Mitigating Social Isolation Following the COVID-19 Pandemic: Remedy Messages Shared by Older People
Abstract
1. Introduction
Guiding Conceptual Framework
2. Methods
2.1. Setting
2.2. Sample
2.3. Data Collection
2.4. Data Analysis
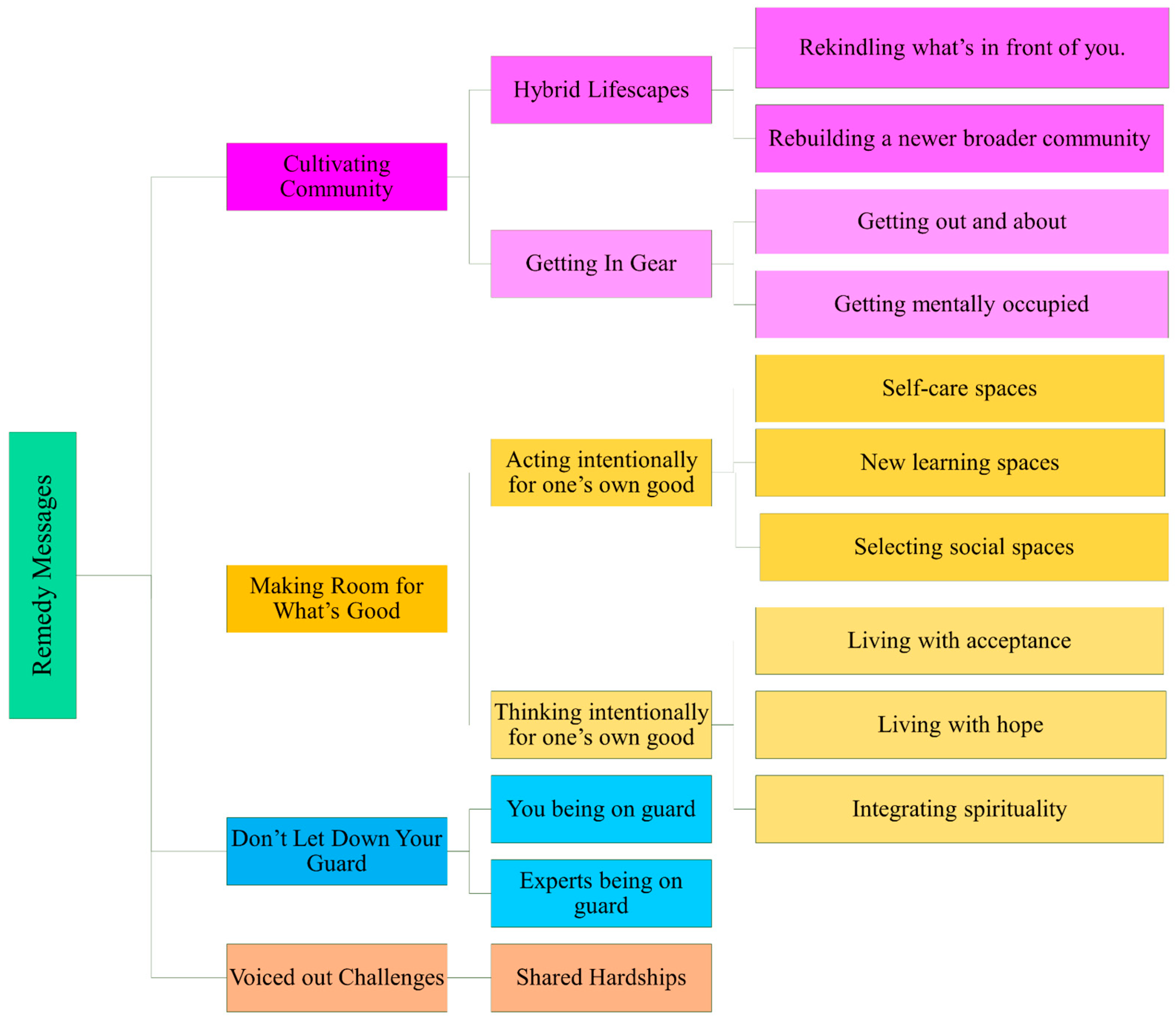
3. Results and Discussion
3.1. Sample Characteristics
3.2. Identified Categories of Content
3.2.1. Content Category 1: Cultivating Community
3.2.2. Content Category 2: Making Room for What Is Good
3.2.3. Content Category 3: Not Letting Your Guard Down
3.2.4. Content Category 4: Voicing out Challenges
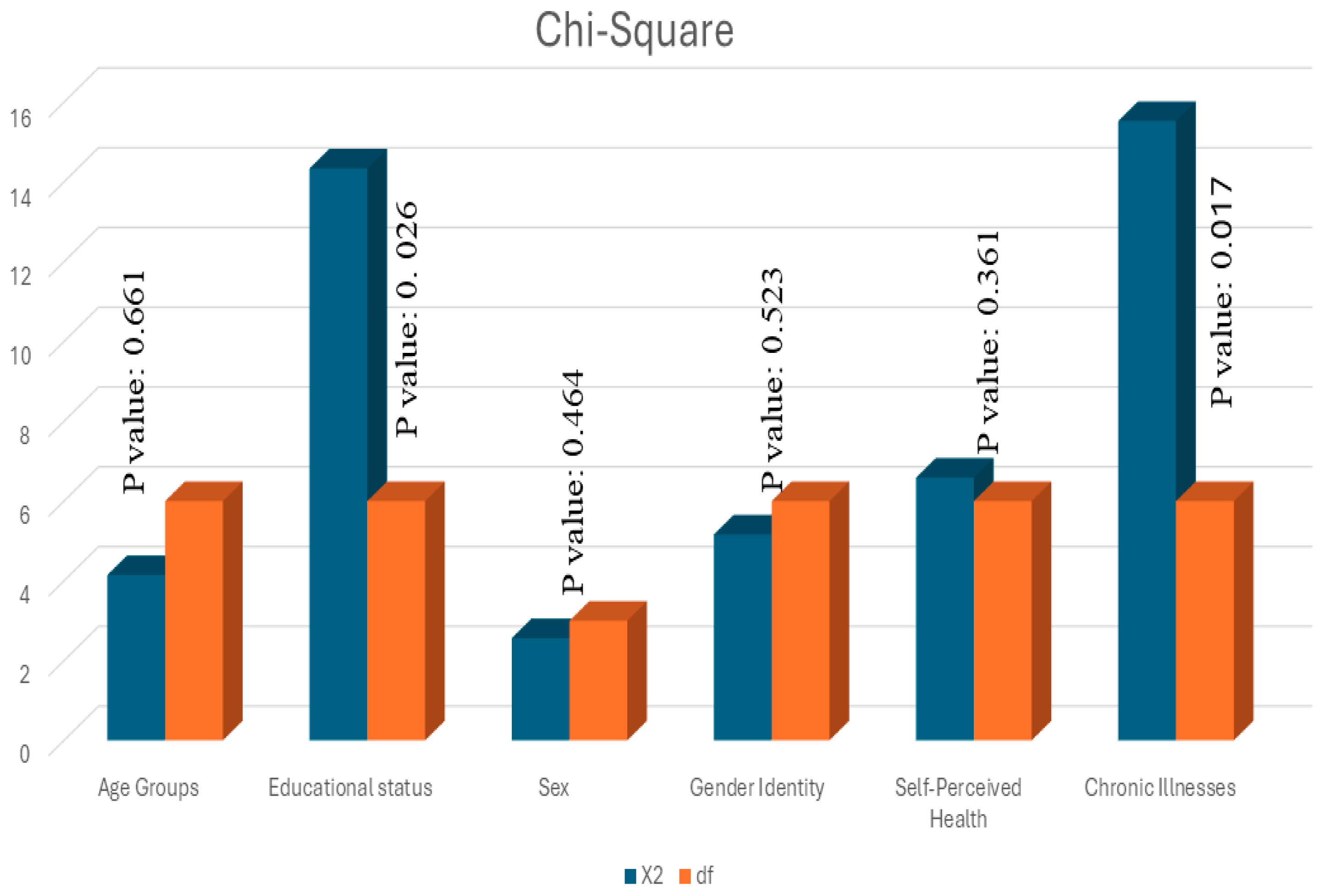
3.3. Between-Group Comparisons
4. Discussion
4.1. Main Findings and Interpretation
4.2. Public Health Implications
4.3. Limitations and Strengths
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. An Ad Hoc WHO Technical Consultation Managing the COVID-19 Infodemic: Call for Action. 2020. Available online: https://www.who.int/publications/i/item/9789240010314 (accessed on 1 May 2024).
- World Health Organization. Mental Health and Psychosocial Considerations during COVID-19. 2020. Available online: https://www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf (accessed on 30 April 2024).
- World Health Organization. Coronavirus Disease (COVID-19) Advice for the Public: MythBusters. 2022. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters (accessed on 4 May 2024).
