A Case of COVID-Related MERS (Clinically Mild Encephalitis/Encephalopathy with a Reversible Splenial Lesion) with a Typical Imaging Course and Hyponatremia in Adults—A Case Report and Literature Review
Abstract
:1. Introduction
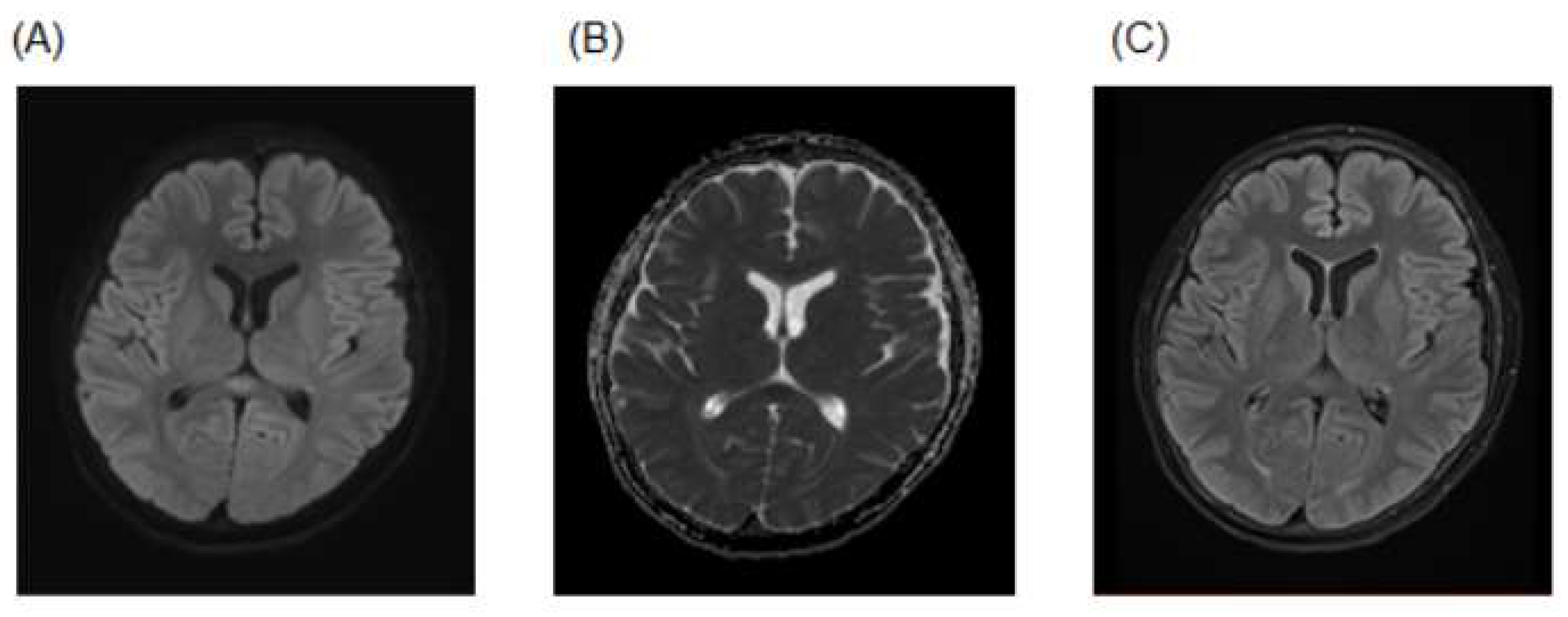
2. Case Presentation
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wu, C.; Chen, X.; Cai, Y.; Zhou, X.; Xu, S.; Huang, H.; Zhang, L.; Zhou, X.; Du, C.; Zhang, Y.; et al. Risk Factors Associated with Acute Respiratory Distress Syndrome and Death in Patients with Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern. Med. 2020, 180, 934–943. [Google Scholar] [CrossRef] [PubMed]
- Adachi, T.; Ayusawa, M.; Ujiie, M.; Omagari, T.; Oda, J.; Kato, Y.; Kamiya, H.; Kawana, A.; Kutsuna, S.; Kotani, T.; et al. Novel Coronavirus Infection COVID-19 Medical Practice Guidelines. Version 8.0. Available online: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000121431_00111.html (accessed on 24 August 2022).
