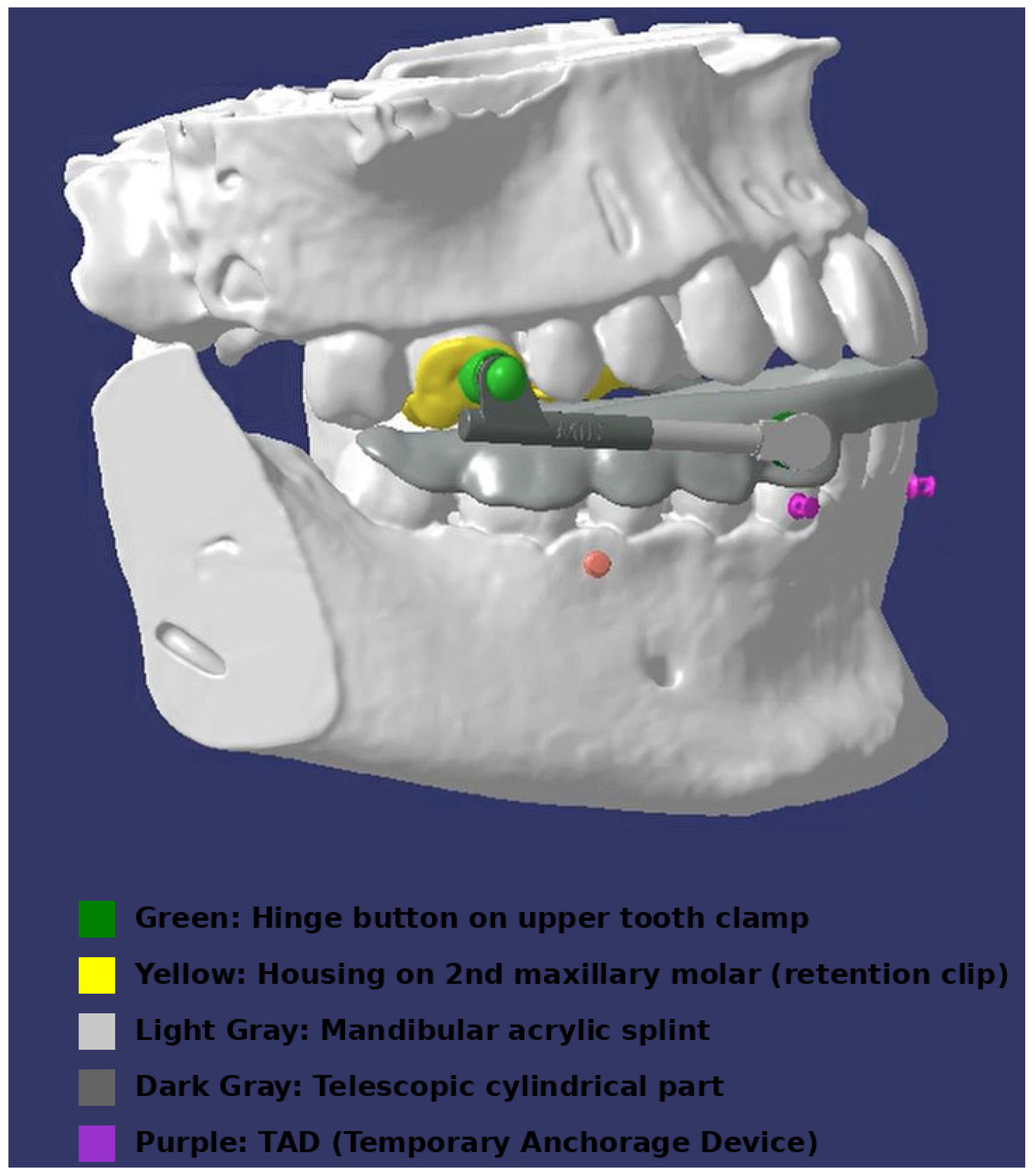
Figure 3 shows a lateral view of the appliance design after mandibular advancement.
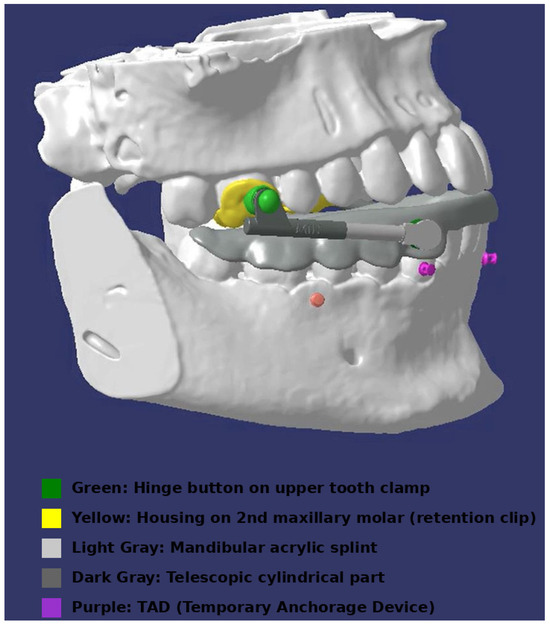
Figure 3.
Lateral view of the appliance design following mandibular advancement.
