Trauma-Related Internalizing and Externalizing Behaviors in Adolescence: A Bridge between Psychoanalysis and Neuroscience
Abstract
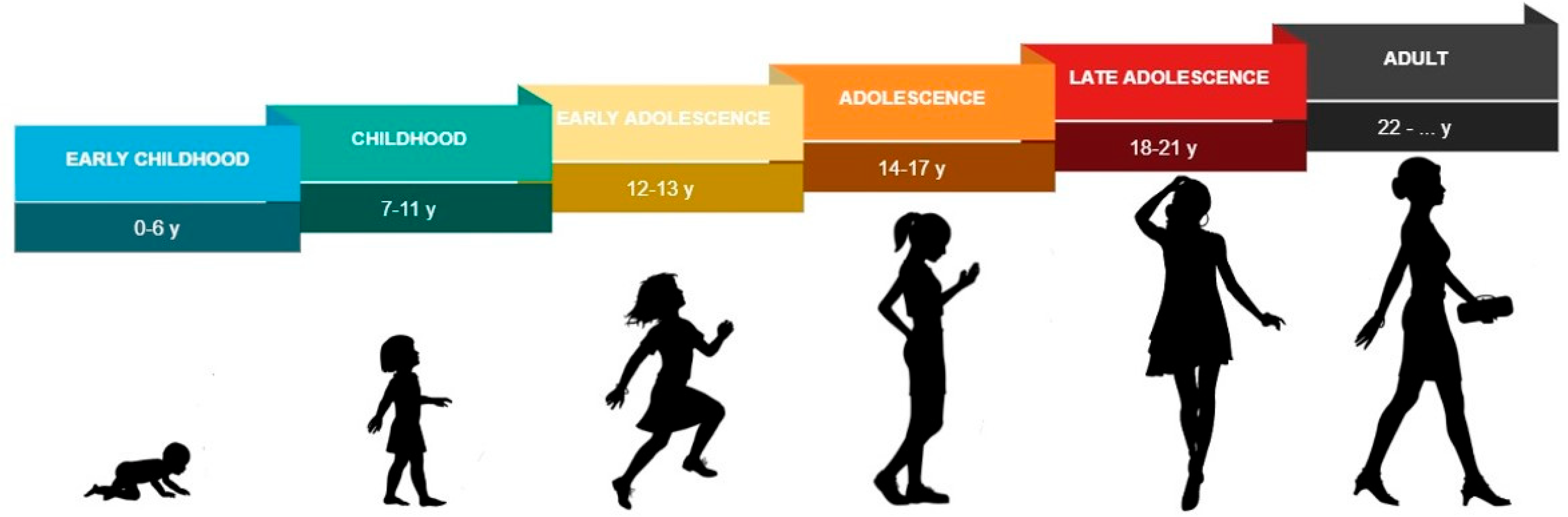
:1. Introduction
2. Diagnostic Aspects and Neurobiological Correlates in Traumatized Adolescents: A Scenario on Externalizing/Internalizing Behaviors
3. Therapeutic Aspects in Traumatized Adolescents: An Enlargement of the Psychoanalytic Setting in Multiple and Multimodal Treatments
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Copeland, W.E.; Keeler, G.; Angold, A.; Costello, E.J. Traumatic Events and Posttraumatic Stress in Childhood. Arch. Gen. Psychiatry 2007, 64, 577–584. [Google Scholar] [CrossRef] [PubMed]
- Birn, R.M.; Patriat, R.; Phillips, M.L.; Germain, A.; Herringa, R.J. Childhood Maltreatment and Combat Posttraumatic Stress Differentially Predict Fear-Related Fronto-Subcortical Connectivity. Depress. Anxiety 2014, 31, 880–892. [Google Scholar] [CrossRef] [PubMed]
- Spear, L.P. The Adolescent Brain and Age-Related Behavioral Manifestations. Neurosci. Biobehav. Rev. 2000, 24, 417–463. [Google Scholar] [CrossRef]
- Kessler, R.C.; Adler, L.A.; Barkley, R.; Biederman, J.; Conners, C.K.; Faraone, S.V.; Greenhill, L.L.; Jaeger, S.; Secnik, K.; Spencer, T.; et al. Patterns and Predictors of ADHD Persistence into Adulthood: Results from the National Comorbidity Survey Replication. Biol. Psychiatry 2005, 57, 1442–1451. [Google Scholar] [CrossRef]
- Paus, T.; Keshavan, M.; Giedd, J.N. Why Do Many Psychiatric Disorders Emerge during Adolescence? Nat. Rev. Neurosci. 2008, 9, 947–957. [Google Scholar] [CrossRef]
- Merikangas, K.R.; He, J.; Burstein, M.; Swanson, S.A.; Avenevoli, S.; Cui, L.; Benjet, C.; Georgiades, K.; Swendsen, J. Lifetime Prevalence of Mental Disorders in U.S. Adolescents: Results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 980–989. [Google Scholar] [CrossRef]
- LeMoult, J.; Humphreys, K.L.; Tracy, A.; Hoffmeister, J.-A.; Ip, E.; Gotlib, I.H. Meta-Analysis: Exposure to Early Life Stress and Risk for Depression in Childhood and Adolescence. J. Am. Acad. Child Adolesc. Psychiatry 2020, 59, 842–855. [Google Scholar] [CrossRef]
- Rudolph, K.D.; Flynn, M. Childhood Adversity and Youth Depression: Influence of Gender and Pubertal Status. Dev. Psychopathol. 2007, 19, 497–521. [Google Scholar] [CrossRef]
- Dahl, R.E.; Gunnar, M.R. Heightened Stress Responsiveness and Emotional Reactivity during Pubertal Maturation: Implications for Psychopathology. Dev. Psychopathol. 2009, 21, 1–6. [Google Scholar] [CrossRef]
- Doom, J.R.; Gunnar, M.R. Stress Physiology and Developmental Psychopathology: Past, Present, and Future. Dev. Psychopathol. 2013, 25, 1359–1373. [Google Scholar] [CrossRef] [Green Version]
- Busso, D.S.; McLaughlin, K.A.; Sheridan, M.A. Dimensions of Adversity, Physiological Reactivity, and Externalizing Psychopathology in Adolescence: Deprivation and Threat. Psychosom. Med. 2017, 79, 162–171. [Google Scholar] [CrossRef]