- Tokano, M.; Takagi, R.; Kawano, M.; Maesaki, S.; Tarumoto, N.; Matsushita, S. Signaling via dopamine and adenosine receptors modulate viral peptide-specific and T-cell IL-8 response in COVID-19. Immunol. Med. 2022, 45, 162–167. [Google Scholar] [CrossRef] [PubMed]
- Paterson, R.W.; Brown, R.L.; Benjamin, L.; Nortley, R.; Wiethoff, S.; Bharucha, T.; Jayaseelan, D.L.; Kumar, G.; Raftopoulos, R.E.; Zambreanu, L.; et al. The emerging spectrum of COVID-19 neurology: Clinical, radiological and laboratory findings. Brain 2020, 143, 3104–3120. [Google Scholar] [CrossRef] [PubMed]
- Tada, H.; Takanashi, J.; Barkovich, A.J.; Oba, H.; Maeda, M.; Tsukahara, H.; Suzuki, M.; Yamamoto, T.; Shimono, T.; Ichiyama, T.; et al. Clinically mild encephalitis/encephalopathy with a reversible splenial lesion. Neurology 2004, 63, 1854–1858. [Google Scholar] [CrossRef] [PubMed]
- Takanashi, J.; Imamura, A.; Hayakawa, F.; Terada, H. Differences in the time course of splenial and white matter lesions in clinically mild encephalitis/encephalopathy with a reversible splenial lesion (MERS). J. Neurol. Sci. 2010, 292, 24–27. [Google Scholar] [CrossRef]
- Rasmussen, C.; Niculescu, I.; Patel, S.; Krishnan, A. COVID-19 and Involvement of the Corpus Callosum: Potential Effect of the Cytokine Storm? AJNR Am. J. Neuroradiol. 2020, 41, 1625–1628. [Google Scholar] [CrossRef]
- Junliang, Y.; Shuna, Y.; Shuangkun, W.; Wei, Q.; Lei, Y.; Wenli, H. Mild encephalitis/encephalopathy with reversible splenial lesion (MERS) in adults-a case report and literature review. BMC Neurol. 2017, 17, 103. [Google Scholar]
- Jay, S.; Kobayashi, N.; Numaguchi, Y.; Moritani, T. Cytotoxic Lesions of the Corpus Callosum That Show Restricted Diffusion: Mechanisms, Causes, and Manifestations. Radiographics 2017, 37, 562–576. [Google Scholar]
- Felipe, O.; Tiago, M.; Pedro, R.F. Transient lesion in the splenium of the corpus callosum associated with COVID-19. Arq. Neuropsiquiatr. 2020, 78, 738. [Google Scholar]
- Tania, R.; Krista, L.H.; Shahab, K.; Karim, R. Behavioral Changes Without Respiratory Symptoms as a Presenting Sign of COVID-19 Encephalitis. Cureus 2020, 12, e10469. [Google Scholar]
- Nivedita, A.; Rosella, M.; Giovanni, P.; Sabino, S. Unusual lesion in the splenium of the corpus callosum and coronavirus infectious disease-19. BJR Case Rep. 2020, 6, 20200068. [Google Scholar]
- Géraud, F.; Isaure, B.; Grégoire, B.; Grégoire, B. Cytotoxic lesion of the corpus callosum as presenting neuroradiological manifestation of COVID-2019 infection. J. Neurol. 2021, 268, 1595–1597. [Google Scholar]
- Laura, R.; Shivani, K.; Lala, P.; Stephanie, E.; Royce, L. Corpus Callosum Lesion Associated with COVID-19–Psychosis. Available online: https://www.consultant360.com/photoclinic/corpus-callosum-lesion-associated-covid-19-psychosis (accessed on 1 November 2022.).
