A Systematic Review Exploring the Psychosocial Factors Affecting Adolescent Access to HIV Treatment Services
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Setting
2.2. Information Source
2.3. Search Strategy
2.4. Quality of the Included Studies
2.5. Data Extraction
2.6. Data Analysis and Synthesis
2.7. Ethical Statement
| Article | 1. Aims | 2. Method | 3. Research Design | 4. Recruitment Strategy | 5. Data Collection | 6. Researcher Role | 7. Ethical Issues | 8. Data Analysis | 9. Rigorous Data Analysis | 10. Psychometric Properties | 11. Findings | 12. Value | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mavangira and Raniga [54] | Y | Y | Y | Y | Y | Y | Y | N/A | Y | N/A | Y | Y | 10 |
| van Wyk and Davids [55] | Y | Y | Y | Y | Y | Y | Y | N/A | Y | N/A | Y | Y | 10 |
| Boyes et al. [56] | Y | Y | N | Y | Y | N/A | Y | Y | Y | Y | Y | Y | 10 |
| Brittain et al. [57] | Y | Y | Y | Y | Y | N/A | Y | Y | Y | Y | Y | Y | 11 |
| Cluver, Pantelic, et al. [58] | Y | Y | Y | Y | Y | N/A | Y | Y | Y | Y | Y | Y | 11 |
| Cluver, Meinck, et al. [59] | Y | Y | Y | Y | Y | N/A | Y | Y | Y | Y | Y | Y | 11 |
| Cluver et al. [60] | Y | Y | Y | Y | Y | N/A | Y | Y | Y | Y | Y | Y | 11 |
| Coetzee et al. [61] | Y | Y | Y | Y | Y | N/A | Y | Y | Y | Y | Y | Y | 11 |
| Crowley et al. [62] | Y | Y | Y | Y | Y | N/A | Y | Y | Y | Y | Y | Y | 11 |
| Hoare et al. [63] | Y | Y | Y | Y | Y | N/A | Y | Y | Y | N | Y | Y | 10 |
| Kagee et al. [64] | Y | Y | Y | Y | Y | N/A | Y | Y | Y | Y | Y | Y | 11 |
| Kidman et al. [65] | Y | Y | N | Y | Y | N/A | Y | Y | Y | N | Y | Y | 9 |
| Kidman and Violari [66] | Y | Y | N | Y | Y | N/A | Y | Y | Y | N | Y | Y | 9 |
| Louw et al. [67] | Y | Y | Y | Y | Y | N/A | Y | Y | Y | N | Y | Y | 10 |
| Pantelic et al. [68] | Y | Y | Y | Y | Y | N/A | Y | Y | Y | Y | Y | Y | 11 |
| Pantelic et al. [69] | Y | Y | Y | Y | Y | N/A | Y | Y | Y | Y | Y | Y | 11 |
| Toska et al. [70] | Y | Y | N | Y | Y | N/A | Y | Y | Y | N | Y | Y | 9 |
| Woollett et al. [71] | Y | Y | Y | Y | Y | N/A | Y | Y | Y | Y | Y | Y | 11 |
3. Results
3.1. Descriptive Overview of the Included Studies
3.2. Quantitative Measures under Investigation
3.3. Psychometric Properties of the Quantitative Measures under Investigation
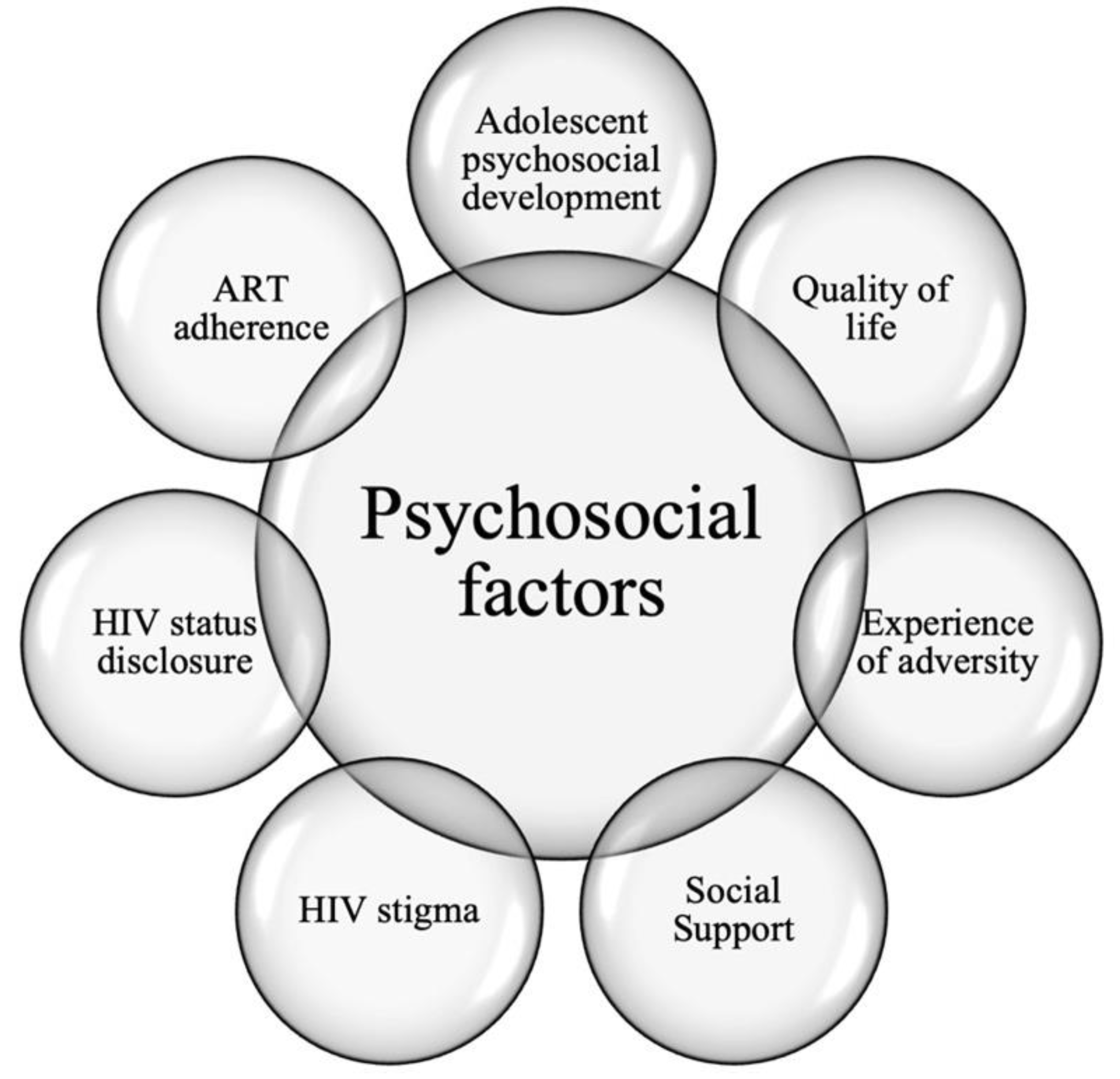
3.4. Thematic Synthesis of Findings across the Studies Included in the Sample
3.4.1. Theme 1: Adolescent Psychosocial Development
3.4.2. Theme 2: Quality of Life
3.4.3. Theme 3: Experience of Adversity
3.4.4. Theme 4: Social Support
3.4.5. Theme 5: HIV Stigma
3.4.6. Theme 6: HIV Status Disclosure
3.4.7. Theme 7: ART Adherence
4. Discussion
Implications for Practice, Theory, and Future Research
5. Conclusions
5.1. Limitations
5.2. Conclusions and Recommendations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| 1. Was there a clear statement of the aims of the research? |
| □ Yes □ Can’t tell □ No |
| Consider: What was the goal of the research? Why it was thought important? Its relevance |
| 2. Is a quantitative methodology appropriate? |
| □ Yes □ Can’t tell □ No |
| Consider: If the research seeks to examine a relationship between variables or comparison of groups. Is quantitative research the right methodology for addressing the research goal? |
| Were all the participants accounted for in the results and the conclusion? |
| □ Yes □ Can’t tell □ No |
| Is it worth continuing? |
| Detailed questions: |
