Investigating Kinematics and Electromyography Changes in Manual Handling Tasks with an Active Lumbar Exoskeleton
Abstract
:1. Introduction
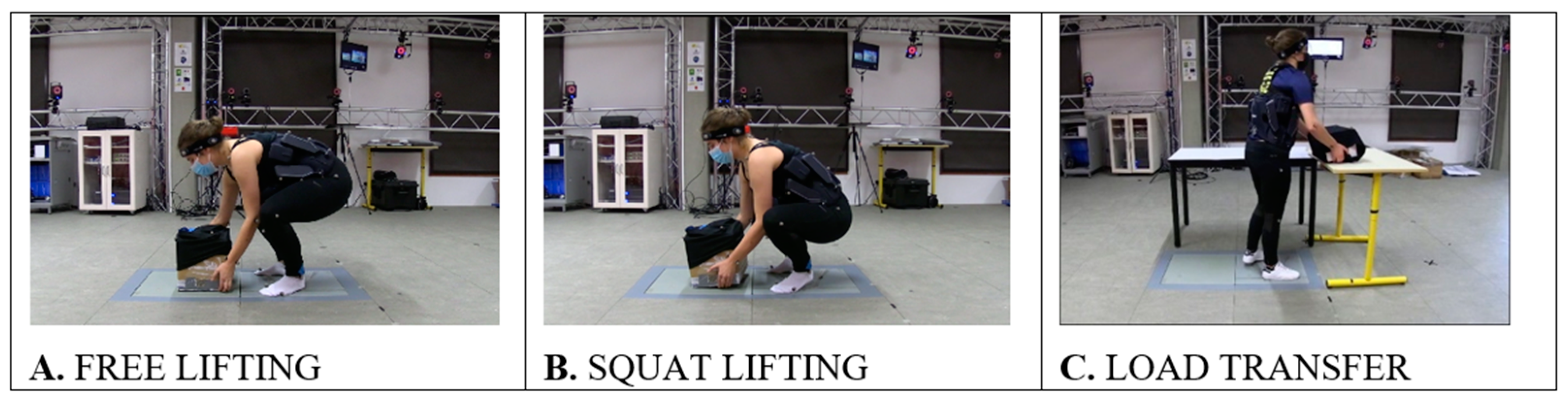
2. Materials and Methods
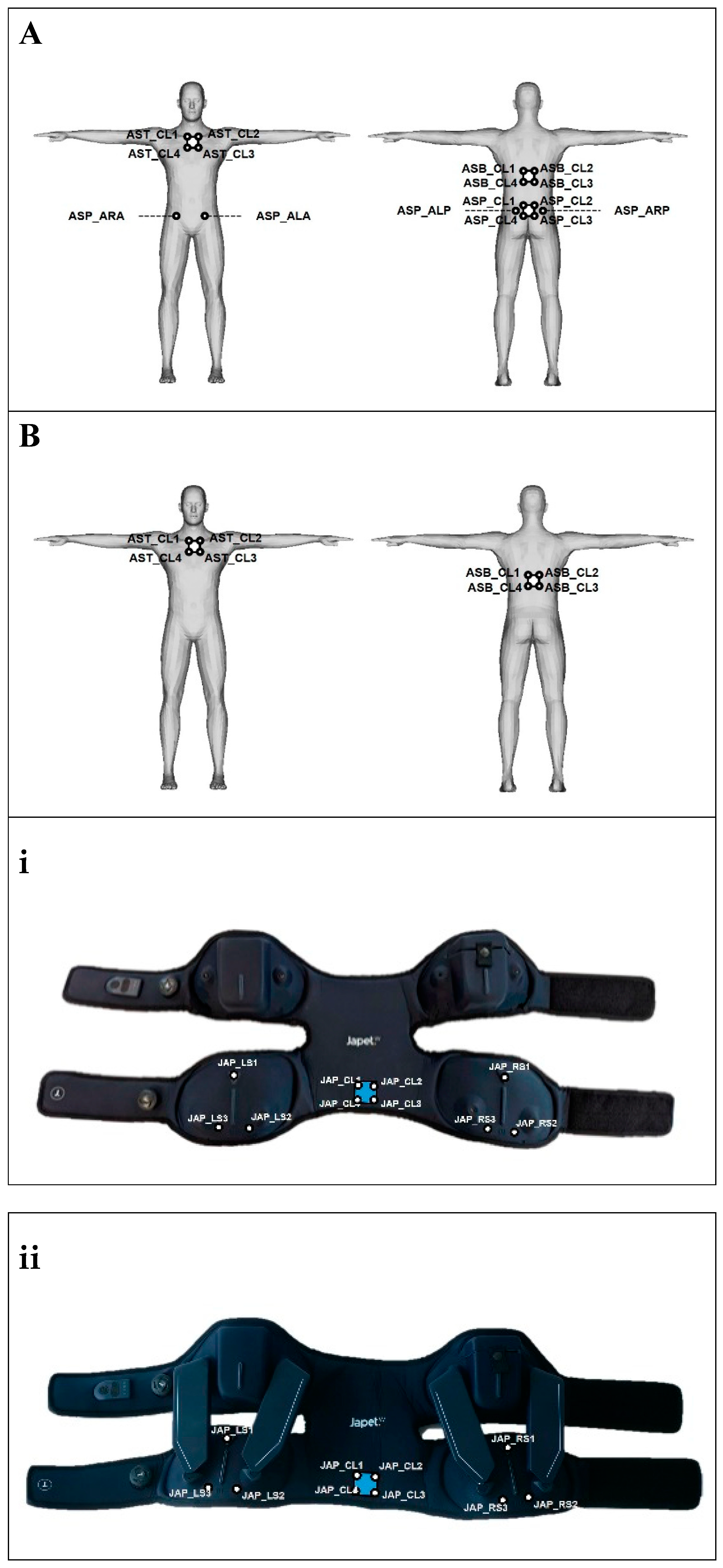
2.1. Exoskeleton
2.2. Belt