- Gursoy, G.; Uzunalioglu, B.M.; Tunc, C.E.; Memis, Z.; Gocgun, N.; Zerdali, E.; Gonul, S.; Cokar, A.O. COVID-19 associated transient cytotoxic lesion of the corpus callosum: Report of two cases and current literature review. Haseki Tip Bulteni. 2021, 59, 50–53. [Google Scholar] [CrossRef]
- Esra, D.; Berna, A. Mild Encephalitis with Reversible Splenial Lesion Associated with COVID-19. Turk. J. Neurol. 2021, 27, 327–329. [Google Scholar]
- Eren, F.; Ozdemir, G.; Ildız, O.F.; Ergun, D.; Ozturk, S. Mild encephalopathy with reversible splenial lesion associated with SARS-CoV-2 infection: A case report. Neurology Asia. 2021, 26, 825–828. [Google Scholar] [CrossRef]
- Chevaliera, K.; Poillon, C. Brutal neurological disorder after SARS-CoV-2 infection. Rev. Med. Interne. 2022, 43, 385–386. [Google Scholar] [CrossRef]
- Jesús, G.C.; Cristina, U.C.; Ángel, M.M. Reversible Cytotoxic Lesion of the Corpus Callosum and COVID-19. Neurohospitalist 2022, 12, 585–586. [Google Scholar]
- Fatma, A.A.; Gönül, A.; Mustafa, Ç.; Niyazi, U.; Sibel, C.K. Isolated corpus callosum lesion associated with cytokine storm in COVID-19. Proc. (Bayl. Univ. Med. Cent.) 2022, 35, 337–338. [Google Scholar]
- Walid, E.; Fatma, B.A.; Naveed, A.; Mohamed, R.A.; Wanis, H.I. A 23-Year-Old Man with SARS-CoV-2 Infection Who Presented with Auditory Hallucinations and Imaging Findings of Cytotoxic Lesions of the Corpus Callosum (CLOCC). Am J Case Rep. 2020, 21, e928798. [Google Scholar]
- Misayo, H.; Yuki, S.; Yasutomo, B.; Hiroyuki, O.; Takayoshi, S. COVID-19-associated mild encephalitis/encephalopathy with a reversible splenial lesion. J. Neurol. Sci. 2020, 415, 116941. [Google Scholar]
- Benameur, K.; Agarwal, A.; Auld, S.C.; Butters, M.P.; Webster, A.S.; Ozturk, T.; Christina Howell, J.; Bassit, L.C.; Velasquez, A.; Schinazi, R.F.; et al. Encephalopathy and Encephalitis Associated with Cerebrospinal Fluid Cytokine Alterations and Coronavirus Disease, Atlanta, Georgia, USA, 2020. Emerg. Infect. Dis. 2020, 26, 2016–2021. [Google Scholar] [CrossRef] [PubMed]
- Edjlali, M.; Le Gal, A.; Louvet, M.; Matt, M.; Leveque, C.; Diffre, C.; Orlikowski, D.; Annane, D.; Carlier, R.-Y.; The Garches COVID-19 Collaborative Group. Teaching NeuroImages: Cytotoxic lesions of the corpus callosum in encephalopathic patients with COVID-19. Neurology 2020, 95, 1021–1022. [Google Scholar] [CrossRef] [PubMed]
- Klironomos, S.; Tzortzakakis, A.; Kits, A.; Öhberg, C.; Kollia, E.; Ahoromazdae, A.; Almqvist, H.; Aspelin, Å.; Martin, H.; Ouellette, R.; et al. Nervous System Involvement in Coronavirus Disease 2019: Results from a Retrospective Consecutive Neuroimaging Cohort. Radiology 2020, 297, E324–E334. [Google Scholar] [CrossRef] [PubMed]
- Kremer, S.; Lersy, F.; de Sèze, J.; Ferré, J.C.; Maamar, A.; Carsin-Nicol, B.; Collange, O.; Bonneville, F.; Adam, G.; Martin-Blondel, G.; et al. MRI Findings in Severe COVID-19: A Retrospective Observational Study. Radiology 2020, 297, E242–E251. [Google Scholar] [CrossRef]
- Kremer, S.; Lersy, F.; Anheim, M.; Merdji, H.; Schenck, M.; Oesterlé, H.; Bolognini, F.; Messie, J.; Khalil, A.; Gaudemer, A.; et al. Neurologic and neuroimaging findings in patients with COVID-19: A retrospective multicenter study. Neurology 2020, 95, e1868–e1882. [Google Scholar] [CrossRef]
- Chauffier, J.; Poey, N.; Husain, M.; De Broucker, T.; Khalil, A.; Lariven, S.; Henry-Feugeas, M.C. First Case of Mild Encephalopathy with Reversible Splenial Lesion in SARS-CoV-2 Infection. Infect. Dis. Now. 2021, 51, 99–101. [Google Scholar] [CrossRef]
- Altmann, K.; Koziol, K.; Palaver, A.; Frisch, G.; Pfausler, B.; Helbok, R.; Kampfl, A. Cytotoxic Edema Involving the Corpus Callosum and Middle Cerebellar Peduncles in a Young Patient with Mild COVID-19. Neurology 2022, 10, 1212. [Google Scholar] [CrossRef]
- Al-Edrus, S.A.; Norzaini, R.; Chua, R.; Puvanarajah, S.; Shuguna, M.; Muda, S. Reversible splenial lesion syndrome in neuroleptic malignant syndrome. Biomed Imaging Interv J. 2009, 5, e24. [Google Scholar] [CrossRef]
- Jialu, X.; Feng, G.; Zhefeng, Y.; Lihua, J.; Zhezhi, X.; Zhengyan, Z. Mild encephalitis/encephalopathy with a reversible splenial lesion (MERS) associated with bacteria meningitis caused by listeria monocytogenes: A case report. Medicine 2018, 97, e11561. [Google Scholar]
- Kometani, H.; Kawatani, M.; Ohta, G.; Okazaki, S.; Ogura, K.; Yasutomi, M.; Tanizawa, A.; Ohshima, Y. Marked elevation of interleukin-6 in mild encephalopathy with a reversible splenial lesion (MERS) associated with acute focal bacterial nephritis caused by Enterococcus faecalis. Brain Dev. 2014, 36, 551–553. [Google Scholar] [CrossRef]
- Shi, B.C.; Li, J.; Jiang, J.W.; Li, M.X.; Zhang, J.; Shang, X.L. Mild encephalitis/encephalopathy with a reversible splenial lesion secondary to encephalitis complicated by hyponatremia: A case report and literature review. Medicine 2019, 98, e17982. [Google Scholar] [CrossRef] [PubMed]
- Goto, Y.; Kishida, K.; Nakasho, T.; Yamamoto, H.; Nakahara, Y. Reversible lesion of the splenium of the corpus callosum following traumatic brain injury: A case report. Neurotraumatology 2019, 42, 207–210. [Google Scholar]
- Galnares-Olalde, J.A.; Vázquez-Mézquita, A.J.; Gómez-Garza, G.; Reyes-Vázquez, D.; Higuera-Ortiz, V.; Alegría-Loyola, M.A.; Mendez-Dominguez, A. Cytotoxic Lesions of the Corpus Callosum Caused by Thermogenic Dietary Supplements. AJNR Am. J. Neuroradiol. 2019, 40, 1304–1308. [Google Scholar] [CrossRef] [PubMed]
- Takanashi, J.; Tada, H.; Maeda, M.; Suzuki, M.; Terada, H.; James, B.A. Encephalopathy with a reversible splenial lesion is associated with hyponatremia. Brain Dev. 2009, 31, 217–220. [Google Scholar] [CrossRef] [PubMed]

| References | Diagnosis | Age/Sex | Past History | Clinical Symptoms | Pneumonia (Chest CT) | Hypoxia | Bronchial Intubation and Mechanical Ventilation | Serum Sodium | CSF Examination | Brain MRI (Diffusion-Weighted Images) | Brain MRI (Apparent Diffusion Coefficient Map) | Brain MRI (Fluid-Attenuated Inversion Recovery) | Changes in Brain MRI over Time | Lesion Extension beyond the Corpus Callosum | Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| [10] | CLOCC | 40/m | None | Flu-like symptoms presenting progressive paresthesia in the extremities, mild headache and visual turbidity | Yes | No | No | N.d. | N.d. | High | Low | high | Follow-up MRI (1 month): complete regression of the corpus callosum lesion | No | Ivermectin and azithromycin | Recovery |
| [11] | CLOCC | 30’s/m | None | Behavioral changes. | Yes | Yes | Yes | N.d. | N.d. | High | Low | N.d. | Follow-up MRI (7 days): demonstrated marked progression of the restricted diffusion now involving the bilateral frontal, parietal temporal and occipital lobes as well as the corpus callosum and basal ganglia | Yes | Acyclovir, ceftriaxone and vancomycin | Death |
| [12] | CLOCC | 73/m | None | Mild influenza-like symptoms which rapidly progressed to respiratory distress, high fever (38℃) and altered consciousness (no focal symptoms) | Yes | Yes | Yes | N.d. | Normal | High | Low | N.d. | Follow-up MRI (5 weeks): focal residual hemosiderin deposits and myelomalacia in the former region of the hemorrhage | No | Darunavir/Cobicistat, antibiotics and hydroxychloroquine | Recovery |
| [13] | MERS | 55/m | None | Fever, minor headache, dizziness and impaired consciousness (no focal symptoms) | Yes | Yes | Yes | Normal | N.d. | High | Low | N.d. | Follow-up MRI (20 days): complete regression of the corpus callosum lesion | No | N.d. | Recovery |
| [14] | CLOCC | 20’s/f | Untreated depression | Auditory and visual hallucinations, paranoia and false beliefs of being a twin and pregnant (no focal symptoms) | N.d. | No | No | N.d. | Normal | High | N.d. | N.d. | Follow-up MRI (30 days): complete regression of the corpus callosum lesion | No | None | Recovery |
| [15] | CLOCC | 58/m | None | Weakness and malaise (no focal symptoms), | Yes | No | No | N.d. | N.d. | High | Low | N.d. | Follow-up MRI (half a month): complete regression of the corpus callosum lesion | No | N.d. | Recovery |
| occasional coughs and presyncope | ||||||||||||||||
| [16] | MERS | 50/m | None | Fever, nausea, vomiting, myalgias, hoarse voice, fatigue, cough and impaired consciousness; tandem gait was clumsy, Romberg sign was positive, and finger-to-nose testing was impaired | Yes | No | No | N.d. | Normal | High | Low | N.d. | Follow-up MRI (8 days): complete regression of the corpus callosum lesion | No | Ceftriaxone, acyclovir and low dose cortisone | Recovery |
| [17] | MERS | 47/m | None | Personality changes, confusion and aggression (no focal symptoms) | Yes | No | No | Normal | N.d. | High | Low | N.d. | Follow-up MRI (15 days): complete regression of the corpus callosum lesion | No | Prednisone | Recovery |
| [18] | CLOCC | 45/m | None | Left hemiparesis and psychomotor retardation (no focal symptoms) | N.d. | No | No | N.d. | N.d. | High | N.d. | High | Follow-up MRI (7 days): almost total regression of the initial pattern | Yes | None | Recovery |
| [19] | CLOCC | 62/m | Hypertension and diabetes mellitus | The patient did not present any neurological manifestation during hospitalization | N.d. | N.d. | N.d. | N.d. | Normal | High | Low | High | Follow-up MRI (3 months): complete regression of the corpus callosum lesion | No | N.d. | Recovery |
| [20] | CLOCC | 43/m | None | Fever, signs of upper respiratory tract infection, cough, dyspnea and speech disorder | Yes | N.d. | N.d. | N.d. | No pathology was found in the cerebrospinal fluid except for the protein height (143 mg/dL) | High | Low | N.d. | Follow-up MRI (40 days): complete regression of the corpus callosum lesion | No | Favipiravir, methylprednisolone and tocilizumab | Recovery |
| [7] | CLOCC | 66/m | Diabetes mellitus and hypertension | Right-sided weakness, decreased alertness and aphasic | Yes | Yes | Yes | N.d. | N.d. | High | N.d. | N.d. | N.d. | Yes | Azithromycin and hydroxychloroquine | Recovery |
| [21] | CLOCC | 23/m | None | Auditory hallucinations, fever, headache, restlessness and suicidal thoughts (no focal symptoms) | Yes | Yes | Yes | Normal | Normal | High | Low | N.d. | N.d. | No | Dexamethasone, favipiravir, piperacillin tazobactam and azithromycin | Death |
| [22] | MERS | 75/m | Mild Alzheimer’s disease | Altered sensorium, tremors, ataxia and urinary incontinence | Yes | No | No | Normal | N.d. | High | Low | N.d. | N.d. | No | Favipiravir, corticosteroid pulse, ciclesonide and meropenem | Death (Neurological symptoms resolved after 3 days) |
| [23] | CLOCC | 34/m | Hypertension | Fever, shortness of breath, cough, consciousness disturbance and myoclonus | Yes | Yes | Yes | N.d. | CSF showed a high opening pressure of 48 cm H2O, no pleocytosis, 27 erythrocytes/mL, a mildly increased protein level and glucose level within the reference range | High | N.d. | High | N.d. | No | Hydroxychloroquine | N.d. |
| [24] | CLOCC | 49/m | None | Confusion | N.d. | N.d. | N.d. | N.d. | N.d. | High | Low | N.d. | N.d. | No | N.d. | N.d. |
| CLOCC | 51/m | None | Confusion | N.d. | N.d. | N.d. | N.d. | N.d. | High | Low | N.d. | N.d. | No | N.d. | N.d. | |
| [25] | CLOCC | 40’s/f | N.d. | Consciousness and paretic extremities | N.d. | N.d. | N.d. | N.d. | N.d. | High | N.d. | N.d. | N.d. | No | N.d. | N.d. |
| [26] | CLOCC | 66/m | N.d. | Consciousness | N.d. | N.d. | N.d. | N.d. | N.d. | High | N.d. | N.d. | N.d. | No | N.d. | N.d. |
| [27] | CLOCC | 55/m | N.d. | N.d. | N.d. | N.d. | N.d. | N.d. | N.d. | High | N.d. | N.d. | N.d. | No | None | N.d. |
| [28] | MERS | 47/m | None | Confusion, fever, dry cough and headache (no focal symptoms) | Yes | Yes | No | Moderate hyponatremia | N.d. | High | N.d. | N.d. | N.d. | No | None | Recovery |
| [29] | CLOCC | 24/m | N.d. | Gait ataxia, scanning speech and otherwise unremarkable neurological examination | N.d. | No | No | N.d. | N.d. | High | Low | N.d. | N.d. | No | Intravenous immunoglobulin following methylprednisolone treatment | Recovery |
| This Case | MERS | 18/m | Orthostatic hypotension | Confusion | Yes | No | No | 128.9 mEq/L | Normal | High | Low | High | Follow-up MRI (11 days): complete regression of the corpus callosum lesion | No | Remdesivir | Recovery |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tokano, M.; Tarumoto, N.; Osawa, I.; Sakai, J.; Okada, M.; Seo, K.; Nakazato, Y.; Yamamoto, T.; Maeda, T.; Maesaki, S. A Case of COVID-Related MERS (Clinically Mild Encephalitis/Encephalopathy with a Reversible Splenial Lesion) with a Typical Imaging Course and Hyponatremia in Adults—A Case Report and Literature Review. COVID 2023, 3, 183-191. https://doi.org/10.3390/covid3020013
Tokano M, Tarumoto N, Osawa I, Sakai J, Okada M, Seo K, Nakazato Y, Yamamoto T, Maeda T, Maesaki S. A Case of COVID-Related MERS (Clinically Mild Encephalitis/Encephalopathy with a Reversible Splenial Lesion) with a Typical Imaging Course and Hyponatremia in Adults—A Case Report and Literature Review. COVID. 2023; 3(2):183-191. https://doi.org/10.3390/covid3020013
Chicago/Turabian StyleTokano, Mieko, Norihito Tarumoto, Iichiro Osawa, Jun Sakai, Mariko Okada, Kazuhide Seo, Yoshihiko Nakazato, Toshimasa Yamamoto, Takuya Maeda, and Shigefumi Maesaki. 2023. "A Case of COVID-Related MERS (Clinically Mild Encephalitis/Encephalopathy with a Reversible Splenial Lesion) with a Typical Imaging Course and Hyponatremia in Adults—A Case Report and Literature Review" COVID 3, no. 2: 183-191. https://doi.org/10.3390/covid3020013
APA StyleTokano, M., Tarumoto, N., Osawa, I., Sakai, J., Okada, M., Seo, K., Nakazato, Y., Yamamoto, T., Maeda, T., & Maesaki, S. (2023). A Case of COVID-Related MERS (Clinically Mild Encephalitis/Encephalopathy with a Reversible Splenial Lesion) with a Typical Imaging Course and Hyponatremia in Adults—A Case Report and Literature Review. COVID, 3(2), 183-191. https://doi.org/10.3390/covid3020013






