A Journey to Hear: The Evolution of Cochlear Implants
Definition
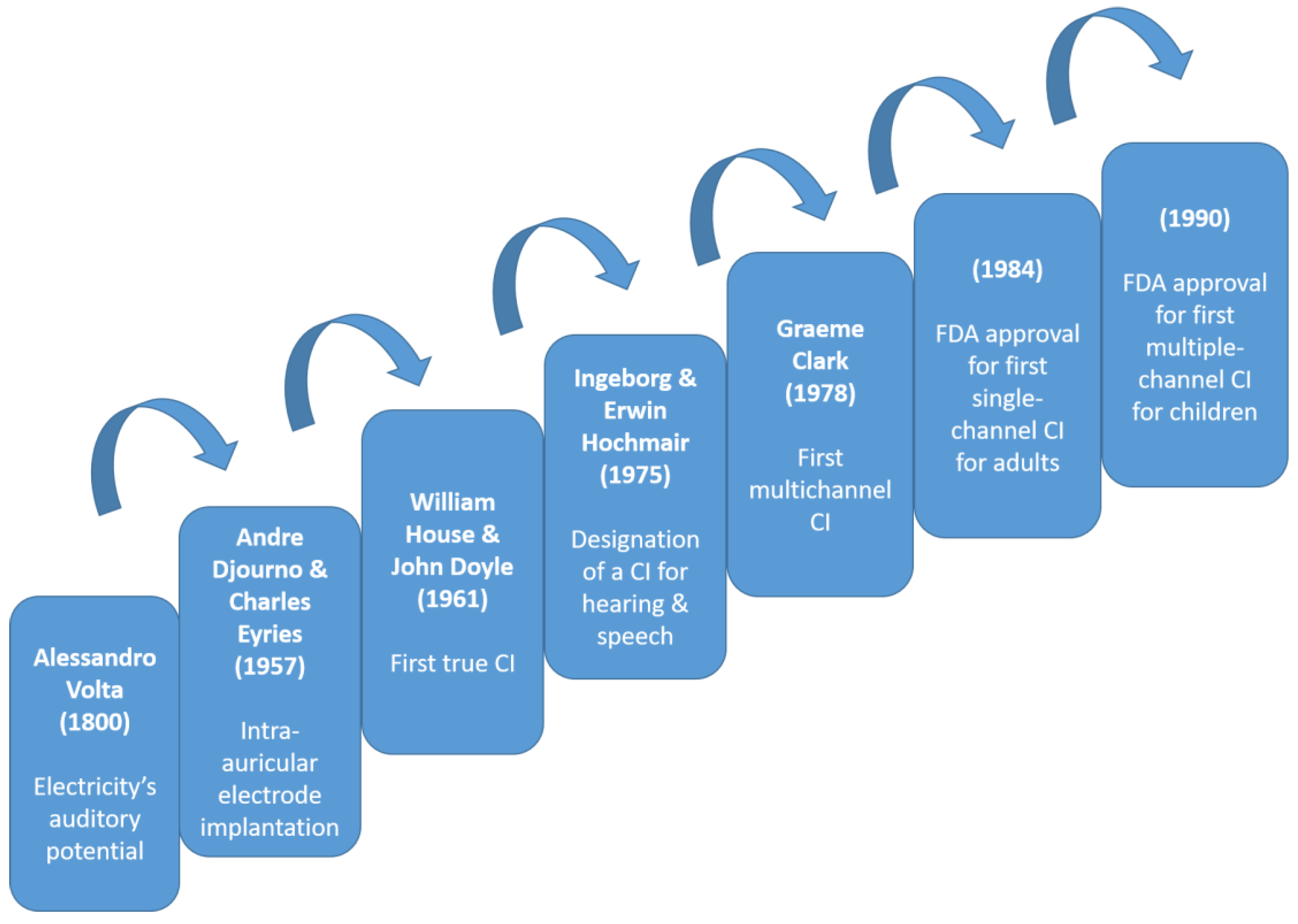
1. Introduction
2. Early Developments: Alessandro Volta’s Groundbreaking Exploration into Harnessing Electricity for Auditory Perception
3. Post-World War II Advances
3.1. Electronics, Auditory Nerve Stimulation Experiments, and the Emergence of Multichannel Cochlear Implants with Silicon Technology Impact
3.2. Limited Success and Ethical Dilemmas: Scientists’ Perspectives on First Cochlear Implants
4. Expanding Applications and Technological Advances (1990s–2000s)
4.1. Pediatric Cochlear Implantation
4.2. Bilateral Cochlear Implants
4.3. Cochlear Implant Processing: Guiding Auditory Perception and Enhancing Speech Recognition
5. Beyond Auditory Restoration
5.1. Cochlear Implants for Single-Sided Deafness and Tinnitus
5.2. Cochlear Implant Innovations in Music Perception
5.3. Advances in Hybrid Devices
6. Social Impact and Ethical Considerations
6.1. Deaf Culture and the Deaf Community’s Response to Cochlear Implants
6.2. The Role of Advocacy Groups and Policy in Shaping Implantation Practices
7. Contemporary Trends and Future Prospects
7.1. Pioneering Companies in Cochlear Implants
7.2. Current Criteria for Cochlear Implantation
7.3. Expanding the Candidate Pool: Aging Populations and Adult Implantation
7.4. Biocompatible Materials and Implant Longevity
7.5. Wireless Connectivity and Smartphone Integration
7.6. Integration of Cochlear Implants with Other Technologies
7.7. Totally Implantable Cochlear Implants and Beyond
7.8. Stem Cells and Gene Therapy in Hearing Restoration
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mudry, A.; Mills, M. The Early History of the Cochlear Implant: A Retrospective. JAMA Otolaryngol. Head Neck Surg. 2013, 139, 446–453. [Google Scholar] [CrossRef]
- Macherey, O.; Carlyon, R.P. Cochlear Implants. Curr. Biol. 2014, 24, R878–R884. [Google Scholar] [CrossRef]
- Wilson, B. A Treatise on Electricity, 2nd ed.; Davis: London, UK, 1752; pp. 202–208. [Google Scholar]
- Volta, A. On the Electricity Excited by the Mere Contact of Conducting Substances of Different Kinds. Philos. Trans. 1800, 90, 403–431. [Google Scholar] [CrossRef]
- Duchenne, G.B.A. De L’électrisation Localisée et de son Application à la Physiologie, à la Pathologie et à la Thérapeutique; Baillière: Paris, France, 1855; Volume 73, pp. 807–813. [Google Scholar]
