Abstract
Background: The coronavirus disease 2019 (COVID-19) pandemic has generated profound health, societal, and economic consequences, which have been further compounded by long-term sequelae commonly referred to as post-COVID-19 or long-COVID syndrome. Understanding the real-world impact of post-COVID-19 mortality is therefore critical for effective healthcare planning and resource allocation. Methods: A descriptive epidemiological study was conducted using data from the US National Center for Health Statistics 2018–2024 to identify deaths attributed to the post-COVID-19 condition, as classified by the ICD-10 code U09.9, from October 2021 to December 2024. Demographic factors such as gender, age, and place of death were also extracted. Results: By December 2024, 2653 US deaths were classified under the ICD-10 code U09.9, corresponding to an age-adjusted mortality rate of 0.089 × 100,000. Mortality was significantly higher in males compared to females (0.098 vs. 0.081 × 100,000; p < 0.001). A clear age-related mortality gradient was observed, with rates increasing almost linearly with advancing age. The largest fraction of post-COVID-19 deaths occurred at home (33.0%), followed by nursing homes (26.3%) and medical facilities (24.1%). Conclusions: These findings highlight the substantial yet complex impact of the post-COVID-19 condition on mortality, with higher rates observed in males, older adults, and individuals at home, highlighting the need for targeted healthcare interventions and resource allocation, particularly for these higher-risk groups.
1. Introduction
The recent coronavirus disease 2019 (COVID-19) pandemic has profoundly impacted public health, society, and the global economy. Estimating the cumulative number of individuals infected by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the associated COVID-19-related mortality remains a significant challenge. This difficulty arises primarily due to the presence of uncontrolled confounding factors inherent in COVID-19 epidemiology, such as variations in testing availability and strategies, differences in healthcare access and quality, underreporting or misclassification of cases and deaths, and demographic and regional disparities [1]. Additionally, the emergence of new SARS-CoV-2 variants with varying transmissibility and severity further complicates accurate estimations [1]. These complexities underscore the need for robust epidemiological modeling and comprehensive data collection to better understand the true impact of the still ongoing pandemic. According to the World Health Organization (WHO) COVID-19 dashboard, over 777 million people may have experienced one or more severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections and approximately 7.1 million deaths may have been attributable to (or associated with) COVID-19 by the end of 2024 [2]. However, these figures are widely recognized as underestimates, with the WHO suggesting that the actual number of COVID-19-related deaths could be up to 2.7 times higher (i.e., approximately 20 million) [3]. If accurate, this would position COVID-19 as the second deadliest pandemic of the past century, surpassed only by the Spanish flu, which caused an estimated 40–50 million deaths [4].
Beyond the acute phase, SARS-CoV-2 infection can lead to persistent and complex sequelae variably defined as post-COVID-19, long-COVID, or long-haul COVID-19 syndrome [5,6,7]. This emerging healthcare challenge prompted the WHO to introduce a specific 10th revision of the International Classification of Diseases (ICD-10) code, U09.9, in October 2021 [8]. This code, designated as “Post COVID-19 condition, unspecified”, encompasses a range of symptoms persisting or emerging at least three months after the initial infection and lasting for over two months with no alternative clinical explanation [8]. The introduction of this ICD-10 code has facilitated the systematic classification, monitoring, and study of post-COVID-19 cases, enabling healthcare providers and scientists to adopt a more standardized approach.
The WHO estimates the incidence of post-COVID-19 syndrome to be 10–20% [8], while US data suggest that 6.9% of adults and 1.3% of children reported experiencing post-COVID-19 syndrome in 2022 [9].
However, this figure may also be underestimated, as evidenced by more recent data. A meta-analysis by Sk Abd Razak et al. [10], which included 16 studies, estimated the global prevalence of post-COVID-19 syndrome to be 41.8% (95% confidence interval (CI): 39.7–43.9%). This prevalence showed minor temporal variation, with rates of 45.1% at three months and 41.3% both 6and 12months post-recovery [10]. Women were found to have higher prevalence than men (52.8% vs. 41.3%). Children are also affected by post-COVID-19 syndrome, as highlighted by a systematic review by Silva et al. [11], which reported that 29% of children experienced exercise intolerance, while respiratory symptoms and psychological distress affected 10–12% of children 3 to 12 months post-infection.
Another recent meta-analysis published by Atchley-Challenner et al. [12] identified the most prevalent symptoms of post-COVID-19 syndrome, including respiratory complaints (e.g., shortness of breath and fatigue), general pain, cognitive and behavioral impairments (e.g., brain fog, insomnia, anxiety, and depression), sensory disturbances (e.g., loss of taste or smell), cardiac symptoms (e.g., palpitations and chest pain), hair loss, fever, and a flu-like syndrome. These symptoms collectively contribute to reductions in quality of life [13] and highlight a significant issue, as the post-COVID-19 syndrome could represent an “epidemic within the pandemic” [14]. The socioeconomic impact of the post-COVID-19 condition is also substantial, as increased medical care and hospital admissions have been shown to raise healthcare costs by 23% in the year following an acute SARS-CoV-2 infection [15]. This economic burden can extend to affected families, causing financial strain and psychological stress [16].
Although the precise mechanisms underlying post-COVID-19 syndrome remain unclear, current hypotheses include viral persistence, autoimmunity, unresolved tissue damage, immune dysregulation, microbiome dysbiosis, endothelial and neuronal inflammation, mitochondrial dysfunction, and the formation of microclots [17]. Risk factors for developing long-term complications include severe acute illness, pre-existing comorbidities, older age, female sex, and lack of vaccination [18].