- Center for Addiction and Mental Health. Coping with Stress and Anxiety. 2024. Available online: https://www.camh.ca/en/health-info/mental-health-and-covid-19/coping-with-stress-and-anxiety (accessed on 30 April 2024).
- Government of Canada. Cases by Age and Gender: Figure 4. Age and Gender Distribution of COVID-19 Cases in Canada as of March 9, 2024 (n = 4,525,785); Government of Canada: Ottawa, ON, Canada, 2024; Available online: https://health-infobase.canada.ca/covid-19/current-situation.html#figure6-header (accessed on 30 April 2024).
- Hobfoll, S.; Watson, P.; Bell, C.C.; Bryant, R.A.; Brymer, M.J.; Friedman, M.J.; Friedman, M.; Gersons, B.P.R.; de Jong, J.T.V.M.; Layne, C.M.; et al. Five Essential Elements of Immediate and Mid-Term Mass Trauma Intervention: Empirical Evidence. Psychiatry 2007, 70, 283–315. [Google Scholar] [CrossRef] [PubMed]
- Cocuzzo, B.; Wrench, A.; O’Malley, C. Effects of COVID-19 on Older Adults: Physical, Mental, Emotional, Social, and Financial Problems Seen and Unseen. Cureus 2022, 14, e29493. [Google Scholar] [CrossRef] [PubMed]
- De Rubeis, V.; Anderson, L.N.; Khattar, J.; de Groh, M.; Jiang, Y.; Oz, U.E.; Basta, N.E.; Kirkland, S.; Wolfson, C.; Griffith, L.E.; et al. Stressors and Perceived Consequences of the COVID-19 Pandemic among Older Adults: A Cross-Sectional Study Using Data from the Canadian Longitudinal Study on Aging. CMAJ Open 2022, 10, 721–730. [Google Scholar] [CrossRef] [PubMed]
- Mental Health Research Canada. Mental Health during COVID-19 Outbreak: Poll #6—Full Report; Health Canada: Ottawa, ON, Canada, 2021; Available online: https://www.mhrc.ca/national-poll-covid/findings-of-poll-6 (accessed on 25 April 2024).
- Dong, L.; Yang, L. COVID-19 Anxiety: The Impact of Older Adults’ Transmission of Negative Information and Online Social Networks. Aging Health Res. 2023, 3, e100119. [Google Scholar] [CrossRef] [PubMed]
- Gutman, G.; de Vries, B.; Beringer, R.; Daudt, H.; Gill, P. COVID-19 Experiences and Advance Care Planning (ACP) among Older Canadians: Influence of Age, Gender and Sexual Orientation; SFU Gerontology Research Centre: Vancouver, BC, Canada, 2021; Available online: http://www.sfu.ca/lgbteol.html (accessed on 1 May 2024).
- Statistics Canada. Survey on COVID-19 and Mental Health, September to December 2020. 2021. Available online: https://www150.statcan.gc.ca/n1/daily-quotidien/210318/dq210318a-eng.htm (accessed on 20 April 2024).
- Donovan, N.J.; Blazer, D. Social Isolation and Loneliness in Older Adults: Review and Commentary of a National Academies Report. Am. J. Geriatr. Psychiatry 2020, 28, 1233–1244. [Google Scholar] [CrossRef] [PubMed]
- Freedman, A.; Nicolle, J. Social Isolation and Loneliness: The New Geriatric Giants: Approach for Primary Care. Can. Fam. Physician 2020, 66, 176–182. [Google Scholar] [PubMed]
- Smith, M.L.; Steinman, L.E.; Casey, E.A. Combating Social Isolation among Older Persons in a Time of Physical Distancing: The COVID-19 Social Connectivity Paradox. Front. Public Health 2020, 8, 403. [Google Scholar] [CrossRef] [PubMed]
- Murthy, V.H. Our Epidemic of Loneliness and Isolation. The U.S. Surgeon General’s Advisory on the Healing Effects of Social Connection and Community. 2023. Available online: https://www.hhs.gov/sites/default/files/surgeon-general-social-connection-advisory.pdf (accessed on 30 April 2024).
- National Institute on Ageing. Understanding Social Isolation and Loneliness among Older Canadians and How to Address It. 2022. Available online: https://cnpea.ca/images/socialisolationreport-final1.pdf (accessed on 3 May 2024).
- National Institute on Ageing; Telus Health. Pandemic Perspectives on Ageing in Canada in Light of COVID-19: Findings from a National Institute on Ageing/TELUS Health National Survey. 2020. Available online: https://static1.squarespace.com/static/5c2fa7b03917eed9b5a436d8/t/5f85fe24729f041f154f5668/1602616868871/PandemicPerspectives+oct13.pdf (accessed on 1 May 2024).
