Abstract
Research over the last several years has demonstrated a wide variety of inequalities in the COVID-19 pandemic by socio-demographic characteristics, place, and political and religious ideology. In this study, by combining several county-level data sources, we examine how the social conditions of counties across the United States relate to their differential COVID-19 mortality rates. We find that percent Black, percent Hispanic, and income inequality are all positively related to higher mortality rates at the county level. Moreover, the percentage of the population that voted for Trump in the 2020 election was a significant and substantively large predictor of higher mortality rates. We also include healthcare-related variables, but compared to the social circumstances of the pandemic, these effects are relatively small. These results indicate that the social conditions of areas are strong predictors of how counties have experienced the pandemic and where the greatest loss of life has occurred.
1. Introduction
On 27 February 2020, U.S. President Trump said in an address to the press, “It’s going to disappear. One day—it’s like a miracle—it will disappear. And from our shores, we—you know, it could get worse before it gets better. It could maybe go away. We’ll see what happens. Nobody really knows.” President Trump reiterated this sentiment many times in the months to follow, suggesting that the pandemic would not be that bad, or that it would be resolved shortly without much need for intervention [1]. However, as we now know, the pandemic would claim over a million lives (at the time of writing) and continues to be an ongoing public health crisis. Moreover, the toll of the pandemic has not been felt evenly across the population. Research has long demonstrated that socioeconomic and demographic variables such as race and income influence an individual’s health-related experiences in society [2,3,4]. The COVID-19 pandemic has been no exception to this pattern [5,6,7,8]. The purpose of this research is to expand this work to simultaneously examine a number of social and demographic variables in a regression analysis to examine how they relate to mortality rates across counties over the course of the pandemic.
In this exploratory study, we examine COVID-19 mortality rates at the county level. In particular, our research questions are: what ecological factors at the county level are related to higher COVID-19 mortality rates across the U.S. throughout the pandemic in 2020–2021? We consider traditional socio-demographic factors such as socio-economic standing and racial/ethnic composition. However, we also expand this literature by considering myriad other factors such as healthcare resources, religion, and political affiliation.
The pandemic years have been marked by a high degree of polarization in behaviors and policies to combat the effects of the virus. As a result, rates of infection, hospitalization, chronic disease, mortality, and vaccination have varied considerably across states and cities. While each of these has been studied to some degree in the robust body of work that has been published on the pandemic in the last few years [5,6,7,8], here we provide a more comprehensive test, which includes data up to the beginning of December 2021, when the Omicron variant became prevalent in the U.S. We also investigate the impact of political affiliation on COVID-19 mortality. This study contributes to the literature by focusing on the percentage of Trump voters, a political subgroup that is aligned with a distinct set of ideals and attitudes towards the pandemic. Moreover, other work connects support for Trump in the election with Christian nationalism [9]. Importantly, we also control for five years of previous mortality rates to account for pre-pandemic population health. Moreover, we focus on COVID-19 death rates as mortality reflects the most extreme outcome of the virus. This study contributes to this literature by exploring healthcare resources, religion, and political affiliation and by examining a more recent dataset of county-level mortality rates across the US.
1.1. The Socio-Demographic Gradient of COVID-19
With the rise of the COVID-19 global health crisis, an emerging body of literature has focused on translating our previous knowledge of the impact of socioeconomic and demographic factors on health outcomes, healthcare, and mortality to the novel case of COVID-19 [10,11]. Economic factors have been demonstrated to be a strong predictor of COVID-19 mortality. Geographic areas with higher levels of income inequality experience higher levels of mortality due to COVID-19 [5,6,12,13]. Moreover, socially vulnerable and disadvantaged communities with higher levels of poverty, crowded housing, and racial and ethnic minorities have disproportionately experienced the burden of COVID-19 [7,14,15,16,17,18,19,20,21,22].
The pandemic has been especially acute for people of color in the U.S., reflecting long-standing patterns of health inequalities by race in the U.S., with a large gap in outcomes by race [23,24,25]. Specifically, Black, Native American, and Hispanic populations have experienced higher rates of hospitalization and mortality due to COVID-19 compared to the White population in the U.S. [8,26,27,28,29,30,31,32]. Moreover, this literature also demonstrates that college-educated White individuals are especially advantaged and have experienced poor COVID-19 outcomes at a substantially lower rate than all other social groups [33,34].
Additionally, residential communities with high social vulnerability, residential segregation, and concentrated poverty that were densely populated prior to the COVID-19 pandemic experienced poorer outcomes throughout the pandemic, magnifying the health disparities among disadvantaged groups, including racial/ethnic minorities and low-income populations [35,36,37,38,39]. Racial and ethnic minority groups are also overrepresented in the essential worker labor-force sector and less likely to work from home, increasing their own and their household members’ risk of exposure to COVID-19 [5,13,40,41].