- Hofstra, M.B.; Van der Ende, J.; Verhulst, F.C. Pathways of Self-Reported Problem Behaviors from Adolescence into Adulthood. Am. J. Psychiatry 2002, 159, 401–407. [Google Scholar] [CrossRef]
- King, S.M.; Iacono, W.G.; McGue, M. Childhood Externalizing and Internalizing Psychopathology in the Prediction of Early Substance Use. Addict. Abingdon Engl. 2004, 99, 1548–1559. [Google Scholar] [CrossRef]
- Reef, J.; Diamantopoulou, S.; van Meurs, I.; Verhulst, F.; van der Ende, J. Predicting Adult Emotional and Behavioral Problems from Externalizing Problem Trajectories in a 24-Year Longitudinal Study. Eur. Child Adolesc. Psychiatry 2010, 19, 577–585. [Google Scholar] [CrossRef]
- Achenbach, T.M.; Howell, C.T.; Quay, H.C.; Conners, C.K. National Survey of Problems and Competencies among Four- to Sixteen-Year-Olds: Parents’ Reports for Normative and Clinical Samples. Monogr. Soc. Res. Child Dev. 1991, 56, 1–131. [Google Scholar] [CrossRef]
- Kovacs, M.; Devlin, B. Internalizing Disorders in Childhood. J. Child Psychol. Psychiatry 1998, 39, 47–63. [Google Scholar] [CrossRef]
- Feldman, R. What Is Resilience: An Affiliative Neuroscience Approach. World Psychiatry 2020, 19, 132–150. [Google Scholar] [CrossRef]
- Feldman, R. Social Behavior as a Transdiagnostic Marker of Resilience. Annu. Rev. Clin. Psychol. 2021, 17, 153–180. [Google Scholar] [CrossRef]
- Houston, S.M.; Herting, M.M.; Sowell, E.R. The Neurobiology of Childhood Structural Brain Development: Conception through Adulthood. Curr. Top. Behav. Neurosci. 2014, 16, 3–17. [Google Scholar] [CrossRef]
- Ho, T.C.; King, L.S. Mechanisms of Neuroplasticity Linking Early Adversity to Depression: Developmental Considerations. Transl. Psychiatry 2021, 11, 517. [Google Scholar] [CrossRef]
- Lingiardi, V.; Gazzillo, F. La Personalità e i Suoi Disturbi; Raffaello Cortina Editore: Milan, Italy, 2014. [Google Scholar]
- APA. Diagnostic and Statistical Manual of Mental Disorders: DSM-5TM, 5th ed.; American Psychiatric Publishing, Inc.: Arlington, VA, USA, 2013; p. xliv, 947; ISBN 978-0-89042-554-1. [Google Scholar]
- De Bellis, M.D.; Zisk, A. The Biological Effects of Childhood Trauma. Child Adolesc. Psychiatr. Clin. N. Am. 2014, 23, 185–222. [Google Scholar] [CrossRef]
- Agorastos, A.; Pervanidou, P.; Chrousos, G.P.; Baker, D.G. Developmental Trajectories of Early Life Stress and Trauma: A Narrative Review on Neurobiological Aspects Beyond Stress System Dysregulation. Front. Psychiatry 2019, 10, 118. [Google Scholar] [CrossRef]
- Kolacz, J.; Kovacic, K.K.; Porges, S.W. Traumatic Stress and the Autonomic Brain-Gut Connection in Development: Polyvagal Theory as an Integrative Framework for Psychosocial and Gastrointestinal Pathology. Dev. Psychobiol. 2019, 61, 796–809. [Google Scholar] [CrossRef]
- Dandash, O.; Cherbuin, N.; Schwartz, O.; Allen, N.B.; Whittle, S. The Long-Term Associations between Parental Behaviors, Cognitive Function and Brain Activation in Adolescence. Sci. Rep. 2021, 11, 11120. [Google Scholar] [CrossRef]
- Blakemore, S.-J. Development of the Social Brain during Adolescence. Q. J. Exp. Psychol. 2006 2008, 61, 40–49. [Google Scholar] [CrossRef]