Despite progress in characterizing and monitoring the prevalence and morbidity of long-COVID, specific mortality data attributable to this syndrome are lacking to the best of our knowledge, mostly because of inconsistent definitions, coding inaccuracies, and documentation challenges. To address this gap, we designed an original retrospective study, one of the first, to the best of our knowledge, to systematically analyze the burden and demographic characteristics of mortality associated with post-COVID-19 syndrome, using the unique U09.9 ICD-10 code and data from the US National Center for Health Statistics [19].
2. Materials and Methods
2.1. Study Design
We conducted a descriptive epidemiological study based on an electronic search of the US National Center for Health Statistics using the Wide-Ranging Online Data for Epidemiologic Research (WONDER) interface, which provides comprehensive statistics derived from death certificates for all US residents [20]. Specifically, we accessed the “Provisional Multiple Cause of Death” database, which contains population and death count data across the US up to the most recently available week. Death certificates include complete demographic, social, and geographic details, along with the primary underlying cause of death.
2.2. Study Setting
For this retrospective study, we used the primary keyword “Post COVID-19”, corresponding to the ICD-10 code U09.9. The search was extended to the period from October 2021 (when the ICD-10 code U09.9 was first introduced) through the end of December 2024 and therefore spanned over 3 years. Additional searches were performed using keywords for “gender”, “ten-year age groups”, and “place of death”. In the ICD-10 classification, U09.9 is defined as “post-acute sequela of COVID-19” [19].
2.3. Data Quality
The mortality data contained in the WONDER database are based on the WHO definition of the underlying cause of death as the “disease or injury which initiated the train of events leading directly to death, or the circumstances of the accident or violence which produced the fatal injury”. The underlying cause is therefore determined based on the information provided by the certifying physician in the cause-of-death section of the death certificate. This method of determination has remained consistent over time, ensuring continuity in the classification process [19]. All causes of death are classified within the WONDER database according to the ICD framework. Death records from 1999 onward have been classified using the tenth revision (ICD-10). In October 2021, the ICD-10 code U09.9 was introduced, and its definition has remained unchanged since its inclusion, thus allowing consistency in mortality data reporting under this code over time [19].
