A Critical Review on Reusable Face Coverings: Mechanism, Development, Factors, and Challenges
Abstract
1. Introduction
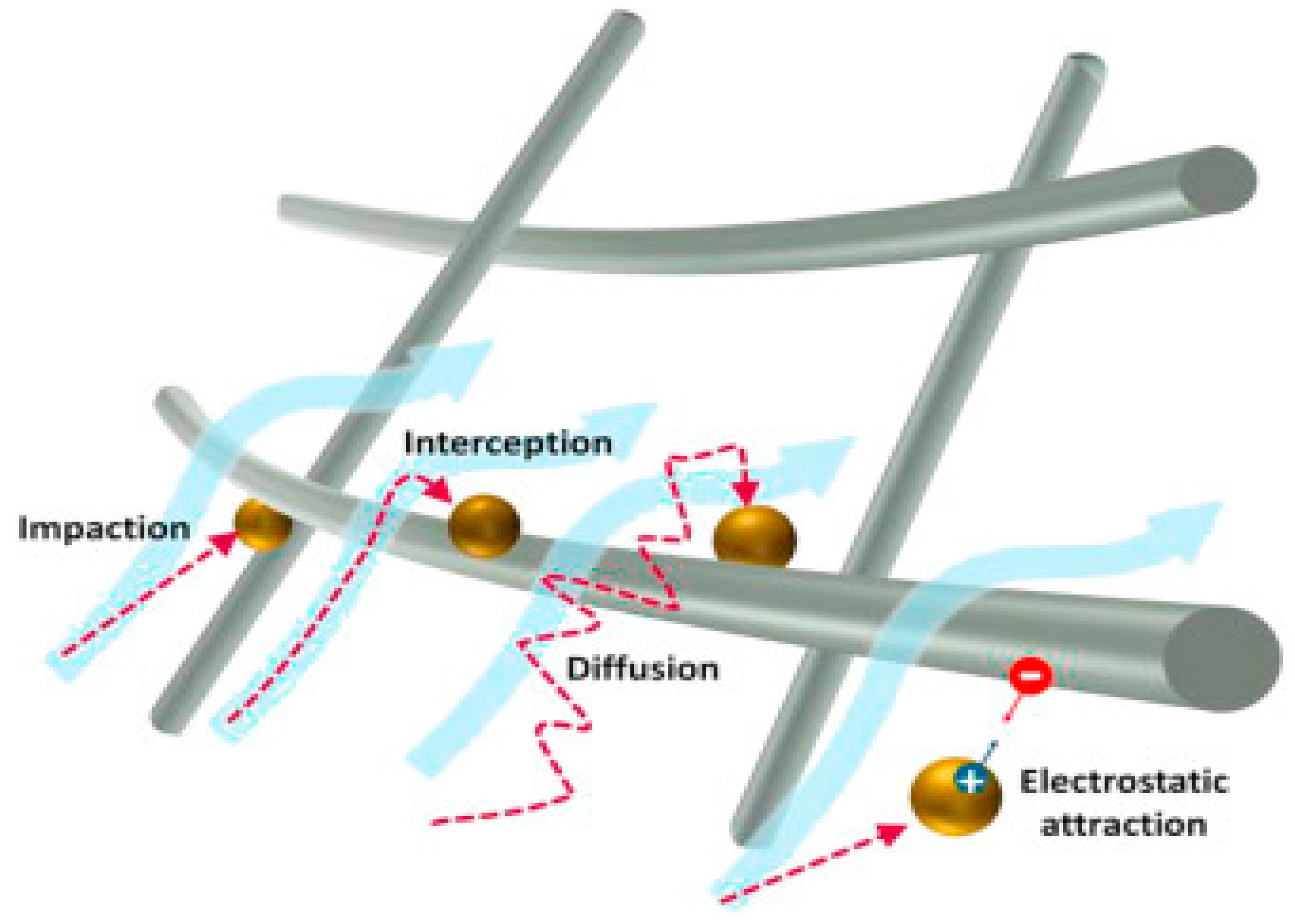
2. Mechanisms of Face Coverings
2.1. Interception and Impaction
2.2. Diffusion
2.3. Electrostatic Attraction
3. Consideration for Developing Face Coverings
3.1. Moisture Management
3.2. Breathing Resistance Factors
3.3. Balancing between Filtration and Breathability
4. Development of Face Coverings
4.1. Fiber and Yarn Construction
4.2. Fabric Construction
4.2.1. Knit Fabric Construction
4.2.2. Woven Fabric Construction
5. Factors Affecting Filtration Performance
5.1. Electrostatic Charge

5.2. Porosity
5.3. Layers
5.4. Finishes
5.5. Particle Size
5.6. Related Effect
6. Clinical Outcomes
7. Quality Control
8. Conclusions and Future Research Direction
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Krammer, F. SARS-CoV-2 vaccines in development. Nature 2020, 586, 516–527. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Infection Prevention and Control of Epidemic-and Pandemic-Prone Acute Respiratory Infections in Health Care; World Health Organization: Geneva, Switzerland, 2014.