2.3. Population
2.4. Instrumented Motion Capture Session and Data Pre-Processing
2.5. Data Analysis
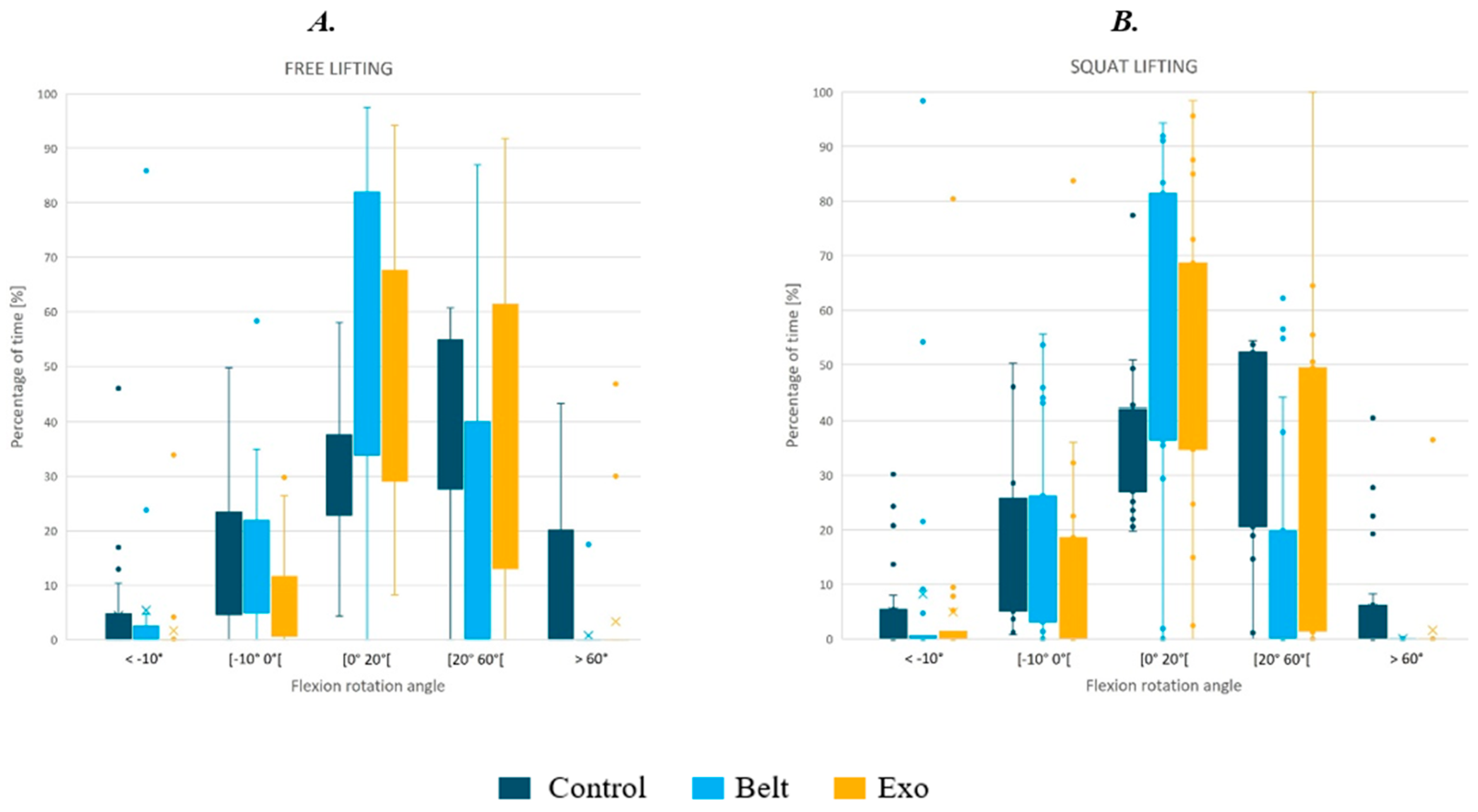
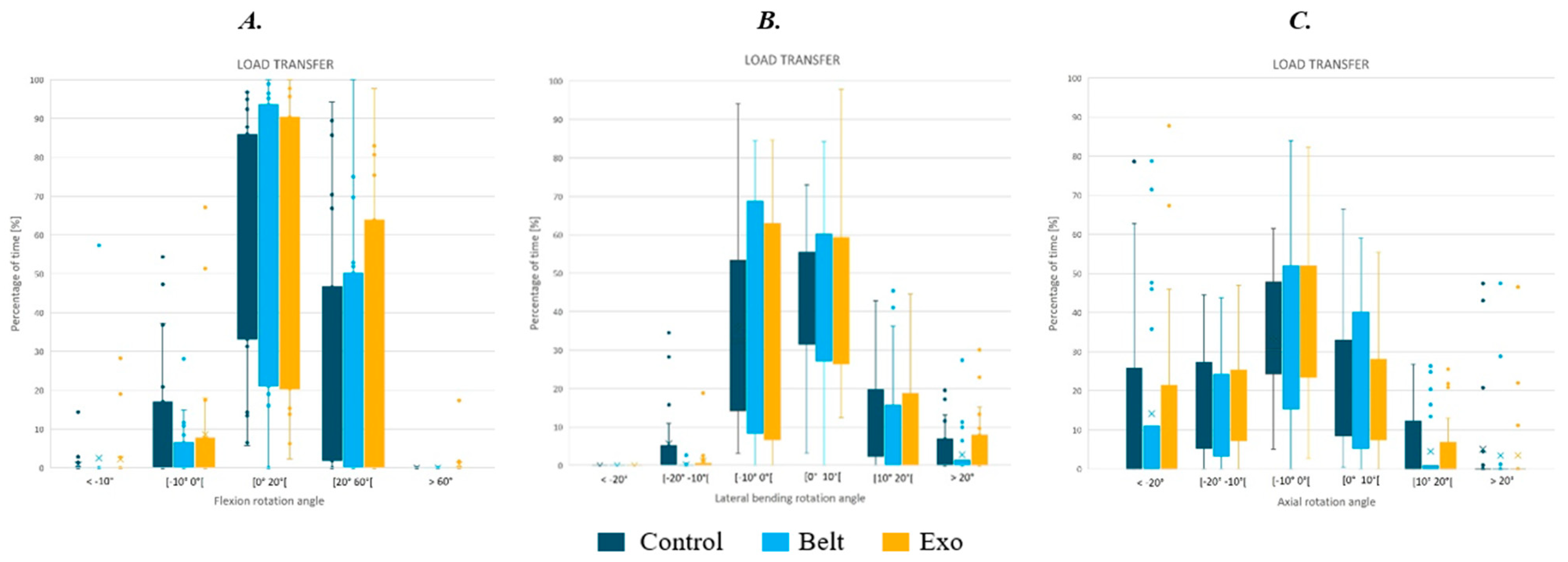
2.5.1. Kinematics Data
2.5.2. EMG
2.5.3. Statistical Analysis
3. Results
3.1. Kinematics Analysis