2.4. Study Population and Measures
The results of our searches were provided as the total numbers of deaths (and percentages) and age-adjusted or crude mortality rates (×100,000) with 95% confidence intervals (95% CIs). According to the WONDER database, age-adjusted death rates are calculated as weighted averages of age-specific death rates. The weights correspond to a fixed population distribution by age, with the ‘Year 2000 U.S. Standard Population’ used as the default reference [20], enabling comparisons of relative mortality risks among population groups and over time. A descriptive analysis encompassing the assessment of statistically significant differences among multiple groups (genders and age groups) was based on Shapiro-Wilk test followed by one-way analysis of variance (ANOVA) applied to the annual number of deaths, the mean death rate, and its standard error using StatPages (Interactive Statistical Calculation; https://statpages.info/anova1sm.html, accessed on 1 January 2025). Statistical significance was set at p < 0.05.
This study was conducted in accordance with the Declaration of Helsinki and the provisions of the relevant local legislation and was exempt from Institutional Review Board review, as the WONDER database is freely searchable and fully anonymized.
3. Results
The results of our analysis are presented in Table 1. As of the end of December 2024, a cumulative number of 2653 US deaths were classified with the ICD-10 code U09.9 for “post COVID-19” as the primary cause of death, corresponding to an age-adjusted mortality rate of 0.089 (95% CI: 0.085–0.092) × 100,000 in the population.

Table 1.
The mortality of post-COVID-19 syndrome in the US in 2024. These data are expressed as age-adjusted values × 100,000, crude death rates ×100,000, or overall numbers of deaths, when appropriate.
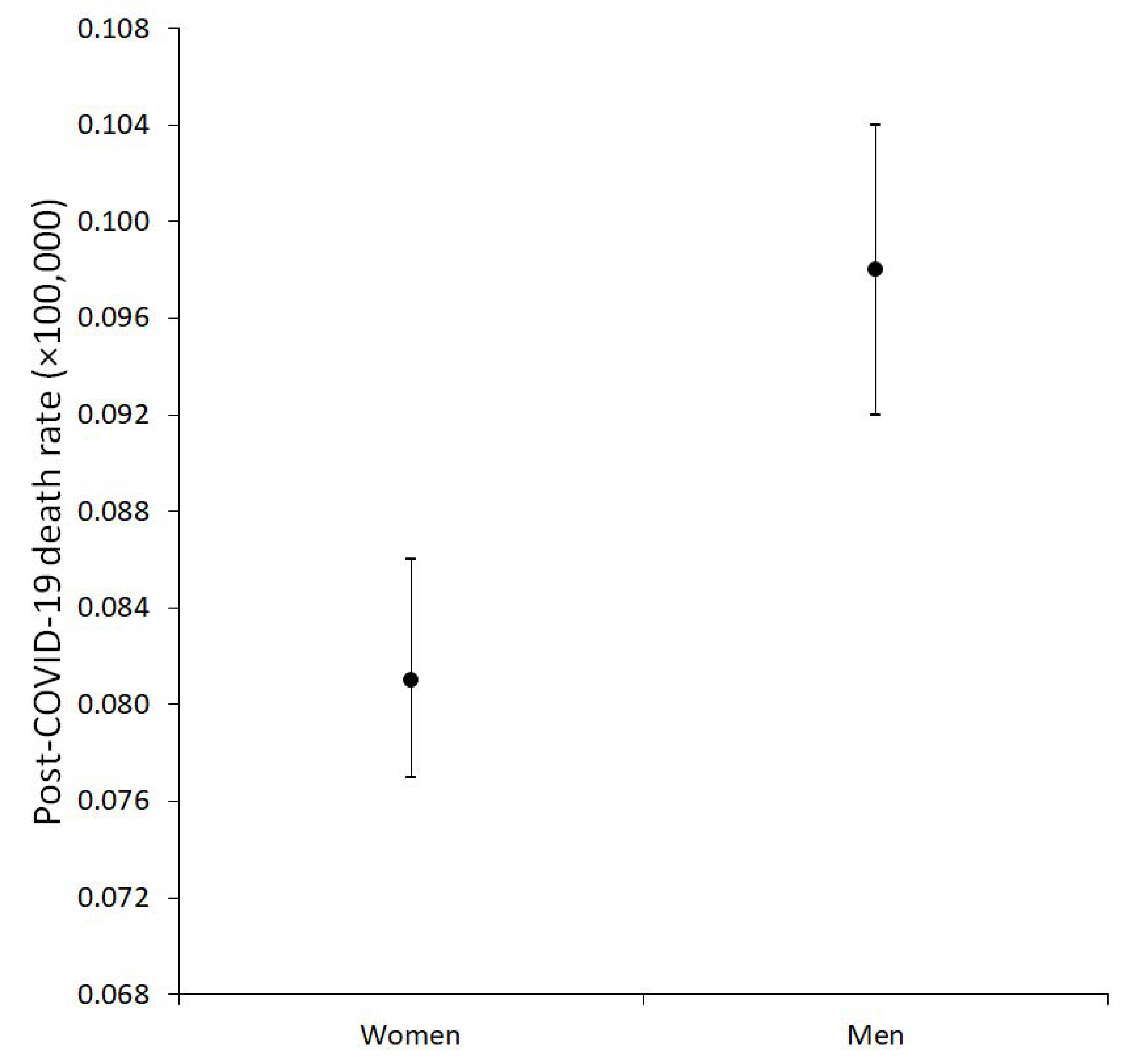
Mortality was significantly higher among males (0.098; 95% CI: 0.092–0.104 × 100,000) compared to females (0.081; 95% CI: 0.077–0.086 × 100,000; f = 23.0; p < 0.001), with a standardized difference of 0.017 (95% CI: 0.010–0.024) × 100,000 (Figure 1).
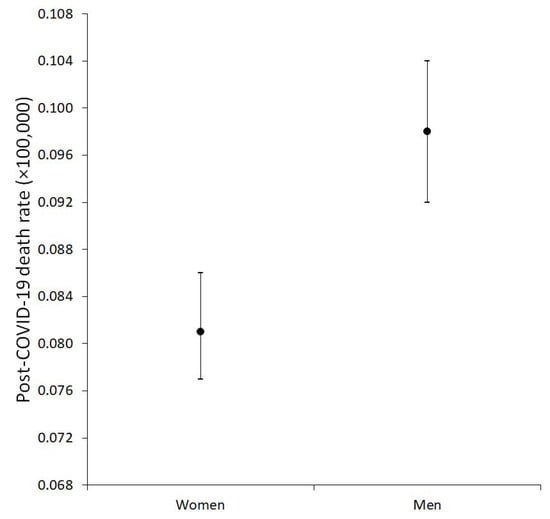
Figure 1.
Age-adjusted mortality rates for post-COVID-19 condition in males and females.
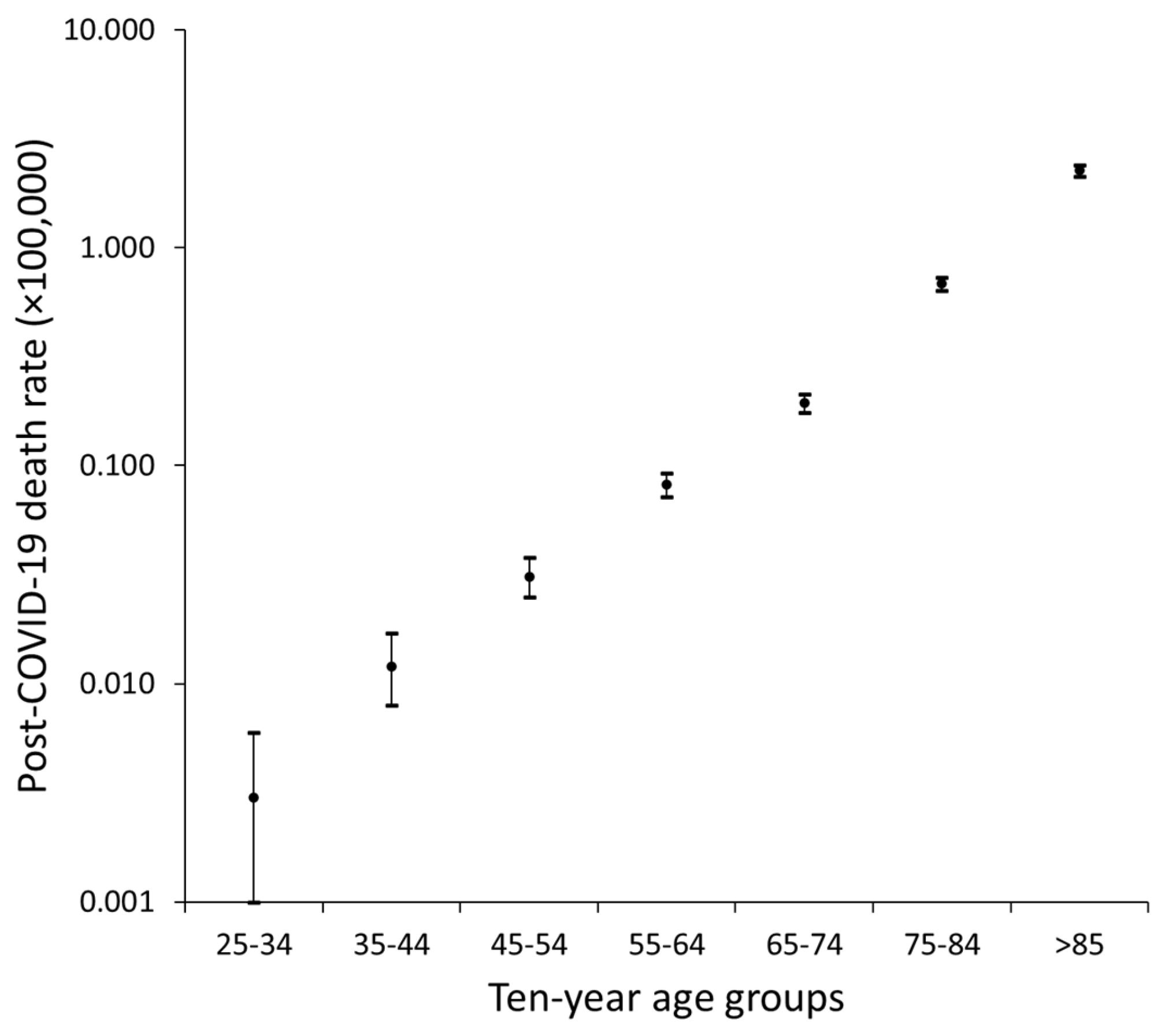
An age-dependent trend was evident, with crude mortality rates for the post-COVID-19 condition increasing steadily and significantly with advancing age (f = 178; p < 0.001), as illustrated in Figure 1. When analyzed on a logarithmic scale, the relationship between the crude death rate and age appeared nearly linear (Figure 2).