| 3. Was the research design appropriate to address the aims of the research? |
| □ Yes □ Can’t tell □ No |
| Consider: If the researcher has justified the research design (E.g. have they discussed how they decided which method to use)? |
| 4. Was the recruitment strategy appropriate to the aims of the research? (Assess selection bias) |
| □ Yes □ Can’t tell □ No |
| Consider: If the researcher has explained how the participants were selected, Are the individuals selected to participate in this study likely to be representative of the target population? If there are any discussions around recruitment (e.g., why some people chose not to take part) |
| 5. Was the data collected in a way that addressed the research issue? |
| □ Yes □ Can’t tell □ No |
| Consider: If the setting for data collection was justified. If it is clear how data were collected. If the researcher has justified the methods chosen. If the researcher has made the methods explicit. Were data collection tools shown to be valid? Were data collection tools shown to be reliable? If methods were modified during the study. If so, has the researcher explained how and why? |
| 7. Have ethical issues been taken into consideration? |
| □ Yes □ Can’t tell □ No |
| Consider: If there are sufficient details of how the research was explained to participants for the reader to assess whether ethical standards were maintained. If the researcher has discussed issues raised by the study (e.g., issues around informed consent, anonymity, and confidentiality or how they have handled the effects of the study on the participants during and after the study). If approval has been sought from the ethics committee |
| 8. Was the correct statistical technique used to analyse the data |
| □ Yes □ Can’t tell □ No |
| Consider: Was descriptive data provided? Was the sample size large enough for the statistical technique carried out? Was basic assumptions of the statistical test utilised met? Were both significant and insignificant results reported? Did the statistical technique used effectively answer the research question? |
| 9. Was the data analysis sufficiently rigorous? |
| □ Yes □ Can’t tell □ No |
| Consider: If there is an in-depth description of the analysis process. Were the statistical methods appropriate for the study design? If sufficient data are presented to support the findings? To what extent contradictory data are taken into account? Were potential sources of bias discussed? |
| 10. Were psychometric properties discussed? |
| □ Yes □ Can’t tell □ No |
| Consider: were reliability and validity of the instruments used discussed or analysed |
| 11. Is there a clear statement of findings? |
| □ Yes □ Can’t tell □ No |
| Consider: If the findings are explicit. If there is adequate discussion of the evidence both for and against the researcher’s arguments. If the findings are discussed in relation to the original research question |
| 12. How valuable is the research? |
| Consider: If the researcher discusses the contribution the study makes to existing knowledge or understanding e.g. do they consider the findings in relation to current practice or policy? Or relevant research-based literature? If they identify new areas where research is necessary? If the researchers have discussed whether or how the findings can be transferred to other populations or considered other ways, the research may be used |
Appendix B






References