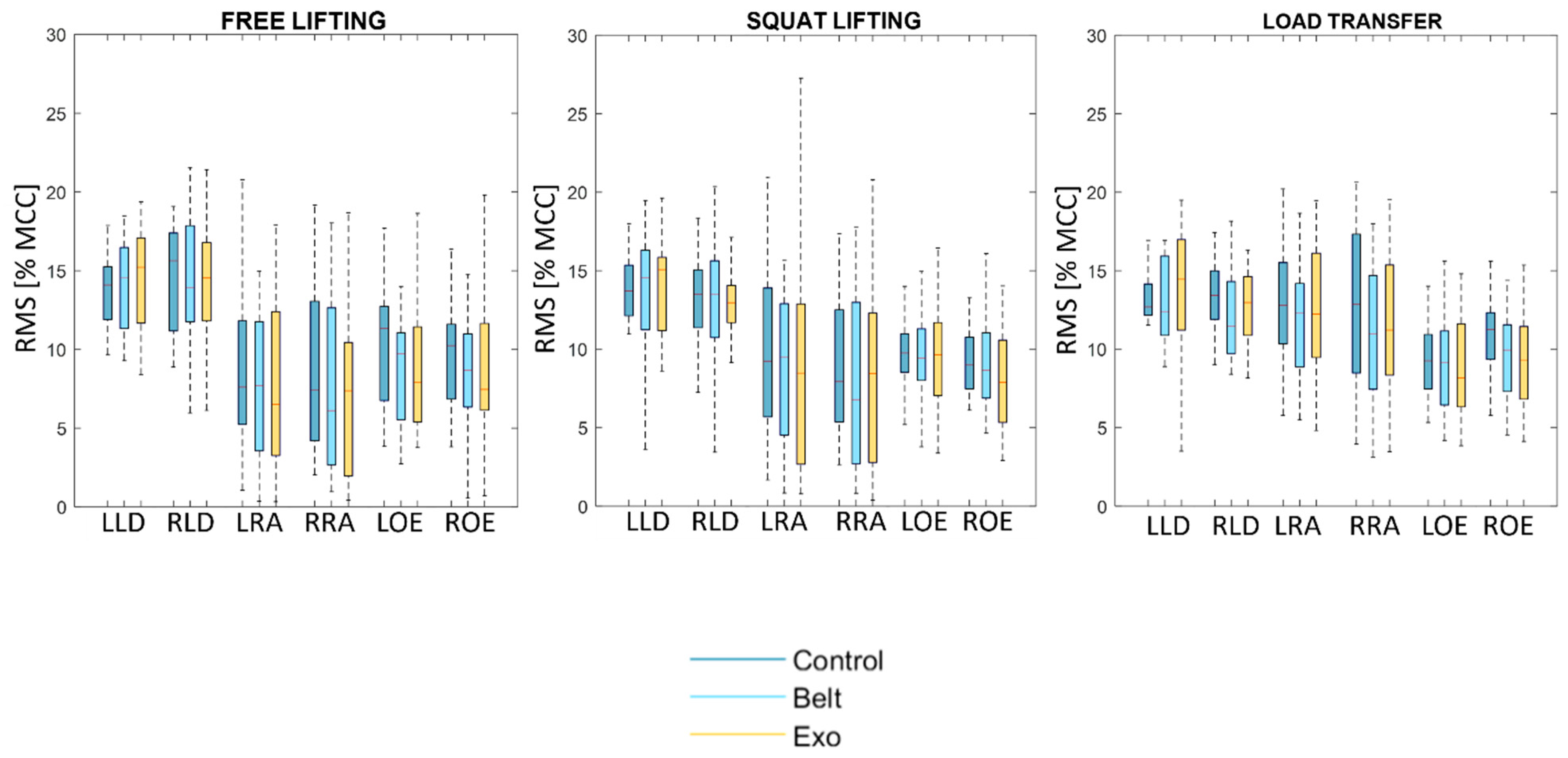
3.2. EMG
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Korhan, O.; Ahmed Memon, A. Introductory Chapter: Work-Related Musculoskeletal Disorders. In Work-Related Musculoskeletal Disorders; Korhan, O., Ed.; IntechOpen: London, UK, 2019; ISBN 978-1-78985-234-9. [Google Scholar]
- Assurance Maladie. Les TMS: Définition et Impact. Available online: https://www.ameli.fr/entreprise/sante-travail/risques/troubles-musculosquelettiques-tms/tms-definition-impact (accessed on 22 May 2024).