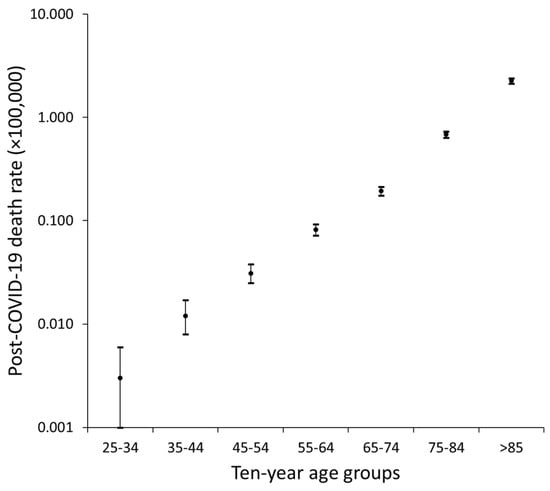
Figure 2.
Crude mortality rates for post-COVID-19 condition across different 10-year age groups.
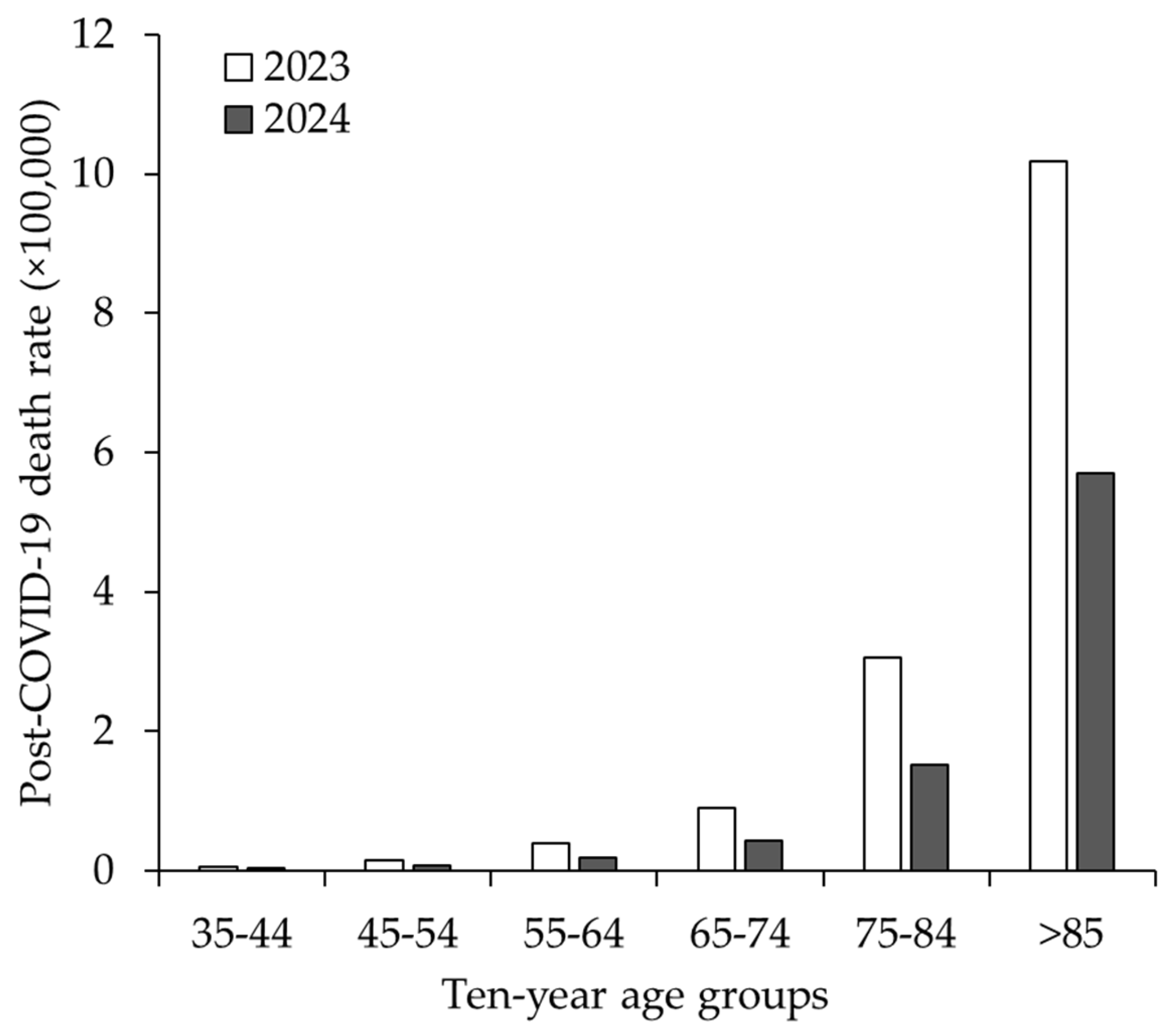
The crude mortality rates for the post-COVID-19 condition across the most representative 10-year age groups, stratified by year of death, are summarized in Figure 3. The data indicate that the age-related trend remained consistent between 2023 and 2024, as no death certificates containing the ICD-10 code U09.9 were recorded in the WONDER database. However, the mortality rates in 2023 were consistently higher than those in 2024 across all age groups.