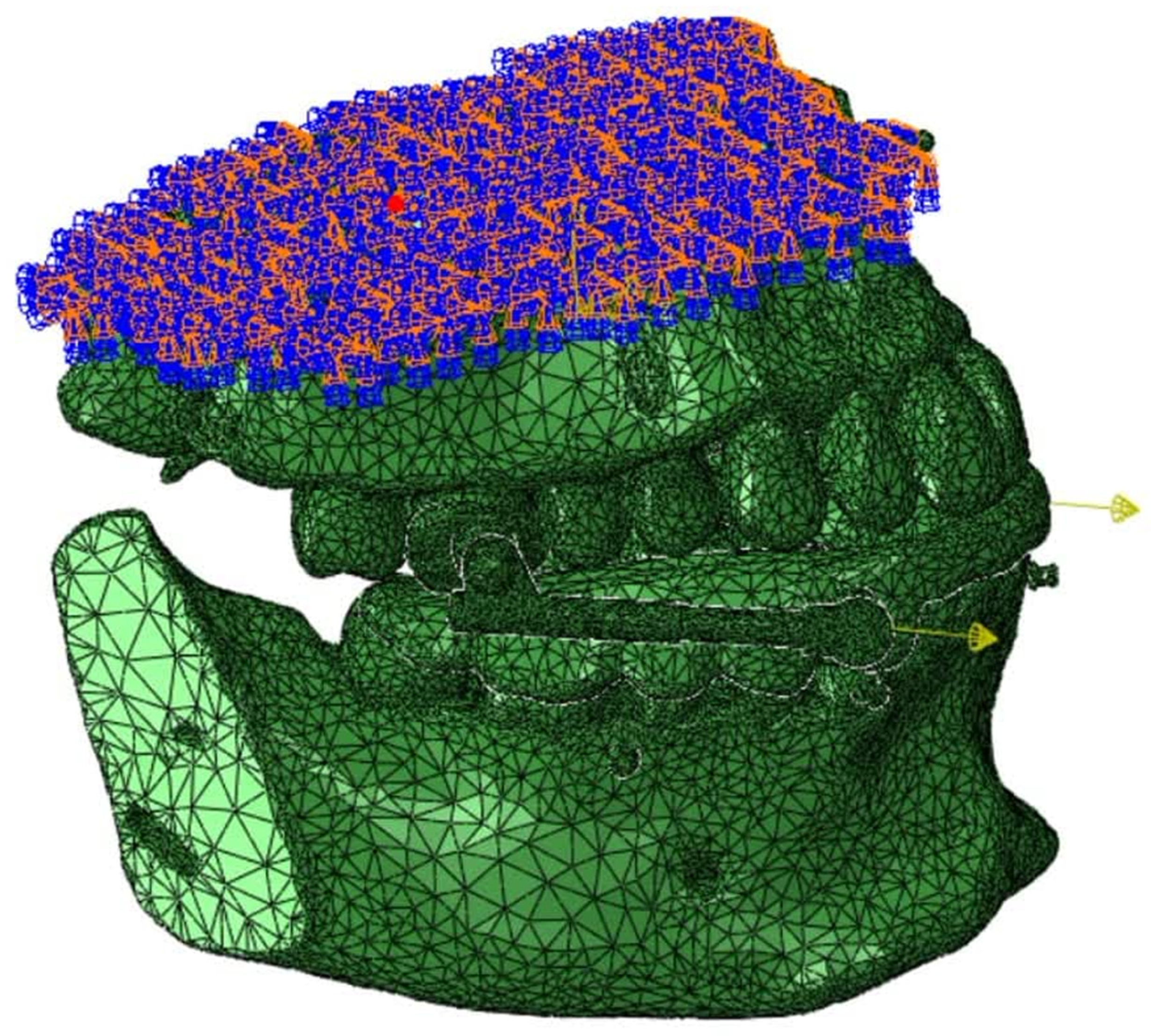
Figure 4 depicts the boundary and loading conditions applied in the finite element analysis (FEA) model to simulate the biomechanical behavior of the maxillary and mandibular structures under forces. The arrows represent the forces exerted from the applliace to the mandible (forward movement).
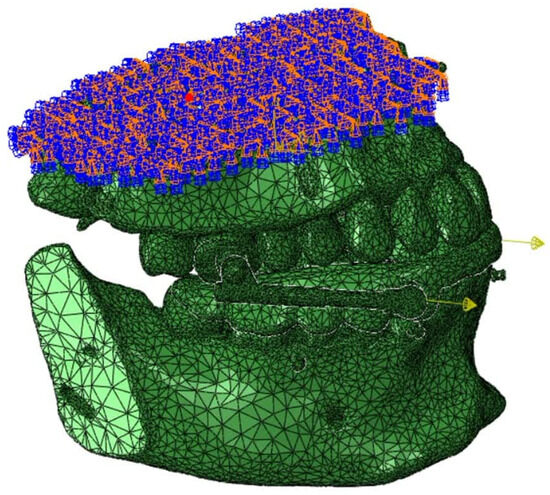
Figure 4.
Boundary conditions and loading conditions in the FEA simulation.
The boundary conditions include fixed supports at key points of the model to simulate the constraints of the model. At the same time, the applied forces represent the load exerted by the functional appliance. These conditions are crucial for accurately assessing the stress distribution, strain, and displacement patterns during the mandibular advancement simulation.
Figure 5 clearly illustrates the Periodontal Dental Ligament (PDL) and its distinct mechanical properties compared to the teeth and the bone.
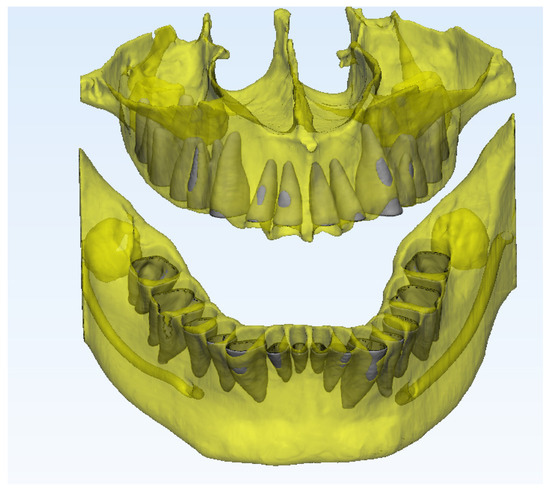
Figure 5.
Periodontal ligament conditions in the FEA simulation.
Friction coefficients and contact conditions between various components are defined as follows:
- PDL with bone and PDL with tooth: a friction coefficient of 0.3 has been assigned to both interfaces to simulate the interaction between the periodontal ligament (PDL) with bone and tooth structures.
