The Role of the Hypothalamus–Pituitary–Adrenal (HPA) Axis in Test-Induced Anxiety: Assessments, Physiological Responses, and Molecular Details
Abstract
:1. Introduction
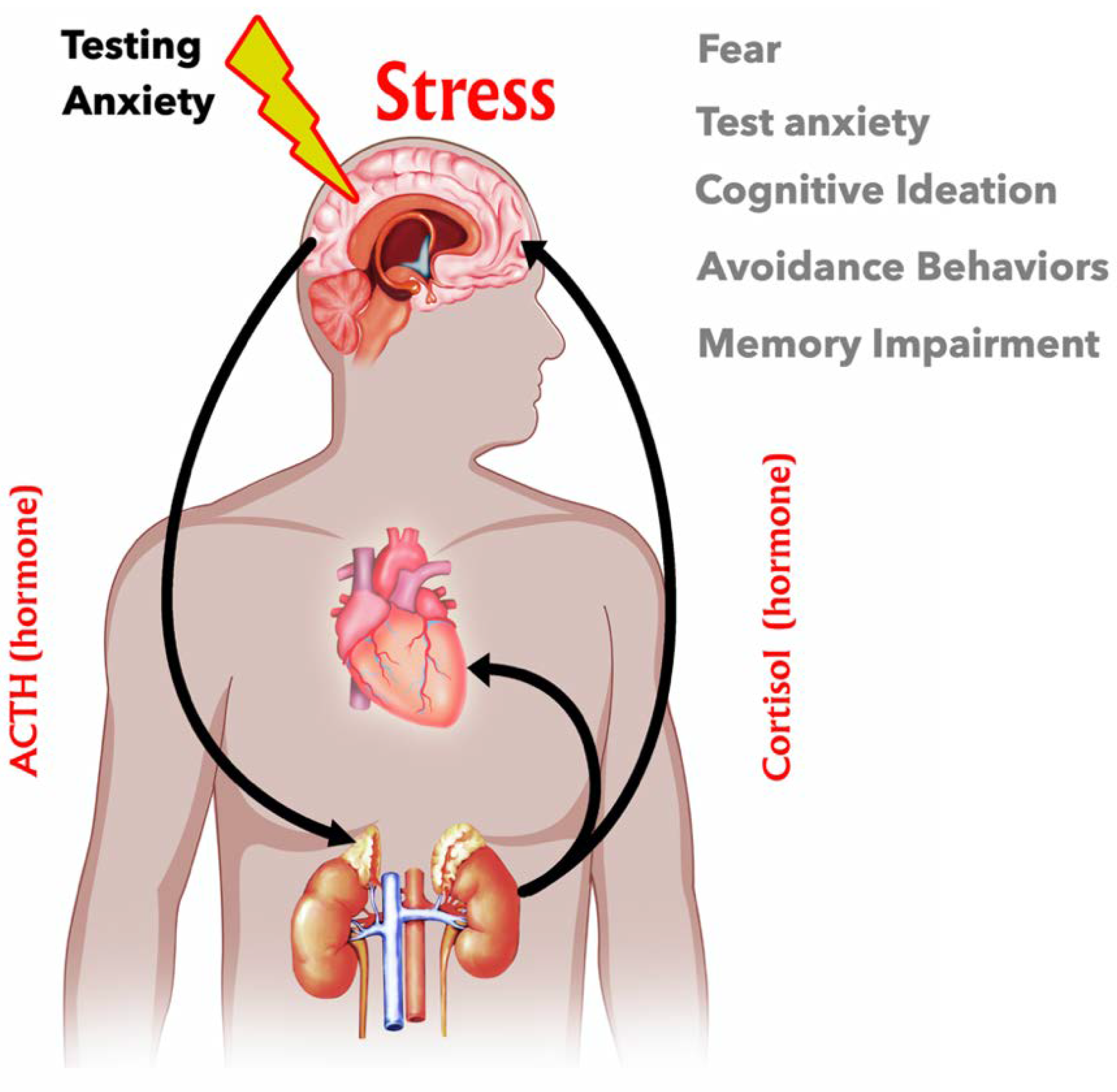
2. Stress Regulation via the Hypothalamus–Pituitary–Adrenal Axis (HPA)
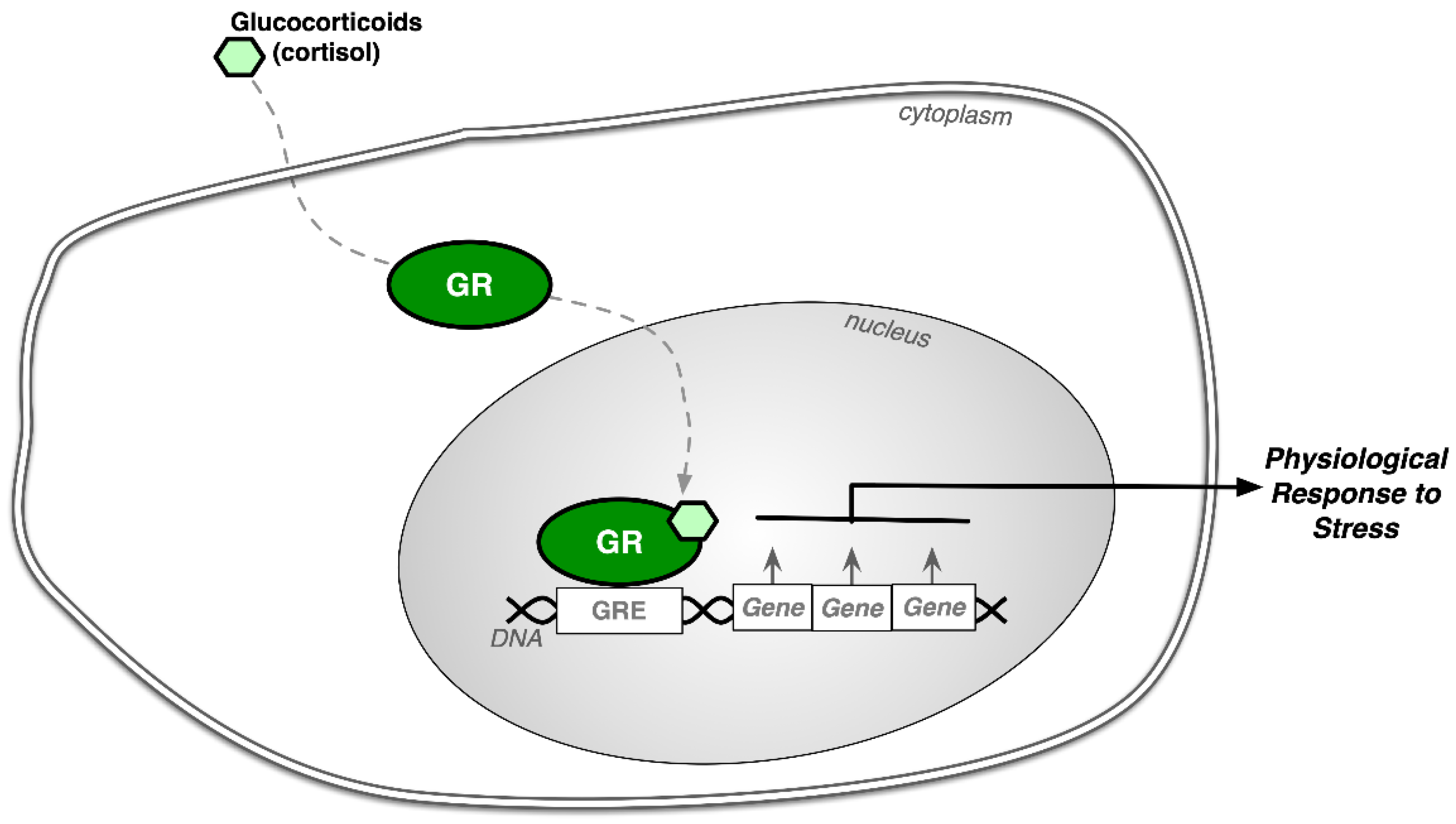
3. Cellular and Molecular Actions of GCs
4. Effects of Glucocorticoids on the Brain
5. Memory and the Effects of Glucocorticoids
6. Effects of Anxiety on Cortisol Levels
7. Test Anxiety and Psychological Assessments: Accommodations as Treatments
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- National Mathematics Advisory Panel Foundations for Success: The Final Report of the National Mathematics Advisory Panel; U.S. Department of Education: Washington, DC, USA, 2008.