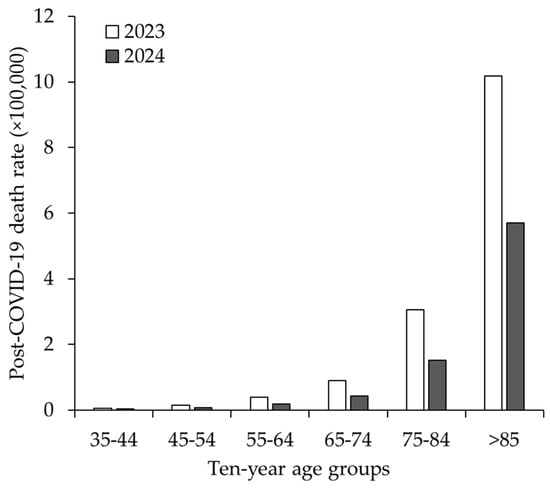
Figure 3.
Crude mortality rates for post-COVID-19 condition across different 10-year age groups, stratified by year of death.
The distribution of the locations of post-COVID-19 condition deaths is also summarized in Table 1. Most deaths occurred at the decedent’s home (33.0%), followed by nursing homes or long-term care facilities (26.3%), medical facilities (as inpatients; 24.1%), and hospice facilities (7.7%).
4. Discussion
The findings of this study provide a detailed epidemiological overview of the mortality burden associated with the post-COVID-19 condition in the US, which was identified using the ICD-10 code U09.9 within data from the National Center for Health Statistics. Our analysis highlights significant demographic patterns, emphasizing the complexity and public health implications of this emerging condition.
As of the end of 2024, over 2600 US deaths have been classified under the ICD-10 code U09.9, representing a critical yet likely underestimated aspect of the long-term impact of the ongoing COVID-19 pandemic. Although an age-adjusted mortality of 0.089 ×100,000 indicates that deaths directly attributed to the post-COVID-19 condition are a relatively infrequent occurrence at the national level, this rate demonstrates substantial variation across specific subpopulations, reflecting disparities rooted in demographic and social determinants of health. These findings underscore the necessity of targeted analyses and interventions to proactively mitigate the post-COVID-19 mortality burden [14].
Although the prevalence and mortality data are not directly comparable, as they were derived from different populations, important insights can still be drawn regarding the distinct demographic impacts of post-COVID-19 syndrome epidemiology and its associated mortality. The higher mortality rate observed in men compared to women (0.098 vs. 0.081 × 100,000) does not align with the known prevalence of post-COVID-19 syndrome in the general population, which has consistently been reported to be higher in females than in males. A comprehensive analysis by the Global Burden of Disease Long COVID Collaborators estimated the prevalence of symptom clusters 3 months after acute, symptomatic SARS-CoV-2 infection to be nearly twice as high in females than in males (10.6% vs. 5.4%) [21]. Similarly, a prospective cohort study involving 377 individuals that had clinically recovered from acute SARS-CoV-2 infection found females to be over three times more likely to be diagnosed with long-COVID syndrome 1–3 months after viral clearance (adjusted odds ratio (AOR): 3.3; 95% CI: 1.8–6.2) [22]. Supporting these findings, a nationwide, retrospective cohort study in Scotland [23], with over 4,676,390 participants, showed a higher rate of post-COVID-19 syndrome diagnosis in females compared to males (65.1% vs. 50.4%). Similarly, a population-representative survey of over 3000 US adults aged ≥18 years reported nearly double the prevalence of post-COVID-19 syndrome in females compared to males 12 months after acute infection (adjusted prevalence ratio (APR): 1.84; 95% CI: 1.40–2.42) [24]. Thus, the unforeseen male predominance in post-COVID-19 mortality may reflect biological factors such as hormonal differences influencing immune responses and a higher prevalence of comorbidities like cardiovascular disease and diabetes in men [10]. Some reasonable explanations may account for this finding. First, women generally exhibit a more robust immune response to SARS-CoV-2 than men, characterized by higher antibody production and greater T-cell activity. This enhanced immune response may provide prolonged protection against the potential long-term complications of COVID-19 [25]. The prevalence of comorbidities is also significantly higher in men than in women during both the acute phase of COVID-19 and the post-acute period. This increased burden of underlying health conditions places men at a heightened risk of complications and mortality associated with this disease [26]. Finally, research indicates that women tend to demonstrate greater health self-awareness. They are more likely to report post-COVID-19 symptoms and actively seek medical care, facilitating earlier and potentially more effective interventions, while men may delay seeking care, contributing to worse outcomes [27]. Nonetheless, the significant gender disparity in mortality (0.017 × 100,000) highlights an actionable difference that warrants further investigation to identify specific interventions in males.
