Assessing the Intention to Use a First-Generation Vaccine against COVID-19 Using Quantile Regression: A Cross-Sectional Study in Spain
Abstract
:1. Introduction
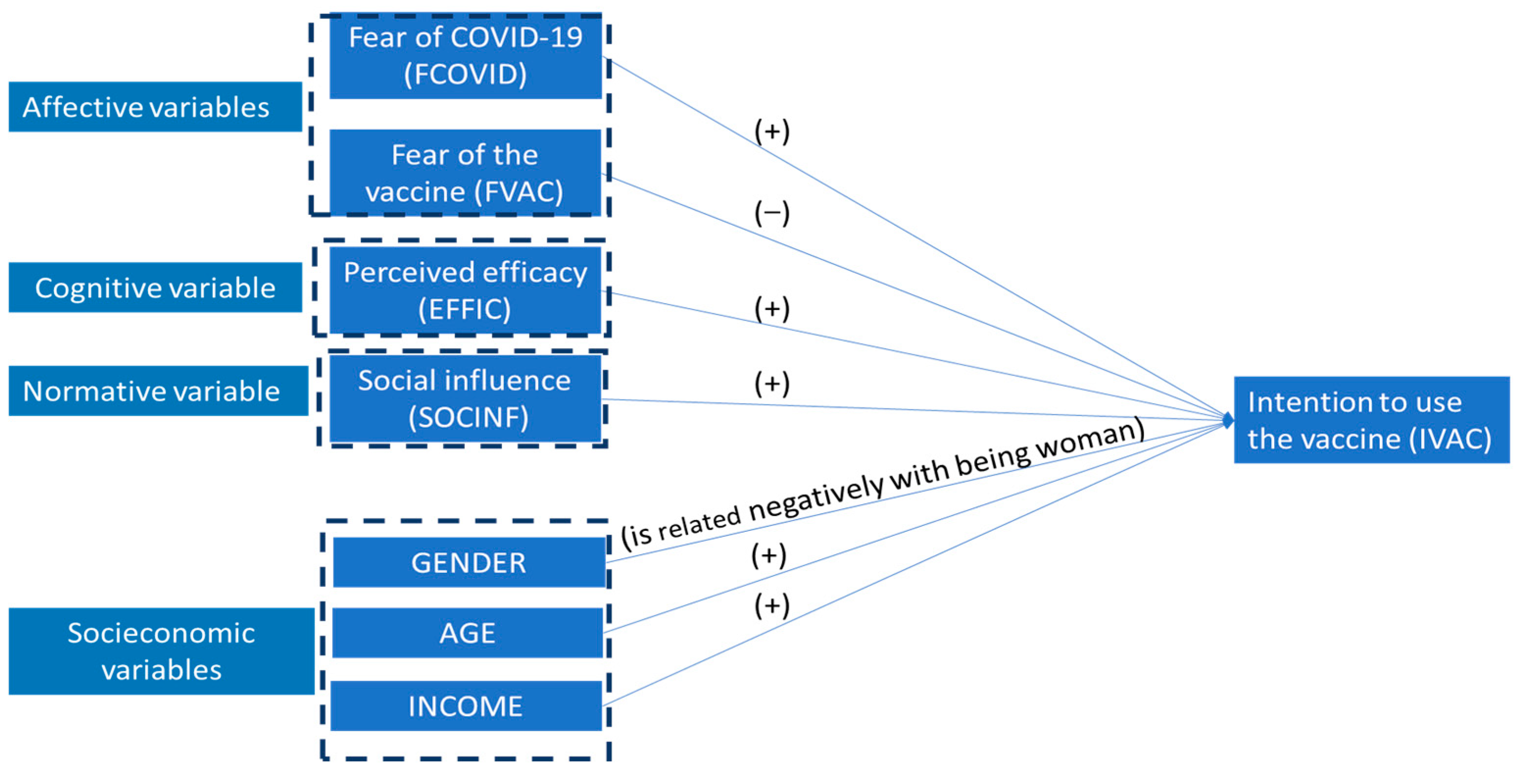
2. Theoretical Groundwork
2.1. Previous Considerations
2.2. Affective and Cognitive Variables
2.3. Normative Variable: Social Influence
2.4. Socioeconomic Variables
3. Materials and Methods
3.1. Sample and Sampling
- A common criterion is the completion of an a priori power analysis (β) for a predefined significance level (α), used to reject the null hypothesis that the proposed regression or the coefficient of interest is not significant [46]. This analysis was performed with the software GPower 3.1 [47]. Thus, we confirmed that this sample size ensured that the statistical power for testing both the overall significance of the model and the significance of the individual coefficients exceeded 99% at the 5% significance level.