- Hu, Q.; Wu, Q.; Cheng, H. Investigation on test anxiety and coping style of middle school students in different nationalities. Creat. Educ. 2018, 9, 1071–1083. [Google Scholar] [CrossRef] [Green Version]
- Sari, S.A.; Bilek, G.; Celik, E. Test anxiety and self-esteem in senior high school students: A cross-sectional study. Nord. J. Psychiatry 2017, 72, 84–88. [Google Scholar] [CrossRef] [PubMed]
- Poorman, S.G.; Mastorovich, M.L.; Gerwick, M. Interventions for test anxiety: How faculty can help. Teach. Learn. Nurs. 2019, 14, 186–191. [Google Scholar] [CrossRef]
- Sawka-Miller, K.D. Test anxiety. In Encyclopedia of Child Behavior and Development; Goldstein, S., Naglieri, J.A., Eds.; Springer: Boston, MA, USA, 2011; pp. 1478–1479. [Google Scholar] [CrossRef]
- Atasheneh, N.; Izadi, A. The role of teachers in reducing/increasing listening comprehension test anxiety: A case of Iranian EFL learners. Engl. Lang. Teach. 2012, 5, 178–187. [Google Scholar] [CrossRef] [Green Version]
- Embse, N.; Jester, D.; Roy, D.; Post, J. Test anxiety effects, predictors, and correlates: A 30-year meta-analytic review. J. Affect. Disord. 2018, 227, 483–493. [Google Scholar] [CrossRef] [PubMed]
- Birenbaum, M.; Gutvirtz, Y. The relationship between test anxiety and seriousness of errors in algebra. J. Psychoeduc. Assess. 1993, 11, 12–19. [Google Scholar] [CrossRef]
- Farooqi, Y.N.; Ghani, R.; Spielberger, C.D. Gender differences in test anxiety and academic performance of medical students. Int. J. Psychol. Behav. Res. 2012, 2, 38–43. [Google Scholar]
- Duraku, Z.H.; Hoxha, L. Self-esteem, study skills, self-concept, social support, psychological distress, and coping mechanism effects on test anxiety and academic performance. Health Psychol. Open 2018, 5, 2055102918799963. [Google Scholar]
- Hembree, R. Correlates, causes, effects, and treatment of test anxiety. Rev. Educ. Res. 1988, 58, 47–77. [Google Scholar] [CrossRef]
- Zeidner, M. Test Anxiety: The State of the Art; Plenum Press: New York, NY, USA, 1998. [Google Scholar]
- Seipp, B. Anxiety and academic performance: A meta-analysis of findings. Anxiety Res. 1991, 4, 27–41. [Google Scholar] [CrossRef]
- Pekrun, R.; Goetz, T.; Titz, W. Academic emotions in students’ self-regulated learning and achievement: A program of qualitative and quantitative research. Educ. Psychol. 2002, 37, 91–105. [Google Scholar] [CrossRef]
- Methia, R.A. Help Your Child Overcome Test Anxiety and Achieve Higher Test Scores; Virtual Bookworm. Com Pub Incorporated: College Station, TX, USA, 2004. [Google Scholar]
- Smedlund, K.B.; Sanchez, E.R.; Hinds, T.D., Jr. FKBP51 and the molecular chaperoning of metabolism. Trends Endocrinol. Metab. 2021, 32, 862–874. [Google Scholar] [CrossRef] [PubMed]
- John, K.; Marino, J.S.; Sanchez, E.R.; Hinds, T.D., Jr. The glucocorticoid receptor: Cause of or cure for obesity? Am. J. Physiol. Endocrinol. Metab. 2016, 310, E249–E257. [Google Scholar] [CrossRef] [Green Version]
- Sherin, J.E.; Nemeroff, C.B. Post-traumatic stress disorder: The neurobiological impact of psychological trauma. Dialogues Clin. Neurosci. 2011, 13, 263–278. [Google Scholar]
- McEwen, B.S.; Sapolsky, R.M. Stress and cognitive function. Curr. Opin. Neurobiol. 1995, 5, 205–216. [Google Scholar] [CrossRef]
- Molina, P. Endocrine Physiology, 3rd ed.; McGraw-Hill Companies: New York, NY, USA, 2010; p. 301. [Google Scholar]
- Doga, M.; Bonadonna, S.; Giustina, A. Glucocorticoids and bone: Cellular, metabolic and endocrine effects. Hormones 2004, 3, 184–190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ashwell, J.D.; Lu, F.W.; Vacchio, M.S. Glucocorticoids in T cell development and function*. Annu. Rev. Immunol. 2000, 18, 309–345. [Google Scholar] [CrossRef]
- Kaplan, N. The adrenal glands. In Textbook of Endocrine Physiology, 2nd ed.; Griffin, J.E., Ojeda, S.R., Eds.; Oxford University Press: Oxford, UK, 1992; pp. 247–275. [Google Scholar]
- Caron, S.; Staels, B. Apolipoprotein CIII: A link between hypertriglyceridemia and vascular dysfunction? Circ. Res. 2008, 103, 1348–1350. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adrenal Insufficiency and Addison’s Disease. Available online: https://www.niddk.nih.gov/health-information/endocrine-diseases/adrenal-insufficiency-addisons-disease (accessed on 20 January 2022).