- Lindsley, W.G.; Pearce, T.A.; Hudnall, J.B.; Davis, K.A.; Davis, S.M.; Fisher, M.A.; Khakoo, R.; Palmer, J.E.; Clark, K.E.; Celik, I.; et al. Quantity and Size Distribution of Cough-Generated Aerosol Particles Produced by Influenza Patients During and after Illness. J. Occup. Environ. Hyg. 2012, 9, 443–449. [Google Scholar] [CrossRef] [PubMed]
- Asadi, S.; Wexler, A.S.; Cappa, C.D.; Barreda, S.; Bouvier, N.M.; Ristenpart, W.D. Aerosol emission and superemission during human speech increase with voice loudness. Sci. Rep. 2019, 9, 2348. [Google Scholar] [CrossRef]
- Alsved, M.; Matamis, A.; Bohlin, R.; Richter, M.; Bengtsson, P.-E.; Fraenkel, C.-J.; Medstrand, P.; Löndahl, J. Exhaled respiratory particles during singing and talking. Aerosol Sci. Technol. 2020, 54, 1245–1248. [Google Scholar] [CrossRef]
- Zayas, G.; Chiang, M.C.; Wong, E.; Macdonald, F.; Lange, C.F.; Senthilselvan, A.; King, M. Cough aerosol in healthy participants: Fundamental knowledge to optimize droplet-spread infectious respiratory disease management. BMC Pulm. Med. 2012, 12, 11. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19); Centers for Disease Control and Prevention: Atlanta, GA, USA, 2020.
- Sickbert-Bennett, E.E.; Samet, J.M.; Clapp, P.W.; Chen, H.; Berntsen, J.; Zeman, K.L.; Tong, H.; Weber, D.J.; Bennett, W.D. Filtration Efficiency of Hospital Face Mask Alternatives Available for Use During the COVID-19 Pandemic. JAMA Intern. Med. 2020, 180, 1607–1612. [Google Scholar] [CrossRef]
- Howard, J.; Huang, A.; Li, Z.; Tufekci, Z.; Zdimal, V.; van der Westhuizen, H.-M.; von Delft, A.; Price, A.; Fridman, L.; Tang, L.-H.; et al. An evidence review of face masks against COVID-19. Proc. Natl. Acad. Sci. USA 2021, 118, e2014564118. [Google Scholar] [CrossRef]
- Gallaway, M.S.; Rigler, J.; Robinson, S.; Herrick, K.; Livar, E.; Komatsu, K.K.; Brady, S.; Cunico, J.; Christ, C.M. Trends in COVID-19 incidence after implementation of mitigation measures—Arizona, January 22–August 7, 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 1460. [Google Scholar] [CrossRef]
- Van Dyke, M.E.; Rogers, T.M.; Pevzner, E.; Satterwhite, C.L.; Shah, H.B.; Beckman, W.J.; Ahmed, F.; Hunt, C.; Rule, J. Trends in county-level COVID-19 incidence in counties with and without a mask mandate—Kansas, June 1–August 23, 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 1777. [Google Scholar] [CrossRef]
- Mitze, T.; Kosfeld, R.; Rode, J.; Wälde, K. Face masks considerably reduce COVID-19 cases in Germany. Proc. Natl. Acad. Sci. USA 2020, 117, 32293–32301. [Google Scholar] [CrossRef]
- Bhattacharjee, S.; Bahl, P.; Chughtai, A.A.; MacIntyre, C.R. Last-resort strategies during mask shortages: Optimal design features of cloth masks and decontamination of disposable masks during the COVID-19 pandemic. BMJ Open Respir. Res. 2020, 7, e000698. [Google Scholar] [CrossRef] [PubMed]
- Clase, C.M.; Fu, E.L.; Ashur, A.; Beale, R.C.; Clase, I.A.; Dolovich, M.B.; Jardine, M.J.; Joseph, M.; Kansiime, G.; Mann, J.F.; et al. Forgotten Technology in the COVID-19 Pandemic: Filtration Properties of Cloth and Cloth Masks—A Narrative Review. Mayo Clin. Proc. 2020, 95, 2204–2224. [Google Scholar] [CrossRef] [PubMed]
- Nanda, A.; Hung, I.; Kwong, A.; Man VC, M.; Roy, P.; Davies, L.; Douek, M. Efficacy of surgical masks or cloth masks in the prevention of viral transmission: Systematic review, meta-analysis, and proposal for future trial. J. Evid. Based Med. 2021, 14, 97–111. [Google Scholar] [CrossRef]