1.2. Political Views and the Political Environment
Consistent with past studies, COVID-19 research addresses the relationship between the COVID-19 burden and both state-level and county-level political environments and voting patterns [42,43,44,45,46,47,48]. On a county level, scholars deployed voting for Donald Trump in the 2016 election as a political measure, an indicator of political polarization, and oftentimes, a particular stance on mitigating measures during a pandemic [42,44,45,48,49]. This work suggests some association between COVID-19-related behaviors and outcomes. At the county level, early findings demonstrated there is not a direct association between Trump voters and negative COVID-19 tests or COVID-19-related mortality [44,45]. However, the rate of COVID-19-related mortality was demonstrated to be higher in counties with more negative SARS CoV-2 tests [44], and as there was an increase in COVID-19 mandates such as business closures, the number of COVID-19-related deaths increased in counties with greater levels of support for Trump [45].
More recent studies have tested the relationship between COVID-19 mortality and political partisanship across a more geographically and temporally diverse sample of COVID-19 mortality rates [42,47]. Research findings demonstrated support for earlier studies, and Democratic counties demonstrated higher rates of COVID-19-associated mortality early in the pandemic, compared with Republican counties [42,47]. However, by the beginning of November 2020, this relationship inverted, and COVID-19 mortality rates were higher in Republican counties than in Democratic counties [42,47]. Possible explanations suggested by this work include political party differences in the enforcement of preventive health behavior mandates such as masking and stay-at-home orders and individual-level political view differences in attitudes towards the pandemic.
Related to this, studies have also explored individual-level behavioral responses to governors’ mandates and suggest an association between political partisanship and engagement in COVID-19 preventive health behaviors such as social distancing and wearing a mask [46,50,51,52]. More specifically, counties with greater levels of Trump support showed lower levels of staying at home and higher levels of working out of the home during the pandemic [45,53]. Additionally, individual-level political party affiliation is a significant predictor of face mask wearing and perceptions of the efficacy of face masks in preventing the spread of COVID-19 [46,52] and risk perception of non-pharmaceutical interventions such as compliance with restriction of mobility and non-essential travel [51].
Taken together, this existing work on COVID-19 outcomes across the U.S. suggests strong patterns by a wide variety of social conditions and experiences. We hypothesize that COVID-19 mortality rates will be higher in counties with a higher percentage of minority populations (Black and Hispanic in particular), lower socio-economic status, higher rates of support for Trump in the 2020 election, and higher adherence to Evangelical Protestantism, net of health and healthcare factors. To expand on this work, we will consider cumulative COVID-19 mortality rates (up to 1 December 2021) in a spatial analysis of U.S. counties. Moreover, in addition to typical socioeconomic factors, we consider a wide range of social variables, including religion and politics to examine how these uniquely contributed to differences in mortality rates across the country. Further, we also control for the previous death rate and healthcare variables to focus on not just social vulnerability to all diseases/illnesses or age, but also to isolate what factors may be particularly salient to COVID-19 mortality rates.
2. Materials and Methods
Data for this study come from multiple sources, which we report in Table 1 for the sake of brevity. In the table, readers can also find a description of each variable. The main outcome is the COVID-19 death rate, measured as cumulative COVID-19 deaths per 100,000 population as of 1 December 2021. The source of this measure is USAFacts, which compiles data from the Centers for Disease Control and Prevention, and public health agencies at the state and local levels [54]. Consistent with the discussion above, we measure several socio-economic traits that are relevant to COVID-19, specifically, the counties’ levels of income inequality, median household income, education, and rurality. We account for population size and density, the share of Black and Hispanic populations, and the share of the population over 85. We measure counties’ ideologies by using the share of Trump voters in the 2020 presidential elections [55] and evangelical protestants [56]. We attempt to account for several health and healthcare metrics as well. Importantly, we use the all-cause death rate in 2014–2019 to capture pre-pandemic levels of community health. We also include the rate of mask usage [57], the share of the uninsured population, the rate of primary care physicians (measured at the state level), and the number of ICU beds. Finally, we would like to note variables sourced from the U.S. Census Bureau, USDA ERS, AAMC, and Kaiser Family Foundation were combined and made available by a group of researchers at Johns Hopkins University [58].

Table 1.
Data description and sources.
Our units of analysis are counties, which are spatial in nature and may have commonalities by region or state. Thus, we estimate a series of spatial error regression models as a statistical test of these associations, which include Z-tests for the regression coefficients using a 0.05 alpha level. We compare cumulative death rates from COVID-19 across U.S. counties given the substantial variation in the outcome by county. We first calculated univariate global Moran’s I scores for our dependent variable and each of our key independent variables and found significant spatial autocorrelation for these variables. Moreover, we found that the k-5 nearest neighbor spatial weight matrix was the distance-based spatial weight that best maximized Moran’s I across these variables [59]. Further, the LaGrange Multiplier statistics indicated that the spatial error model was preferred to the spatial lag model to contend with spatial autocorrelation in our data [59,60]. We also include Kelejian and Prucha robust standard errors to account for significant heteroscedasticity [61]. Of note, the term for lambda is large and statistically significant across all model specifications, suggesting that correlated errors in omitted variables may be a problem without the spatial error model. However, as a check on this choice of method, the ordinary least squares regression results were similar to what is presented here with only minor differences in effect sizes.