- Potter, L.F. Electric Ostephone. U.S. Patent 792162, 13 June 1905. [Google Scholar]
- Wever, E.G.; Bray, C. The Nature of Acoustic Response: The Relation Between Sound Frequency and Frequency of Impulse in the Auditory Nerve. J. Exp. Psychol. 1930, 11, 373–387. [Google Scholar] [CrossRef]
- Gersuni, G.V.; Volokhov, A.A. On the Electrical Excitability of the Auditory Organ: The Effect of Alternating Currents on the Normal Auditory Apparatus. J. Exp. Psychol. 1936, 19, 370–382. [Google Scholar] [CrossRef]
- Dudley, H. Remaking Speech. J. Acoust. Soc. Am. 1939, 11, 1969–1977. [Google Scholar] [CrossRef]
- Jones, R.C.; Stevens, S.S.; Lurie, M.H. Three Mechanisms of Hearing by Electrical Stimulation. J. Acoust. Soc. Am. 1940, 12, 281–290. [Google Scholar] [CrossRef]
- Deep, N.L.; Dowling, E.M.; Jethanamest, D.; Carlson, M.L. Cochlear Implantation: An Overview. J. Neurol. Surg. B Skull Base 2019, 80, 169–177. [Google Scholar] [CrossRef]
- Djourno, A.; Eyries, C. Auditory Prosthesis by Means of a Distant Electrical Stimulation of the Sensory Nerve with the Use of an Indwelt Coiling. Presse Med. 1957, 65, 1417. [Google Scholar]
- Doyle, J.; Doyle, D.; House, W. Electrical Stimulation of Eight Nerve Deafness. Bull. Los Angeles Neurol. Soc. 1963, 28, 148–150. [Google Scholar]
- Simmons, F.B. Electrical Stimulation of the Auditory Nerve in Man. Arch. Otolaryngol. 1966, 84, 2–54. [Google Scholar] [CrossRef] [PubMed]
- Merzenich, M.M.; Michelson, R.P.; Pettit, C.R.; Schindler, R.A.; Reid, M. Neural Encoding of Sound Sensation Evoked by Electrical Stimulation of the Acoustic Nerve. Ann. Otol. Rhinol. Laryngol. 1973, 82, 486–503. [Google Scholar] [CrossRef] [PubMed]
- Eshraghi, A.A.; Nazarian, R.; Telischi, F.F.; Rajguru, S.M.; Truy, E.; Gupta, C. The Cochlear Implant: Historical Aspects and Future Prospects. Anat Rec. 2012, 295, 1967–1980. [Google Scholar] [CrossRef] [PubMed]
- Bilger, R.C.; Black, F.O. Auditory Prostheses in Perspective. Ann. Otol. Rhinol. Laryngol. 1977, 86, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Clark, G.M.; Tong, Y.C.; Black, R.; Forster, I.C.; Patrick, J.F.; Dewhurst, D.J. A Multiple-Electrode Cochlear Implant. J. Otolaryngol. Soc. Austral. 1978, 4, 208–212. [Google Scholar] [CrossRef] [PubMed]