- Pfeifer, J.H.; Allen, N.B. Puberty Initiates Cascading Relationships between Neurodevelopmental, Social, and Internalizing Processes across Adolescence. Biol. Psychiatry 2021, 89, 99–108. [Google Scholar] [CrossRef]
- Averbeck, B.B. Pruning Recurrent Neural Networks Replicates Adolescent Changes in Working Memory and Reinforcement Learning. Proc. Natl. Acad. Sci. USA 2022, 119, e2121331119. [Google Scholar] [CrossRef]
- Meldrum, B.S. Glutamate as a Neurotransmitter in the Brain: Review of Physiology and Pathology. J. Nutr. 2000, 130, 1007S–1015S. [Google Scholar] [CrossRef] [PubMed]
- Deidda, G.; Bozarth, I.F.; Cancedda, L. Modulation of GABAergic Transmission in Development and Neurodevelopmental Disorders: Investigating Physiology and Pathology to Gain Therapeutic Perspectives. Front. Cell. Neurosci. 2014, 8, 119. [Google Scholar] [CrossRef]
- Laricchiuta, D.; Saba, L.; De Bartolo, P.; Caioli, S.; Zona, C.; Petrosini, L. Maintenance of Aversive Memories Shown by Fear Extinction-Impaired Phenotypes Is Associated with Increased Activity in the Amygdaloid-Prefrontal Circuit. Sci. Rep. 2016, 6, 21205. [Google Scholar] [CrossRef] [Green Version]
- Laricchiuta, D.; Sciamanna, G.; Gimenez, J.; Termine, A.; Fabrizio, C.; Caioli, S.; Balsamo, F.; Panuccio, A.; De Bardi, M.; Saba, L.; et al. Optogenetic Stimulation of Prelimbic Pyramidal Neurons Maintains Fear Memories and Modulates Amygdala Pyramidal Neuron Transcriptome. Int. J. Mol. Sci. 2021, 22, 810. [Google Scholar] [CrossRef] [PubMed]
- Borgomaneri, S.; Battaglia, S.; Sciamanna, G.; Tortora, F.; Laricchiuta, D. Memories Are Not Written in Stone: Re-Writing Fear Memories by Means of Non-Invasive Brain Stimulation and Optogenetic Manipulations. Neurosci. Biobehav. Rev. 2021, 127, 334–352. [Google Scholar] [CrossRef] [PubMed]
- Tottenham, N.; Sheridan, M.A. A Review of Adversity, the Amygdala and the Hippocampus: A Consideration of Developmental Timing. Front. Hum. Neurosci. 2009, 3, 68. [Google Scholar] [CrossRef]
- Tottenham, N. Human Amygdala Development in the Absence of Species-Expected Caregiving. Dev. Psychobiol. 2012, 54, 598–611. [Google Scholar] [CrossRef]
- McEwen, B.S.; Stellar, E. Stress and the Individual. Mechanisms Leading to Disease. Arch. Intern. Med. 1993, 153, 2093–2101. [Google Scholar] [CrossRef]
- Lupien, S.J.; Maheu, F.; Tu, M.; Fiocco, A.; Schramek, T.E. The Effects of Stress and Stress Hormones on Human Cognition: Implications for the Field of Brain and Cognition. Brain Cogn. 2007, 65, 209–237. [Google Scholar] [CrossRef]
- Belelli, D.; Herd, M.B.; Mitchell, E.A.; Peden, D.R.; Vardy, A.W.; Gentet, L.; Lambert, J.J. Neuroactive Steroids and Inhibitory Neurotransmission: Mechanisms of Action and Physiological Relevance. Neuroscience 2006, 138, 821–829. [Google Scholar] [CrossRef]
- Rasmusson, A.M.; Pineles, S.L.; Brown, K.D.; Pinna, G. A Role for Deficits in GABAergic Neurosteroids and Their Metabolites with NMDA Receptor Antagonist Activity in the Pathophysiology of Posttraumatic Stress Disorder. J. Neuroendocrinol. 2022, 34, e13062. [Google Scholar] [CrossRef]