- Da Costa, B.R.; Vieira, E.R. Risk factors for work-related musculoskeletal disorders: A systematic review of recent longitudinal studies. Am. J. Ind. Med. 2010, 53, 285–323. [Google Scholar] [CrossRef] [PubMed]
- Flor-Unda, O.; Casa, B.; Fuentes, M.; Solorzano, S.; Narvaez-Espinoza, F.; Acosta-Vargas, P. Exoskeletons: Contribution to Occupational Health and Safety. Bioengineering 2023, 10, 1039. [Google Scholar] [CrossRef] [PubMed]
- Farah, L.; Roll, D.; Sorais, A.; Vallée, A. Assessment of Exoskeletons on Nurses’ Quality of Work Life: A Pilot Study at Foch Hospital. Nurs. Rep. 2023, 13, 780–791. [Google Scholar] [CrossRef] [PubMed]
- Thamsuwan, O.; Milosavljevic, S.; Srinivasan, D.; Trask, C. Potential exoskeleton uses for reducing low back muscular activity during farm tasks. Am. J. Ind. Med. 2020, 63, 1017–1028. [Google Scholar] [CrossRef] [PubMed]
- Inoue, G.; Uchida, K.; Miyagi, M.; Saito, W.; Nakazawa, T.; Imura, T.; Shirasawa, E.; Akazawa, T.; Orita, S.; Inage, K.; et al. Occupational Characteristics of Low Back Pain Among Standing Workers in a Japanese Manufacturing Company. Workplace Health Saf. 2020, 68, 13–23. [Google Scholar] [CrossRef] [PubMed]
- Rabal-Pelay, J.; Cimarras-Otal, C.; Macia-Calvo, M.; Laguna-Miranda, C.; Bataller-Cervero, A.V. Use of a Spinal Traction Device during Work Shift in Assembly Line Workers. Int. J. Environ. Res. Public Health 2021, 18, 7708. [Google Scholar] [CrossRef] [PubMed]
- Moon, C.; Bae, J.; Kwak, J.; Hong, D. A Lower-Back Exoskeleton With a Four-Bar Linkage Structure for Providing Extensor Moment and Lumbar Traction Force. IEEE Trans. Neural Syst. Rehabil. Eng. 2022, 30, 729–737. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Galán, M.; Pérez-Alonso, J.; Callejón-Ferre, Á.-J.; López-Martínez, J. Musculoskeletal disorders: OWAS review. Ind. Health 2017, 55, 314–337. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, S.A.; Marras, W.S.; Burr, D. Workplace design guidelines for asymptomatic vs. low-back-injured workers. Appl. Ergon. 2005, 36, 85–95. [Google Scholar] [CrossRef]
- Ma, T.; Zhang, Y.; Choi, S.D.; Xiong, S. Modelling for design and evaluation of industrial exoskeletons: A systematic review. Appl. Ergon. 2023, 113, 104100. [Google Scholar] [CrossRef]
- De Looze, M.P.; Bosch, T.; Krause, F.; Stadler, K.S.; O’Sullivan, L.W. Exoskeletons for industrial application and their potential effects on physical work load. Ergonomics 2016, 59, 671–681. [Google Scholar] [CrossRef] [PubMed]
- Moulart, M.; Olivier, N.; Giovanelli, Y.; Marin, F. Subjective assessment of a lumbar exoskeleton’s impact on lower back pain in a real work situation. Heliyon 2022, 8, e11420. [Google Scholar] [CrossRef]
- Sghaier, N.; Bellhari-Trahin, S.; Marin, F.; Ben Mansour, K. How to estimate the transparency assistance of a passive exoskeleton? a case study. Comput. Methods Biomech. Biomed. Engin. 2019, 22, S460–S462. [Google Scholar] [CrossRef]
- Schwartz, M.; Desbrosses, K.; Theurel, J.; Mornieux, G. Biomechanical Consequences of Using Passive and Active Back-Support Exoskeletons during Different Manual Handling Tasks. Int. J. Environ. Res. Public Health 2023, 20, 6468. [Google Scholar] [CrossRef]
- Botti, L.; Melloni, R. Occupational Exoskeletons: Understanding the Impact on Workers and Suggesting Guidelines for Practitioners and Future Research Needs. Appl. Sci. 2023, 14, 84. [Google Scholar] [CrossRef]
- Koopman, A.S.; Toxiri, S.; Power, V.; Kingma, I.; Van Dieën, J.H.; Ortiz, J.; De Looze, M.P. The effect of control strategies for an active back-support exoskeleton on spine loading and kinematics during lifting. J. Biomech. 2019, 91, 14–22. [Google Scholar] [CrossRef]
- Massardi, S.; Rodriguez-Cianca, D.; Pinto-Fernandez, D.; Moreno, J.C.; Lancini, M.; Torricelli, D. Characterization and Evaluation of Human–Exoskeleton Interaction Dynamics: A Review. Sensors 2022, 22, 3993. [Google Scholar] [CrossRef]
- Li-Baboud, Y.-S.; Virts, A.; Bostelman, R.; Yoon, S.; Rahman, A.; Rhode, L.; Ahmed, N.; Shah, M. Evaluation Methods and Measurement Challenges for Industrial Exoskeletons. Sensors 2023, 23, 5604. [Google Scholar] [CrossRef]
- Golabchi, A.; Chao, A.; Tavakoli, M. A Systematic Review of Industrial Exoskeletons for Injury Prevention: Efficacy Evaluation Metrics, Target Tasks, and Supported Body Postures. Sensors 2022, 22, 2714. [Google Scholar] [CrossRef]
- European Parliament Regulation (EU) 2017/745 of the European Parliament and of the Council of 5 April 2017 on Medical Devices 2023. Available online: http://data.europa.eu/eli/reg/2017/745/oj (accessed on 22 May 2024).