3. Results
Table 2 reports the descriptive statistics for the 3,023 counties included in the analysis. As of 1 December 2021, the average COVID-19 mortality rate was 286.78 deaths per 100,000 people. To provide some context, the CDC estimated heart disease to be the leading cause of death in 2020 with a crude rate of 211.50 deaths per 100,000 [62]. It is important to note that these two rates are calculated over different time periods. If we split our data into two periods, we have a COVID-19 death rate of 118.34 in 2020 (closer to the CDC estimate) and 168.43 in 2021. In any case, these numbers show that the COVID-19 death rate is high and has increased in the second year of the pandemic. Mortality by COVID-19 also shows a remarkable variation across counties with a standard deviation of 134.88.

Table 2.
Descriptive statistics.
Table 3 shows our full regression model with standardized regression coefficients, standard errors, Z-ratios, and confidence intervals to indicate significance. To ease comparisons of effects, we report standardized coefficients, which show the change in standard deviations in the outcome for an increase of one standard deviation in the predictors. Several variables present a statistically significant association with the COVID-19 crude death rate, with directions that are largely in line with the expectations set forth above. Two community socio-economic traits are significantly associated with the outcome: mortality is higher in more unequal and less educated counties. The population composition presents strong associations with COVID-19 mortality. Counties that have higher population density and a larger share of people above 85 have higher death rates. Importantly, counties that have a larger share of the Black population and people of Hispanic/Latino descent experienced higher mortality rates. This is an important finding, which is consistent with extant research and provides support to the theorized mechanisms linking structural racism to population health. In terms of ideology, communities that voted for Trump in larger numbers have higher COVID-19 mortality rates. Scholars have discussed at length how support for Trump’s ideology affected health-relevant behaviors, such as resistance to mask mandates and vaccine refusal, and our findings are consistent with these arguments.

Table 3.
Full model.
Finally, our model includes several variables that measure relevant health characteristics of the counties. The 2014–2019 age-adjusted death rate provides a robust assessment of pre-pandemic community health. It is crucial to account for general population health. COVID-19 tends to be more severe for immunocompromised individuals, thus it is reasonable to hypothesize that it would affect less healthy communities more severely. The overall pre-pandemic death rate is a synthetic measure that works as a proxy for other health variables not introduced in the model (e.g., obesity or smoking rates). As expected, the 2014–2019 death rate is strong and positively associated with COVID-19 mortality. Finally, two healthcare measures show significant associations with the outcome. First, the primary care physician rate, which is measured at the state level, is associated with lower mortality. Second, the share of the uninsured population is associated with higher mortality.
Figure 1 is a coefficient plot showing coefficient estimates and 95% confidence intervals for the full model (reported in Table 3) and the respective simple models. Given that these are standardized effects, we can also see their relative effect sizes. For example, the previous death rate and age above 85 were the strongest predictors in the model, perhaps unsurprisingly. However, aside from these, race/ethnicity (in terms of percent Hispanic and percent Black) and the percentage of the county that voted for Trump appear to be some of the strongest predictors in the model, even after accounting for a wide variety of variables related to the socio-demographic composition of the area and healthcare measures. It is also possible to notice that several associations were significant in the simple models but did not hold after controlling for the full set of variables (e.g., median household income, mask usage, and share of evangelicals). In some cases, there was a strong reduction of variable effects in the full model (e.g., education and share of uninsured). Interestingly, some associations became stronger in the full model suggesting that the relationship was suppressed in the simple models (e.g., the share of the Hispanic/Latino population and people above 85).
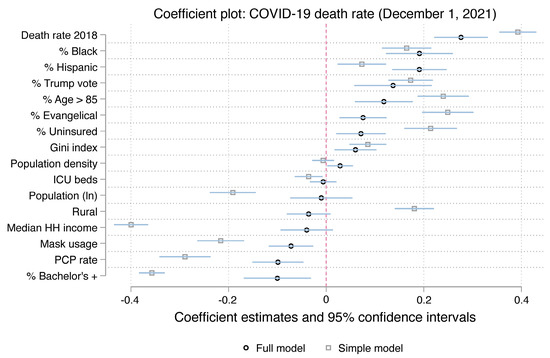
Figure 1.
Coefficient plot of full and simple models.