- Callaghan, B.L.; Tottenham, N. The Stress Acceleration Hypothesis: Effects of Early-Life Adversity on Emotion Circuits and Behavior. Curr. Opin. Behav. Sci. 2016, 7, 76–81. [Google Scholar] [CrossRef]
- Belsky, J. Early-Life Adversity Accelerates Child and Adolescent Development. Curr. Dir. Psychol. Sci. 2019, 28, 241–246. [Google Scholar] [CrossRef] [Green Version]
- Gee, D.G.; Gabard-Durnam, L.J.; Flannery, J.; Goff, B.; Humphreys, K.L.; Telzer, E.H.; Hare, T.A.; Bookheimer, S.Y.; Tottenham, N. Early Developmental Emergence of Human Amygdala-Prefrontal Connectivity after Maternal Deprivation. Proc. Natl. Acad. Sci. USA 2013, 110, 15638–15643. [Google Scholar] [CrossRef] [PubMed]
- Gee, D.G.; Humphreys, K.L.; Flannery, J.; Goff, B.; Telzer, E.H.; Shapiro, M.; Hare, T.A.; Bookheimer, S.Y.; Tottenham, N. A Developmental Shift from Positive to Negative Connectivity in Human Amygdala-Prefrontal Circuitry. J. Neurosci. Off. J. Soc. Neurosci. 2013, 33, 4584–4593. [Google Scholar] [CrossRef] [PubMed]
- Keding, T.J.; Herringa, R.J. Paradoxical Prefrontal–Amygdala Recruitment to Angry and Happy Expressions in Pediatric Posttraumatic Stress Disorder. Neuropsychopharmacology 2016, 41, 2903–2912. [Google Scholar] [CrossRef]
- Wu, M.; Kujawa, A.; Lu, L.H.; Fitzgerald, D.A.; Klumpp, H.; Fitzgerald, K.D.; Monk, C.S.; Phan, K.L. Age-Related Changes in Amygdala-Frontal Connectivity during Emotional Face Processing from Childhood into Young Adulthood. Hum. Brain Mapp. 2016, 37, 1684–1695. [Google Scholar] [CrossRef]
- Ono, M.; Kikusui, T.; Sasaki, N.; Ichikawa, M.; Mori, Y.; Murakami-Murofushi, K. Early Weaning Induces Anxiety and Precocious Myelination in the Anterior Part of the Basolateral Amygdala of Male Balb/c Mice. Neuroscience 2008, 156, 1103–1110. [Google Scholar] [CrossRef]
- Fani, N.; King, T.Z.; Brewster, R.; Srivastava, A.; Stevens, J.S.; Glover, E.M.; Norrholm, S.D.; Bradley, B.; Ressler, K.J.; Jovanovic, T. Fear-Potentiated Startle during Extinction Is Associated with White Matter Microstructure and Functional Connectivity. Cortex J. Devoted Study Nerv. Syst. Behav. 2015, 64, 249–259. [Google Scholar] [CrossRef]
- Tottenham, N.; Hare, T.A.; Quinn, B.T.; McCarry, T.W.; Nurse, M.; Gilhooly, T.; Millner, A.; Galvan, A.; Davidson, M.C.; Eigsti, I.-M.; et al. Prolonged Institutional Rearing Is Associated with Atypically Large Amygdala Volume and Difficulties in Emotion Regulation. Dev. Sci. 2010, 13, 46–61. [Google Scholar] [CrossRef]
- Troller-Renfree, S.V.; Barker, T.V.; Pine, D.S.; Fox, N.A. Cognitive Functioning in Socially Anxious Adults: Insights from the NIH Toolbox Cognition Battery. Front. Psychol. 2015, 6, 764. [Google Scholar] [CrossRef]
- McKenna, M.C.; Tildon, J.T.; Stevenson, J.H.; Hopkins, I.B. Energy Metabolism in Cortical Synaptic Terminals from Weanling and Mature Rat Brain: Evidence for Multiple Compartments of Tricarboxylic Acid Cycle Activity. Dev. Neurosci. 1994, 16, 291–300. [Google Scholar] [CrossRef]