- European Agency for Safety and Health at Work (OSHA) The Impact of Using Exoskeletons on Occupational Safety and Health 2019. Available online: https://osha.europa.eu/sites/default/files/2021-11/Exoskeletons%26OSH.pdf (accessed on 22 May 2024).
- Pesenti, M.; Antonietti, A.; Gandolla, M.; Pedrocchi, A. Towards a Functional Performance Validation Standard for Industrial Low-Back Exoskeletons: State of the Art Review. Sensors 2021, 21, 808. [Google Scholar] [CrossRef]
- Robertson, D.G.E.; Caldwell, G.E.; Hamill, J.; Kamen, G.; Whittlesey, S.N. Research Methods in Biomechanics, 2nd ed.; Human Kinetics: Champaign, IL, USA, 2014; ISBN 978-0-7360-9340-8. [Google Scholar]
- Marin, F. Human and Animal Motion Tracking Using Inertial Sensors. Sensors 2020, 20, 6074. [Google Scholar] [CrossRef] [PubMed]
- Garg, A.; Kapellusch, J.M. Applications of biomechanics for prevention of work-related musculoskeletal disorders. Ergonomics 2009, 52, 36–59. [Google Scholar] [CrossRef] [PubMed]
- Zaciorskij, V.M. Kinetics of Human Motion; Human Kinetics: Champaign, IL, USA, 2002; ISBN 978-0-7360-3778-5. [Google Scholar]
- McAtamney, L.; Nigel Corlett, E. RULA: A survey method for the investigation of work-related upper limb disorders. Appl. Ergon. 1993, 24, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Vignais, N.; Miezal, M.; Bleser, G.; Mura, K.; Gorecky, D.; Marin, F. Innovative system for real-time ergonomic feedback in industrial manufacturing. Appl. Ergon. 2013, 44, 566–574. [Google Scholar] [CrossRef]
- Normand, M.A.; Lee, J.; Su, H.; Sulzer, J.S. The effect of hip exoskeleton weight on kinematics, kinetics, and electromyography during human walking. J. Biomech. 2023, 152, 111552. [Google Scholar] [CrossRef]
- Reimeir, B.; Calisti, M.; Mittermeier, R.; Ralfs, L.; Weidner, R. Effects of back-support exoskeletons with different functional mechanisms on trunk muscle activity and kinematics. Wearable Technol. 2023, 4, e12. [Google Scholar] [CrossRef] [PubMed]
- Huysamen, K.; De Looze, M.; Bosch, T.; Ortiz, J.; Toxiri, S.; O’Sullivan, L.W. Assessment of an active industrial exoskeleton to aid dynamic lifting and lowering manual handling tasks. Appl. Ergon. 2018, 68, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Chung, T.-S.; Yang, H.-E.; Ahn, S.J.; Park, J.H. Herniated Lumbar Disks: Real-time MR Imaging Evaluation during Continuous Traction. Radiology 2015, 275, 755–762. [Google Scholar] [CrossRef] [PubMed]
- Cappozzo, A.; Catani, F.; Della Croce, U.; Leardini, A. Position and orientation in space of bones during movement: Anatomical frame definition and determination. Clin. Biomech. 1995, 10, 171–178. [Google Scholar] [CrossRef]
- Seniam Recommendations for Sensor Locations On individual Muscles 2022. Available online: http://www.seniam.org/ (accessed on 22 May 2024).