While our full model included numerous variables accounting for several dimensions, we are particularly interested in measures that reflect the racial and ideological systems that dramatically intensified COVID-19 mortality in the United States. Thus, we also present a parsimonious model with only four variables: Trump support to measure community ideology, the share of Black and Hispanic/Latino populations to assess the effect of structural racism, and the 2014–2019 death rate to account for pre-pandemic population health. Table 4 shows the parsimonious model results. All the variables are statistically significantly associated with the outcome. Counties with larger shares of Trump support and people of color experienced higher COVID-19 mortality, even after controlling for their pre-pandemic death rates. The effect of Trump support is particularly striking as it is quite close to the 2014–2019 death rate. Specifically, an increase of a standard deviation in the percentage of the population that voted for Trump is related to a 0.304 standard deviation increase in the mortality rate. This same figure is 0.374 for the 2014–2019 death rate. It is also worth noting that using these four variables alone accounts for a large part of the explained variation observed in the full model (35% vs. 44%).

Table 4.
Parsimonious model.
Figure 2 shows the coefficient plot for the parsimonious model. The effect of Trump-support, percent Black, and percent Hispanic/Latino increases in the parsimonious model showing how the joint use of these variables increases the predictive accuracy of the model [63].
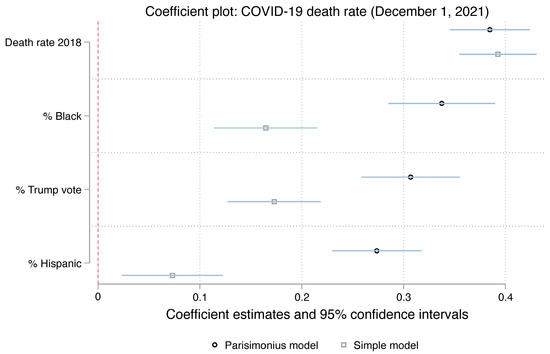
Figure 2.
Coefficient plot of parsimonious and simple models.
4. Discussion
The goal of this study is to examine the myriad social factors that may contribute to higher COVID-19 mortality rates across counties in the United States during the pandemic period. We found that several factors are related to higher mortality rates across counties and compared their relative effect sizes. In particular, we found that several dimensions of inequality are related to higher mortality rates, particularly race/ethnicity as measured by the percent Black and percent Hispanic, the Gini index for income inequality, and the percentage of people with a bachelor’s degree or higher. This is in keeping with the long tradition of racial/ethnic and socioeconomic disparities in health and in the case of the COVID-19 pandemic specifically [7,14,15,16,17,18,19,20,21,22].
Moreover, we find that two ideological variables are related to mortality rates. In particular, the percentage of people in the county who voted for Trump in the 2020 election was significant and positive and had a particularly high effect size relative to other variables, especially those with a positive relationship to the outcome. Much research since the beginning of the pandemic has demonstrated strong negative effects of support for Trump and a wide variety of measures indicating a willingness to engage in prophylactic measures, such as mask-wearing and vaccine uptake [43,44,45,46,48]. This finding extends that literature to the case of mortality specifically. Only two previous studies directly addressed the question of Trump support and mortality, and one found no direct association, only a moderating one in conjunction with other measures [45], while the other found a direct association with Republican voting patterns [47]. Here, we find a direct, and strong, association between the two variables. Further, we also examine religion with a score for the percentage of people who espouse Evangelical religious ideologies. In this case, we find an association with mortality only in the simple model, which drops to non-significance when accounting for all other variables in the model. This runs contrary to some work that has found an association between Evangelism and a number of pandemic-related outcomes [64,65,66,67,68]. However, this measure for religion is not particularly refined, as some scholars have noted that it is not simply Evangelicalism, but a particular brand of Christian nationalism that is related to resistance to mitigating measures in the pandemic [9,69]. Thus, perhaps in tandem with measures for Trump support and other forms of social inequality, the direct effect of religious affiliation is lost in this analysis.
Finally, we also examined a number of indicators of the healthcare system in the county that may be related to mortality specifically, not just infection, as they may serve as indicators of how well the system can handle an increased patient load or severity of the disease. While two of these are statistically significant in the models (percent uninsured and the rate of PCPs in the population), these are relatively weak effect sizes, and two of the included measures (mask usage and the number of ICU beds) are not significant at all in the full models. Thus, the social story of the pandemic, through the reproduction of social inequality and ideological patterns across counties, seems to be a more important predictor of how places have fared throughout the course of the pandemic in the United States.
Of course, this study is not without its limitations. Most notably, the measures included in this study are all at the county or, for one variable, the state level. This ignores the individual-level context that may relate to how people have made sense of the pandemic and how their own individual-level behaviors may have increased or decreased their own risk profile. The county is also a rather large spatial unit, and as such, potentially glosses over some important differences in neighborhood-level outcomes, exposures, and risks. Future work may benefit from a more fine-grained examination of how people in different contexts have contracted the virus, and who was at risk for experiencing mortality as a result. However, the goal here was to examine mortality rates throughout the pandemic as a population-level indicator and to examine a wide variety of independent variables that may help account for these differential rates.