- Ooi, L.L.; Liu, L.; Roberts, K.C.; Gariépy, G.; Capaldi, C.A. Social Isolation, Loneliness and Positive Mental Health among Older Adults in Canada during the COVID-19 Pandemic. Health Promot. Chronic Dis. Prev. Can. 2023, 43, 171–181. [Google Scholar] [CrossRef] [PubMed]
- Su, Y.; Rao, W.; Li, M.; Caron, G.; D’Arcy, C.; Meng, X. Prevalence of Loneliness and Social Isolation among Older Persons during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Int. Psychogeriatr. 2023, 35, 229–241. [Google Scholar] [CrossRef]
- World Health Organization. Statement on the Fifteenth Meeting of the IHR (2005) Emergency Committee on the COVID-19 Pandemic. 2024. Available online: https://www.who.int/news/item/05-05-2023-statement-on-the-fifteenth-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-coronavirus-disease-(covid-19)-pandemic (accessed on 22 April 2024).
- World Health Organization. Social Isolation and Loneliness. 2024. Available online: https://www.who.int/teams/social-determinants-of-health/demographic-change-and-healthy-ageing/social-isolation-and-loneliness (accessed on 4 May 2024).
- Ehni, H.J.; Wahl, H.W. Six Propositions against Ageism in the COVID-19 Pandemic. J. Aging Soc. Policy 2020, 32, 515–525. [Google Scholar] [CrossRef]
- Lagacé, M.; O’Sullivan, T.; Dangoisse, P.; Mac, M.; Oostander, S.; Doucet, A. A Case Study on Ageism during the COVID-19 Pandemic; Prepared for Employment and Social Development Canada: Gatineau, QC, Canada, 2022; Available online: https://publications.gc.ca/site/eng/9.910866/publication.html (accessed on 10 April 2024).
- United Nations Department of Economic and Social Affairs; United Nations Institute for Training and Research. Stakeholder Engagement. 2020. Available online: https://sdgs.un.org/stakeholders (accessed on 10 April 2024).
- Stangl, A.L.; Earnshaw, V.A.; Logie, C.H.; van Brakel, W.; Simbayi, L.C.; Barré, I. The Health Stigma and Discrimination Framework: A Global, Crosscutting Framework to Inform Research, Intervention Development, and Policy on Health-Related Stigmas. BMC Med. 2019, 17, 31. [Google Scholar] [CrossRef] [PubMed]
- Tsutsumimoto, K.; Doi, T.; Makizako, H.; Hotta, R.; Nakakubo, S.; Kim, M.; Kurita, S.; Suzuki, T.; Shimada, H. Social Frailty Has a Stronger Impact on the Onset of Depressive Symptoms than Physical Frailty or Cognitive Impairment: A 4-Year Follow-Up Longitudinal Cohort Study. J. Am. Med. Dir. Assoc. 2018, 19, 504–510. [Google Scholar] [CrossRef] [PubMed]
- Sepúlveda-Loyola, W.; Rodríguez-Sánchez, I.; Pérez-Rodríguez, P.; Ganz, F.; Torralba, R.; Oliveira, D.V.; Rodríguez-Mañaz, L. Impact of Social Isolation due to COVID-19 on Health in Older People: Mental and Physical Effects and Recommendations. J. Nutr. Health Aging 2020, 24, 938–947. [Google Scholar] [CrossRef]
- Röhr, S.; Reininghaus, U.; Riedel-Heller, S.G. Mental Wellbeing in the German Old Age Population Largely Unaltered during COVID-19 Lockdown: Results of a Representative Survey. BMC Geriatr. 2020, 20, 489. [Google Scholar] [CrossRef]
- Raina, P.; Wolfson, C.; Griffith, L.; Kirkland, S.; McMillan, J.; Basta, N.; Joshi, D.; Erbas Oz, U.; Sohel, N.; Maimon, G.; et al. A Longitudinal Analysis of the Impact of the COVID-19 Pandemic on the Mental Health of Middle-aged and Older Adults from the Canadian Longitudinal Study on Aging. Nat. Aging 2021, 1, 1137–1147. [Google Scholar] [CrossRef] [PubMed]
- Robb, C.E.; de Jager, C.A.; Ahmadi-Abhari, S.; Giannakopoulou, P.; Udeh-Momoh, C.; McKeand, J.; Price, G.; Car, J.; Majeed, A.; Ward, H.; et al. Associations of Social Isolation with Anxiety and Depression during the Early COVID-19 Pandemic: A Survey of Older Persons in London, UK. Front. Psychiatry 2020, 11, 591120. [Google Scholar] [CrossRef]
- Carstensen, L.L.; Shavit, Y.Z.; Barnes, J.T. Age Advantages in Emotional Experience Persist even under Threat from the COVID-19 Pandemic. Psychol. Sci. 2020, 31, 1374–1385. [Google Scholar] [CrossRef]
- Müller, F.; Röhr, S.; Reininghaus, U.; Riedel-Heller, S.G. Social Isolation and Loneliness during COVID-19 Lockdown: Associations with Depressive Symptoms in the German Old-Age Population. Int. J. Environ. Res. Public Health 2021, 18, 3615. [Google Scholar] [CrossRef]
- Menze, I.; Mueller, P.; Mueller, N.G.; Schmicker, M. Age-Related Cognitive Effects of the COVID-19 Pandemic Restrictions and Associated Mental Health Changes in Germans. Sci. Rep. 2022, 12, 8172. [Google Scholar] [CrossRef]
- Canadian Mental Health Association. Policy Brief: COVID-19 and Mental Health: Heading off an Echo Pandemic; Canadian Mental Health Association: Toronto, ON, Canada, 2020; Available online: https://cmha.ca/brochure/covid-19-and-mental-health-heading-off-an-echo-pandemic/ (accessed on 20 October 2023).