- Second, with the software GPower 3.1, we found that the sample size was sufficient for analyzing small effect sizes (greater than 0.05). For a predefined statistical power level of β = 85% and a statistical significance level of α = 5%, the sample size was suitable for effect sizes of 0.021 for the coefficients and 0.036 for the overall regression model.
3.2. Measurement of Variables
| Variable | Item | Source |
|---|---|---|
| Intention to use AstraZeneca vaccine (IVAC) | IVAC1. I will try to get vaccinated with the Oxford-AstraZeneca vaccine. IVAC2. I will use the Oxford-AstraZeneca vaccine. | Based on [48] |
| Fear of COVID-19 (FCOVID) | FCOVID1: I will use the Oxford-AstraZeneca vaccine. FCOVID2. I am worried about transmitting COVID-19. | Based on [12] |
| Fear of AstraZeneca vaccine (FVAC) | FVAC1. I am worried about the temporary effects of the COVID-19 vaccine. FVAC2. I am worried about the permanent effects of the COVID-19 vaccine. | Based on [51] |
| Perceived efficacy (EFFIC) | EFFIC1. I am convinced of the efficacy of the Oxford vaccine. EFFIC2. The Oxford vaccine will protect me from COVID-19. EFFIC3. With the Oxford vaccine, I have a lower probability of contracting COVID-19. EFFIC4. The Oxford vaccine will prevent me from needing other treatments for COVID-19. | Based on [49,50] |
| Social influence (SOCINF) | SOCINF1. People who are important to me think I should use the Oxford vaccine. SOCINF2. People who influence me think I should use the Oxford vaccine. SOCINF3. People whose opinions I value think I should use the Oxford vaccine. | Based on [48] |
| SEX | Dichotomous variable coded 0 for men and 1 for women. | |
| AGE | Variable coded 0 for those under 40 years old and 1 for those over 60 years old. For those between 40 and 60 years old, it is linearly graduated in the interval [0, 1]. | |
| Net monthly income (INCOME) | Variable ranging from 0 (for monthly income less than EUR 1000) to 1 (for monthly income greater than EUR 3000). Between these income levels, it is linearly graduated. |
| Item | Mean | SD | Factor Loading | CA | CR | AVE |
|---|---|---|---|---|---|---|
| Intention to be vaccinated (IVAC) | 0.95 | 0.95 | 0.90 | |||
| IVAC1 | 5.07 | 3.48 | 0.95 | |||
| IVAC2 | 4.96 | 3.4 | 0.95 | |||
| Fear of COVID (FCOVID) | 0.734 | 0.883 | 0.799 | |||
| FCOVID1 | 6.60 | 2.72 | 0.889 | |||
| FCOVID2 | 7.86 | 2.74 | 0.889 | |||
| Fear of vaccine (FVAC) | 0.92 | 0.961 | 0.926 | |||
| FVAC1 | 6.75 | 3.02 | 0.962 | |||
| FVAC2 | 7.23 | 3.04 | 0.962 | |||
| Efficacy (EFFIC) | 0.933 | 0.953 | 0.836 | |||
| EFFIC1 | 4.93 | 2.81 | 0.920 | |||
| EFFIC2 | 5.31 | 2.80 | 0.950 | |||
| EFFIC3 | 5.95 | 2.97 | 0.935 | |||
| EFFIC4 | 4.89 | 2.94 | 0.849 | |||
| Social influence (SOCINF) | 0.971 | 0.981 | 0.945 | |||
| SOCINF1 | 4.85 | 2.95 | 0.964 | |||
| SOCINF2 | 4.64 | 2.95 | 0.979 | |||
| SOCINF3 | 4.68 | 3.03 | 0.974 |
3.3. Data Analysis
- First step. We verified the internal consistency and convergent validity of the scales used for the IVAC and CAN variables (FCOVID, FVAC, EFFIC, and SOCINF) using standard measures: Cronbach’s alpha (CA), convergent reliability (CR), average variance extracted (AVE), and factor loading.
- Second step. We quantified the variables involved in our analysis as follows:
- IVAC, FCOVID, FVAC, EFFIC, and SOCINF were quantified as the standardized scores obtained via factor analysis.
- SEX was a dummy variable which took a value of 1 if the observation came from a woman and was 0 otherwise.