- Tooth with resin splint: similarly, a friction coefficient of 0.3 has been defined between the tooth and the resin splint to represent their interaction accurately.
- TAD (Temporary Anchorage Device) with bone: a fully bonded contact has been assumed between the TAD and bone, reflecting the osseointegration and stable anchorage typically observed in clinical scenarios.
- Cortical and cancellous bone interface: a fully bonded contact has been considered between cortical and cancellous bone layers, ensuring unified mechanical behavior under loading conditions.
- Titanium components: to accurately simulate their interaction, a friction coefficient of 0.12 has been defined between the titanium components.
2.5. Geometric Optimization in STL Format
The STL models generated from Mimics were further refined in Geomagic x Design to prepare for finite element analysis. This step involved automated and manual correction of open meshes, surface irregularities, and non-uniform edge profiles to achieve optimal model integrity for meshing and simulation.
2.6. Finite Element Model Development
The optimized STL models were imported into Abaqus, where essential mechanical properties were assigned based on validated data:
- Titanium: elastic modulus of 113,000 MPa; Poisson’s ratio of 0.33.
- 316L stainless steel: elastic modulus of 200,000 MPa; Poisson’s ratio of 0.3.
- Bone and dental structures: the elastic moduli are set at 2000 MPa and 20,000 MPa, respectively, with a Poisson’s ratio of 0.3.
- Periodontal ligament (PDL): represented with an elastic modulus of 0.5 MPa and a Poisson’s ratio of 0.49 to simulate its biomechanical properties.
Material properties for each component used in the FE model can be seen in Table 1.

Table 1.
Material properties for each component used in the FE model.
2.7. Mesh Generation and Boundary Conditions
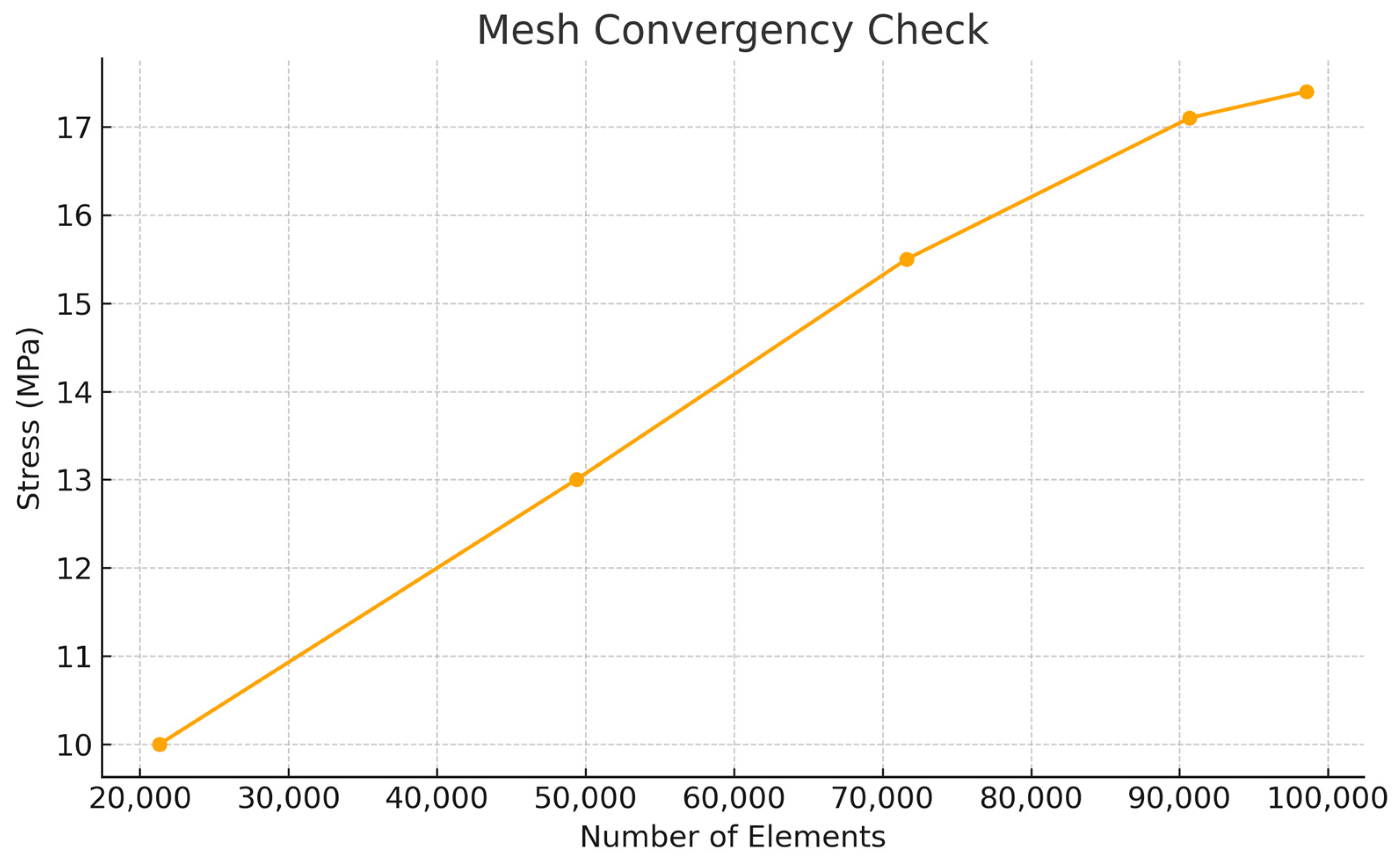
Meshing was performed using tetrahedral C3D4 elements, which balanced computational efficiency and detailed anatomical representation. Boundary conditions were rigorously defined to simulate physiological constraints, including fixed points for anchorage and mobile interactions for dynamic analysis. Contact properties between the PDL and bone, teeth, and orthodontic appliances were precisely modeled to replicate realistic biomechanical interactions. Table 2 shows the number of nodes. Mesh convergence analysis can be seen in Scheme 1.