- World Health Organization. World Mental Health Report: Transforming Mental Health for All. 2022. Available online: https://apps.who.int/iris/handle/10665/356119 (accessed on 1 April 2024).
- Canadian Coalition for Seniors’ Mental Health. Social Isolation and Loneliness in Older Adults: A Survey of Canadian Older Adults; Summary of Results; Canadian Coalition for Seniors’ Mental Health: Markham, ON, Canada, 2024; Available online: https://ccsmh.ca/wp-content/uploads/2024/01/CCSMH-Social-Isolation-Survey-Results-Report-by-older-adults-ENGLISH-1.pdf (accessed on 29 February 2024).
- Low, G.; Gutman, G.; Gao, Z.; França, A.; von Humboldt, S.; Vitorino, L.M.; Wilson, D.M.; Allana, H. Mentally Healthy Living after Pandemic Social Distancing: A Study of Older Canadians Reveals Helpful Anxiety Reduction Strategies. PubMed Central 2024, 24, 605–616. [Google Scholar] [CrossRef]
- Statistics Canada. 2016 Census Topic: Population and Dwelling Counts. 2017. Available online: https://www12.statcan.gc.ca/census-recensement/2016/rt-td/population-eng.cfm (accessed on 26 January 2022).
- Grady, A.; Stinchcombe, A. The Impact of COVID-19 on the Mental Health of Older Sexual Minority Canadians in the CLSA. BMC Geriatr. 2023, 23, 816–825. [Google Scholar] [CrossRef]
- Moreno, A.; Belhouari, S.; Dussault, A. A Systematic Literature Review of the Impact of COVID-19 on the Health of LGBTQIA+ Older Adults: Identification of Risk and Protective Health Factors and Development of a Model of Health and Disease. J. Homosex. 2024, 71, 1297–1331. [Google Scholar] [CrossRef] [PubMed]
- Statistics Canada. Dictionary, Census of Population 2021. 2022. Available online: https://www12.statcan.gc.ca/census-recensement/2021/ref/dict/index-eng.cfm (accessed on 26 January 2022).
- Elo, S.; Kyngäs, H. The Qualitative Content Analysis Process. J. Adv. Nurs. 2008, 62, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Kyngäs, H. Inductive Content Analysis. In The Application of Content Analysis in Nursing Science Research; Kyngäs, H., Mikkonen, K., Kääriäinen, M., Eds.; Springer: Cham, Switzerland, 2020; pp. 13–21. [Google Scholar] [CrossRef]
- NVIVO, Version 14.23.2; Lumivero: Denver, CO, USA, 2023. Available online: https://lumivero.com/shop/?Family=nvivo (accessed on 1 December 2023).
- Kim, H.Y. Statistical Notes for Clinical Researchers: Chi-Squared Test and Fisher’s Exact Test. Restor. Dent. Endod. 2017, 42, 152–155. [Google Scholar] [CrossRef] [PubMed]
- IBM SPSS Statistics for Windows, Version 29.01.0; IBM Corp.: Armonk, NY, USA, 2023. Available online: https://www.ibm.com/support/pages/downloading-ibm-spss-statistics-29 (accessed on 6 May 2024).