- AGE: We based our approach on the fact that the probability of suffering a severe illness or even death due to contracting SARS-CoV-2 increases with age in individuals older than 40 years [45]. Therefore, we transformed age into a value in the interval [0, 1] as follows:
- Here, x is the age (in years) of the surveyed person.
- INCOME was obtained by transforming the categories in Figure 1 into a value within the [0, 1] interval:
- Here, y is the monthly income.
- Third step. We fitted a linear regression to IVAC via OLS, which was explained by FVAC, FCOVID, EFFIC, SOCINF, SEX, AGE and INCOME:IVAC = a0 + a1 × FVAC + a2 × FCOVID + a3 × EFFIC + a4 × SOCINF + a5 × SEX + a6 × AGE + a7 × INCOME
- Fourth step. We estimated the same quantile regression model as in the third step for various probability levels: τ = 0.2, 0.25, 0.3, 0.45, 0.5, 0.55, 0.7, 0.75, and 0.8. This allowed us to assess the influence of the variables near the central positions of the intention to use the vaccine for τ = 0.45, 0.5, and 0.55 and to evaluate the influence of the factors on responses which showed strong rejection (intention to use) compared with the central tendency for τ = 0.2, 0.25, and 0.3 (τ = 0.7, 0.75, and 0.8).
4. Results
5. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- OMS. Coronavirus Disease COVID-19. 2021. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 3 June 2024).
- World Bank Global Economic Prospects. January 2021. Available online: https://www.worldbank.org/en/publication/global-economic-prospects (accessed on 3 June 2024).
- Massó-Guijarro, E. Infancia y pandemia: Crónica de una ausencia anunciada. Salud Colect. 2021, 17, e3303. [Google Scholar] [CrossRef] [PubMed]
- Machingaidze, S.; Wiysonge, C.S. Understanding COVID-19 vaccine hesitancy. Nat. Med. 2021, 27, 1338–1339. [Google Scholar] [CrossRef]
- Nehal, K.R.; Steendam, L.M.; Campos Ponce, M.; van der Hoeven, M.; Smit, G.S.A. Worldwide Vaccination Willingness for COVID-19: A Systematic Review and Meta-Analysis. Vaccines 2021, 9, 1071. [Google Scholar] [CrossRef] [PubMed]
- Pelegrín-Borondo, J.; Reinares-Lara, E.; Olarte-Pascual, C.; Garcia-Sierra, M. Assessing the moderating effect of the end user in consumer behavior: The acceptance of technological implants to increase innate human capacities. Front. Psychol. 2016, 7, 132. [Google Scholar] [CrossRef]
- Pelegrín-Borondo, J.; Arias-Oliva, M.; Almahameed, A.A.; Román, M.P. Covid-19 Vaccines: A Model of Acceptance Behavior in the Healthcare Sector. Eur. Res. Manag. Bus. Econ. 2021, 27, 100171. [Google Scholar] [CrossRef]
- Koenker, R.; Bassett, G., Jr. Regression quantiles. Econometrica 1978, 46, 33–50. [Google Scholar] [CrossRef]
- Cade, B.S.; Noon, B.R. A gentle introduction to quantile regression for ecologists. Front. Ecol. Environ. 2003, 1, 412–420. [Google Scholar] [CrossRef]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User Acceptance of Information Technology: Toward a Unified View. MIS Q. 2003, 27, 425–478. [Google Scholar] [CrossRef]
- Andrés Sánchez, J.; Arias-Oliva, M.A.; Pelegrín-Borondo, J.P.; Lima-Rúa, O. Factores explicativos de la aceptación de la vacuna para el SARS-CoV-2 desde la perspectiva del comportamiento del consumidor. Rev. Esp. Sal. Púb. 2021, 95, 103. Available online: https://www.sanidad.gob.es/biblioPublic/publicaciones/recursos_propios/resp/revista_cdrom/VOL95/ORIGINALES/RS95C_202107101.pdf (accessed on 3 June 2024).