- Hinds, T.D., Jr.; Sanchez, E.R. Protein phosphatase 5. Int. J. Biochem. Cell Biol. 2008, 40, 2358–2362. [Google Scholar] [CrossRef] [PubMed]
- Goosens, K.A.; Sapolsky, R.M. Stress and glucocorticoid contributions to normal and pathological aging. In Brain Aging: Models, Methods, and Mechanisms; Taylor & Francis Group, LLC: Boca Raton, FL, USA, 2007. [Google Scholar]
- Peffer, M.E.; Zhang, J.Y.; Umfrey, L.; Rudine, A.C.; Monaghan, A.P.; DeFranco, D.B. Minireview: The impact of antenatal therapeutic synthetic glucocorticoids on the developing fetal brain. Mol. Endocrinol. 2015, 29, 658–666. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Quervain, D.J.; Aerni, A.; Schelling, G.; Roozendaal, B. Glucocorticoids and the regulation of memory in health and disease. Front. Neuroendocrinol. 2009, 30, 358–370. [Google Scholar] [CrossRef] [PubMed]
- De Quervain, D.; Roozendaal, B.; McGaugh, J.L. Stress and glucocorticoids impair retrieval of long-term spatial memory. Nature 1998, 394, 787–790. [Google Scholar] [CrossRef] [PubMed]
- Wolkowitz, O.M.; Epel, E.S.; Reus, V.I. Stress hormone-related psychopathology: Pathophysiological and treatment implications. World J. Biol. Psychiatry 2001, 2, 115–143. [Google Scholar] [CrossRef] [PubMed]
- Holtzman, C.W.; Trotman, H.D.; Goulding, S.M.; Ryan, A.T.; Macdonald, A.N.; Shapiro, D.I.; Brasfield, J.L.; Walker, E.F. Stress and neurodevelopmental processes in the emergence of psychosis. Neuroscience 2013, 249, 172–191. [Google Scholar] [CrossRef] [Green Version]
- Sapolsky, R.M. Why stress is bad for your brain. Science 1996, 273, 749–750. [Google Scholar] [CrossRef]
- Jia, M.; Smerin, S.E.; Zhang, L.; Xing, G.; Li, X.; Benedek, D.; Ursano, R.; Li, H. Corticosterone mitigates the stress response in an animal model of PTSD. J. Psychiatr. Res. 2015, 60, 29–39. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Krishnan, V.; Nestler, E.J. The molecular neurobiology of depression. Nature 2008, 455, 894–902. [Google Scholar] [CrossRef]
- Burden of Mental And Behavioural Disorder; World Health Organization: Geneva, Switzerland, 2001; pp. 20–46. Available online: https://www.who.int/whr/2001/en/whr01_en.pdf (accessed on 20 January 2022).
- Anacker, C.; Zunszain, P.A.; Carvalho, L.A.; Pariante, C.M. The glucocorticoid receptor: Pivot of depression and of antidepressant treatment? Psychoneuroendocrinology 2011, 36, 415–425. [Google Scholar] [CrossRef] [Green Version]
- Parmenon, C.; Guillard, J.; Caignard, D.H.; Hennuyer, N.; Staels, B.; Audinot-Bouchez, V.; Boutin, J.A.; Dacquet, C.; Ktorza, A.; Viaud-Massuard, M.C. 4,4-Dimethyl-1,2,3,4-tetrahydroquinoline-based PPARalpha/gamma agonists. Part. II: Synthesis and pharmacological evaluation of oxime and acidic head group structural variations. Bioorganic Med. Chem. Lett. 2009, 19, 2683–2687. [Google Scholar] [CrossRef]
- Ashford, M. How are Memories Stored in the Brain. Available online: http://www.livescience.com/32798-how-are-memories-stored-in-the-brain.html (accessed on 20 January 2022).