- Iftene, F.; Milev, R.; Farcas, A.; Squires, S.; Smirnova, D.; Fountoulakis, K.N. COVID-19 Pandemic: The Impact of COVID-19 on Mental Health and Life Habits in the Canadian Population. Front. Psychiatry 2022, 13, e871119. [Google Scholar] [CrossRef] [PubMed]
- Statistics Canada. Canada Is the First Country to Provide Census Data on Transgender and Non-Binary People. 2022. Available online: https://www150.statcan.gc.ca/n1/daily-quotidien/220427/dq220427b-eng.htm (accessed on 25 February 2024).
- Independent Panel for Pandemic Preparedness and Response. COVID-19: Make It the Last Pandemic. Available online: https://theindependentpanel.org (accessed on 6 January 2024).
- Government of Canada. What Did Canadians Do to Maintain Their Mental Health during the COVID-19 Pandemic? Government of Canada: Ottawa, ON, Canada, 2022; Available online: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/what-did-canadians-do-for-mental-health-during-covid-19.html (accessed on 20 November 2023).
- Cavallini, E.; Rosi, A.; van Vugt, F.T.; Ceccato, I.; Rapisarda, F.; Vallarino, M.; Ronchi, T.; Lecce, S. Closeness to Friends Explains Age Differences in Positive Emotional Experience during the Lockdown Period of COVID-19 Pandemic. Aging Clin. Exp. Res. 2021, 33, 2623–2631. [Google Scholar] [CrossRef] [PubMed]
- Derrer-Merk, E.; Ferson, S.; Mannis, A.; Bentall, R.P.; Bennett, K.M. Belongingness Challenged: Exploring the Impact on Older Persons during the COVID-19 Pandemic. PLoS ONE 2022, 17, e0276561. [Google Scholar] [CrossRef] [PubMed]
- Karmann, J.; Handlovsky, I.; Lu, S.; Moullec, G.; Frohlich, K.L.; Ferlatte, O. Resilience among Older Persons during the COVID-19 Pandemic: A Photovoice Study. SSM-Qual. Res. Health 2023, 3, 100256. [Google Scholar] [CrossRef]
- Hahmann, T.; du Plessis, V.; Fournier-Savard, P. Volunteering in Canada: Challenges and Opportunities during the COVID-19 Pandemic; Statistics Canada: Ottawa, ON, Canada, 2020; Available online: https://www150.statcan.gc.ca/n1/pub/45-28-0001/2020001/article/00037-eng.htm (accessed on 20 April 2024).
- Volunteer Canada; Volunteer Management Professionals of Canada; Spinktank. The Volunteering Lens of COVID-19: Fall 2020 Survey. Impacts of COVID-19 on Volunteer Engagement. 2020. Available online: https://volunteer.ca/index.php?MenuItemID=433 (accessed on 20 April 2024).
- Capaldi, C.A.; Dopko, R.L. Positive Mental Health and Perceived Change in Mental Health among Adults in Canada during the Second Wave of the COVID-19 Pandemic. Health Promot. Chronic Dis. Prev. Can. 2021, 41, 359–377. [Google Scholar] [CrossRef]
- Fiocco, A.J.; Gryspeerdt, C.; Franco, G. Stress and Adjustment during the COVID-19 Pandemic: A Qualitative Study on the Lived Experience of Canadian Older Persons. Int. J. Environ. Res. Public Health 2021, 18, 12922. [Google Scholar] [CrossRef]
- Rodney, Y. Volunteerism. In Crisis or at a Crossroads? The Philanthropist Journal: News and Analysis for the Non-Profit Sector. 2023. Available online: https://volunteer.ca/vdemo/ResearchAndResources_DOCS/Vol%20Lens%202020%20Survey%20Results/VC_FallSurveyReport_2020_ENG_FINAL.pdf (accessed on 30 April 2024).
- Lachance, E.L. COVID-19 and Its Impact on Volunteering: Moving towards Virtual Volunteering. Leis. Sci. 2020, 43, 104–110. [Google Scholar] [CrossRef]
- Moyser, M. Gender Differences in Mental Health during the COVID-19 Pandemic; Statistics Canada: Ottawa, ON, Canada, 2020; Available online: https://publications.gc.ca/collections/collection_2020/statcan/45-28/CS45-28-1-2020-44-eng.pdf (accessed on 6 July 2023).