We also observed a clear age-dependent relationship in post-COVID-19 mortality, with rates increasing steadily and significantly with advancing age. Unlike the gender effect, age has occasionally been identified as a determinant of post-COVID-19 syndrome. In a study by Bai et al. [22], advanced age was associated with a higher risk of developing long COVID (AOR: 1.03 per 10-year increase; 95% CI: 1.01–1.05). However, this finding has been contradicted by other epidemiological investigations. A nationwide population cohort study conducted in Scotland involving 198,096 individuals with acute SARS-CoV-2 infection reported a higher prevalence of long-COVID symptoms 6 months after recovery in the 40–59 age group, with a substantial decline in prevalence among those aged ≥70 years [28]. Similarly, a US population-representative survey by Robertson et al. found a lower prevalence of long-COVID syndrome in individuals aged ≥65 years (APR: 0.43; 95% CI: 0.27–0.66) [24]. However, Ford et al., using data from the US national Household Pulse Survey, reported higher rates of significant activity limitations among adults aged >40 years with long COVID, and a marked 1-year decline in post-COVID-19 symptoms was observed, primarily in individuals aged <60 years [29]. This inherently suggests that although the post-COVID-19 condition may be more prevalent in younger age groups, its morbidity and mortality consequences appear to be significantly more severe in older individuals. Although the biological relationship between the prevalence and mortality of post-COVID-19 syndrome remains unclear, several plausible explanations can be proposed. Older individuals are more likely to experience severe acute disease, prolonged hospitalizations and complications, making them more susceptible to post-COVID-19 sequelae, as clearly indicated by a meta-analysis conducted by Li et al. [30].
The distribution of post-COVID-19 mortality by place of death provides valuable insights into the healthcare settings most affected by the post-COVID-19 condition. A substantial proportion of the deaths occurred at the decedent’s home (33.0%), followed by nursing homes or long-term care facilities (26.3%). These findings underscore two critical aspects: challenges in care access—as home deaths potentially reflect isolation, barriers to timely medical intervention, or under-recognition of the post-COVID-19 condition [31,32]—and the heightened vulnerability of elderly populations residing in long-term care settings, as many individuals in these facilities may already have severe underlying comorbidities that could be exacerbated by post-COVID-19 sequelae [33].
Altogether, our findings highlight the need for a more structured approach to identifying, managing and preventing post-COVID-19 mortality, providing useful recommendations to lower the risk of death from or with post-COVID-19 syndrome. In particular, the disproportionate impacts on males, older individuals and residents of long-term care facilities emphasize the importance of targeted interventions in subjects with the post-COVID-19 condition. Prioritizing vaccination for these high-risk groups—not only with COVID-19 vaccines but also those for influenza, pneumococci and respiratory syncytial virus—is crucial to reducing the risk of clinical deterioration and death among vulnerable individuals [34]. Facilitating access to post-COVID-19 care for elderly individuals and those with mobility limitations is also imperative [35], alongside the expanded use of remote monitoring systems and telehealth to promptly detect physical or cognitive decline [36]. Moreover, healthcare providers will need enhanced training to improve recognition and management of the post-COVID-19 condition, especially outside the hospital environment [37]. Addressing the gender and age disparities in post-COVID-19 mortality demands a deeper understanding of the biological and social determinants of health, so that public health initiatives can be more focused on raising awareness and ensuring equitable access to diagnostic and therapeutic resources.
We identified a similar study that quantified the burden of post-COVID-19 mortality using the ICD-10 code U09.9 listed on death certificates [38]. The authors analyzed data from the Italian National Cause of Death Register and calculated the post-COVID-19 mortality rate for 2021 to be 5.1 × 100,000 inhabitants. Consistent with our findings, that study reported that the mortality rates increased with age and were higher in men compared to women (6.0 vs. 4.3 × 100,000, respectively).
Although our study provides significant insights into post-COVID-19 mortality, we acknowledge some limitations in our analysis. First, the ICD-10 code U09.9 may underestimate the true burden of post-COVID-19 deaths, mostly due to variability in documentation and coding practices across the US, but also among different countries (e.g., the mortality rates observed in Italy appear significantly higher than those reported in our analysis of data from the US National Center for Health Statistics). Second, the 2024 data remain provisional, reflecting inherent delays in death certificate processing and reporting through the end of the year. Another potential limitation is the inability to perform a multivariate analysis incorporating key determinants of the post-COVID-19 condition such as the numbers and types of comorbidities, history of infection or multiple infections with different SARS-CoV-2 variants, clinical severity, access to current therapies, and vaccination status, as these data are unavailable in the WONDER database. Future studies should therefore aim to address these limitations by collecting additional information that is not available through the WONDER interface of the US National Center for Health Statistics, including data on the severity of acute SARS-CoV-2 infections, access to COVID-19 vaccines, ethnic origin, census information, educational level and assignment of the ICD-10 code U09.9. Continued monitoring of post-COVID-19 mortality trends over time will also be critical for understanding the long-term trajectory of this syndrome as the acute phase of the pandemic recedes. Finally, additional research into the precise biological mechanisms underlying post-COVID-19 mortality will be essential for developing effective health strategies to mitigate the burden of post-COVID-19 deaths.
5. Conclusions
The results of our analysis highlight the significant yet complex impact of the post-COVID-19 condition on mortality. Although the absolute number of death certificates featuring the ICD-10 code U09.9 alone remains relatively low compared to acute COVID-19 fatalities in the US, the observed patterns reveal critical areas for targeted interventions and resource allocation. Addressing the identified disparities and gaps in care will enable healthcare systems to more effectively manage the ongoing burden of the post-COVID-19 condition and improve outcomes for affected individuals.