Table 2.
The number of nodes for each material.
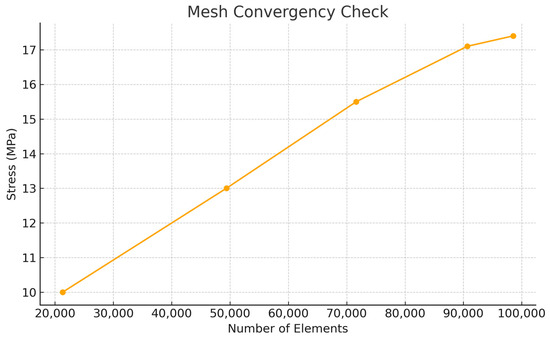
Scheme 1.
Mesh convergence analysis within finite element analysis.
2.8. Dynamic Simulation in CATIA
The refined 3D models were imported into CATIA’s DMU kinematic module for kinematic analysis. Customized motion constraints were applied to simulate mandibular advancements and related dental displacements, aligning with patient-specific treatment protocols. This phase enabled the evaluation of mandibular response and stress transmission across dentoalveolar structures under controlled conditions.
2.9. Finite Element Analysis and Evaluation of Results
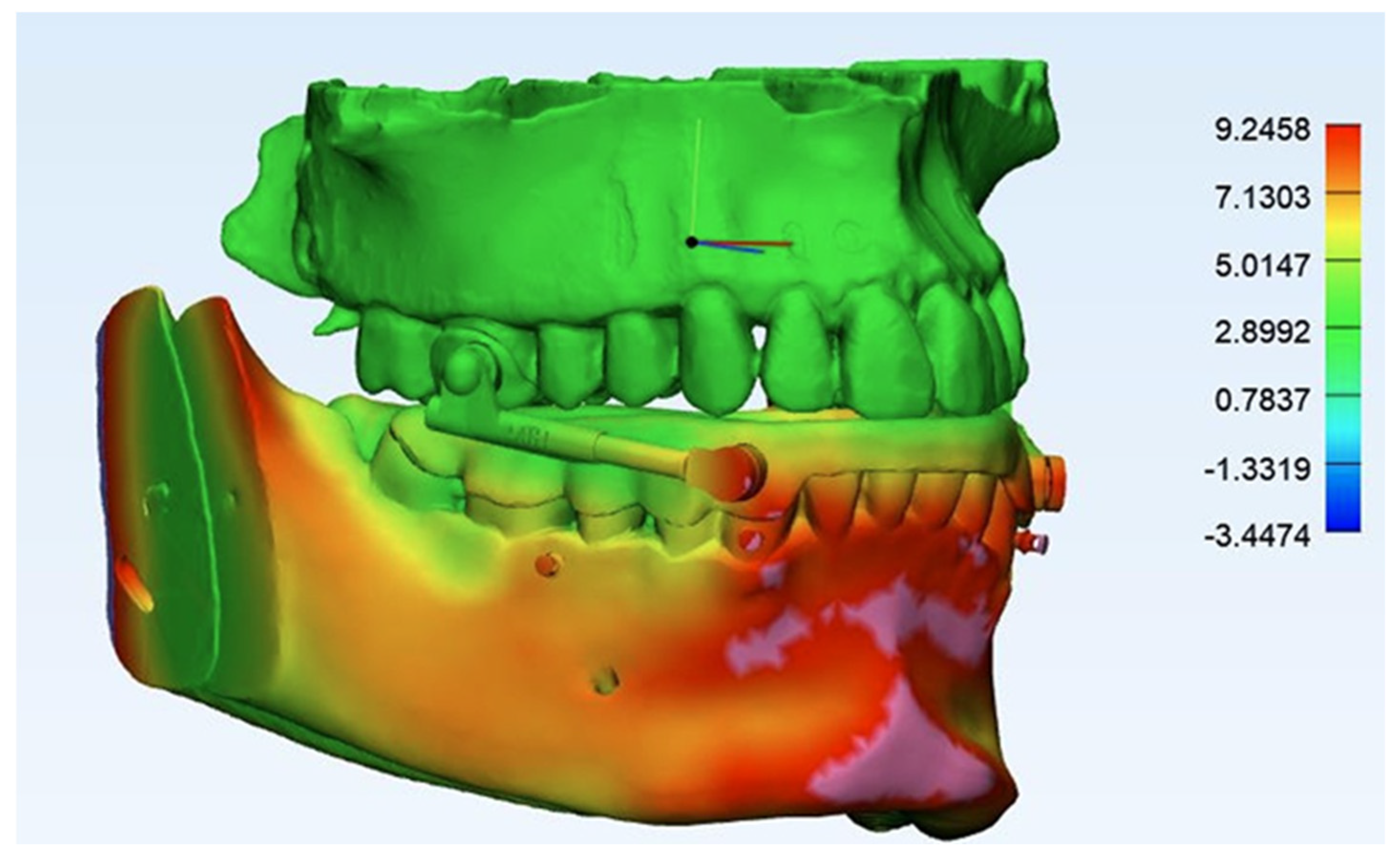
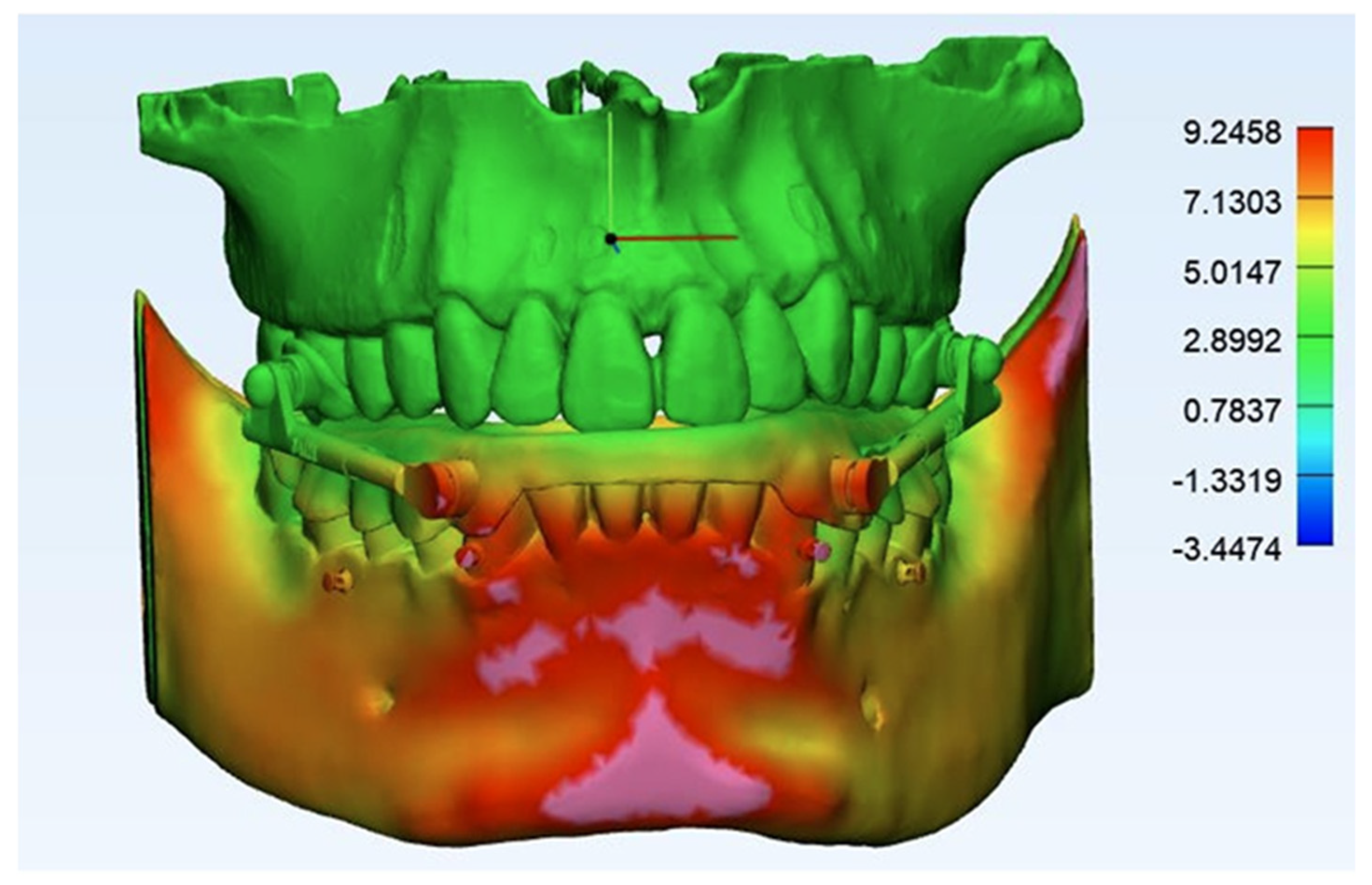
Advanced FEA simulations were conducted in Abaqus, focusing on analyzing stress distribution, strain, and deformation patterns within the maxillary and mandibular complexes under orthodontic forces. Displacement vectors were extracted and interpreted to assess biomechanical stability, appliance efficacy, and potential areas of excessive stress, ensuring precise insights for clinical implications and treatment optimization. Figure 6 and Figure 7 show the lateral and frontal views of finite element analysis after mandibular advancement.