- Roser, M.; Ritchie, H. HIV/AIDS. Our World in Data. 2020. Available online: https://ourworldindata.org/hiv-aids (accessed on 30 April 2021).
- Close, K.; Rigamonti, A.X. Psychosocial aspects of HIV/AIDS: Children and adolescents. In HIV Curriculum: For the Health Professional, 4th ed.; Baylor International Pediatric AIDS Initiative, Ed.; Baylor College of Medicine: Houston, TX, USA, 2010; pp. 319–333. Available online: https://bipai.org/sites/bipai/files/HIV_Curriculum_Web.pdf (accessed on 30 April 2021).
- Staden, Q.; Laurenzi, C.A.; Toska, E. Two years after lockdown: Reviewing the effects of COVID-19 on health services and support for adolescents living with HIV in South Africa. J. Int. AIDS Soc. 2022, 25, e25904. [Google Scholar] [CrossRef] [PubMed]
- Ashaba, S.; Cooper-Vince, C.; Vořechovská, D.; Maling, S.; Rukundo, G.Z.; Akena, D.; Tsai, A.C. Development and validation of a 20-item screening scale to detect major depressive disorder among adolescents with HIV in rural Uganda: A mixed-methods study. SSM-Popul. Health 2019, 7, 100332. [Google Scholar] [CrossRef] [PubMed]
- Evans, D.; Menezes, C.; Mahomed, K.; Macdonald, P.; Untiedt, S.; Levin, L.; Jaffray, I.; Bhana, N.; Firnhaber, C.; Maskew, M. Treatment Outcomes of HIV-Infected Adolescents Attending Public-Sector HIV Clinics Across Gauteng and Mpumalanga, South Africa. AIDS Res. Hum. Retrovir. 2013, 29, 892–900. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, M.H.; Mazenga, A.C.; Yu, X.; Devandra, A.; Nguyen, C.; Ahmed, S.; Kazembe, P.N.; Sharp, C. Factors associated with depression among adolescents living with HIV in Malawi. BMC Psychiatry 2015, 15, 264. [Google Scholar] [CrossRef] [Green Version]
- Maskew, M.; Bor, J.; MacLeod, W.; Carmona, S.; Sherman, G.G.; Fox, M.P. Adolescent HIV treatment in South Africa’s national HIV programme: A retrospective cohort study. Lancet HIV 2019, 6, e760–e768. [Google Scholar] [CrossRef]
- Vreeman, R.C.; McCoy, B.M.; Lee, S. Mental health challenges among adolescents living with HIV. J. Int. AIDS Soc. 2017, 20 (Suppl. S3), 21497. [Google Scholar] [CrossRef]
- Kemigisha, E.; Zanoni, B.; Bruce, K.; Menjivar, R.; Kadengye, D.; Atwine, D.; Rukundo, G.Z. Prevalence of depressive symptoms and associated factors among adolescents living with HIV/AIDS in South Western Uganda. AIDS Care 2019, 31, 1297–1303. [Google Scholar] [CrossRef]
- Toska, E.; Cluver, L.; Orkin, M.; Bains, A.; Sherr, L.; Berezin, M.; Gulaid, L. Screening and supporting through schools: Educational experiences and needs of adolescents living with HIV in a South African cohort. BMC Public Health 2019, 19, 272. [Google Scholar] [CrossRef]
- West, N.; Schwartz, S.; Mudavanhu, M.; Hanrahan, C.; France, H.; Nel, J.; Mutunga, L.; Bernhardt, S.; Bassett, J.; Van Rie, A. Mental health in South African adolescents living with HIV. AIDS Care 2019, 31, 117–124. [Google Scholar] [CrossRef]
- Collins, P.Y.; Velloza, J.; Concepcion, T.; Oseso, L.; Chwastiak, L.; Kemp, C.G.; Simoni, J.; Wagenaar, B.H. Intervening for HIV prevention and mental health: A review of global literature. J. Int. AIDS Soc. 2021, 24, e25710. [Google Scholar] [CrossRef]
- Jaspan, H.B.; Li, R.; Johnson, L.; Bekker, L.-G. The emerging need for adolescent-focused HIV care in South Africa. South Afr. J. HIV Med. 2009, 10, 9. [Google Scholar] [CrossRef]