- Nguyen, T.T.M.; Lafond, K.E.; Nguyen, T.X.; Tran, P.D.; Nguyen, H.M.; Ha, V.T.C.; Do, T.T.; Ha, N.T.; Seward, J.F.; McFarland, J.W. Acceptability of seasonal influenza vaccines among health care workers in Vietnam in 2017. Vaccine 2020, 38, 2045–2050. [Google Scholar] [CrossRef]
- Harapan, H.; Wagner, A.L.; Yufika, A.; Winardi, W.; Anwar, S.; Gan, A.K.; Setiawan, A.M.; Rajamoorthy, Y.; Sofyan, H.; Mudatsir, M. Acceptance of a COVID-19 vaccine in Southeast Asia: A cross-sectional study in Indonesia. Front. Public Health 2020, 8, 381. [Google Scholar] [CrossRef] [PubMed]
- Njororai, F.J.; Amulla, W.; Nyaranga, C.K.; Cholo, W.; Adekunle, T. A Qualitative Exploration of Factors Associated with COVID-19 Vaccine Uptake and Hesitancy in Selected Rural Communities in Kenya. COVID 2024, 4, 715–730. [Google Scholar] [CrossRef]
- Bono, S.A.; Faria de Moura Villela, E.; Siau, C.S.; Chen, W.S.; Pengpid, S.; Hasan, M.T.; Sessou, P.; Ditekemena, J.D.; Amodan, B.O.; Hosseinipour, M.C.; et al. Factors affecting COVID-19 vaccine acceptance: An international survey among Low-and Middle-Income Countries. Vaccines 2021, 9, 515. [Google Scholar] [CrossRef] [PubMed]
- Kerr, J.R.; Schneider, C.R.; Recchia, G.; Dryhurst, S.; Sahlin, U.; Dufouil, C.; Arwidson, P.; Freeman, A.L.; van der Linden, S. Correlates of intended COVID-19 vaccine acceptance across time and countries: Results from a series of cross-sectional surveys. BMJ Open 2021, 11, e048025. [Google Scholar] [CrossRef]
- Wong, M.C.S.; Wong, E.L.Y.; Huang, J.; Cheung, A.W.L.; Law, K.; Chong, M.K.C.; Ng, R.W.Y.; Lai, C.K.C.; Boon, S.S.; Lau, J.T.F.; et al. Acceptance of the COVID-19 vaccine based on the health belief model: A population-based survey in Hong Kong. Vaccine 2021, 39, 1148–1156. [Google Scholar] [CrossRef] [PubMed]
- Schwarzinger, M.; Watson, V.; Arwidson, P.; Alla, F.; Luchini, S. COVID-19 vaccine hesitancy in a representative working-age population in France: A survey experiment based on vaccine characteristics. Lancet Public Health 2021, 6, e210–e221. [Google Scholar] [CrossRef] [PubMed]
- Maltezou, H.C.; Koutroumanis, P.P.; Kritikopoulou, C.; Theodoridou, K.; Katerelos, P.; Tsiaousi, I.; Rodolakis, A.; Loutradis, D. Knowledge about influenza and adherence to the recommendations for influenza vaccination of pregnant women after an educational intervention in Greece. Hum. Vaccines Immunother. 2019, 15, 1070–1074. [Google Scholar] [CrossRef] [PubMed]
- Otieno, N.A.; Otiato, F.; Nyawanda, B.; Adero, M.; Wairimu, W.N.; Ouma, D.; Atito, R.; Wilson, A.; Gonzalez-Casanova, I.; Malik, F.A.; et al. Drivers and barriers of vaccine acceptance among pregnant women in Kenya. Hum. Vaccines Immunother. 2020, 16, 2429–2437. [Google Scholar] [CrossRef] [PubMed]
- Kose, S.; Mandiracioglu, A.; Sahin, S.; Kaynar, T.; Karbus, O.; Ozbel, Y. Vaccine hesitancy of the COVID-19 by health care personnel. Int. J. Clin. Pract. 2021, 75, e13917. [Google Scholar] [CrossRef]
- Reno, C.; Maietti, E.; Fantini, M.P.; Savoia, E.; Manzoli, L.; Montalti, M.; Gori, D. Enhancing COVID-19 Vaccines Acceptance: Results from a Survey on Vaccine Hesitancy in Northern Italy. Vaccines 2021, 9, 378. [Google Scholar] [CrossRef]
- Alqudeimat, Y.; Alenezi, D.; AlHajri, B.; Alfouzan, H.; Almokhaizeem, Z.; Altamimi, S.; Almansouri, W.; Alzalzalah, S.; Ziyab, A.H. Acceptance of a COVID-19 vaccine and its related determinants among the general adult population in Kuwait. Med. Princ. Pract. 2021, 30, 262–271. [Google Scholar] [CrossRef] [PubMed]
- Eguia, H.; Vinciarelli, F.; Bosque-Prous, M.; Kristensen, T.; Saigí-Rubió, F. Spain’s Hesitation at the Gates of a COVID-19 Vaccine. Vaccines 2021, 9, 170. [Google Scholar] [CrossRef] [PubMed]