- Mahase, E. COVID-19: What is the evidence for cloth masks? BMJ 2020, 369, m14222020. [Google Scholar] [CrossRef]
- Milewska, B. The Impact of Instability in the Business Environment on the Competitiveness of Enterprises Using the Example of the Apparel Industry. Sustainability 2022, 14, 14673. [Google Scholar] [CrossRef]
- Shruti, V.; Pérez-Guevara, F.; Elizalde-Martínez, I.; Kutralam-Muniasamy, G. Reusable masks for COVID-19: A missing piece of the microplastic problem during the global health crisis. Mar. Pollut. Bull. 2020, 161, 111777. [Google Scholar] [CrossRef]
- Aydin, O.; Emon, B.; Cheng, S.; Hong, L.; Chamorro, L.P.; Saif, M.T.A. Performance of fabrics for home-made masks against the spread of COVID-19 through droplets: A quantitative mechanistic study. Extreme Mech. Lett. 2020, 40, 100924. [Google Scholar] [CrossRef]
- SARS-CoV-2 Resources—NCBI. Available online: https://www.ncbi.nlm.nih.gov/sars-cov-2/ (accessed on 15 January 2023).
- Luisetto, M.; Nili, B.; Khaled, E.; Mashori, G.; Rafa, A.Y.; Latishev, O.Y. Bioaerosols and Corona Virus Diffusion, Transmission, Carriers, Viral Size, Surfaces Properties and other Factor Involved. Int. J. Med. Healthc. Reports 2021, 1, 1004. [Google Scholar]
- Tucho, G.T.; Kumsa, D.M. Universal Use of Face Masks and Related Challenges During COVID-19 in Developing Countries. Risk Manag. Healthc. Policy 2021, 14, 511–517. [Google Scholar] [CrossRef]
- O’Kelly, E.; Pirog, S.; Ward, J.; Clarkson, P.J. Ability of fabric face mask materials to filter ultrafine particles at coughing velocity. BMJ Open 2020, 10, e039424. [Google Scholar] [CrossRef]
- Hao, W.; Parasch, A.; Williams, S.; Li, J.; Ma, H.; Burken, J.; Wang, Y. Filtration performances of non-medical materials as candidates for manufacturing facemasks and respirators. Int. J. Hyg. Environ. Health 2020, 229, 113582. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, M.; Marr, L.C. Uniting Infectious Disease and Physical Science Principles on the Importance of Face Masks for COVID-19. Med 2020, 2, 29–32. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Ji, D.; He, H.; Ramakrishna, S. Electrospun ultrafine fibers for advanced face masks. Mater. Sci. Eng. R Rep. 2020, 143, 100594. [Google Scholar] [CrossRef] [PubMed]
- Han, S.; Kim, J.; Ko, S. Advances in air filtration technologies: Structure-based and interaction-based approaches. Mater. Today Adv. 2021, 9, 100134. [Google Scholar] [CrossRef]
- World Health Organization. Advice on the Use of Masks in the Community, during Home Care and in Healthcare Settings in the Context of the Novel Coronavirus (COVID-19) Outbreak. Available online: https://www.who.int/publications/i/item/advice-on-the-use-of-masks-in-the-community-during-home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak (accessed on 15 January 2023).
- Zieliński, J.; Przybylski, J. How much water is lost during breathing? Pneumonol. Alergol. Polska 2012, 80, 339–342. [Google Scholar]
- Wardiningsih, W.; Troynikov, O. Influence of cover factor on liquid moisture transport performance of bamboo knitted fabrics. J. Text. Inst. 2012, 103, 89–98. [Google Scholar] [CrossRef]
- Lai, M.Y.Y.; Cheng, P.K.C.; Lim, W.W.L. Survival of Severe Acute Respiratory Syndrome Coronavirus. Clin. Infect. Dis. 2005, 41, e67–e71. [Google Scholar] [CrossRef]
- Iqbal, M.I. Adaptive Textiles for Thermal Management Using Wool Fibers. 2021. Available online: https://theses.lib.polyu.edu.hk/handle/200/11310 (accessed on 20 February 2023).