In sum, when examining all of these factors jointly, we find some important patterns in county-level COVID-19 mortality, particularly in terms of social inequality and ideological considerations. This study identifies some key social and political factors, aside from healthcare, that are related to higher mortality rates from the disease. Unfortunately, in terms of public health interventions, these factors are particularly challenging to ameliorate. What these results demonstrate in terms of socio-demographic inequality is that the COVID-19 pandemic has been no exception to what public health scholars and social epidemiologists have been arguing for decades. After more than two years from the beginning of the pandemic, not only did the virus not “go away” [1], but the underlying social inequalities that enabled this catastrophe have become all the more evident. We must address systemic racial/ethnic and socioeconomic inequalities in health, especially as a fundamental cause of poor health. Moreover, the more recent trend of political and religious polarization in this county has rendered public health measures more difficult to implement. Without changes in these trends, we are likely to see more health inequalities in the future for this current pandemic as well as future health crises.
Author Contributions
Conceptualization, S.R.; Methodology, S.R. and K.F.A.; Formal analysis, S.R. and K.F.A.; Resources, C.W.; Writing—original draft, S.R., C.W. and K.F.A.; Writing—review & editing, S.R., C.W. and K.F.A.; Visualization, S.R.; Project administration, S.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data for this project from the Killeen et al. 2020 as referenced in the text can be found on the following Github webpage: https://github.com/JieYingWu/COVID-19_US_County-level_Summaries/tree/master/data (accessed on 3 December 2021).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Wolfe, D.; Dale, D. ‘It’s Going to Disappear’: A Timeline of Trump’s Claims That Covid-19 Will Vanish. CNN, 31 October 2020. [Google Scholar]
- Rask, K.; O’Malley, E.; Druss, B. Impact of socioeconomic, behavioral and clinical risk factors on mortality. J. Public Health 2009, 31, 231–238. [Google Scholar] [CrossRef]
- Lantz, P.M.; Golberstein, E.; House, J.S.; Morenoff, J. Socioeconomic and behavioral risk factors for mortality in a national 19-year prospective study of U.S. adults. Soc. Sci. Med. 2010, 70, 1558–1566. [Google Scholar] [CrossRef]
- Rogers, R.G.; Hummer, R.A.; Nam, C.B.; Peters, K. Demographic, Socioeconomic, and Behavioral Factors Affecting Ethnic Mortality by Cause. Soc. Forces 1996, 74, 1419–1438. [Google Scholar] [CrossRef]
- Oronce, C.I.A.; Scannell, C.A.; Kawachi, I.; Tsugawa, Y. Association Between State-Level Income Inequality and COVID-19 Cases and Mortality in the USA. J. Gen. Intern. Med. 2020, 35, 2791–2793. [Google Scholar] [CrossRef] [PubMed]
- Liao, T.F.; De Maio, F. Association of Social and Economic Inequality with Coronavirus Disease 2019 Incidence and Mortality Across US Counties. JAMA Netw. Open 2021, 4, e2034578. [Google Scholar] [CrossRef]
- Rifat, S.A.A.; Liu, W. One year into the pandemic: The impacts of social vulnerability on COVID-19 outcomes and urban–rural differences in the conterminous United States. Int. J. Environ. Health Res. 2022, 32, 2601–2619. [Google Scholar] [CrossRef] [PubMed]
- Tai, D.B.G.; Shah, A.; Doubeni, C.A.; Sia, I.G.; Wieland, M.L. The Disproportionate Impact of COVID-19 on Racial and Ethnic Minorities in the United States. Clin. Infect. Dis. 2021, 72, 703–706. [Google Scholar] [CrossRef]
- Perry, S.L.; Whitehead, A.L.; Grubbs, J.B. Culture Wars and COVID-19 Conduct: Christian Nationalism, Religiosity, and Americans’ Behavior During the Coronavirus Pandemic. J. Sci. Study Relig. 2020, 59, 405–416. [Google Scholar] [CrossRef]
- Bambra, C.; Riordan, R.; Ford, J.; Matthews, F. The COVID-19 pandemic and health inequalities. J. Epidemiol. Community Health 2020, 74, 964. [Google Scholar] [CrossRef]
- Krieger, N. ENOUGH: COVID-19, Structural Racism, Police Brutality, Plutocracy, Climate Change—And Time for Health Justice, Democratic Governance, and an Equitable, Sustainable Future. Am. J. Public Health 2020, 110, 1620–1623. [Google Scholar] [CrossRef]