- Marfatia, Y.; Naswa, S. Adolescent HIV/AIDS: Issues and challenges. Indian J. Sex. Transm. Dis. AIDS 2010, 31, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Koenig, L.J.; Nesheim, S.; Abramowitz, S. Adolescents with perinatally acquired HIV: Emerging behavioral and health needs for long-term survivors. Curr. Opin. Obstet. Gynecol. 2011, 23, 321–327. [Google Scholar] [CrossRef] [PubMed]
- Whetten, K.; Reif, S.; Whetten, R.; Murphy-McMillan, L.K. Trauma, Mental Health, Distrust, and Stigma Among HIV-Positive Persons: Implications for Effective Care. Psychosom. Med. 2008, 70, 531–538. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anderson, K.; Muloiwa, R.; Davies, M.-A. Long-term outcomes in perinatally HIV-infected adolescents and young adults on antiretroviral therapy: A review of South African and global literature. Afr. J. AIDS Res. 2020, 19, 1–12. [Google Scholar] [CrossRef]
- Sohn, A.H.; Hazra, R. The changing epidemiology of the global paediatric HIV epidemic: Keeping track of perinatally HIV-infected adolescents. J. Int. AIDS Soc. 2013, 16, 18555. [Google Scholar] [CrossRef] [PubMed]
- Sherr, L.; Cluver, L.D.; Toska, E.; He, E. Differing psychological vulnerabilities among behaviourally and perinatally HIV infected adolescents in South Africa—Implications for targeted health service provision. AIDS Care 2018, 30, 92–101. [Google Scholar] [CrossRef]
- Gellman, M.D.; Turner, J.R. (Eds.) Encyclopedia of Behavioral Medicine, 1st ed.; Springer: Berlin, Germany, 2013; Available online: https://link.springer.com/referencework/10.1007/978-1-4419-1005-9 (accessed on 30 April 2021).
- MacLeod, J. Psychosocial factors and public health: A suitable case for treatment? J. Epidemiol. Community Health 2003, 57, 565–570. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Programme on Mental Health: WHOQOL User Manual. World Health Organization. 2012, pp. 1–106. Available online: https://apps.who.int/iris/bitstream/handle/10665/77932/WHO_HIS_HSI_Rev.2012.03_eng.pdf?sequence=1&isAllowed=y&ua=1 (accessed on 30 April 2021).
- Lutgendorf, S.; Antoni, M.H.; Schneiderman, N.; Fletcher, M.A. Psychosocial counseling to improve quality of life in HIV infection. Patient Educ. Couns. 1994, 24, 217–235. [Google Scholar] [CrossRef]
- Vu, G.T.; Tran, B.X.; Hoang, C.L.; Hall, B.J.; Phan, H.T.; Ha, G.H.; Latkin, C.A.; Ho, C.S.; Ho, R.C. Global Research on Quality of Life of Patients with HIV/AIDS: Is It Socio-Culturally Addressed? (GAPRESEARCH). Int. J. Environ. Res. Public Health 2020, 17, 2127. [Google Scholar] [CrossRef]
- Variava, T.; Graham, T. Mental Health Considerations in HIV Research Published in South Africa. 2021; Manuscript submitted for publication. [Google Scholar]
- Variava, T.; Graham, T. The National Response to the HIV Epidemic in Post-Apartheid South Africa: Implications for Mental Health Care. 2021; Manuscript submitted for publication. [Google Scholar]
- Coovadia, H.; Jewkes, R.; Barron, P.; Sanders, D.; McIntyre, D. The health and health system of South Africa: Historical roots of current public health challenges. Lancet 2009, 374, 817–834. [Google Scholar] [CrossRef] [PubMed]
- Spedding, M.F.; Stein, D.J.; Sorsdahl, K. Task-shifting psychosocial interventions in Public Mental Health: A review of the evidence in the South African context. S. Afr. Health Rev. 2014, 2014, 73–87. [Google Scholar]
- Cooper, D.; De Lannoy, A.; Rule, C. Youth health and well-being: Why it matters? S. Afr. Child Gauge 2015, 60–68. Available online: http://hdl.handle.net/20.500.11910/1739 (accessed on 30 April 2021).