- Iqbal, M.I.; Shuo, S.; Jiang, Y.; Fei, B.; Xia, Q.; Wang, X.; Hu, W.; Hu, J. Woolen Respirators for Thermal Management. Adv. Mater. Technol. 2021, 6, 2100201. [Google Scholar] [CrossRef]
- Parlin, A.F.; Stratton, S.M.; Culley, T.M.; Guerra, P.A. A laboratory-based study examining the properties of silk fabric to evaluate its potential as a protective barrier for personal protective equipment and as a functional material for face coverings during the COVID-19 pandemic. PLoS ONE 2020, 15, e0239531. [Google Scholar] [CrossRef]
- Parajuli, P.; Acharya, S.; Rumi, S.S.; Hossain, M.T.; Abidi, N. Regenerated cellulose in textiles: Rayon, lyocell, modal and other fibres. In Fundamentals of Natural Fibres and Textiles; Elsevier: Amsterdam, The Netherlands, 2021; pp. 87–110. [Google Scholar]
- Durur, G.; Öner, E. The Comfort Properties of the Terry Towels Made of Cotton and Polypropylene Yarns. J. Eng. Fibers Fabr. 2013, 8, 155892501300800201. [Google Scholar] [CrossRef]
- Syed, Q.; Sopwith, W.; Regan, M.; Bellis, M.A. Behind the mask. Journey through an epidemic: Some observations of contrasting public health responses to SARS. J. Epidemiol. Community Health 2003, 57, 855–856. [Google Scholar] [CrossRef]
- Kähler, C.J.; Hain, R. Fundamental protective mechanisms of face masks against droplet infections. J. Aerosol Sci. 2020, 148, 105617. [Google Scholar] [CrossRef] [PubMed]
- Davies, A.; Thompson, K.-A.; Giri, K.; Kafatos, G.; Walker, J.; Bennett, A. Testing the Efficacy of Homemade Masks: Would They Protect in an Influenza Pandemic? Disaster Med. Public Health Prep. 2013, 7, 413–418. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, M.I.; Sun, F.; Fei, B.; Xia, Q.; Wang, X.; Hu, J. Knit Architecture for Water-Actuating Woolen Knitwear and Its Personalized Thermal Management. ACS Appl. Mater. Interfaces 2021, 13, 6298–6308. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.-P.; Yip, J.; Kan, C.-W.; Chiou, J.-C.; Yung, K.-F. Reusable Face Masks as Alternative for Disposable Medical Masks: Factors that Affect their Wear-Comfort. Int. J. Environ. Res. Public Health 2020, 17, 6623. [Google Scholar] [CrossRef]
- Konda, A.; Prakash, A.; Moss, G.A.; Schmoldt, M.; Grant, G.D.; Guha, S. Aerosol filtration efficiency of common fabrics used in respiratory cloth masks. ACS Nano 2020, 14, 6339–6347. [Google Scholar] [CrossRef]
- Hancock, J.N.; Plumley, M.J.; Schilling, K.; Sheets, D.; Wilen, L. Comment on “Aerosol Filtration Efficiency of Common Fabrics Used in Respiratory Cloth Masks”. ACS Nano 2020, 14, 10758–10763. [Google Scholar] [CrossRef]
- Liao, M.; Liu, H.; Wang, X.; Hu, X.; Huang, Y.; Liu, X.; Brenan, K.; Mecha, J.; Nirmalan, M.; Lu, J.R. A technical review of face mask wearing in preventing respiratory COVID-19 transmission. Curr. Opin. Colloid Interface Sci. 2021, 52, 101417. [Google Scholar] [CrossRef]
- Bourouiba, L.; Dehandschoewercker, E.; Bush, J.W.M. Violent expiratory events: On coughing and sneezing. J. Fluid Mech. 2014, 745, 537–563. [Google Scholar] [CrossRef]
- Wei, J.; Li, Y. Human Cough as a Two-Stage Jet and Its Role in Particle Transport. PLoS ONE 2017, 12, e0169235. [Google Scholar] [CrossRef]
- Zangmeister, C.D.; Radney, J.G.; Vicenzi, E.P.; Weaver, J.L. Filtration efficiencies of nanoscale aerosol by cloth mask materials used to slow the spread of SARS-CoV-2. ACS Nano 2020, 14, 9188–9200. [Google Scholar] [CrossRef] [PubMed]
- Tahvildar, A.; Ezazshahabi, N.; Mousazadegan, F. Appearance and comfort properties considering yarn-spinning system and weave structure in worsted woven fabrics. J. Eng. Fibers Fabr. 2019, 14, 1558925019845978. [Google Scholar] [CrossRef]
- Nguyen, M.; Donalson, G.; Bradley, N.; Templeton, T.; Verma, M.; Aldridge, A.; Spalding, S. Evaluation of the Efficacy of Fabric Face Masks on the Number of Wash during the Outbreak of Coronavirus (COVID-19). 2021. Available online: https://ursa.mercer.edu/handle/10898/12658 (accessed on 21 January 2023).