- Kandel, E.R. Biology and the Future of Psychoanalysis: A New Intellectual Framework for Psychiatry Revisited. Am. J. Psychiatry 1999, 156, 505–524. [Google Scholar] [CrossRef]
- Kandel, E.R. The Molecular Biology of Memory Storage: A Dialog between Genes and Synapses. Biosci. Rep. 2004, 24, 475–522. [Google Scholar] [CrossRef]
- Cozolino, L. The Neuroscience of Psychotherapy: Healing the Social Brain; W. W. Norton & Company: New York, NY, USA, 2017; ISBN 978-0-393-71265-0. [Google Scholar]
- Mancia, M. Come Le Neuroscienze Possono Contribuire Alla Psicoanalisi; Springer: Milan, Italy, 2007. [Google Scholar]
- Viinamäki, H.; Kuikka, J.; Tiihonen, J.; Lehtonen, J. Change in Monoamine Transporter Density Related to Clinical Recovery: A Case-Control Study. Nord. J. Psychiatry 1998, 52, 39–44. [Google Scholar] [CrossRef]
- Gallese, V. The Manifold Nature of Interpersonal Relations: The Quest for a Common Mechanism. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2003, 358, 517–528. [Google Scholar] [CrossRef]
- Gallese, V. Intentional Attunement: A Neurophysiological Perspective on Social Cognition and Its Disruption in Autism. Brain Res. 2006, 1079, 15–24. [Google Scholar] [CrossRef] [PubMed]
- Stern, D.N. The Present Moment in Psychotherapy and Everyday Life; W. W. Norton & Company: New York, NY, USA, 2004; ISBN 978-0-393-06872-6. [Google Scholar]
- Stern, D.N.; Bruschweiler-Stern, N.; Harrison, A.M.; Lyons-Ruth, K.; Morgan, A.C.; Nahum, J.P.; Sander, L.; Tronick, E.Z. The Process of Therapeutic Change Involving Implicit Knowledge: Some Implications of Developmental Observations for Adult Psychotherapy. Infant Ment. Health J. 1998, 19, 300–308. [Google Scholar] [CrossRef]
- Stern, D.N.; Sander, L.W.; Nahum, J.P.; Harrison, A.M.; Lyons-Ruth, K.; Morgan, A.C.; Bruschweiler-Stern, N.; Tronick, E.Z. Non-Interpretive Mechanisms in Psychoanalytic Therapy. The “something More” than Interpretation. The Process of Change Study Group. Int. J. Psychoanal. 1998, 79, 903–921. [Google Scholar] [PubMed]
- Piovano, B. Comment on “Parent-Infant Psychotherapy and Psychoanalytic Treatment: Contradiction or Mutual Inspiration”? Int. Forum Psychoanal. 2003, 12, 259–264. [Google Scholar] [CrossRef]
- Piovano, B. Acting, Dreaming, Thinking in Adolescence: An Analysis from the Beginning to the End. Int. Forum Psychoanal. 2010, 19, 27–33. [Google Scholar] [CrossRef]
- Biondo, D. Fare Gruppo Con Gli Adolescenti; Franco Angeli: Milan, Italy, 2008. [Google Scholar]
- Biondo, D. Gruppo Evolutivo e Branco; Franco Angeli: Milan, Italy, 2020. [Google Scholar]
- Piovano, B. The Body in the Analytic Consulting Room. In When the Body Speaks; Routledge: London, UK, 2021. [Google Scholar]
- Guelfo, M. L’Insieme Multistrato. Gruppi, Masse ed Istituzioni tra Caos e Psicoanalisi; Armando: Roma, Italy, 2012. [Google Scholar]
- Van der Kolk, B. The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma; Viking Press: New York City, NY, USA, 2015. [Google Scholar]