- Rauterkus, G.; Maxwell, A.K.; Kahane, J.B.; Lentz, J.J.; Arriaga, M.A. Conversations in Cochlear Implantation: The Inner Ear Therapy of Today. Biomolecules 2022, 12, 649. [Google Scholar] [CrossRef] [PubMed]
- Varadarajan, V.V.; Sydlowski, S.A.; Li, M.M.; Anne, S.; Adunka, O.F. Evolving Criteria for Adult and Pediatric Cochlear Implantation. Ear Nose Throat J. 2021, 100, 31–37. [Google Scholar] [CrossRef]
- Mangabeira Albernaz, P.L. History of Cochlear Implants. Braz. J. Otorhinolaryngol. 2015, 81, 124–125. [Google Scholar] [CrossRef]
- Wilson, B.S.; Dorman, M.F. Cochlear Implants: A Remarkable Past and a Brilliant Future. Hear. Res. 2008, 242, 3–21. [Google Scholar] [CrossRef]
- Gifford, R.; Shallop, J.; Peterson, A. Speech Recognition Materials and Ceiling Effects: Considerations for Cochlear Implant Programs. Audiol. Neurotol. 2008, 13, 193–205. [Google Scholar] [CrossRef]
- Tamati, T.; Pisoni, D.B.; Moberly, A.C. Speech and Language Outcomes in Adults and Children with Cochlear Implants. Annu. Rev. Linguist. 2022, 8, 299–319. [Google Scholar] [CrossRef]
- Dhanasingh, A.; Hochmair, I. Bilateral Cochlear Implantation. Acta Otolaryngol. 2021, 141, 1–21. [Google Scholar] [CrossRef]
- Sturm, J.J.; Stern Shavit, S.; Vicario-Quinoñes, F.; Lalwani, A.K. Is Bilateral Cochlear Implantation Cost-Effective Compared to Unilateral Cochlear Implantation? Laryngoscope 2021, 131, 947–949. [Google Scholar] [CrossRef] [PubMed]
- Forli, F.; Bruschini, L.; Franciosi, B.; Berrettini, S.; Lazzerini, F. Sequential bilateral cochlear implant: Long-term speech perception results in children first implanted at an early age. Eur. Arch. Otorhinolaryngol. 2023, 280, 1073–1080. [Google Scholar] [CrossRef] [PubMed]
- Dhanasingh, A.; Hochmair, I. Signal processing & audio processors. Acta Otolaryngol. 2021, 141, 106–134. [Google Scholar] [PubMed]
- Pisoni, D.B.; Kronenberger, W.G.; Harris, M.S.; Moberly, A.C. Three Challenges for Future Research on Cochlear Implants. World J. Otorhinolaryngol. Head Neck Surg. 2018, 3, 240–254. [Google Scholar] [CrossRef] [PubMed]
- Levy, D.A.; Lee, J.A.; Nguyen, S.A.; McRackan, T.R.; Meyer, T.A.; Lambert, P.R. Cochlear Implantation for Treatment of Tinnitus in Single-sided Deafness: A Systematic Review and Meta-analysis. Otol. Neurotol. 2020, 41, e1004–e1012. [Google Scholar] [CrossRef] [PubMed]