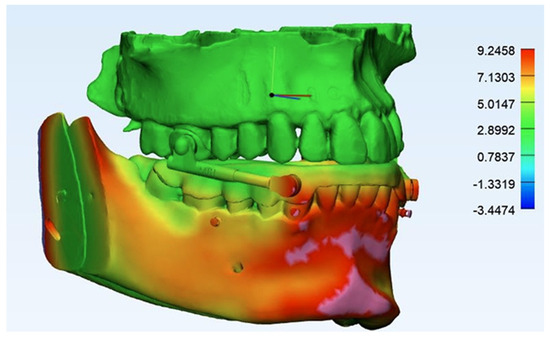
Figure 6.
Lateral view of finite element analysis following mandibular advancement.
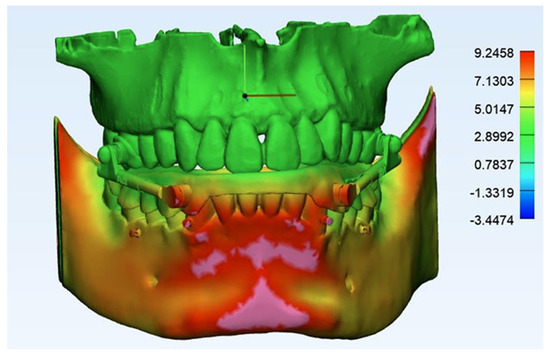
Figure 7.
Frontal view of finite element analysis after mandibular advancement.
FEA provided three-dimensional results with respect to displacement. The movement along the X-axis indicates the amount of displacement to the left and right. The plus value indicates the right movement and the minus value indicates the left movement. Movement along the Y-axis represents vertical displacement (upward and downward). The plus sign indicates upward movement and the minus sign indicates downward movement. Meanwhile, movement along the Z-axis reflects the anterior–posterior displacement of the teeth. A plus sign indicates a forward movement and a minus sign indicates a backward movement. The following skeletal points were considered in the analysis: Pogonion (Pog), Menton (Me), Point B, and Point A. For dental evaluation, the following points were considered: the incisors’ incisal edge, the crown center of the posterior teeth, and the apex of the upper and lower central incisors, lateral incisors, canines, first and second premolars, and first and second molars.
3. Results
The resulting displacements of the considered structures along the X, Y, and Z axes are reported in Table 3, Table 4 and Table 5. In particular, displacements of skeletal points are reported in Table 1. On the Z plane, forces from the appliance caused the mandible to move forward. The most significant forward mandibular movement occurred at Point B, which was 10.18 millimeters (mm), followed by chin prominence (the Pogonion), which was 10.11 millimeters (mm), and the Menton, which also moved forward 8.25 mm. On the contrary, Point A moved 0.22 mm backwards. The mandible did not move in the X displacement, identifying no lateral movements. Finally, Y displacement identifies the downward rotation of the mandible: Point B, Pogonion, and Menton were moved downward −0.32, −0.52, and −0.67 mm, respectively.

Table 3.
Skeletal displacement.

Table 4.
Displacement of mandibular dentition.

Table 5.
Displacement of maxillary dentition.
Z displacement showed that the incisal edge of the lower central, lateral, and canines moved lingually 0.41, 0.45, and 0.47 mm, respectively. On the contrary, the crown center of the lower first, the second premolar, and the first and second molar moved forward 0.65, 0.55, 021, and 0.46 mm, respectively. The apex of the lower central lateral and canines moved backward 0.05, 0.05, and 0.07 mm, respectively. The upper central, lateral, and canine incisal edges moved palatally 0.05, 0.06, and 0.08 mm, respectively. On the other hand, the apex of these teeth was moved labially 0.07, 0.05, and 0.05 mm, respectively.
4. Discussion
Finite element analysis (FEA) plays a crucial role in investigating orthodontic biomechanics and tooth movement. Several studies have utilized FEA to evaluate 3D orthodontic force measurements and assess lingual orthodontic systems. It serves as a fundamental assessment tool for studying growth modulation, myofunctional therapy, and analyzing various mechanical aspects involved in orthodontic treatment planning [19,20,21,22]. With the advancement of computing technology, there is a growing preference for virtual analysis and tools that cater to the evaluation of mechanical properties in hard and soft facial tissues, osteosynthesis materials, implant components, and various biological and synthetic bone substitutes. These tools offer a more accurate, reproducible, safe, and cost-effective approach, regardless of the complexity of the materials. Finite element analysis (FEA) effectively meets this demand by enabling the generation of models that provide insights into the biological responses of bone to biomechanical changes. Additionally, FEA allows the simulation of numerous complementary components to assess their impact on the tested subject and the adjacent anatomical structures [23]. Functional appliances, stimulating mandibular advancement, have been used for over a century to treat Class II malocclusion. The Herbst appliance is effective and efficient in treating Class II Division I malocclusions resulting from mandibular deficiency, as it does not depend on patient compliance [7,8,24]. Research indicates that the Manni Telescopic Herbst (MTH) can help manage the dental side effects associated with the Herbst appliance by combining lower and upper TADs with elastomeric chains. In particular it reduces buccal flaring of lower incisors and palatal tipping of the upper ones, preserving the overjet needed for a proper skeletal advancement. Additionally, the lower splint better control both the occlusal plane (limiting the clockwise rotation of the mandible) and the inclination of the lower incisors [10,11].
In this study, the displacement of the mandible and movement of lower and upper dentition were investigated by FEA in a fixed functional appliance for a Class II Division I malocclusion. This study showed that the mandible was moved forward, the clockwise rotation of the lower jaw was limited, while the lower incisors were retracted. The lower and upper dentition movements were negligible in X displacement and Y displacement. This study emphasizes that the incisal edge of the lower incisors was moved lingually. At the same time, the apex of the lower incisors was moved in a backward position, which shows that the lower incisors were moved bodily in a backward position. On the contrary, in most functional appliances, the lower anterior teeth move forward [7,25,26]. However, in this appliance, not only did the lower anterior teeth not move forward, but they were also moved backwards, with great anchorage control. This study also showed that the incisal edge and the apex of the upper incisors were almost stable, confirming proper control also in the upper arch. Looking at the posterior teeth, the crown and apex of the lower first and second premolars and first and second molars moved slightly forward, resulting in a bodily movement. On the other hand, the crown of the upper posterior teeth moved mesially, while the apex of the posterior segment was displaced distally. This indicates a mild tipping movement of the upper posterior teeth.
As highlighted in this article, incorporating skeletal anchorage can address the limitations of traditional nonsurgical treatments for Class II Division I patients. In these patients, the malocclusion is usually managed through dental camouflage techniques such as proclination of the lower incisors, retroclination of the upper incisors, and clockwise rotation of the occlusal and mandibular planes. All these dental compensations seem to be reduced when combining an MTH Herbst appliance and skeletal anchorage in both the upper and lower arch. Therefore, the STM4 protocol could be a viable alternative for correcting skeletal Class II malocclusion, reducing dental compensations and increasing the skeletal outcome, as observed in clinical practice [27]. Other FEA studies analyzing mandibular advancement devices without skeletal anchorage have observed a greater distribution of stress across all teeth, leading to forward movement of the mandibular teeth and periodontal ligament while shifting the maxillary teeth and periodontal ligament backwards [28]. On the other hand, when the appliance is combined with skeletal anchorage, a greater skeletal correction in growing children with minimal alterations in the inclination of the lower incisors was observed [29].
Implants, mini-implants (or miniscrews), and miniplates have been proposed as anchorage devices to enhance orthodontic biomechanics. Miniplates offer absolute anchorage because they are anchored outside the alveolar bone, supported by dense trabecular structures and thick cortical bone. However, they are more invasive. On the contrary, miniscrews, despite having certain limitations, particularly when subjected to multiple forces or high-force magnitudes, and despite their placement being dependent on bone availability, are widely used and can be easily managed by orthodontists.