- Crugnola, C.R. Attachment and Affects in the Analytical Dialogue. Riv. Psicoanal. 2015, 61, 865–890. [Google Scholar]
- Howell, E. Trauma and Dissociation-Informed Psychotherapy: Relational Healing and the Therapeutic Connection; W W Norton & Co. Inc.: New York, NY, USA, 2020; ISBN 978-0-393-71373-2. [Google Scholar]
- Hart, O.V.D.; Nijenhuis, E.R.S.; Steele, K. Haunted Self: Structural Dissociation and the Treatment of Chronic Traumatization, 1st ed.; W W Norton & Co. Inc.: New York, NY, USA, 2006; ISBN 978-0-393-70401-3. [Google Scholar]
- Bucci, W. Discourse Patterns in “Good” and Troubled Hours: A Multiple Code Interpretation. J. Am. Psychoanal. Assoc. 1997, 45, 155–187. [Google Scholar] [CrossRef]
- LeDoux, J.E. As Soon as There Was Life, There Was Danger: The Deep History of Survival Behaviours and the Shallower History of Consciousness. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2022, 377, 20210292. [Google Scholar] [CrossRef]
- Protopopescu, X.; Gerber, A.J. Bridging the Gap between Neuroscientific and Psychodynamic Models in Child and Adolescent Psychiatry. Child Adolesc. Psychiatr. Clin. N. Am. 2013, 22, 1–31. [Google Scholar] [CrossRef]
- Roque-Lopez, S.; Llanez-Anaya, E.; Álvarez-López, M.J.; Everts, M.; Fernández, D.; Davidson, R.J.; Kaliman, P. Mental Health Benefits of a 1-Week Intensive Multimodal Group Program for Adolescents with Multiple Adverse Childhood Experiences. Child Abuse Negl. 2021, 122, 105349. [Google Scholar] [CrossRef]
- Malchiodi, C. Expressive Therapies, 1st ed.; Guilford Press: New York, NY, USA, 2006; ISBN 978-1-59385-379-2. [Google Scholar]
- Gillies, D.; Maiocchi, L.; Bhandari, A.P.; Taylor, F.; Gray, C.; O’Brien, L. Psychological Therapies for Children and Adolescents Exposed to Trauma. Cochrane Database Syst. Rev. 2016, 10, CD012371. [Google Scholar] [CrossRef]
- Ortiz, R.; Sibinga, E.M. The Role of Mindfulness in Reducing the Adverse Effects of Childhood Stress and Trauma. Children 2017, 4, 16. [Google Scholar] [CrossRef]
- Jarero, I.; Artigas, L. The EMDR Integrative Group Treatment Protocol: EMDR Group Treatment for Early Intervention Following Critical Incidents. Eur. Rev. Appl. Psychol. 2012, 62, 219–222. [Google Scholar] [CrossRef]
- Silverstone, P.; Suen, V. Are Complex Multimodal Interventions the Best Treatments for Mental Health Disorders in Children and Youth? J. Child Adolesc. Behav. 2016, 4, 305–315. [Google Scholar] [CrossRef]
- Simkin, D.R.; Thatcher, R.W.; Lubar, J. Quantitative EEG and Neurofeedback in Children and Adolescents: Anxiety Disorders, Depressive Disorders, Comorbid Addiction and Attention-Deficit/Hyperactivity Disorder, and Brain Injury. Child Adolesc. Psychiatr. Clin. N. Am. 2014, 23, 427–464. [Google Scholar] [CrossRef]
- Lanius, R.A.; Vermetten, E.; Pain, C. (Eds.) The Impact of Early Life Trauma on Health and Disease: The Hidden Epidemic; Cambridge University Press: Cambridge, UK, 2010; ISBN 978-0-521-88026-8. [Google Scholar]