- Lesser, I.A.; Nijenhuis, C.P. The Impact of COVID-19 on Physical Activity Behavior and Well-Being of Canadians. Int. J. Environ. Behav. Res. 2020, 17, 3899. [Google Scholar] [CrossRef] [PubMed]
- Herron, R.V.; Newall, N.E.G.; Lawrence, B.C.; Ramsey, D.; Waddell, C.M.; Dauphinais, J. Conversations in Times of Isolation: Exploring Rural-Dwelling Older Persons’ Experiences of Isolation and Loneliness during the COVID-19 Pandemic in Manitoba, Canada. Int. J. Environ. Res. Public Health 2021, 18, 3028. [Google Scholar] [CrossRef] [PubMed]
- von Humboldt, S.; Mendoza-Ruvalcaba, N.; Arias-Merino, E.; Ribeiro-Gonçalves, J.A.; Cabras, E.; Low, G.; Leal, I.P. The Upside of Negative Emotions: How Do Older Persons from Different Cultures Challenge Their Self-Growth during the COVID-19 Pandemic? Front. Psychol. 2022, 13, e648078. [Google Scholar] [CrossRef] [PubMed]
- Thauvoye, E.; Vanhooren, S.; Vandenhoeck, A.; Dezutter, J. Spirituality and Well-Being in Old Age: Exploring the Dimensions of Spirituality in Relation to Late-Life Functioning. J. Relig. Health 2018, 57, 2167–2181. [Google Scholar] [CrossRef] [PubMed]
- Kornadt, A.; Albert, I.; Hoffmann, M.; Murdock, E.; Nell, J. Perceived Ageism during the COVID-19-Crisis Is Longitudinally Related to Subjective Perceptions of Aging. Front. Public Health 2021, 9, 679711. [Google Scholar] [CrossRef] [PubMed]
- von Humboldt, S.; Low, G.; Leal, I. Health Service Accessibility, Mental Health and Changes in Behavior during the COVID-19 Pandemic: A Qualitative Study with Older Persons. Int. J. Environ. Res. Public Health 2022, 19, 4277. [Google Scholar] [CrossRef] [PubMed]
- Koenig, H.G. Maintaining Health and Well-Being by Putting Faith into Action during the COVID-19 Pandemic. J. Relig. Health 2020, 59, 2205–2214. [Google Scholar] [CrossRef]
- Mukhtar, S. Mental Health and Psychosocial Aspects of Coronavirus Outbreak in Pakistan: Psychological Intervention for Public Mental Health Crisis. Asian J. Psychiatry 2020, 51, 102069. [Google Scholar] [CrossRef]
- Rossi, R.; Jannini, T.B.; Socci, V.; Pacitti, F.; Di Lorenzo, G.D. Stressful Life Events and Resilience during the COVID-19 Lockdown Measures in Italy: Association with Mental Health Outcomes and Age. Front. Psychiatry 2021, 12, 635832. [Google Scholar] [CrossRef]
- McFadden, S.H. Pandemic Disruptions of Older Adults’ Meaningful Connections: Linking Spirituality and Religion to Suffering and Resilience. Religions 2022, 13, 622. [Google Scholar] [CrossRef]
- Upenieks, L. Religious/Spiritual Struggles and Well-Being during the COVID-19 Pandemic: Does “Talking Religion” Help or Hurt? Rev. Relig. Res. 2022, 64, 249–278. [Google Scholar] [CrossRef] [PubMed]
- Detsky, A.S.; Bogoch, I.I. COVID-19 in Canada—The Fourth through Seventh Waves. JAMA Health Forum 2022, 3, e224160. [Google Scholar] [CrossRef] [PubMed]
- Lytle, A.; Apriceno, M.B.; Macdonald, J.; Monahan, C.; Levy, S.R. Pre-Pandemic Ageism toward Older Adults Predicts Behavioral Intentions during the COVID-19 Pandemic. J. Gerontol. B Psychol. Sci. Soc. Sci. 2022, 77, e11–e15. [Google Scholar] [CrossRef] [PubMed]
- Werner, P.; AboJabel, H. The Conceptual and Methodological Characteristics of Ageism during COVID-19: A Scoping Review of Empirical Studies. Gerontologist 2022, 63, 1526–1535. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Launches Commission to Foster Social Connection. 2023. Available online: https://www.who.int/news/item/15-11-2023-who-launches-commission-to-foster-social-connection (accessed on 5 April 2024).
- Phipps, D.; Cummins, J.; Pepler, D.; Craig, W.; Cardinal, S. The Co-Produced Pathway to Impact Describes Knowledge Mobilization Processes. J. Community Engagem. Scholarsh. 2016, 9, 31–40. [Google Scholar] [CrossRef]
- Low, G.; Gutman, G.; Gao, Z.; França, A.; von Humboldt, S.; Vitorino, L.M.; Wilson, D.M.; Allana, H. Cooking up Calm: Design Your Menu for Mentally Healthy Living in the Later Years; RTEORO: Edmonton, AB, Canada, 2023; Available online: https://rtoero.ca/wp-content/uploads/2023/09/cooking_up_calm_singles.pdf (accessed on 9 May 2024).