- Kung, T.H.; Wallace, M.; Snyder, K.L.; Robson, V.K.; Mabud, T.S.; Kalombo, C.D.; Bekker, L.-G. South African healthcare provider perspectives on transitioning adolescents into adult HIV care. S. Afr. Med. J. 2016, 106, 804–808. [Google Scholar] [CrossRef]
- National Department of Health. National Adolescent & Youth Health Policy 2017; National Department of Health: Pretoria, South Africa, 2017; pp. 1–12.
- Geary, R.S.; Gómez-Olivé, F.X.; Kahn, K.; Tollman, S.; Norris, S.A. Barriers to and facilitators of the provision of a youth-friendly health services programme in rural South Africa. BMC Health Serv. Res. 2014, 14, 259. [Google Scholar] [CrossRef] [Green Version]
- James, S.; Pisa, P.T.; Imrie, J.; Beery, M.P.; Martin, C.; Skosana, C.; Delany-Moretlwe, S. Assessment of adolescent and youth friendly services in primary healthcare facilities in two provinces in South Africa. BMC Health Serv. Res. 2018, 18, 809. [Google Scholar] [CrossRef] [Green Version]
- Nkosi, B.; Seeley, J.; Ngwenya, N.; Mchunu, S.L.; Gumede, D.; Ferguson, J.; Doyle, A.M. Exploring adolescents and young people’s candidacy for utilising health services in a rural district, South Africa. BMC Health Serv. Res. 2019, 19, 195. [Google Scholar] [CrossRef] [Green Version]
- Shabani, O.; Moleki, M.M.; Thupayagale-Tshweneagae, G.G. Individual determinants associated with utilisation of sexual and reproductive health care services for HIV and AIDS prevention by male adolescents. Curationis 2018, 41, 6. [Google Scholar] [CrossRef]
- Schneider, M.; Baron, E.; Breuer, E.; Docrat, S.; Honikman, S.; Onah, M.; Sorsdahl, K.; Van der Westhuizen, C.; Lund, C.; Kagee, A.; et al. Integrating mental health into South Africa’s health system: Current status and way forward. S. Afr. Health Rev. 2016, 2016, 153–163. [Google Scholar]
- South African Government. Child Care Amendment Act of 1996. South African Government. 1996. Available online: https://www.gov.za/sites/default/files/gcis_document/201409/act96of1996.pdf (accessed on 30 April 2021).
- South African Government. Mental Health Care Act 17 of 2002. South African Government. 2002. Available online: https://www.gov.za/documents/mental-health-care-act (accessed on 30 April 2021).
- South African Government. National Mental Health Policy Framework and Strategic Plan 2013–2020. Health-e. 23 October 2014. Available online: https://health-e.org.za/2014/10/23/policy-national-mental-health-policy-framework-strategic-plan-2013-2020/ (accessed on 30 April 2021).
- Docrat, S.; Besada, D.; Cleary, S.; Daviaud, E.; Lund, C. Mental health system costs, resources and constraints in South Africa: A national survey. Health Policy Plan. 2019, 34, 706–719. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Mental Health Atlas; World Health Organization: Geneva, Switzerland, 2017; pp. 1–72. [Google Scholar]
- Burns, J.K. Mental health advocacy—Lessons from HIV activism. S. Afr. Med. J. 2010, 100, 654. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Naidoo, P.; Nyembezi, A.; Thomas, E.; Lachman, A.; Kagee, A. Perceived barriers and facilitators for healthy behaviours among parents of adolescents receiving mental health care in a public hospital in Cape Town, South Africa: A qualitative study. J. Child Adolesc. Ment. Health 2019, 31, 39–50. [Google Scholar] [CrossRef] [PubMed]
- Petersen, I.; Lund, C. Mental health service delivery in South Africa from 2000 to 2010: One step forward, one step back. S. Afr. Med. J. 2011, 101, 751–757. [Google Scholar]
- Schierenbeck, I.; Johansson, P.; Andersson, L.; Van Rooyen, D. Barriers to accessing and receiving mental health care in Eastern Cape, South Africa. Health Hum. Rights 2013, 15, 110–123. [Google Scholar] [PubMed]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (prisma-p) 2015 statement. Syst. Rev. 2015, 4, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cooke, A.; Smith, D.; Booth, A. Beyond PICO: The SPIDER tool for qualitative evidence synthesis. Qual. Health Res. 2012, 22, 1435–1443. [Google Scholar] [CrossRef]
- Methley, A.M.; Campbell, S.; Chew-Graham, C.; McNally, R.; Cheraghi-Sohi, S. PICO, PICOS and SPIDER: A comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv. Res. 2014, 14, 579. [Google Scholar] [CrossRef] [Green Version]