- Haine-Schlagel, R.; Brookman-Frazee, L.; Fettes, D.L.; Baker-Ericzén, M.; Garland, A.F. Therapist Focus on Parent Involvement in Community-Based Youth Psychotherapy. J. Child Fam. Stud. 2012, 21, 646–656. [Google Scholar] [CrossRef]
- Warshaw, M.G.; Fierman, E.; Pratt, L.; Hunt, M.; Yonkers, K.A.; Massion, A.O.; Keller, M.B. Quality of Life and Dissociation in Anxiety Disorder Patients with Histories of Trauma or PTSD. Am. J. Psychiatry 1993, 150, 1512–1516. [Google Scholar] [CrossRef]
- Chambers, R.A.; Potenza, M.N. Neurodevelopment, Impulsivity, and Adolescent Gambling. J. Gambl. Stud. 2003, 19, 53–84. [Google Scholar] [CrossRef]
- McLaughlin, K.A.; Green, J.G.; Hwang, I.; Sampson, N.A.; Zaslavsky, A.M.; Kessler, R.C. Intermittent Explosive Disorder in the National Comorbidity Survey Replication Adolescent Supplement. Arch. Gen. Psychiatry 2012, 69, 1131–1139. [Google Scholar] [CrossRef] [PubMed]
- De Bellis, M.D. Developmental Traumatology: A Contributory Mechanism for Alcohol and Substance Use Disorders. Psychoneuroendocrinology 2002, 27, 155–170. [Google Scholar] [CrossRef]
- Steinberg, L. A Social Neuroscience Perspective on Adolescent Risk-Taking. Dev. Rev. DR 2008, 28, 78–106. [Google Scholar] [CrossRef]
- Heleniak, C.; Jenness, J.L.; Stoep, A.V.; McCauley, E.; McLaughlin, K.A. Childhood Maltreatment Exposure and Disruptions in Emotion Regulation: A Transdiagnostic Pathway to Adolescent Internalizing and Externalizing Psychopathology. Cogn. Ther. Res. 2016, 40, 394–415. [Google Scholar] [CrossRef]
- Proctor, L.J.; Lewis, T.; Roesch, S.; Thompson, R.; Litrownik, A.J.; English, D.; Arria, A.M.; Isbell, P.; Dubowitz, H. Child Maltreatment and Age of Alcohol and Marijuana Initiation in High-Risk Youth. Addict. Behav. 2017, 75, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Darnell, D.; Flaster, A.; Hendricks, K.; Kerbrat, A.; Comtois, K.A. Adolescent Clinical Populations and Associations between Trauma and Behavioral and Emotional Problems. Psychol. Trauma Theory Res. Pract. Policy 2019, 11, 266–273. [Google Scholar] [CrossRef] [PubMed]
- Crone, E.A.; Dahl, R.E. Understanding Adolescence as a Period of Social-Affective Engagement and Goal Flexibility. Nat. Rev. Neurosci. 2012, 13, 636–650. [Google Scholar] [CrossRef]
- Ulmer-Yaniv, A.; Djalovski, A.; Yirmiya, K.; Halevi, G.; Zagoory-Sharon, O.; Feldman, R. Maternal Immune and Affiliative Biomarkers and Sensitive Parenting Mediate the Effects of Chronic Early Trauma on Child Anxiety. Psychol. Med. 2018, 48, 1020–1033. [Google Scholar] [CrossRef]
- Halevi, G.; Djalovski, A.; Vengrober, A.; Feldman, R. Risk and Resilience Trajectories in War-Exposed Children across the First Decade of Life. J. Child Psychol. Psychiatry 2016, 57, 1183–1193. [Google Scholar] [CrossRef]
- Halevi, G.; Djalovski, A.; Kanat-Maymon, Y.; Yirmiya, K.; Zagoory-Sharon, O.; Koren, L.; Feldman, R. The Social Transmission of Risk: Maternal Stress Physiology, Synchronous Parenting, and Well-Being Mediate the Effects of War Exposure on Child Psychopathology. J. Abnorm. Psychol. 2017, 126, 1087–1103. [Google Scholar] [CrossRef]