- Sbocchia, V. “Si hay un riesgo, quiero poder elegir”: Gestión y percepción del riesgo en los movimientos de reticencia a la vacunación italianos. Salud Colect. 2021, 17, e3231. [Google Scholar] [CrossRef] [PubMed]
- Dubé, E.; Gagnon, D.; Ouakki, M.; Bettinger, J.A.; Witteman, H.O.; MacDonald, S.; Fisher, W.; Saini, V.; Greyson, D. Measuring vaccine acceptance among Canadian parents: A survey of the Canadian Immunisation Research Network. Vaccine 2018, 36, 545–552. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.; Wagner, A.L.; Ji, J.; Huang, Z.; Zikmund-Fisher, B.J.; Boulton, M.L.; Ren, J.; Prosser, L.A. A conjoint analysis of stated vaccine preferences in Shanghai, China. Vaccine 2020, 38, 1520–1525. [Google Scholar] [CrossRef] [PubMed]
- Mir, H.H.; Parveen, S.; Mullick, N.H.; Nabi, S. Using Structural equation modeling to predict Indian people’s attitudes and intentions towards COVID-19 vaccination. Diabetes Metab. Syndr. Clin. Res. Rev. 2021, 15, 1017–1022. [Google Scholar] [CrossRef] [PubMed]
- Borriello, A.; Master, D.; Pellegrini, A.; Rose, J.M. Preferences for a COVID-19 vaccine in Australia. Vaccine 2021, 39, 473–479. [Google Scholar] [CrossRef] [PubMed]
- McPhedran, R.; Toombs, B. Efficacy or delivery? An online Discrete Choice Experiment to explore preferences for COVID-19 vaccines in the UK. Econ. Lett. 2021, 200, 109747. [Google Scholar] [CrossRef] [PubMed]
- Abbas, K.M.; Kang, G.J.; Chen, D.; Werre, S.R.; Marathe, A. Demographics, perceptions, and socioeconomic factors affecting influenza vaccination among adults in the United States. PeerJ 2018, 6, e5171. [Google Scholar] [CrossRef]
- Sarathchandra, D.; Navin, M.C.; Largent, M.A.; McCright, A.M. A Survey Instrument for Measuring Vaccine Acceptance. Prev. Med. 2018, 109, 1–7. [Google Scholar] [CrossRef]
- Almohaithef, M.A.; Padhi, B.K. Determinants of COVID-19 vaccine acceptance in Saudi Arabia: A web-based national survey. J. Multidiscip. Healthc. 2020, 13, 1657–1663. [Google Scholar] [CrossRef] [PubMed]
- Harrison, N.; Poeppl, W.; Miksch, M.; Machold, K.; Kiener, H.; Aletaha, D.; Smolen, J.S.; Forstner, C.; Burgmann, H.; Lagler, H. Predictors for Influenza Vaccine Acceptance among Patients with Inflammatory Rheumatic Diseases. Vaccine 2018, 36, 4875–4879. [Google Scholar] [CrossRef] [PubMed]
- Ayieko, S.; Markham, C.; Baker, K.; Messiah, S.E. Psychological Determinants of COVID-19 Vaccination Uptake among Pregnant Women in Kenya: A Comprehensive Model Integrating Health Belief Model Constructs, Anticipated Regret, and Trust in Health Authorities. COVID 2024, 4, 749–760. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Ratzan, S.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. Hesitant or not? A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2021, 27, 225–228. [Google Scholar] [CrossRef] [PubMed]
- Sarathchandra, D.; Johnson-Leung, J. How Political Ideology and Media Shaped Vaccination Intention in the Early Stages of the COVID-19 Pandemic in the United States. COVID 2024, 4, 658–671. [Google Scholar] [CrossRef]
- Camargo, E.L.S.; Ribeiro, C.J.N.; Santos, G.R.d.S.; Almeida, V.S.; Carvalho, H.E.F.d.; Schneider, G.; Vieira, L.G.; Alvim, A.L.S.; Pimenta, F.G.; Carneiro, L.M.; et al. Belief in Conspiracy Theories about COVID-19 Vaccines among Brazilians: A National Cross-Sectional Study. COVID 2024, 4, 518–530. [Google Scholar] [CrossRef]