- Haleem, N.; Wang, X. Recent research and developments on yarn hairiness. Text. Res. J. 2014, 85, 211–224. [Google Scholar] [CrossRef]
- Al-Amin, M. A Comparative Study of Mechanical Performance Characteristics Between Treated and Untreated Ham Nets; Mississippi State University: Mississippi State, MS, USA, 2020; Available online: https://scholarsjunction.msstate.edu/cgi/viewcontent.cgi?article=1057&context=td (accessed on 8 February 2023).
- Cheng, S.; Hao, W.; Wang, Y.; Wang, Y.; Yang, S. Commercial Janus Fabrics as Reusable Facemask Materials: A Balance of Water Repellency, Filtration Efficiency, Breathability, and Reusability. ACS Appl. Mater Interfaces 2022, 14, 32579–32589. [Google Scholar] [CrossRef]
- Ogulata, R.T.; Mavruz, S. Investigation of Porosity and Air Permeability Values of Plain Knitted Fabrics. FIBRES TEXTILES East. Eur. 2010, 18, 71–75. [Google Scholar]
- Neupane, B.B.; Mainali, S.; Sharma, A.; Giri, B. Optical microscopic study of surface morphology and filtering efficiency of face masks. PeerJ 2019, 7, e7142. [Google Scholar] [CrossRef]
- World Health Organization. Mask Use in the Context of COVID-19: Interim Guidance, 1 December 2020; World Health Organization: Geneva, Switzerland, 2020.
- CDC. Science Briefs|CDC. 2020. Available online: https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/ (accessed on 15 January 2023).
- Rengasamy, S.; Eimer, B.; Shaffer, R. Simple Respiratory Protection—Evaluation of the Filtration Performance of Cloth Masks and Common Fabric Materials Against 20–1000 nm Size Particles. Ann. Occup. Hyg. 2010, 54, 789–798. [Google Scholar] [CrossRef]
- Zhao, M.; Liao, L.; Xiao, W.; Yu, X.; Wang, H.; Wang, Q.; Lin, Y.L.; Kilinc-Balci, F.S.; Price, A.; Chu, L.; et al. Household Materials Selection for Homemade Cloth Face Coverings and Their Filtration Efficiency Enhancement with Triboelectric Charging. Nano Lett. 2020, 20, 5544–5552. [Google Scholar] [CrossRef]
- Verma, S.; Dhanak, M.; Frankenfield, J. Visualizing the effectiveness of face masks in obstructing respiratory jets. Phys. Fluids 2020, 32, 061708. [Google Scholar] [CrossRef]
- Ghatak, B.; Banerjee, S.; Ali, S.B.; Bandyopadhyay, R.; Das, N.; Mandal, D.; Tudu, B. Design of a self-powered triboelectric face mask. Nano Energy 2020, 79, 105387. [Google Scholar] [CrossRef]
- Das, A.; Alagirusamy, R. Improving tactile comfort in fabrics and clothing. In Improving Comfort in Clothing; Song, G., Ed.; Elsevier Masson SAS: Oxford, UK, 2011; pp. 216–244. [Google Scholar] [CrossRef]
- Sear, R.P.L.; de Anda, I.R.; Wilkins, J.W.; Robinson, J.F.; Royall, C.P. Modelling the Filltration Efficiency of a Woven Fabric: The Role of Multiple Lengthscales. Phys. Fluids. Available online: https://openresearch.surrey.ac.uk/esploro/outputs/journalArticle/Modelling-the-filltration-efficiency-of-a/99628465402346?institution=44SUR_INST (accessed on 22 January 2023).