- Lindquist, N.R.; Holder, J.T.; Patro, A.; Cass, N.D.; Tawfik, K.O.; O’Malley, M.R.; Bennett, M.L.; Haynes, D.S.; Gifford, R.H.; Perkins, E.L. Cochlear Implants for Single-Sided Deafness: Quality of Life, Daily Usage, and Duration of Deafness. Laryngoscope 2023, 133, 2362–2370. [Google Scholar] [CrossRef]
- Peters, J.P.M.; van Heteren, J.A.A.; Wendrich, A.W.; van Zanten, G.A.; Grolman, W.; Stokroos, R.J.; Smit, A.L. Short-term outcomes of cochlear implantation for single-sided deafness compared to bone conduction devices and contralateral routing of sound hearing aids-Results of a Randomised controlled trial (CINGLE-trial). PLoS ONE 2021, 16, e0257447. [Google Scholar] [CrossRef]
- Chandrasekar, B.; Hogg, E.S.; Patefield, A.; Strachan, L.; Sharma, S.D. Hearing outcomes in children with single sided deafness: Our experience at a tertiary paediatric otorhinolaryngology unit. Int. J. Pediatr. Otorhinolaryngol. 2023, 167, 111296. [Google Scholar] [CrossRef]
- Sharp, A.; Delcenserie, A.; Champoux, F. Auditory Event-Related Potentials Associated With Music Perception in Cochlear Implant Users. Front. Neurosci. 2018, 7, 538. [Google Scholar] [CrossRef] [PubMed]
- Spangmose, S.; Hjortkjær, J.; Marozeau, J. Perception of Musical Tension in Cochlear Implant Listeners. Front. Neurosci. 2019, 20, 987. [Google Scholar] [CrossRef]
- Salmon, M.K.; Quimby, A.E.; Bartellas, M.; Kaufman, H.S.; Bigelow, D.C.; Brant, J.A.; Ruckenstein, M.J. Long-Term Hearing Outcomes After Hybrid Cochlear Implantation. Otol. Neurotol. 2023, 44, 679–683. [Google Scholar] [CrossRef] [PubMed]
- Cooper, A. Hear Me Out: Hearing Each Other for the First Time-The Implications of Cochlear Implant Activation. Mo. Med. 2019, 116, 469–471. [Google Scholar]
- Putnam, B.; Alexander, S.P.; McMenamin, K.; Welch, D. Deaf community views on paediatric cochlear implantation. N. Z. Med. J. 2022, 135, 26–42. [Google Scholar]
- Chen, F.; Ni, W.; Li, W.; Li, H. Cochlear Implantation and Rehabilitation. Adv. Exp. Med. Biol. 2019, 1130, 129–144. [Google Scholar] [PubMed]
- Biever, A.; Kelsall, D.C.; Lupo, J.E.; Haase, G.M. Evolution of the Candidacy Requirements and Patient Perioperative Assessment Protocols for Cochlear Implantation. J. Acoust. Soc. Am. 2022, 152, 3346. [Google Scholar] [CrossRef]
- