- Article
Psychometric Validation of the Fear of COVID-19 Scale (FCV-19S) in a US Academic Health Sciences Center
- Brandt Wiskur,
- Kavya Boyina and
- Michael W. Brand
- + 6 authors
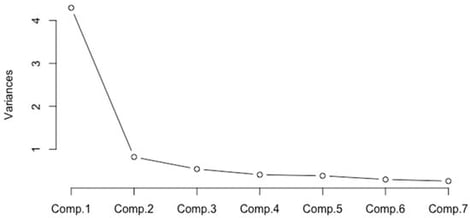
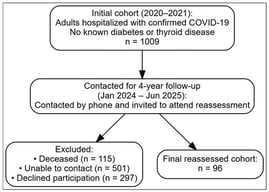
The COVID-19 pandemic (2020–2023) profoundly disrupted healthcare systems and imposed sustained psychological burdens on healthcare professionals and trainees. Reliable instruments are essential for assessing these impacts. This study evaluated the construct validity and reliability of the Fear of COVID-19 Scale (FCV-19S) in a convenience sample of 1761 healthcare professionals, trainees, and academic staff at a single U.S. academic health sciences center (the University of Oklahoma Health Campus). Participants completed the FCV-19S; confirmatory factor analysis (CFA) examined its dimensional structure; and internal consistency was assessed using Cronbach’s α and McDonald’s ω. The one-factor model demonstrated good internal consistency (α = 0.89; ω = 0.89) but exhibited sub-optimal model fit (CFI = 0.89; TLI = 0.83; SRMR = 0.06; RMSEA = 0.18). The two-factor model, distinguishing emotional and somatic fear, showed substantially improved fit (CFI = 0.97; TLI = 0.96; SRMR = 0.03; RMSEA = 0.09) and acceptable internal consistency for both factors (α = 0.85 and 0.86; ω = 0.85 and 0.87), although RMSEA remained above conventional thresholds for close fit. Overall, findings support a two-factor structure as a comparatively superior and more nuanced representation of fear responses among an academic health workforce. The validated FCV-19S offers a reliable tool for assessing COVID-19-related distress in clinical and educational health settings, informing targeted interventions to strengthen workforce resilience.
4 February 2026