- Laher, S.; Hasseem, T. Doing systematic reviews in psychology. S. Afr. J. Psychol. 2022; in press. [Google Scholar] [CrossRef]
- Boland, A.; Cherry, G.; Dickson, R. Doing a Systematic Review: A Student’s Guide; SAGE: Thousand Oaks, CA, USA, 2017. [Google Scholar]
- Data Extraction Template. 268394 Bytes. Available online: https://opal.latrobe.edu.au/articles/journal_contribution/Data_extraction_template/6818852 (accessed on 24 August 2022). [CrossRef]
- Thomas, J.; Harden, A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med. Res. Methodol. 2008, 8, 45. [Google Scholar] [CrossRef] [Green Version]
- Braun, V.; Clarke, V.; Hayfield, N.; Terry, G. Thematic Analysis. In Handbook of Research Methods in Health Social Sciences; Liamputtong, P., Ed.; Springer: Singapore, 2019; pp. 843–860. [Google Scholar] [CrossRef]
- Mavangira, V.; Raniga, T. Psycho-Social Experiences of Perinatally HIV-Infected Adolescents Residing in Child and Youth Care Centres in South Africa. Soc. Work. Werk 2015, 50, 421–433. [Google Scholar] [CrossRef] [Green Version]
- Van Wyk, B.E.; Davids, L.-A.C. Challenges to HIV treatment adherence amongst adolescents in a low socio-economic setting in Cape Town. South Afr. J. HIV Med. 2019, 20, 1002. [Google Scholar] [CrossRef] [Green Version]
- Boyes, M.E.; Cluver, L.D.; Meinck, F.; Casale, M.; Newnham, E. Mental health in South African adolescents living with HIV: Correlates of internalising and externalising symptoms. AIDS Care 2018, 31, 95–104. [Google Scholar] [CrossRef] [PubMed]
- Brittain, K.; Myer, L.; Phillips, N.; Cluver, L.D.; Zar, H.J.; Stein, D.J.; Hoare, J. Behavioural health risks during early adolescence among perinatally HIV-infected South African adolescents and same-age, HIV-uninfected peers. AIDS Care 2019, 31, 131–140. [Google Scholar] [CrossRef] [PubMed]
- Cluver, L.; Pantelic, M.; Orkin, M.; Toska, E.; Medley, S.; Sherr, L. Sustainable Survival for adolescents living with HIV: Do SDG-aligned provisions reduce potential mortality risk? J. Int. AIDS Soc. 2018, 21, e25056. [Google Scholar] [CrossRef] [PubMed]
- Cluver, L.; Meinck, F.; Toska, E.; Orkin, F.M.; Hodes, R.J.; Sherr, L. Multitype violence exposures and adolescent antiretroviral nonadherence in South Africa. Aids 2018, 32, 975–983. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cluver, L.D.; Orkin, F.M.; Campeau, L.; Toska, E.; Webb, D.; Carlqvist, A.; Sherr, L. Improving lives by accelerating progress towards the UN Sustainable Development Goals for adolescents living with HIV: A prospective cohort study. Lancet Child Adolesc. Health 2019, 3, 245–254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coetzee, B.J.; Loades, M.E.; Du Toit, S.; Kagee, A. Correlates of Fatigue Among South African Adolescents Living with HIV and Receiving Antiretroviral Therapy. AIDS Behav. 2019, 23, 602–608. [Google Scholar] [CrossRef]
- Crowley, T.; Van Der Merwe, A.; Kidd, M.; Skinner, D. Adolescent human immunodeficiency virus self-management: Associations with treatment adherence, viral suppression, sexual risk behaviours and health-related quality of life. South. Afr. J. HIV Med. 2020, 21, 11. [Google Scholar] [CrossRef]
- Hoare, J.; Phillips, N.; Brittain, K.; Myer, L.; Zar, H.J.; Stein, D.J. Mental Health and Functional Competence in the Cape Town Adolescent Antiretroviral Cohort. Am. J. Ther. 2019, 81, e109–e116. [Google Scholar] [CrossRef]
- Kagee, A.; Coetzee, B.; Du Toit, S.; Loades, M.E. Psychosocial predictors of quality of life among South Africa adolescents receiving antiretroviral therapy. Qual. Life Res. 2019, 28, 57–65. [Google Scholar] [CrossRef]
- Kidman, R.; Nachman, S.; Dietrich, J.; Liberty, A.; Violari, A. Childhood adversity increases the risk of onward transmission from perinatal HIV-infected adolescents and youth in South Africa. Child Abus. Negl. 2018, 79, 98–106. [Google Scholar] [CrossRef] [PubMed]