- Mastin, L. Parts of the Brain. Available online: https://human-memory.net/parts-of-the-brain/ (accessed on 29 January 2022).
- McGaugh, J.L.; Roozendaal, B. Role of adrenal stress hormones in forming lasting memories in the brain. Neurobiology 2002, 12, 205–210. [Google Scholar] [CrossRef]
- Wolf, O.T. Stress and memory in humans: Twelve years of progress? Brain Res. 2009, 1293, 142–154. [Google Scholar] [CrossRef] [PubMed]
- Roozendaal, B. Stress and memory: Opposing effects of glucocorticoids on memory consolidation and memory retrieval. Neurobiol. Learn. Mem. 2002, 78, 578–595. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takai, N.; Yamaguchi, M.; Aragaki, T.; Eto, K.; Uchihashi, K.; Nishikawa, Y. Effect of psychological stress on the salivary cortisol and amylase levels in healthy young adults. Arch. Oral Biol. 2004, 49, 963–968. [Google Scholar] [CrossRef] [PubMed]
- Alhaddad, H.; Gordon, D.M.; Bell, R.L.; Jarvis, E.E.; Kipp, Z.A.; Hinds, T.D., Jr.; Sari, Y. Chronic ethanol consumption alters glucocorticoid receptor isoform expression in stress neurocircuits and mesocorticolimbic brain regions of alcohol-preferring rats. Neuroscience 2020, 437, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Tronche, F.; Kellendonk, C.; Kretz, O.; Gass, P.; Anlag, K.; Orban, P.C.; Bock, R.; Klein, R.; Schutz, G. Disruption of the glucocorticoid receptor gene in the nervous system results in reduced anxiety. Nat. Genet. 1999, 23, 99–103. [Google Scholar] [CrossRef]
- Heiman, T.; Precel, K. Students with learning disabilities in higher education: Academic strategies profile. J. Learn. Disabil. 2003, 36, 248–258. [Google Scholar] [CrossRef] [Green Version]
- Zargarzadeh, M.; Shirazi, M. The effect of progressive muscle relaxation method on test anxiety in nursing students. Iran J. Nurs. Midwifery 2014, 19, 607. [Google Scholar]
- Killu, K.; Crundwell, M.A. Students with anxiety in the classroom: Educational accommodations and interventions. Beyond Behav. 2016, 25, 30–40. [Google Scholar] [CrossRef]
- More on CBT. Available online: http://www.anxietybc.com/help-resources/cbt/more-on-cbt (accessed on 7 July 2015).
- Dialectical Behavior Therapy. Available online: http://www.nrepp.samhsa.gov/ViewIntervention.aspx?id=36 (accessed on 30 July 2020).
- Eye Movement Desensitization and Reprocessing. Available online: http://www.nrepp.samhsa.gov/ViewIntervention.aspx?id=199 (accessed on 30 July 2020).
- Ergene, T. Effective interventions on test anxiety reduction: A meta-analysis. Sch. Psychol. Int. 2003, 24, 313–328. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hinds, J.A.; Sanchez, E.R. The Role of the Hypothalamus–Pituitary–Adrenal (HPA) Axis in Test-Induced Anxiety: Assessments, Physiological Responses, and Molecular Details. Stresses 2022, 2, 146-155. https://doi.org/10.3390/stresses2010011
Hinds JA, Sanchez ER. The Role of the Hypothalamus–Pituitary–Adrenal (HPA) Axis in Test-Induced Anxiety: Assessments, Physiological Responses, and Molecular Details. Stresses. 2022; 2(1):146-155. https://doi.org/10.3390/stresses2010011
Chicago/Turabian StyleHinds, Jenalee A., and Edwin R. Sanchez. 2022. "The Role of the Hypothalamus–Pituitary–Adrenal (HPA) Axis in Test-Induced Anxiety: Assessments, Physiological Responses, and Molecular Details" Stresses 2, no. 1: 146-155. https://doi.org/10.3390/stresses2010011
APA StyleHinds, J. A., & Sanchez, E. R. (2022). The Role of the Hypothalamus–Pituitary–Adrenal (HPA) Axis in Test-Induced Anxiety: Assessments, Physiological Responses, and Molecular Details. Stresses, 2(1), 146-155. https://doi.org/10.3390/stresses2010011