- Hossain, T.; Liyanage, S.; Abidi, N. FTIR microspectroscopic approach to investigate macromolecular distribution in seed coat cross-sections. Vib. Spectrosc. 2022, 120, 103376. [Google Scholar] [CrossRef]
- Mansour, E.; Vishinkin, R.; Rihet, S.; Saliba, W.; Fish, F.; Sarfati, P.; Haick, H. Measurement of temperature and relative humidity in exhaled breath. Sens. Actuators B Chem. 2019, 304, 127371. [Google Scholar] [CrossRef]
- Liu, S.; Zheng, W.; Yang, B.; Tao, X. Triboelectric charge density of porous and deformable fabrics made from polymer fibers. Nano Energy 2018, 53, 383–390. [Google Scholar] [CrossRef]
- Application Note ITI-041. Mechanisms of Filtration for High Efficiency Fibrous. Available online: https://tsi.com/getmedia/d8a4412d-3050-41c8-9e89-bc3a20ffda4d/ITI-041?ext=.pdf (accessed on 2 January 2023).
- Chughtai, A.A.; Seale, H.; MacIntyre, C.R. Effectiveness of Cloth Masks for Protection Against Severe Acute Respiratory Syndrome Coronavirus 2. Emerg. Infect. Dis. 2020, 26, e200948. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Mishra, M.; Mudgal, S. Efficacy of cloth face mask in prevention of novel coronavirus infection transmission: A systematic review and meta-analysis. J. Educ. Health Promot. 2020, 9, 192. [Google Scholar] [CrossRef]
- Sousa-Pinto, B.; Fonte, A.P.; Eng, A.A.L.; Oliveira, B.M.; Fonseca, J.A.; Costa-Pereira, A.; Correia, O. Face masks for community use: An awareness call to the differences in materials. Respirology 2020, 25, 894–895. [Google Scholar] [CrossRef]
- Mueller, A.V.; Eden, M.J.; Oakes, J.M.; Bellini, C.; Fernandez, L.A. Quantitative Method for Comparative Assessment of Particle Removal Efficiency of Fabric Masks as Alternatives to Standard Surgical Masks for PPE. Matter 2020, 3, 950–962. [Google Scholar] [CrossRef]
- Whiley, H.; Keerthirathne, T.P.; Nisar, M.A.; White, M.A.F.; Ross, K.E. Viral Filtration Efficiency of Fabric Masks Compared with Surgical and N95 Masks. Pathogens 2020, 9, 762. [Google Scholar] [CrossRef]
- Varallyay, C.; Li, N.; Case, B.; Wolf, B. Material Suitability Testing for Nonmedical Grade Community Face Masks to Decrease Viral Transmission During a Pandemic. Disaster Med. Public Health Prep. 2020, 15, e26–e32. [Google Scholar] [CrossRef]
- Standard Test Method for Determining the Initial Efficiency of Materials Used in Medical Face Masks to Penetration by Particulates Using Latex Spheres. Available online: https://www.astm.org/f2299_f2299m-03r17.html (accessed on 9 February 2023).
- What Are Microbes?—InformedHealth.org—NCBI Bookshelf. Available online: https://www.ncbi.nlm.nih.gov/books/NBK279387/ (accessed on 11 February 2023).
- Kalaycı, S.; Iyigundogdu, Z.U.; Yazici, M.M.; Asutay, A.B.; Demir, O.; Sahin, F. Evaluation of Antimicrobial and Antiviral Activities of Different Venoms. Infect. Disord.-Drug Targets 2016, 16, 44–53. [Google Scholar] [CrossRef]
- Balasubramaniam, B.; Prateek; Ranjan, S.; Saraf, M.; Kar, P.; Singh, S.P.; Thakur, V.K.; Singh, A.; Gupta, R.K. Antibacterial and Antiviral Functional Materials: Chemistry and Biological Activity toward Tackling COVID-19-like Pandemics. ACS Pharmacol. Transl. Sci. 2020, 4, 8–54. [Google Scholar] [CrossRef]
- Pollard, Z.A.; Karod, M.; Goldfarb, J.L. Metal leaching from antimicrobial cloth face masks intended to slow the spread of COVID-19. Sci. Rep. 2021, 11, 19216. [Google Scholar] [CrossRef] [PubMed]
- Liyanage, S.; Parajuli, P.; Hossain, M.T.; Chaudhari, H.; Abidi, N. Antimicrobials for protective clothing. In Antimicrobial Textiles from Natural Resources; Elsevier: Amsterdam, The Netherlands, 2021; pp. 349–376. [Google Scholar]
- Jayakumar, R.; Menon, D.; Manzoor, K.; Nair, S.; Tamura, H. Biomedical applications of chitin and chitosan based nanomaterials—A short review. Carbohydr. Polym. 2010, 82, 227–232. [Google Scholar] [CrossRef]
- AFNOR. Barrier Masks___Guide to Minimum Requirements, Methods of Testing, Making and Use Serial Manufacture and Artisanal Making (or DIY). 2020. Available online: www.veritaszim.net (accessed on 15 January 2023).