- Sepulveda, E.R.; Brooker, A.-S. Income inequality and COVID-19 mortality: Age-stratified analysis of 22 OECD countries. SSM Popul. Health 2021, 16, 100904. [Google Scholar] [CrossRef]
- Tan, A.X.; Hinman, J.A.; Abdel Magid, H.S.; Nelson, L.M.; Odden, M.C. Association Between Income Inequality and County-Level COVID-19 Cases and Deaths in the US. JAMA Netw. Open 2021, 4, e218799. [Google Scholar] [CrossRef] [PubMed]
- Dasgupta, S.; Bowen, V.B.; Leidner, A.; Fletcher, K.; Musial, T.; Rose, C.; Cha, A.; Kang, G.; Dirlikov, E.; Pevzner, E.; et al. Association Between Social Vulnerability and a County’s Risk for Becoming a COVID-19 Hotspot—United States, 1 June–25 July 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1535–1541. [Google Scholar] [CrossRef] [PubMed]
- Khazanchi, R.; Beiter, E.R.; Gondi, S.; Beckman, A.L.; Bilinski, A.; Ganguli, I. County-Level Association of Social Vulnerability with COVID-19 Cases and Deaths in the USA. J. Gen. Intern. Med. 2020, 35, 2784–2787. [Google Scholar] [CrossRef]
- Wrigley-Field, E.; Garcia, S.; Leider, J.P.; Van Riper, D. COVID-19 Mortality at The Neighborhood Level: Racial And Ethnic Inequalities Deepened In Minnesota In 2020. Health Aff. 2021, 40, 1644–1653. [Google Scholar] [CrossRef]
- Freese, K.E.; Vega, A.; Lawrence, J.J.; Documet, P.I. Social Vulnerability Is Associated with Risk of COVID-19 Related Mortality in U.S. Counties with Confirmed Cases. J. Health Care Poor Underserved 2021, 32, 245–257. [Google Scholar] [CrossRef]
- Biggs, E.N.; Maloney, P.M.; Rung, A.L.; Peters, E.S.; Robinson, W.T. The Relationship Between Social Vulnerability and COVID-19 Incidence Among Louisiana Census Tracts. Front. Public Health 2021, 8, 617976. [Google Scholar] [CrossRef]
- Gaynor, T.S.; Wilson, M.E. Social Vulnerability and Equity: The Disproportionate Impact of COVID-19. Public Adm. Rev. 2020, 80, 832–838. [Google Scholar] [CrossRef]
- Kim, S.J.; Bostwick, W. Social Vulnerability and Racial Inequality in COVID-19 Deaths in Chicago. Health Educ. Behav. 2020, 47, 509–513. [Google Scholar] [CrossRef]
- Karaye, I.M.; Horney, J.A. The Impact of Social Vulnerability on COVID-19 in the U.S.: An Analysis of Spatially Varying Relationships. Am. J. Prev. Med. 2020, 59, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Bilal, U.; Tabb, L.P.; Barber, S.; Diez Roux, A.V. Spatial Inequities in COVID-19 Testing, Positivity, Confirmed Cases, and Mortality in 3 U.S. Cities. Ann. Intern. Med. 2021, 174, 936–944. [Google Scholar] [CrossRef]
- Garcia, M.A.; Homan, P.A.; García, C.; Brown, T.H. The Color of COVID-19: Structural Racism and the Disproportionate Impact of the Pandemic on Older Black and Latinx Adults. J. Gerontol. Ser. B 2021, 76, e75–e80. [Google Scholar] [CrossRef] [PubMed]
- Laster Pirtle, W.N. Racial Capitalism: A Fundamental Cause of Novel Coronavirus (COVID-19) Pandemic Inequities in the United States. Health Educ. Behav. 2020, 47, 504–508. [Google Scholar] [CrossRef]
- Wrigley-Field, E. US racial inequality may be as deadly as COVID-19. Proc. Natl. Acad. Sci. USA 2020, 117, 21854–21856. [Google Scholar] [CrossRef]
- Khanijahani, A.; Tomassoni, L. Socioeconomic and Racial Segregation and COVID-19: Concentrated Disadvantage and Black Concentration in Association with COVID-19 Deaths in the USA. J. Racial Ethn. Health Disparities 2022, 9, 367–375. [Google Scholar] [CrossRef]
- Laurencin, C.T.; Wu, Z.H.; Grady, J.J.; Wu, R.; Walker, J.M. Changes in COVID-19-Associated Deaths During a Year Among Blacks and Hispanics Compared to Whites in the State of Connecticut. J. Racial Ethn. Health Disparities 2022, 9, 2049–2055. [Google Scholar] [CrossRef] [PubMed]
- Marrett, C.B. Racial Disparities and COVID-19: The Social Context. J. Racial Ethn. Health Disparities 2021, 8, 794–797. [Google Scholar] [CrossRef] [PubMed]
- Mude, W.; Oguoma, V.M.; Nyanhanda, T.; Mwanri, L.; Njue, C. Racial disparities in COVID-19 pandemic cases, hospitalisations, and deaths: A systematic review and meta-analysis. J. Glob. Health 2021, 11, 05015. [Google Scholar] [CrossRef]
- Bassett, M.T.; Chen, J.T.; Krieger, N. Variation in racial/ethnic disparities in COVID-19 mortality by age in the United States: A cross-sectional study. PLoS Med. 2020, 17, e1003402. [Google Scholar] [CrossRef]
- Acosta, A.M.; Garg, S.; Pham, H.; Whitaker, M.; Anglin, O.; O’Halloran, A.; Milucky, J.; Patel, K.; Taylor, C.; Wortham, J.; et al. Racial and Ethnic Disparities in Rates of COVID-19–Associated Hospitalization, Intensive Care Unit Admission, and In-Hospital Death in the United States from March 2020 to February 2021. JAMA Netw. Open 2021, 4, e2130479. [Google Scholar] [CrossRef]
- Cordes, J.; Castro, M.C. Spatial analysis of COVID-19 clusters and contextual factors in New York City. Spat. Spatiotemporal Epidemiol. 2020, 34, 100355. [Google Scholar] [CrossRef]
- Feldman, J.M.; Bassett, M.T. Variation in COVID-19 Mortality in the US by Race and Ethnicity and Educational Attainment. JAMA Netw. Open 2021, 4, e2135967. [Google Scholar] [CrossRef]
- Wadhera, R.K.; Wadhera, P.; Gaba, P.; Figueroa, J.F.; Joynt Maddox, K.E.; Yeh, R.W.; Shen, C. Variation in COVID-19 Hospitalizations and Deaths Across New York City Boroughs. JAMA 2020, 323, 2192–2195. [Google Scholar] [CrossRef]
- Anderson, K.F.; Lopez, A.; Simburger, D. Racial/Ethnic Residential Segregation and the First Wave of SARS-CoV-2 Infection Rates: A Spatial Analysis of Four U.S. Cities. Sociol. Perspect. 2021, 64, 804–830. [Google Scholar] [CrossRef]
- Anderson, K.F.; Ray-Warren, D. Racial-Ethnic Residential Clustering and Early COVID-19 Vaccine Allocations in Five Urban Texas Counties. J. Health Soc. Behav. 2022, 63, 472–490. [Google Scholar] [CrossRef]
- Benfer, E.A.; Vlahov, D.; Long, M.Y.; Walker-Wells, E.; Pottenger, J.L.; Gonsalves, G.; Keene, D.E. Eviction, Health Inequity, and the Spread of COVID-19: Housing Policy as a Primary Pandemic Mitigation Strategy. J. Urban Health 2021, 98, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.; Grigsby-Toussaint, D.S. Housing stability and the residential context of the COVID-19 pandemic. Cities Health 2021, 5, S159–S161. [Google Scholar] [CrossRef]
- Kamis, C.; Stolte, A.; West, J.S.; Fishman, S.H.; Brown, T.; Brown, T.; Farmer, H.R. Overcrowding and COVID-19 mortality across U.S. counties: Are disparities growing over time? SSM Popul. Health 2021, 15, 100845. [Google Scholar] [CrossRef]
- Do, D.P.; Frank, R. The Diverging Impacts of Segregation on Obesity Risk by Nativity and Neighborhood Poverty Among Hispanic Americans. J. Racial Ethn. Health Disparities 2020, 7, 1214–1224. [Google Scholar] [CrossRef]
- McCormack, G.; Avery, C.; Spitzer, A.K.-L.; Chandra, A. Economic Vulnerability of Households with Essential Workers. JAMA 2020, 324, 388–390. [Google Scholar] [CrossRef]
- Chen, H.-F.; Karim, S.A. Relationship between political partisanship and COVID-19 deaths: Future implications for public health. J. Public Health 2022, 44, 716–723. [Google Scholar] [CrossRef]
- Neelon, B.; Mutiso, F.; Mueller, N.T.; Pearce, J.L.; Benjamin-Neelon, S.E. Associations Between Governor Political Affiliation and COVID-19 Cases, Deaths, and Testing in the U.S. Am. J. Prev. Med. 2021, 61, 115–119. [Google Scholar] [CrossRef]
- Robertson, L.S. Association of COVID-19 mortality with politics and on-demand testing in 217 U.S. counties. BMC Public Health 2021, 21, 2203. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Radford, B.J. Death by political party: The relationship between COVID-19 deaths and political party affiliation in the United States. World Med. Health Policy 2021, 13, 224–249. [Google Scholar] [CrossRef] [PubMed]
- Grossman, G.; Kim, S.; Rexer, J.M.; Thirumurthy, H. Political partisanship influences behavioral responses to governors’ recommendations for COVID-19 prevention in the United States. Proc. Natl. Acad. Sci. USA 2020, 117, 24144–24153. [Google Scholar] [CrossRef] [PubMed]
- Sehgal, N.J.; Yue, D.; Pope, E.; Wang, R.H.; Roby, D.H. The Association Between COVID-19 Mortality and The County-Level Partisan Divide In The United States. Health Aff. 2022, 41, 853–863. [Google Scholar] [CrossRef]
- Yamey, G.; Gonsalves, G. Donald Trump: A political determinant of covid-19. BMJ 2020, 369, m1643. [Google Scholar] [CrossRef]
- Gonzalez, K.E.; James, R.; Bjorklund, E.T.; Hill, T.D. Conservatism and infrequent mask usage: A study of US counties during the novel coronavirus (COVID-19) pandemic. Soc. Sci. Q. 2021, 102, 2368–2382. [Google Scholar] [CrossRef] [PubMed]
- Howard, M.C. Are face masks a partisan issue during the COVID-19 pandemic? Differentiating political ideology and political party affiliation. Int. J. Psychol. 2022, 57, 153–160. [Google Scholar] [CrossRef]
- Hsiehchen, D.; Espinoza, M.; Slovic, P. Political partisanship and mobility restriction during the COVID-19 pandemic. Public Health 2020, 187, 111–114. [Google Scholar] [CrossRef]
- Kemmelmeier, M.; Jami, W.A. Mask Wearing as Cultural Behavior: An Investigation Across 45 U.S. States During the COVID-19 Pandemic. Front. Psychol. 2021, 12, 648692. [Google Scholar] [CrossRef]
- Huang, Q.; Jackson, S.; Derakhshan, S.; Lee, L.; Pham, E.; Jackson, A.; Cutter, S.L. Urban-rural differences in COVID-19 exposures and outcomes in the South: A preliminary analysis of South Carolina. PLoS ONE 2021, 16, e0246548. [Google Scholar] [CrossRef]
- USAFacts. Detailed Methodology and Sources: COVID-19 Data. 2020. Available online: https://usafacts.org/articles/detailed-methodology-covid-19-data/ (accessed on 3 December 2021).
- MIT Election Data and Science Lab. County Presidential Election Returns 2000–2020. 2018. Available online: https://electionlab.mit.edu/data (accessed on 20 July 2021).
- Grammich, C.; Hadaway, K.; Houseal, R.; Jones, D.; Krindatch, A.; Stanley, R.; Taylor, R. U.S. Religion Census Religious Congregations and Membership Study, 2010 (County File). 2018. Available online: https://www.usreligioncensus.org/images/2010_US_Religion_Census_Introduction.pdf (accessed on 20 July 2021).
- Dynata, The New York Times. Mask-Wearing Survey Data. 2020. Available online: https://github.com/nytimes/covid-19-data/blob/master/mask-use/README.md (accessed on 20 July 2021).
- Killeen, B.D.; Wu, J.Y.; Shah, K.; Zapaishchykova, A.; Nikutta, P.; Tamhane, A.; Chakraborty, S.; Wei, J.; Gao, T.; Thies, M.; et al. A County-Level Dataset for Informing the United States’ Response to COVID-19. arXiv 2020, arXiv:2004.00756. [Google Scholar]
- Anselin, L. Local Indicators of Spatial Association—LISA. Geogr. Anal. 1995, 27, 93–115. [Google Scholar] [CrossRef]
- Anselin, L.; Florax, R.J.G.M.; Rey, S.J. Advances in Spatial Econometrics: Methodology, Tools and Applications; Springer: Berlin/Heidelberg, Germany, 2004. [Google Scholar]
- Kelejian, H.H.; Prucha, I.R. Specification and estimation of spatial autoregressive models with autoregressive and heteroskedastic disturbances. J. Econom. 2010, 157, 53–67. [Google Scholar] [CrossRef]
- CDC. Underlying Cause of Death, 1999–2020. Available online: https://wonder.cdc.gov/controller/saved/D76/D266F024 (accessed on 22 April 2021).
- Kim, Y. The Causal Structure of Suppressor Variables. J. Educ. Behav. Stat. 2019, 44, 367–389. [Google Scholar] [CrossRef]
- Barmania, S.; Reiss, M.J. Health promotion perspectives on the COVID-19 pandemic: The importance of religion. Glob. Health Promot. 2020, 28, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Dein, S.; Loewenthal, K.; Lewis, C.A.; Pargament, K.I. COVID-19, mental health and religion: An agenda for future research. Ment. Health Relig. Cult. 2020, 23, 1–9. [Google Scholar] [CrossRef]
- DeFranza, D.; Lindow, M.; Harrison, K.; Mishra, A.; Mishra, H. Religion and reactance to COVID-19 mitigation guidelines. Am. Psychol. 2021, 76, 744–754. [Google Scholar] [CrossRef]
- Wildman, W.J.; Bulbulia, J.; Sosis, R.; Schjoedt, U. Religion and the COVID-19 pandemic. Relig. Brain Behav. 2020, 10, 115–117. [Google Scholar] [CrossRef]
- Vermeer, P.; Kregting, J. Religion and the Transmission of COVID-19 in The Netherlands. Religions 2020, 11, 393. [Google Scholar] [CrossRef]
- Perry, S.L.; Whitehead, A.L.; Grubbs, J.B. Save the Economy, Liberty, and Yourself: Christian Nationalism and Americans’ Views on Government COVID-19 Restrictions. Sociol. Relig. 2020, 82, 426–446. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).