Author Contributions
Conceptualization, G.L. and F.S.-G.; software, G.L.; formal analysis, G.L.; data curation, G.L.; writing—original draft preparation, G.L.; writing—review and editing, F.S.-G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and the provisions of the relevant local legislation and was exempt from Institutional Review Board review, as the CDC WONDER database is freely searchable and fully anonymized.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| COVID-19 | coronavirus disease 2019 |
| WHO | World Health Organization |
| SARS-CoV-2 | severe acute respiratory syndrome coronavirus 2 |
| ICD-10 | 10th revision of the International Classification of Diseases |
| CI | confidence interval |
| WONDER | Wide-Ranging Online Data for Epidemiologic Research |
| ANOVA | one-way analysis of variance |
| AOR | adjusted odds ratio |
| APR | adjusted prevalence ratio |
References
- Lippi, G.; Mattiuzzi, C.; Henry, B.M. Uncontrolled Confounding in COVID-19 Epidemiology. Diagnosis 2022, 10, 200–202. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO COVID-19 Dashboard. Available online: https://data.who.int/dashboards/covid19/cases (accessed on 1 January 2025).
- Msemburi, W.; Karlinsky, A.; Knutson, V.; Aleshin-Guendel, S.; Chatterji, S.; Wakefield, J. The WHO Estimates of Excess Mortality Associated with the COVID-19 Pandemic. Nature 2023, 613, 130–137. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sampath, S.; Khedr, A.; Qamar, S.; Tekin, A.; Singh, R.; Green, R.; Kashyap, R. Pandemics Throughout the History. Cureus 2021, 13, e18136. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lippi, G.; Henry, B.M.; Favresse, J.; Plebani, M. Addressing Standardized Definitions of Post-COVID and Long-COVID. Clin. Chem. Lab. Med. 2023, 61, 1361–1362. [Google Scholar] [CrossRef] [PubMed]
- Gheorghita, R.; Soldanescu, I.; Lobiuc, A.; Caliman Sturdza, O.A.; Filip, R.; Constantinescu-Bercu, A.; Dimian, M.; Mangul, S.; Covasa, M. The Knowns and Unknowns of Long COVID-19: From Mechanisms to Therapeutical Approaches. Front. Immunol. 2024, 15, 1344086. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gutzeit, J.; Weiß, M.; Nürnberger, C.; Lemhöfer, C.; Appel, K.S.; Pracht, E.; Reese, J.P.; Lehmann, C.; Polidori, M.C.; Hein, G.; et al. Definitions and Symptoms of the Post-COVID Syndrome: An Updated Systematic Umbrella Review. Eur. Arch. Psychiatry Clin. Neurosci. 2024. Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Post COVID-19 Condition (Long COVID). Available online: https://www.who.int/europe/news-room/fact-sheets/item/post-covid-19-condition (accessed on 1 January 2025).
- Centers for Disease Control and Prevention. CDC Science and the Public Health Approach to Long COVID. Available online: https://www.cdc.gov/covid/php/long-covid/index.html#cdc_generic_section_2-key-findings (accessed on 7 January 2025).
- Sk Abd Razak, R.; Ismail, A.; Abdul Aziz, A.F.; Suddin, L.S.; Azzeri, A.; Sha’ari, N.I. Post-COVID Syndrome Prevalence: A Systematic Review and Meta-Analysis. BMC Public Health 2024, 24, 1785. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Silva, M.M.D.; Benites, M.N.; Castro, Y.M.; Moura, P.V.; Zhang, L. Prevalence of Symptoms of Post-COVID-19 Condition (Long COVID) in Children Hospitalized with COVID-19: A Systematic Review of Observational Studies. Pediatr. Pulmonol. 2024, 59, 3159–3169. [Google Scholar] [CrossRef] [PubMed]
- Atchley-Challenner, R.; Strasser, Z.; Krishnamoorthy, A.; Pant, D.; Chibnik, L.B.; Karlson, E.W. Long COVID: A Narrative Review and Meta-Analysis of Individual Symptom Frequencies. COVID 2024, 4, 1513–1545. [Google Scholar] [CrossRef]
- Kim, J.; Duru, E.E.; Weir, P.; Lee, S. Long COVID Is Associated with Decreased Quality of Life and Increased Mental Disability. COVID 2024, 4, 1719–1730. [Google Scholar] [CrossRef]
- Mattiuzzi, C.; Lippi, G. Long COVID: An Epidemic Within the Pandemic. COVID 2023, 3, 773–776. [Google Scholar] [CrossRef]
- Scott, A.; Ansari, W.; Khan, F.; Chambers, R.; Benigno, M.; Di Fusco, M.; McGrath, L.; Malhotra, D.; Draica, F.; Nguyen, J.; et al. Substantial Health and Economic Burden of COVID-19 During the Year After Acute Illness Among US Adults at High Risk of Severe COVID-19. BMC Med. 2024, 22, 46. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mukhida, S.; Khan, S. Does Long COVID-19 Affect the Quality of Life Only to COVID-19 Patients or Family Member Also? J. Fam. Med. Prim. Care 2024, 13, 5442–5443. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Al-Aly, Z.; Topol, E. Solving the Puzzle of Long COVID. Science 2024, 383, 830–832. [Google Scholar] [CrossRef] [PubMed]
- Muthuka, J.K.; Nzioki, J.M.; Kelly, J.O.; Musangi, E.N.; Chebungei, L.C.; Nabaweesi, R.; Kiptoo, M.K. Prevalence and Predictors of Long COVID-19 and the Average Time to Diagnosis in the General Population: A Systematic Review, Meta-Analysis and Meta-Regression. COVID 2024, 4, 968–981. [Google Scholar] [CrossRef]
- International Classification of Diseases. ICD-10-CM Diagnosis Code U09.9. Available online: https://www.icd10data.com/ICD10CM/Codes/U00-U85/U00-U49/U09-/U09.9 (accessed on 1 January 2025).
- Centers for Disease Control and Prevention; National Center for Health Statistics. National Vital Statistics System, Provisional Mortality on CDC WONDER Online Database. Data are from the final Multiple Cause of Death Files, 2018–2022, and from Provisional Data for Years 2023–2024, as Compiled from Data Provided by the 57 Vital Statistics Jurisdictions Through the Vital Statistics Cooperative Program. Available online: https://wonder.cdc.gov/mcd-icd10-provisional.html (accessed on 2 January 2025).