- Kidman, R.; Violari, A. Dating Violence Against HIV-Infected Youth in South Africa: Associations with Sexual Risk Behavior, Medication Adherence, and Mental Health. Am. J. Ther. 2018, 77, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Louw, K.-A.; Ipser, J.; Phillips, N.; Hoare, J. Correlates of emotional and behavioural problems in children with perinatally acquired HIV in Cape Town, South Africa. AIDS Care 2016, 28, 842–850. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pantelic, M.; Boyes, M.; Cluver, L.; Meinck, F. HIV, violence, blame and shame: Pathways of risk to internalized HIV stigma among South African adolescents living with HIV. J. Int. AIDS Soc. 2017, 20, 21771–21779. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pantelic, M.; Casale, M.; Cluver, L.; Toska, E.; Moshabela, M. Multiple forms of discrimination and internalized stigma compromise retention in HIV care among adolescents: Findings from a South African cohort. J. Int. AIDS Soc. 2020, 23, e25488. [Google Scholar] [CrossRef] [PubMed]
- Toska, E.; Cluver, L.D.; Boyes, M.E.; Isaacsohn, M.; Hodes, R.; Sherr, L. School, Supervision and Adolescent-Sensitive Clinic Care: Combination Social Protection and Reduced Unprotected Sex Among HIV-Positive Adolescents in South Africa. AIDS Behav. 2017, 21, 2746–2759. [Google Scholar] [CrossRef] [Green Version]
- Woollett, N.; Cluver, L.; Bandeira, M.; Brahmbhatt, H. Identifying risks for mental health problems in HIV positive adolescents accessing HIV treatment in Johannesburg. J. Child Adolesc. Ment. Health 2017, 29, 11–26. [Google Scholar] [CrossRef]
- Fatusi, A.O.; Hindin, M.J. Adolescents and youth in developing countries: Health and development issues in context. J. Adolesc. 2010, 33, 499–508. [Google Scholar] [CrossRef]
- Goga, A.; Slogrove, A.; Scrymgeour-Wedderburn, C.; Feucht, U.; Wessels, J.; Ramokolo, V.; Bhana, A.; Du Plessis, N.; Green, R.J.; Pillay, Y.; et al. The impact of health programmes to prevent vertical transmission of HIV. Advances, emerging health challenges and research priorities for children exposed to or living with HIV: Perspectives from South Africa. S. Afr. Med. J. 2019, 109, 77–82. [Google Scholar] [CrossRef] [Green Version]
- A Hussen, S.; Chahroudi, A.; Boylan, A.; Camacho-Gonzalez, A.F.; Hackett, S.; Chakraborty, R. Transition of youth living with HIV from pediatric to adult-oriented healthcare: A review of the literature. Futur. Virol. 2014, 9, 921–929. [Google Scholar] [CrossRef] [Green Version]
- Slogrove, A.L.; Sohn, A.H. The global epidemiology of adolescents living with HIV. Curr. Opin. HIV AIDS 2018, 13, 170–178. [Google Scholar] [CrossRef] [PubMed]

| Article | Study Design | Sample Size | Sample Age Range | Sample Gender | Setting |
|---|---|---|---|---|---|
| Mavangira and Raniga [54] | Qualitative, exploratory, cross-sectional, descriptive, interpretive | n = 8 | 14–17 years old | Female and Male | Child and youth care centre in Gauteng |
| Van Wyk and Davids [55] | Qualitative, exploratory, cross-sectional | n = 15 | 10–19 years old | Female and Male | 5 paediatric facilities in the Western Cape providing adolescent antiretroviral therapy |
| Boyes et al. [56] | Quantitative, exploratory, cross-sectional, descriptive, correlational | n = 1060 | 10–19 years old | Female and Male | 53 facilities in the Eastern Cape providing adolescent antiretroviral therapy |
| Brittain et al. [57] | Quantitative, exploratory, cross-sectional, descriptive, correlational, cohort | n = 616 | 9–14 years old | Female | Seven facilities in the Western Cape providing adolescent antiretroviral therapy |
| Cluver, Pantelic, et al. [58] | Quantitative, exploratory, cross-sectional, descriptive, correlational | n = 1060 | 10–19 years old | Female and Male | 53 facilities in the Eastern Cape providing adolescent antiretroviral therapy |
| Cluver, Meinck, et al. [59] | Quantitative, exploratory, cross-sectional, descriptive, correlational | n = 1060 | 10–19 years old | Female and Male | 53 facilities in the Eastern Cape providing adolescent antiretroviral therapy |
| Cluver et al. [60] | Quantitative, exploratory, longitudinal, descriptive, correlational | n = 1063 | 10–19 years old | Female and Male | 52 facilities in the Eastern Cape providing adolescent antiretroviral therapy |