- AATCC. AATCC-AATCC. 2020. Available online: https://members.aatcc.org/store/m014/3085/ (accessed on 15 January 2023).
- ASTM. Standard Test Method for Evaluating the Bacterial Filtration Efficiency (BFE) of Medical Face Mask Materials, Using a Biological Aerosol of Staphylococcus aureus. 2020. Available online: https://www.astm.org/f2101-22.html (accessed on 15 January 2023).
- Van Der Sande, M.; Teunis, P.; Sabel, R. Professional and Home-Made Face Masks Reduce Exposure to Respiratory Infections among the General Population. PLoS ONE 2008, 3, e2618. [Google Scholar] [CrossRef]
- Fischer, E.P.; Fischer, M.C.; Grass, D.; Henrion, I.; Warren, W.S.; Westman, E. Low-cost measurement of face mask efficacy for filtering expelled droplets during speech. Sci. Adv. 2020, 6, eabd3083. [Google Scholar] [CrossRef]
- MacIntyre, C.R.; Seale, H.; Dung, T.C.; Hien, N.T.; Nga, P.T.; Chughtai, A.A.; Rahman, B.; Dwyer, D.E.; Wang, Q. A cluster randomised trial of cloth masks compared with medical masks in healthcare workers. BMJ Open 2015, 5, e006577. [Google Scholar] [CrossRef] [PubMed]
- Courtney, J.M.; Bax, A. Hydrating the respiratory tract: An alternative explanation why masks lower severity of COVID-19. Biophys. J. 2021, 120, 994–1000. [Google Scholar] [CrossRef] [PubMed]
- Rovira, J.; Domingo, J.L. Human health risks due to exposure to inorganic and organic chemicals from textiles: A review. Environ. Res. 2018, 168, 62–69. [Google Scholar] [CrossRef]
- Bussan, D.D.; Snaychuk, L.; Bartzas, G.; Douvris, C. Quantification of trace elements in surgical and KN95 face masks widely used during the SARS-COVID-19 pandemic. Sci. Total Environ. 2021, 814, 151924. [Google Scholar] [CrossRef] [PubMed]
- Blevens, M.S.; Pastrana, H.F.; Mazzotta, H.C.; Tsai, C.S.-J. Cloth Face Masks Containing Silver: Evaluating the Status. ACS Chem. Health Saf. 2021, 28, 171–182. [Google Scholar] [CrossRef]
- Tuñón-Molina, A.; Takayama, K.; Redwan, E.M.; Uversky, V.N.; Andrés, J.; Serrano-Aroca, Á. Protective Face Masks: Current Status and Future Trends. ACS Appl Mater Interfaces 2021, 13, 56725–56751. [Google Scholar] [CrossRef] [PubMed]
- Saleem, H.; Zaidi, S.J. Sustainable Use of Nanomaterials in Textiles and Their Environmental Impact. Materials 2020, 13, 5134. [Google Scholar] [CrossRef] [PubMed]
- Okuku, E.; Kiteresi, L.; Owato, G.; Otieno, K.; Mwalugha, C.; Mbuche, M.; Gwada, B.; Nelson, A.; Chepkemboi, P.; Achieng, Q.; et al. The impacts of COVID-19 pandemic on marine litter pollution along the Kenyan Coast: A synthesis after 100 days following the first reported case in Kenya. Mar. Pollut. Bull. 2020, 162, 111840. [Google Scholar] [CrossRef]
- Dharmaraj, S.; Ashokkumar, V.; Hariharan, S.; Manibharathi, A.; Show, P.L.; Chong, C.T.; Ngamcharussrivichai, C. The COVID-19 pandemic face mask waste: A blooming threat to the marine environment. Chemosphere 2021, 272, 129601. [Google Scholar] [CrossRef]