- Kuter, B.J.; Browne, S.; Momplaisir, F.M.; Feemster, K.A.; Shen, A.K.; Green-McKenzie, J.; Faig, W.; Offit, P.A. Perspectives on the receipt of a COVID-19 vaccine: A survey of employees in two large hospitals in Philadelphia. Vaccine 2021, 39, 1693–1700. [Google Scholar] [CrossRef] [PubMed]
- Daly, M.; Robinson, E. Willingness to vaccinate against COVID-19 in the US: Representative longitudinal evidence from April to October 2020. Am. J. Prev. Med. 2021, 60, 766–773. [Google Scholar] [CrossRef]
- Malik, A.A.; McFadden, S.M.; Elharake, J.; Omer, S.B. Determinants of COVID-19 Vaccine Acceptance in the US. EClinicalMedicine 2020, 26, 100495. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Nguyen, N.T.; Chinn, J.; De Ferrante, M.; Kirby, K.A.; Hohmann, S.F.; Amin, A. Male gender is a predictor of higher mortality in hospitalized adults with COVID-19. PLoS ONE 2021, 16, e0254066. [Google Scholar] [CrossRef]
- Male, V. Menstrual changes after covid-19 vaccination. BMJ 2021, 374, n2211. [Google Scholar] [CrossRef] [PubMed]
- CDC. Risk for COVID-19 Infection, Hospitalisation, and Death by Age Group. 2021. Available online: https://archive.cdc.gov/www_cdc_gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-age.html (accessed on 4 June 2024).
- Latkin, C.A.; Dayton, L.; Yi, G.; Colon, B.; Kong, X. Mask usage, social distancing, racial, and gender correlates of COVID-19 vaccine intentions among adults in the US. PLoS ONE 2021, 16, e0246970. [Google Scholar] [CrossRef]
- Lakens, D. Sample size justification. Collabra Psychol. 2022, 8, 33267. [Google Scholar] [CrossRef]
- Venkatesh, V.; Thong, J.Y.L.; Xu, X. Consumer Acceptance and Use of Information Technology: Extending the Unified Theory of Acceptance and Use of Technology. MIS Q. 2012, 36, 157–178. [Google Scholar] [CrossRef]
- Remschmidt, C.; Walter, D.; Schmich, P.; Wetzstein, M.; Deleré, Y.; Wichmann, O. Knowledge, attitude, and uptake related to human papillomavirus vaccination among young women in Germany recruited via a social media site. Hum. Vaccines Immunother. 2014, 10, 2527–2535. [Google Scholar] [CrossRef] [PubMed]
- Nan, X.; Daily, K.; Richards, A.; Holt, C.; Wang, M.Q.; Tracy, K.; Qin, Y. The role of trust in health information from medical authorities in accepting the HPV vaccine among African American parents. Hum. Vaccines Immunother. 2019, 15, 1723–1731. [Google Scholar] [CrossRef] [PubMed]
- Borena, W.; Luckner-Hornischer, A.; Katzgraber, F.; Holm-Von Laer, D. Factors affecting HPV vaccine acceptance in west Austria: Do we need to revise the current immunisation scheme? Papillomavirus Res. 2016, 2, 173–177. [Google Scholar] [CrossRef] [PubMed]
- DiStefano, C.; Zhu, M.; Mîndrilã, D. Understanding and Using Factor Scores: Considerations for the Applied Researcher. Pract. Assess. Res. Eval. 2009, 14, 20. [Google Scholar] [CrossRef]
- Koenker, R.; Machado, J.A. Goodness of fit and related inference processes for quantile regression. J. Am. Stat. Assoc. 1999, 94, 1296–1310. [Google Scholar] [CrossRef]
- Recio-Vivas, A.M.; Font-Jiménez, I.; Mansilla-Domínguez, J.M.; Belzunegui-Eraso, A.; Díaz-Pérez, D.; Lorenzo-Allegue, L.; Peña-Otero, D. Fear and Attitude towards SARS-CoV-2 COVID-19 Infection in Spanish Population during the Period of Confinement. Int. J. Environ. Res. Public Health 2022, 19, 834. [Google Scholar] [CrossRef] [PubMed]
- Martín, I. Reacción Médica. El Pasaporte COVID, Poco “útil” en Países con Alta Cobertura de Vacunación. 2021. Available online: https://www.redaccionmedica.com/secciones/sanidad-hoy/el-pasaporte-covid-poco-util-en-paises-con-alta-cobertura-de-vacunacion-3326#:~:text=Pasaporte%20covid%2C%20%C3%BAtil%20en%20pa%C3%ADses,la%20introducci%C3%B3n%20del%20pasaporte%20covid (accessed on 3 June 2024).