- Garcia, A.; Privott, C. Meal Preparation and Cooking Group Participation in Mental Health: A Community Transition. Food Stud. Interdiscip. J. 2023, 13, 85–101. [Google Scholar] [CrossRef]
- Choi, S. The Effects of Social Participation Restriction on Psychological Distress among Older Adults with Chronic Illness. J. Gerontol. Soc. Work 2020, 63, 850–863. [Google Scholar] [CrossRef]
- Lu, M.; Bronskill, S.E.; Strauss, R.; Boblitz, A.; Guan, J.; Im, J.H.B.; Rochon, P.A.; Grunier, A.; Savage, R.D. Factors Associated with Loneliness in Immigrant and Canadian-born Older Adults in Ontario, Canada: A Population-based Study. BMC Geriatr. 2023, 23, 380. [Google Scholar] [CrossRef]
- Ahn, J.; Falk, E.B.; Kang, Y. Relationships between Physical Activity and Loneliness: A Systematic Review of Intervention Studies. Curr. Res. Behav. Sci. 2024, 6, 100141. [Google Scholar] [CrossRef]
- RTOERO Foundation. Top 6 Reasons to CHIME IN. Available online: https://rtoero.ca/wp-content/uploads/2023/03/Top_6_Reasons_to_Chime_In_EN_FINAL-ua.pdf (accessed on 9 June 2024).
- Skevington, S.M.; Gunson, K.S.; O’Connell, K.A. Introducing the WHOQOL-SRPB BREF: Developing a Short-Form Instrument for Assessing Spiritual, Religious and Personal Beliefs within Quality of Life. Qual. Life Res. 2013, 22, 1073–1083. [Google Scholar] [CrossRef]
- Women’s College Hospital. There Is a Loneliness Epidemic among Older People in Canada. Available online: https://www.womenscollegehospital.ca/there-is-a-loneliness-epidemic-among-older-adults-in-canada/ (accessed on 5 March 2024).

| Characteristic | Number (%) |
|---|---|
| 60–69 years of age | 719 (54.5%) |
| 70–79 years of age | 395 (29.9%) |
| 80 years of age and older | 206 (15.6%) |
| Post-secondary degree/certificate | 681 (51.4%) |
| Secondary school diploma | 392 (29.6%) |
| No degree, certificate, or diploma | 251 (19.0%) |
| Female | 671 (52%) |
| Male | 620 (48%) |
| Cis-gendered woman | 502 (42%) |
| Cis-gendered man | 516 (43.1%) |
| Non-binary persons | 178 (14.9%) |
| No chronic illnesses | 507 (39.2%) |
| One chronic illness | 359 (27.7%) |
| Two or more chronic illnesses | 429 (33.1%) |
| Poor/fair perceived health | 407 (31.1%) |
| Good perceived health | 604 (46.1%) |
| Very good/excellent perceived health | 298 (22.8%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Low, G.; Humboldt, S.v.; Gutman, G.; Gao, Z.; Allana, H.; Naz, A.; Wilson, D.M.; Vastani, M. Mitigating Social Isolation Following the COVID-19 Pandemic: Remedy Messages Shared by Older People. COVID 2024, 4, 798-814. https://doi.org/10.3390/covid4060053
Low G, Humboldt Sv, Gutman G, Gao Z, Allana H, Naz A, Wilson DM, Vastani M. Mitigating Social Isolation Following the COVID-19 Pandemic: Remedy Messages Shared by Older People. COVID. 2024; 4(6):798-814. https://doi.org/10.3390/covid4060053
Chicago/Turabian StyleLow, Gail, Sofia von Humboldt, Gloria Gutman, Zhiwei Gao, Hunaina Allana, Anila Naz, Donna M. Wilson, and Muneerah Vastani. 2024. "Mitigating Social Isolation Following the COVID-19 Pandemic: Remedy Messages Shared by Older People" COVID 4, no. 6: 798-814. https://doi.org/10.3390/covid4060053
APA StyleLow, G., Humboldt, S. v., Gutman, G., Gao, Z., Allana, H., Naz, A., Wilson, D. M., & Vastani, M. (2024). Mitigating Social Isolation Following the COVID-19 Pandemic: Remedy Messages Shared by Older People. COVID, 4(6), 798-814. https://doi.org/10.3390/covid4060053