- Yirmiya, K.; Motsan, S.; Zagoory-Sharon, O.; Schonblum, A.; Koren, L.; Feldman, R. Continuity of Psychopathology v. Resilience across the Transition to Adolescence: Role of Hair Cortisol and Sensitive Caregiving. Psychol. Med. 2022, 1–12. [Google Scholar] [CrossRef]
- Gröger, N.; Matas, E.; Gos, T.; Lesse, A.; Poeggel, G.; Braun, K.; Bock, J. The Transgenerational Transmission of Childhood Adversity: Behavioral, Cellular, and Epigenetic Correlates. J. Neural Transm. 2016, 123, 1037–1052. [Google Scholar] [CrossRef]
- Sharma, V.; Sood, R.; Khlaifia, A.; Eslamizade, M.J.; Hung, T.-Y.; Lou, D.; Asgarihafshejani, A.; Lalzar, M.; Kiniry, S.J.; Stokes, M.P.; et al. EIF2α Controls Memory Consolidation via Excitatory and Somatostatin Neurons. Nature 2020, 586, 412–416. [Google Scholar] [CrossRef]
- Roeckner, A.R.; Oliver, K.I.; Lebois, L.A.M.; van Rooij, S.J.H.; Stevens, J.S. Neural Contributors to Trauma Resilience: A Review of Longitudinal Neuroimaging Studies. Transl. Psychiatry 2021, 11, 508. [Google Scholar] [CrossRef]
- Schore, A.N. Affect Regulation and the Repair of the Self, 1st ed.; W. W. Norton & Company: New York, NY, USA, 2003; ISBN 978-0-393-70407-5. [Google Scholar]
- Gillies, D.; Taylor, F.; Gray, C.; O’Brien, L.; D’Abrew, N. Psychological Therapies for the Treatment of Post-Traumatic Stress Disorder in Children and Adolescents. Cochrane Database Syst. Rev. 2012, 12, 1004–1116. [Google Scholar] [CrossRef]
- Steinert, C.; Munder, T.; Rabung, S.; Hoyer, J.; Leichsenring, F. Psychodynamic Therapy: As Efficacious as Other Empirically Supported Treatments? A Meta-Analysis Testing Equivalence of Outcomes. Am. J. Psychiatry 2017, 174, 943–953. [Google Scholar] [CrossRef]
- Patton, G.C.; Coffey, C.; Romaniuk, H.; Mackinnon, A.; Carlin, J.B.; Degenhardt, L.; Olsson, C.A.; Moran, P. The Prognosis of Common Mental Disorders in Adolescents: A 14-Year Prospective Cohort Study. Lancet 2014, 383, 1404–1411. [Google Scholar] [CrossRef]
- Johnson, D.; Dupuis, G.; Piche, J.; Clayborne, Z.; Colman, I. Adult Mental Health Outcomes of Adolescent Depression: A Systematic Review. Depress. Anxiety 2018, 35, 700–716. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Panuccio, A.; Biondo, D.; Picerni, E.; Genovesi, B.; Laricchiuta, D. Trauma-Related Internalizing and Externalizing Behaviors in Adolescence: A Bridge between Psychoanalysis and Neuroscience. Adolescents 2022, 2, 413-423. https://doi.org/10.3390/adolescents2040032
Panuccio A, Biondo D, Picerni E, Genovesi B, Laricchiuta D. Trauma-Related Internalizing and Externalizing Behaviors in Adolescence: A Bridge between Psychoanalysis and Neuroscience. Adolescents. 2022; 2(4):413-423. https://doi.org/10.3390/adolescents2040032
Chicago/Turabian StylePanuccio, Anna, Daniele Biondo, Eleonora Picerni, Benedetto Genovesi, and Daniela Laricchiuta. 2022. "Trauma-Related Internalizing and Externalizing Behaviors in Adolescence: A Bridge between Psychoanalysis and Neuroscience" Adolescents 2, no. 4: 413-423. https://doi.org/10.3390/adolescents2040032