- Global Burden of Disease Long COVID Collaborators; Wulf Hanson, S.; Abbafati, C.; Aerts, J.G.; Al-Aly, Z.; Ashbaugh, C.; Ballouz, T.; Blyuss, O.; Bobkova, P.; Bonsel, G.; et al. Estimated Global Proportions of Individuals with Persistent Fatigue, Cognitive, and Respiratory Symptom Clusters Following Symptomatic COVID-19 in 2020 and 2021. JAMA 2022, 328, 1604–1615. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bai, F.; Tomasoni, D.; Falcinella, C.; Barbanotti, D.; Castoldi, R.; Mulè, G.; Augello, M.; Mondatore, D.; Allegrini, M.; Cona, A.; et al. Female Gender is Associated with Long COVID Syndrome: A Prospective Cohort Study. Clin. Microbiol. Infect. 2022, 28, 611.e9–611.e16. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jeffrey, K.; Woolford, L.; Maini, R.; Basetti, S.; Batchelor, A.; Weatherill, D.; White, C.; Hammersley, V.; Millington, T.; Macdonald, C.; et al. Prevalence and Risk Factors for Long COVID Among Adults in Scotland Using Electronic Health Records: A National, Retrospective, Observational Cohort Study. eClinicalMedicine 2024, 71, 102590. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Robertson, M.M.; Qasmieh, S.A.; Kulkarni, S.G.; Teasdale, C.A.; Jones, H.E.; McNairy, M.; Borrell, L.N.; Nash, D. The Epidemiology of Long Coronavirus Disease in US Adults. Clin. Infect. Dis. 2023, 76, 1636–1645. [Google Scholar] [CrossRef] [PubMed]
- Paschou, S.A.; Psaltopoulou, T.; Halvatsiotis, P.; Raptis, A.; Vlachopoulos, C.V.; Dimopoulos, M.A. Gender Differences in COVID-19. Maturitas 2022, 161, 72–73. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nielsen, J.; Nørgaard, S.K.; Lanzieri, G.; Vestergaard, L.S.; Moelbak, K. Sex-Differences in COVID-19 Associated Excess Mortality Is Not Exceptional for the COVID-19 Pandemic. Sci. Rep. 2021, 11, 20815. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Marcilla-Toribio, I.; Moratalla-Cebrián, M.L.; Notario-Pacheco, B.; Escudero-Lopez, M.A.; Morales-Cuenca, N.; Martinez-Andres, M. Gender Differences in Symptomatology, Socio-Demographic Information and Quality of Life in Spanish Population with Long COVID Condition: A Cross-Sectional Study. Front. Public Health 2024, 12, 1355973. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hastie, C.E.; Lowe, D.J.; McAuley, A.; Mills, N.L.; Winter, A.J.; Black, C.; Scott, J.T.; O’Donnell, C.A.; Blane, D.N.; Browne, S.; et al. True Prevalence of Long-COVID in a Nationwide, Population Cohort Study. Nat. Commun. 2023, 14, 7892. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ford, N.D.; Slaughter, D.; Edwards, D.; Dalton, A.; Perrine, C.; Vahratian, A.; Saydah, S. Long COVID and Significant Activity Limitation Among Adults, by Age—United States, June 1–13, 2022, to June 7–19, 2023. MMWR Morb. Mortal. Wkly. Rep. 2023, 72, 866–870. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Li, X.; Zhong, X.; Wang, Y.; Zeng, X.; Luo, T.; Liu, Q. Clinical Determinants of the Severity of COVID-19: A Systematic Review and Meta-Analysis. PLoS ONE 2021, 16, e0250602. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Au, L.; Capotescu, C.; Eyal, G.; Finestone, G. Long COVID and Medical Gaslighting: Dismissal, Delayed Diagnosis, and Deferred Treatment. SSM Qual. Res. Health 2022, 2, 100167. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sunkersing, D.; Ramasawmy, M.; Alwan, N.A.; Clutterbuck, D.; Mu, Y.; Horstmanshof, K.; Banerjee, A.; Heightman, M. What is Current Care for People with Long COVID in England? A Qualitative Interview Study. BMJ Open 2024, 14, e080967. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Russell, C.D.; Lone, N.I.; Baillie, J.K. Comorbidities, Multimorbidity and COVID-19. Nat. Med. 2023, 29, 334–343. [Google Scholar] [CrossRef] [PubMed]
- Reynard, C.; Campling, J.; Gordon, A.L.; Kassianos, G.; Liu, H.H.; Richter, A.; Vyse, A.; Wiseman, D.J.; Wright, H.; Ellsbury, G. Adult Risk Groups for Vaccine Preventable Respiratory Infections: An Overview of the UK Environment. Expert. Rev. Vaccines 2024, 23, 1052–1067. [Google Scholar] [CrossRef] [PubMed]
- Choe, E.Y.; Du, Y.; Sun, G. Decline in Older Adults’ Daily Mobility During the COVID-19 Pandemic: The Role of Individual and Built Environment Factors. BMC Public Health 2022, 22, 2317. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kim, Y.K.; Ang, S. Older Adults with Functional Limitations and Their Use of Telehealth During COVID-19. Res. Aging 2023, 45, 609–619. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Frenk, J.; Chen, L.C.; Chandran, L.; Groff, E.O.H.; King, R.; Meleis, A.; Fineberg, H.V. Challenges and Opportunities for Educating Health Professionals After the COVID-19 Pandemic. Lancet 2022, 400, 1539–1556. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Grippo, F.; Minelli, G.; Crialesi, R.; Marchetti, S.; Pricci, F.; Onder, G. Deaths Related to Post-COVID in Italy: A National Study Based on Death Certificates. Front. Med. 2024, 11, 1401602. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).