- Collie, S.; Champion, J.; Moultrie, H.; Bekker, L.G.; Gray, G. Effectiveness of BNT162b2 vaccine against omicron variant in South Africa. N. Engl. J. Med. 2021, 386, 494–496. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M. COVID-19 vaccine hesitancy worldwide: A concise systematic review of vaccine acceptance rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef] [PubMed]
- Solís Arce, J.S.; Warren, S.S.; Meriggi, N.F.; Scacco, A.; McMurry, N.; Voors, M.; Syunyaev, G.; Malik, A.A.; Aboutajdine, S.; Adeojo, O.; et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat. Med. 2021, 27, 1385–1394. [Google Scholar] [CrossRef]
- Our World in Data 2021. Coronavirus COVID-19 Vaccinations. Available online: https://ourworldindata.org/covid-vaccinations (accessed on 3 June 2024).

| Category | Number of Responses | Percentage |
|---|---|---|
| Sex | ||
| Male | 269 | 44.83% |
| Women | 331 | 55.17% |
| Age | ||
| ≤30 years | 200 | 33.33% |
| >30 years and ≤50 years | 197 | 32.83% |
| >50 years | 203 | 33.83% |
| Mean = 41.97, SD = 15.52 | ||
| Income | ||
| EUR > 3000 | 149 | 24.83% |
| EUR ≥ 2500 and ≤3000 | 78 | 13.00% |
| EUR ≥ 1750 and <2499 | 120 | 20.00% |
| EUR ≥ 1000 and ≤1749 | 134 | 22.33% |
| EUR < 1000 | 38 | 6.33% |
| Unanswered | 81 | 13.50% |
| Education | ||
| University graduate, PhD, or doctorate | 339 | 56.59% |
| Secondary school or vocational training | 206 | 34.39% |
| Primary school | 54 | 9.02% |
| Region | ||
| Centre of Spain (Castilla and León, Castilla-la Mancha, and La Rioja) | 112 | 18.67% |
| Catalonia | 128 | 21.33% |
| Madrid | 106 | 17.67% |
| Northern Spain (Galicia, Asturias, and Cantabria) | 88 | 14.67% |
| Basque Country and Navarra | 40 | 6.67% |
| Southern Spain (Extremadura and Andalusia) | 47 | 7.83% |
| Aragón and Levante (Valencia and Murcia) | 61 | 10.17% |
| Balearic Islands and Canary Islands | 15 | 2.50% |
| Ceuta and Melilla | 3 | 0.50% |
| Coefficient | t Ratio | p Value | |
|---|---|---|---|
| Constant | 0.0569 | 1.208 | 0.2275 |
| FCOVID | 0.0736 | 3.044 | 0.0024 |
| FVAC | −0.0984 | −4.304 | <0.0001 |
| EFFIC | 0.5227 | 17.45 | <0.0001 |
| SOCINF | 0.3484 | 12.01 | <0.0001 |
| SEX | 0.0049 | 0.1128 | 0.9102 |
| AGE | 0.0293 | 0.463 | 0.6435 |
| INCOME | −0.1379 | −2.459 | 0.0142 |
| R2 = 0.7456 | |||
| Global Significance of the Model: Snedecor’s F = 251.81 (p < 0.0001) White Test: LM Statistic = 121.099 (p < 0.0001) Normality Test: χ2 Statistic = 12.978 (p = 0.00152) | |||
| Quantile | τ = 0.45 | τ = 0.5 | τ = 0.55 | |||
|---|---|---|---|---|---|---|
| Variable | Coefficient | p Value | Coefficient | p Value | Coefficient | p Value |
| Constant | −0.0284 | 0.3475 | 0.0215 | 0.5579 | 0.0777 | 0.0568 |
| FCOVID | 0.0424 | 0.0064 | 0.0428 | 0.0233 | 0.0283 | 0.1760 |
| FVACC | −0.0724 | <0.0001 | −0.0657 | 0.0002 | −0.0540 | 0.0065 |
| EFFIC | 0.5147 | <0.0001 | 0.5377 | <0.0001 | 0.5803 | <0.0001 |