4.1. Limitations
The reliability of the present model may have been affected by certain methodological limitations, including the use of a single subject’s CT scan, variations in material properties, and the discrepancy between anatomic modeling and the realistic behavior of peri-oral muscles and soft tissue, as their activation was not considered. To overcome these limitations, future studies should incorporate different force levels and diverse craniofacial forms and growth patterns, utilizing a larger sample size with age-specific material properties. This would provide a more comprehensive understanding of the biomechanical behavior of skeletally anchored FFAs.
Furthermore, advancements in imaging systems and post-processing software could facilitate the direct segmentation of the TMJ region, articular disc, and surrounding muscles, significantly improving the model’s anatomical accuracy and overall quality. These improvements would ultimately enhance the credibility and clinical applicability of the obtained results.
4.2. Future Directions
- Further research should incorporate multi-subject cohorts with diverse craniofacial morphologies.
- Advanced imaging techniques should be integrated to enable direct segmentation of the TMJ, articular disc, and associated soft tissues for greater anatomical precision.
- Prospective clinical studies are necessary to substantiate the biomechanical insights provided by this computational model.
4.3. Clinical Relevance
The clinical relevance of this study lies in its evaluation of a Manni Telescopic Herbst Appliance with skeletal anchorage in both the arches as a valuable treatment option for Class II Division I malocclusion. By combining miniscrews and elastic chains, this approach may minimize dentoalveolar compensations in both the arches and may better control the vertical dimension. The consequent result is greater mandibular advancement and proper vertical control. Unlike conventional orthodontic camouflage, which can lead to undesirable incisor proclination and clockwise rotation of the occlusal plane, this method enhances treatment outcomes, precision, and stability. Consequently, it provides orthodontists with a reliable and biomechanically efficient alternative, one that is particularly beneficial for growing patients requiring comprehensive skeletal correction.
5. Conclusions
This study highlights the effectiveness of a Herbst appliance with skeletal anchorage in treating Class II Division I malocclusion. The findings reveal that an MTH Herbst Appliance with four miniscrews and elastic chains (STM4), distinct from classic Class II devices, successfully advanced the mandible, controlled the vertical dimension, and reduced dentoalveolar compensations. The appliance retracted the lower incisors, while the upper incisors demonstrated good stability. These biomechanical effects suggest that the appliance offers a precise and efficient solution for managing Class II malocclusion without the drawbacks of conventional dental camouflage, particularly proclination of the lower incisors. Therefore, incorporation of skeletal anchorage addresses the limitations of traditional treatments, making this approach a promising one for growing patients.
Author Contributions
Conceptualization, A.B., A.J. and A.M.; methodology, A.J.; software, R.F. and M.H.; validation, G.G. and A.M.; formal analysis, R.F. and M.H.; writing—original draft preparation, A.B. and A.J.; writing—review and editing, M.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The datasets generated and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Owayda, A.; Al-Sabbagh, R.; Farah, H.; Owayda, T.; Al-Ahmad, S. The effectiveness of the total-maxillary-arch-distalization approach in treating class II division 1 malocclusion: A systematic review. Clin. Oral Investig. 2024, 28, 333. [Google Scholar] [CrossRef] [PubMed]
- Almrayati, D.M.; Hajeer, M.Y.; Almusawi, A.O.A.; Jaber, S.T.; Baba, M.O.; Ajaj, M.A.; Ajaj Sr, M.A. Evaluation of the External Soft Tissue Changes Following the Correction of Class II Skeletal Malocclusion in the Adolescence Period Using Removable and Fixed Functional Appliances: A Systematic Review and Meta-Analysis. Cureus 2024, 16, e57070. [Google Scholar] [CrossRef] [PubMed]
- Habumugisha, J.; Cheng, B.; Ma, S.Y.; Zhao, M.Y.; Bu, W.Q.; Wang, G.L.; Liu, Q.; Zou, R.; Wang, F. A non-randomized concurrent controlled trial of myofunctional treatment in the mixed dentition children with functional mouth breathing assessed by cephalometric radiographs and study models. BMC Pediatr. 2022, 22, 506. [Google Scholar] [CrossRef]
- Nucera, R.; Lo Giudice, A.; Rustico, L.; Matarese, G.; Papadopoulos, M.A.; Cordasco, G. Effectiveness of orthodontic treatment with functional appliances on maxillary growth in the short term: A systematic review and meta-analysis. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 600–611.e3. [Google Scholar] [CrossRef]
- Santori, F.; Masedu, F.; Ciavarella, D.; Staderini, E.; Chimenti, C.; Tepedino, M. Effect of Class II functional treatment on facial attractiveness, as perceived by professionals and laypeople. Sci. Rep. 2021, 11, 13989. [Google Scholar] [CrossRef]
- Staderini, E.; Ventura, V.; Meuli, S.; Maltagliati, L.Á.; Gallenzi, P. Analysis of the Changes in Occlusal Plane Inclination in a Class II Deep Bite “Teen” Patient Treated with Clear Aligners: A Case Report. Int. J. Environ. Res. Public Health 2022, 19, 651. [Google Scholar] [CrossRef]