- Chino, K.; Ohya, T.; Suzuki, Y. Association between expiratory mouth pressure and abdominal muscle activity in healthy young males. Eur. J. Appl. Physiol. 2024. [Google Scholar] [CrossRef]
- Moulart, M.; Acien, M.; Olivier, N.; Marin, F. Preliminary study of angular velocity vs. angular position phase diagram of the thoraco-pelvis joint with ambulatory lumbar traction exoskeleton. In Proceedings of the 47th congress of the Society of Biomechanics, Monastir, Tunisia, 26–28 October 2022; pp. s213–s214. [Google Scholar]
- Wu, G.; Siegler, S.; Allard, P.; Kirtley, C.; Leardini, A.; Rosenbaum, D.; Whittle, M.; D’Lima, D.D.; Cristofolini, L.; Witte, H.; et al. ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion—Part I: Ankle, hip, and spine. J. Biomech. 2002, 35, 543–548. [Google Scholar] [CrossRef] [PubMed]
- Simon, A.A.; Alemi, M.M.; Asbeck, A.T. Kinematic effects of a passive lift assistive exoskeleton. J. Biomech. 2021, 120, 110317. [Google Scholar] [CrossRef] [PubMed]
- Koopman, A.S.; Näf, M.; Baltrusch, S.J.; Kingma, I.; Rodriguez-Guerrero, C.; Babič, J.; De Looze, M.P.; Van Dieën, J.H. Biomechanical evaluation of a new passive back support exoskeleton. J. Biomech. 2020, 105, 109795. [Google Scholar] [CrossRef] [PubMed]
- Marras, W.S.; Davis, K.G.; Maronitis, A.B. A non-MVC EMG normalization technique for the trunk musculature: Part 2. Validation and use to predict spinal loads. J. Electromyogr. Kinesiol. 2001, 11, 11–18. [Google Scholar] [CrossRef] [PubMed]
- Shahvarpour, A.; Preuss, R.; Sullivan, M.J.L.; Negrini, A.; Larivière, C. The effect of wearing a lumbar belt on biomechanical and psychological outcomes related to maximal flexion-extension motion and manual material handling. Appl. Ergon. 2018, 69, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Hansen, C.; Gosselin, F.; Ben Mansour, K.; Devos, P.; Marin, F. Design-validation of a hand exoskeleton using musculoskeletal modeling. Appl. Ergon. 2018, 68, 283–288. [Google Scholar] [CrossRef] [PubMed]
- Abdoli-E, M.; Agnew, M.J.; Stevenson, J.M. An on-body personal lift augmentation device (PLAD) reduces EMG amplitude of erector spinae during lifting tasks. Clin. Biomech. 2006, 21, 456–465. [Google Scholar] [CrossRef] [PubMed]
- Walter, T.; Stutzig, N.; Siebert, T. Active exoskeleton reduces erector spinae muscle activity during lifting. Front. Bioeng. Biotechnol. 2023, 11, 1143926. [Google Scholar] [CrossRef] [PubMed]
- Bär, M.; Luger, T.; Seibt, R.; Rieger, M.A.; Steinhilber, B. Using a Passive Back Exoskeleton During a Simulated Sorting Task: Influence on Muscle Activity, Posture, and Heart Rate. Hum. Factors J. Hum. Factors Ergon. Soc. 2024, 66, 40–55. [Google Scholar] [CrossRef]
- Kranenborg, S.E.; Greve, C.; Reneman, M.F.; Roossien, C.C. Side-effects and adverse events of a shoulder- and back-support exoskeleton in workers: A systematic review. Appl. Ergon. 2023, 111, 104042. [Google Scholar] [CrossRef]
- Huxel Bliven, K.C.; Anderson, B.E. Core Stability Training for Injury Prevention. Sports Health Multidiscip. Approach 2013, 5, 514–522. [Google Scholar] [CrossRef] [PubMed]