| Coetzee et al. [61] | Quantitative, exploratory, cross-sectional, descriptive, correlational | n = 134 | 11–18 years old | Female and Male | Facilities in the Western Cape providing adolescent antiretroviral therapy |
| Crowley et al. [62] | Quantitative, exploratory, cross-sectional, descriptive, correlational | n = 385 | 13–18 years old | Female and Male | 11 facilities in the Western Cape providing adolescent antiretroviral therapy |
| Hoare et al. [63] | Quantitative, exploratory, longitudinal, descriptive, correlational, cohort | n = 232 | 9–11 years old | Female and Male | Facilities in the Western Cape providing adolescent antiretroviral therapy |
| Kagee et al. [64] | Quantitative, exploratory, cross-sectional, descriptive, correlational | n = 134 | 11–18 years old | Female and Male | Facilities in the Western Cape providing adolescent antiretroviral therapy |
| Kidman et al. [65] | Quantitative, exploratory, cross-sectional, descriptive, correlational | n = 250 | 13–24 years old | Female and Male | Paediatric facility in Gauteng providing adolescent antiretroviral therapy |
| Kidman and Violari [66] | Quantitative, exploratory, cross-sectional, descriptive, correlational | n = 129 | 13–24 years old | Female | Paediatric facility in Gauteng providing adolescent antiretroviral therapy |
| Louw et al. [67] | Quantitative, exploratory, cross-sectional, descriptive, correlational | n = 108 | 6–16 years old | Female and Male | Facilities in the Western Cape providing adolescent antiretroviral therapy |
| Pantelic et al. [68] | Quantitative, exploratory, cross-sectional, descriptive, correlational | n = 1060 | 10–19 years old | Female and Male | 53 public health facilities in the Eastern Cape providing adolescent antiretroviral therapy |
| Pantelic et al. [69] | Quantitative, exploratory, longitudinal, descriptive, correlational | n = 1059 | 10–19 years old | Female and Male | 53 public health facilities in the Eastern Cape providing adolescent antiretroviral therapy |
| Toska et al. [70] | Exploratory, cross-sectional, descriptive, correlational | n = 1060 | 10–19 years old | Female and Male | 53 public health facilities in the Eastern Cape providing adolescent antiretroviral therapy |
| Woollett et al. [71] | Quantitative, exploratory, cross-sectional, descriptive, correlational | n = 343 | 13–19 years old | Female and Male | Primary healthcare clinic in Gauteng providing adolescent antiretroviral therapy |
| Article | Psychosocial Constructs Investigated | Measures Used |
|---|---|---|
| Mavangira and Raniga [54] |
|
|
| Van Wyk and Davids [55] |
|
|
| Boyes et al. [56] |
|
|
| Brittain et al. [57] |
|
|
| Cluver, Pantelic, et al. [58] |
|
|
| Cluver, Meinck, et al. [59] |
|
|
| Cluver et al. [60] |
|
|
| Coetzee et al. [61] |
|
|
| Crowley et al. [62] |
|
|
| Hoare et al. [63] |
|
|
| Kagee et al. [64] |
|
|
| Kidman et al. [65] |
|
|
| Kidman and Violari [66] |
|
|
| Louw et al. [67] |
|
|
| Pantelic et al. [68] |
|
|
| Pantelic et al. [69] |
|
|
| Toska et al. [70] |
|
|
| Woollett et al. [71] |
|
|
| Themes | Sub-Themes |
|---|---|
| Adolescent psychosocial development |
|
| Quality of life |
|
| Experience of adversity |
|
| Access to social support |
|
| Experience of HIV stigma |
|
| ART adherence |
|
| HIV status disclosure |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Variava, T.; Watermeyer, J. A Systematic Review Exploring the Psychosocial Factors Affecting Adolescent Access to HIV Treatment Services. Adolescents 2023, 3, 10-40. https://doi.org/10.3390/adolescents3010002
Variava T, Watermeyer J. A Systematic Review Exploring the Psychosocial Factors Affecting Adolescent Access to HIV Treatment Services. Adolescents. 2023; 3(1):10-40. https://doi.org/10.3390/adolescents3010002
Chicago/Turabian StyleVariava, Tarique, and Jennifer Watermeyer. 2023. "A Systematic Review Exploring the Psychosocial Factors Affecting Adolescent Access to HIV Treatment Services" Adolescents 3, no. 1: 10-40. https://doi.org/10.3390/adolescents3010002
APA StyleVariava, T., & Watermeyer, J. (2023). A Systematic Review Exploring the Psychosocial Factors Affecting Adolescent Access to HIV Treatment Services. Adolescents, 3(1), 10-40. https://doi.org/10.3390/adolescents3010002