| SOCINF | 0.3600 | <0.0001 | 0.3316 | <0.0001 | 0.3011 | <0.0001 |
| SEX | 0.0301 | 0.2814 | 0.0354 | 0.2971 | 0.0318 | 0.3991 |
| AGE | 0.0364 | 0.3711 | 0.0553 | 0.2632 | 0.0480 | 0.3819 |
| INCOME | −0.0323 | 0.3688 | −0.0690 | 0.1154 | −0.0657 | 0.1763 |
| Pseudo-R2 | 0.5592 | 0.5616 | 0.5669 | |||
| Quantile | τ = 0.2 | τ = 0.25 | τ = 0.3 | |||
|---|---|---|---|---|---|---|
| Variable | Coefficient | p Value | Coefficient | p Value | Coefficient | p Value |
| Constant | −0.2818 | 0.0003 | −0.2719 | <0.0001 | −0.1923 | <0.0001 |
| FCOVID | 0.0730 | 0.0658 | 0.0863 | 0.0023 | 0.0485 | 0.0402 |
| FVACC | −0.1065 | 0.0046 | −0.0975 | 0.0003 | −0.0923 | <0.0001 |
| EFFIC | 0.4600 | <0.0001 | 0.4293 | <0.0001 | 0.4501 | <0.0001 |
| SOCINF | 0.3972 | <0.0001 | 0.4315 | <0.0001 | 0.4018 | <0.0001 |
| SEX | 0.0191 | 0.7887 | 0.0659 | 0.1947 | 0.0754 | 0.0768 |
| AGE | 0.0247 | 0.8122 | 0.0461 | 0.5320 | 0.0585 | 0.3449 |
| INCOME | −0.2295 | 0.0128 | −0.1242 | 0.0577 | −0.1006 | 0.0667 |
| Pseudo-R2 | 0.6023 | 0.5912 | 0.5818 | |||
| Quantile | τ = 0.7 | τ = 0.75 | τ = 0.8 | |||
|---|---|---|---|---|---|---|
| Variable | Coefficient | p Value | Coefficient | p Value | Coefficient | p Value |
| Constant | 0.2770 | <0.0001 | 0.3501 | <0.0001 | 0.4434 | <0.0001 |
| FCOVID | 0.0036 | 0.8683 | 0.0043 | 0.8515 | 0.0096 | 0.6838 |
| FVAC | −0.0463 | 0.0263 | −0.0306 | 0.1608 | −0.0547 | 0.0147 |
| EFFIC | 0.6233 | <0.0001 | 0.6278 | <0.0001 | 0.6267 | <0.0001 |
| SOCINF | 0.3140 | <0.0001 | 0.3238 | <0.0001 | 0.3334 | <0.0001 |
| SEX | 0.0463 | 0.2429 | 0.0132 | 0.7516 | −0.0120 | 0.7790 |
| AGE | −0.0146 | 0.8003 | −0.0475 | 0.4320 | −0.0685 | 0.2694 |
| INCOME | −0.1022 | 0.0455 | −0.0798 | 0.1364 | −0.0918 | 0.0948 |
| Pseudo-R2 | 0.5779 | 0.5811 | 0.5797 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Andrés-Sánchez, J.; Arias-Oliva, M.; Pelegrín-Borondo, J. Assessing the Intention to Use a First-Generation Vaccine against COVID-19 Using Quantile Regression: A Cross-Sectional Study in Spain. COVID 2024, 4, 1211-1226. https://doi.org/10.3390/covid4080086
de Andrés-Sánchez J, Arias-Oliva M, Pelegrín-Borondo J. Assessing the Intention to Use a First-Generation Vaccine against COVID-19 Using Quantile Regression: A Cross-Sectional Study in Spain. COVID. 2024; 4(8):1211-1226. https://doi.org/10.3390/covid4080086
Chicago/Turabian Stylede Andrés-Sánchez, Jorge, Mario Arias-Oliva, and Jorge Pelegrín-Borondo. 2024. "Assessing the Intention to Use a First-Generation Vaccine against COVID-19 Using Quantile Regression: A Cross-Sectional Study in Spain" COVID 4, no. 8: 1211-1226. https://doi.org/10.3390/covid4080086
APA Stylede Andrés-Sánchez, J., Arias-Oliva, M., & Pelegrín-Borondo, J. (2024). Assessing the Intention to Use a First-Generation Vaccine against COVID-19 Using Quantile Regression: A Cross-Sectional Study in Spain. COVID, 4(8), 1211-1226. https://doi.org/10.3390/covid4080086