- Macedo, L.G.; Latimer, J.; Maher, C.G.; Hodges, P.W.; McAuley, J.H.; Nicholas, M.K.; Tonkin, L.; Stanton, C.J.; Stanton, T.R.; Stafford, R. Effect of Motor Control Exercises Versus Graded Activity in Patients With Chronic Nonspecific Low Back Pain: A Randomized Controlled Trial. Phys. Ther. 2012, 92, 363–377. [Google Scholar] [CrossRef] [PubMed]
- Luger, T.; Bär, M.; Seibt, R.; Rieger, M.A.; Steinhilber, B. Using a Back Exoskeleton During Industrial and Functional Tasks—Effects on Muscle Activity, Posture, Performance, Usability, and Wearer Discomfort in a Laboratory Trial. Hum. Factors J. Hum. Factors Ergon. Soc. 2023, 65, 5–21. [Google Scholar] [CrossRef] [PubMed]
- Zaïri, F.; Moulart, M.; Fontaine, C.; Zaïri, F.; Tiffreau, V.; Logier, R. Relevance of a novel external dynamic distraction device for treating back pain. Proc. Inst. Mech. Eng. Part H 2021, 235, 264–272. [Google Scholar] [CrossRef] [PubMed]
- Goršič, M.; Song, Y.; Dai, B.; Novak, D. Evaluation of the HeroWear Apex back-assist exosuit during multiple brief tasks. J. Biomech. 2021, 126, 110620. [Google Scholar] [CrossRef]
- Kee, D. Systematic Comparison of OWAS, RULA, and REBA Based on a Literature Review. Int. J. Environ. Res. Public Health 2022, 19, 595. [Google Scholar] [CrossRef]

| RULA Area | <−10° | [−10° 0°[ | [0° 20°[ | [20° 60°[ | ≥60° |
|---|---|---|---|---|---|
| FREE LIFTING | 0.0248 * | 0.0366 * | 0.0046 * | 0.0125 * | 0.0036 * |
| SQUAT LIFTING | 0.0208 * | 0.1767 | 0.0091 * | 0.0026 * | 0.0062 * |
| RULA Area | <−10° | [−10° 0°[ | [0° 20°[ | [20° 60°[ | ≥60° |
|---|---|---|---|---|---|
| Control vs. Belt | 0.3894 | 0.8005 | 0.0074 * | 0.0068 * | 0.0046 * |
| Control vs. Exo | 0.0131 * | 0.0304 * | 0.0095 * | 0.9825 | 0.0276 * |
| Belt vs. Exo | 0.0942 | 0.0490 * | 0.4290 | 0.0110 * | 0.5380 |
| RULA Area | <−10° | [−10° 0°[ | [0° 20°[ | [20° 60°[ | ≥60° |
|---|---|---|---|---|---|
| Control vs. Belt | 0.3894 | 0.8005 | 0.0074 * | 0.0068 * | 0.0046 * |
| Control vs. Exo | 0.0131 * | 0.0304 * | 0.0095 * | 0.9825 | 0.0276 * |
| Belt vs. Exo | 0.0942 | 0.0490 * | 0.4290 | 0.0110 * | 0.5380 |
| RMS | LeftLD | RightLD | LeftRA | RightRA | LeftOE | RightOE |
|---|---|---|---|---|---|---|
| FREE LIFTING | 0.4013 | 0.5682 | 0.0147 * | 0.0429 * | 0.0363 * | 0.0122 * |
| SQUAT LIFTING | 0.8404 | 0.0175 * | 0.3480 | 0.0657 * | 0.1787 | 0.0351 * |
| LOAD TRANSFER | 0.0175 | 0.1188 | 0.0013 * | 7.8 × 10−5 * | 0.2765 | 0.0074 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moulart, M.; Acien, M.; Leonard, A.; Loir, M.; Olivier, N.; Marin, F. Investigating Kinematics and Electromyography Changes in Manual Handling Tasks with an Active Lumbar Exoskeleton. Biomechanics 2024, 4, 357-368. https://doi.org/10.3390/biomechanics4020025
Moulart M, Acien M, Leonard A, Loir M, Olivier N, Marin F. Investigating Kinematics and Electromyography Changes in Manual Handling Tasks with an Active Lumbar Exoskeleton. Biomechanics. 2024; 4(2):357-368. https://doi.org/10.3390/biomechanics4020025
Chicago/Turabian StyleMoulart, Mélissa, Maxime Acien, Audrey Leonard, Mathilde Loir, Nicolas Olivier, and Frédéric Marin. 2024. "Investigating Kinematics and Electromyography Changes in Manual Handling Tasks with an Active Lumbar Exoskeleton" Biomechanics 4, no. 2: 357-368. https://doi.org/10.3390/biomechanics4020025