- Pancherz, H. The Herbst appliance: Its biologic effects and clinical use. Am. J. Orthod. 1985, 87, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Pancherz, H. Treatment of Class II malocclusions by jumping the bite with the Herbst appliance. A cephalometric investigation. Am. J. Orthod. 1979, 76, 423–442. [Google Scholar] [CrossRef]
- Pancher, Z.H.; Hansen, K. Mandibular anchorage in Herbst treatment. Eur. J. Orthod. 1988, 10, 149–164. [Google Scholar] [CrossRef]
- Manni, A.; Migliorati, M.; Boggio, A.; Drago, S.; Paggi, E.; Calzolari, C.; Gastaldi, G.; Cozzani, M. Evaluation of the Co–Go–Me angle as a predictor in Class II patients treated with Herbst appliance and skeletal anchorage: A retrospective cohort study. Front. Oral Health 2024, 5, 1389628. [Google Scholar] [CrossRef]
- Gotti, E.; Doldo, T.; Castellana, F.; Cozzani, M.; Manni, A.; Gastaldi, G.; Boggio, A. Mandibular Advancement and Skeletal Anchorage in Class II Malocclusion Patients: A Systematic Review with Meta-Analysis. Oral 2024, 4, 417–440. [Google Scholar] [CrossRef]
- Al-Dboush, R.; Soltan, R.; Rao, J.; El-Bialy, T. Skeletal and dental effects of Herbst appliance anchored with temporary anchorage devices: A systematic review with meta-analysis. Orthod. Craniofac. Res. 2022, 25, 31–48. [Google Scholar] [CrossRef]
- Huang, Y.; Sun, W.; Xiong, X.; Zhang, Z.; Liu, J.; Wang, J. Effects of fixed functional appliances with temporary anchorage devices on Class II malocclusion: A systematic review and meta analysis. J. World Fed. Orthod. 2021, 10, 59–69. [Google Scholar] [CrossRef]
- Neves, A.M.; Nascimento, M.; de Almeida Cardoso, M.; Meloti, F.; Silva, E.; An, T.L. Finite element analysis of a newly designed miniplate for orthodontic anchorage in the maxillary anterior region. Am. J. Orthod. Dentofac. Orthop. 2022, 162, 656–667. [Google Scholar] [CrossRef] [PubMed]
- Akis, H.; Doruk, C. Dentofacial Effects of Fixed Functional Appliances with or without Mini Screw Anchorage in the Treatment of Class II Division I Malocclusion: A Finite Element Analysis. Turk. J. Orthod. 2018, 31, 7–12. [Google Scholar] [CrossRef]
- Kumar, D.; Sharma, R.; Arora, V.; Bhupali, N.R.; Tuteja, N. Evaluation of displacements and stress changes in the maxillo-mandibular complex with fixed functional appliance skeletally anchored on mandible using miniplates: A finite element study. J. Orthod. Sci. 2022, 11, 42. [Google Scholar] [CrossRef]
- Zhang, M.; Liu, X.; Zhang, R.; Chen, X.; Song, Z.; Ma, Y.; Jin, Z. Biomechanical effects of functional clear aligners on the stomatognathic system in teens with class II malocclusion: A new model through finite element analysis. BMC Oral Health 2024, 24, 1313. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Liu, Y.; Zhang, J.; Peng, W.; Jiang, X. Biomechanical investigation of orthodontic treatment planning based on orthodontic force measurement and finite element method before implementation: A case study. Technol. Health Care 2018, 26, 347–359. [Google Scholar] [CrossRef]
- Mascarenhas, R.; Parveen, S.; Shenoy, B.S.; Kumar, G.S.; Ramaiah, V.V. Infinite applications of finite element method. J. Indian Orthod. Soc. 2018, 52, 142–150. [Google Scholar] [CrossRef]
- Sugii, M.M.; Barreto, B.C.F.; Francisco Vieira Júnior, W.; Simone, K.R.I.; Bacchi, A.; Caldas, R.A. Extruded upper first molar intrusion: Comparison between unilateral and bilateral miniscrew anchorage. Dental Press J. Orthod. 2018, 23, 63–70. [Google Scholar] [CrossRef]
- Kushwah, A.; Kumar, M.; Goyal, M.; Premsagar, S.; Rani, S.; Sharma, S. Analysis of stress distribution in lingual orthodontics system for effective en masse retraction using various combinations of lever arm and mini implants: A finite element method study. Am. J. Orthod. Dentofac. Orthop. 2020, 158, e161–e172. [Google Scholar] [CrossRef]
- Cattaneo, P.M.; Cornelis, M.A. Orthodontic tooth movement studied by finite element analysis: An update. What can we learn from these simulations? Curr. Osteoporos. Rep. 2021, 19, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Scarano, A.; Lorusso, F.; Santos de Oliveira, P.; Kunjalukkal Padmanabhan, S.; Licciulli, A. Hydroxyapatite block produced by sponge replica method: Mechanical, clinical and histologic observations. Materials 2019, 12, 3079. [Google Scholar] [CrossRef] [PubMed]
- Torsello, F.; D’Amico, G.; Staderini, E.; Marigo, L.; Cordaro, M.; Castagnola, R. Factors Influencing Appliance Wearing Time during Orthodontic Treatments: A Literature Review. Appl. Sci. 2022, 12, 7807. [Google Scholar] [CrossRef]
- Pancherz, H. The mechanism of Class II correction in Herbst appliance treatment. A cephalometric investigation. Am. J. Orthod. 1982, 82, 104–113. [Google Scholar] [CrossRef]
- Showkatbakhsh, R.; Castaldo, M.I.; Jamilian, A.; Padricelli, G.; Cappabianca, S.; Perillo, L. Treatment effects of R-appliance and Frankel-2 in Class II division 1 malocclusions. Eur. J. Paediatr. Dent. 2013, 14, 17–22. [Google Scholar]
- Manni, A.; Boggio, A.; Castellana, F.; Gastaldi, G.; Cozzani, M. Mandibular Advancement after Pubertal Peak with Acrylic Splint Herbst Appliance Anchored to Four Miniscrews: A Retrospective Controlled Study. Oral 2024, 4, 449–458. [Google Scholar] [CrossRef]
- Zhu, C.; Li, R.; Yuan, L.; Zheng, Y.; Jin, Y.; Li, H.; Liu, C.; Xia, L.; Fang, B. Effects of the advanced mandibular spring on mandibular retrognathia treatment: A three-dimensional finite element study. BMC Oral Health 2022, 22, 271. [Google Scholar] [CrossRef]
- Duggal, I.; Sidhu, M.S.; Chawla, A.; Dabas, A.; Dhimole, V.K. Effects of miniplate anchored Herbst appliance on skeletal, dental and masticatory structures of the craniomandibular apparatus: A finite element study. Int. Orthod. 2021, 19, 301–309. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).