- De-La-Torre, G.E.; Aragaw, T.A. What we need to know about PPE associated with the COVID-19 pandemic in the marine environment. Mar. Pollut. Bull. 2020, 163, 111879. [Google Scholar] [CrossRef]




| Sample | No. of Layer | Fiber Content | Weight | Porosity% Mean ± SD n = 9 | Blocking Efficiency (%) at 25 mm High Momentum Droplet) | Breathability (mm/pa-s); Mean ± SD, n = 3 | ||
|---|---|---|---|---|---|---|---|---|
| (g/m2) | Minimum | Medium | Maximum | |||||
| Medical mask | - | Polypropylene | 53.9 | n/a | 96.4 | 98.5 | 99.9 | 1.83 ± 0.15 |
| Used shirt | 1 | 100% cotton | 114.2 | 0.7 ± 1 | 87.9 | 96.8 | 99.8 | 1.37 ± 0.06 |
| Used undershirt | 1 | 100% cotton | 111.5 | 4.5 ± 1 | 41.1 | 81.9 | 95.2 | 10.7 ± 0.66 |
| Used undershirt | 2 | 100% cotton | - | - | 78.3 | 94.1 | 98.3 | 5.53 ± 0.35 |
| Used undershirt | 3 | 100% cotton | - | - | 96.8 | 98.9 | 99.8 | 3.77 ± 0.06 |
| New t-shirt | 1 | 60/40% cotton/poly | 183.2 | 1.1 ± 0.3 | 42 | 83.1 | 98.3 | 7.23 ± 0.55 |
| New t-shirt | 2 | 60/40% cotton/poly | - | - | 94 | 98.1 | 99.6 | 3.87 ± 0.06 |
| New t-shirt | 3 | 60/40% cotton/poly | - | - | - | >98.1 | - | 2.63 ± 0.06 |
| Category of Chemicals Used in Fabrics | Restricted Chemical Compounds |
|---|---|
| Additives/Plasticizers | Flame retardants (polybrominated diphenyl ethers, Phthalates, organophosphate esters, hexabromocyclodecane, and Sb2O3). |
| Trace Elements | Metal complex dye (cobalt, copper, chromium, and lead), pigments, mordant, antimicrobials (nanoparticles of silver, titanium oxide, and zinc oxide), trace metals (Ag, Al, As, B, Ba, Be, Bi, Cd, Co, Cr, Cu, Fe, Hg, Mg, Mn, Mo, Ni, Pb, Sb, Sc, Se, Sm, Sn, Sr, Ti, Tl, V, and Zn) |
| Dyes | Aromatic Amine (azo), Quinoline and derivatives, bisphenols (BPAs), benzothiazoles (BTHs), and benzotriazoles (BTRs) |
| Nanoparticles | Carbon nanotubes, nanoclays, aluminum oxide, silicon dioxide, zinc oxide, titanium oxide, and silver. |
| Finishing agents | Formaldehydes (anti-creasing), nanoparticles (nano Ag), antimicrobial agents (Ag-coating) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Amin, M.; Hossain, M.T.; Tahir, M.; Wyman, D.; Kabir, S.M.F. A Critical Review on Reusable Face Coverings: Mechanism, Development, Factors, and Challenges. Textiles 2023, 3, 142-162. https://doi.org/10.3390/textiles3010011
Al-Amin M, Hossain MT, Tahir M, Wyman D, Kabir SMF. A Critical Review on Reusable Face Coverings: Mechanism, Development, Factors, and Challenges. Textiles. 2023; 3(1):142-162. https://doi.org/10.3390/textiles3010011
Chicago/Turabian StyleAl-Amin, Md, Md Tanjim Hossain, Muneeb Tahir, Diana Wyman, and S M Fijul Kabir. 2023. "A Critical Review on Reusable Face Coverings: Mechanism, Development, Factors, and Challenges" Textiles 3, no. 1: 142-162. https://doi.org/10.3390/textiles3010011
APA StyleAl-Amin, M., Hossain, M. T., Tahir, M., Wyman, D., & Kabir, S. M. F. (2023). A Critical Review on Reusable Face Coverings: Mechanism, Development, Factors, and Challenges. Textiles, 3(1), 142-162. https://doi.org/10.3390/textiles3010011








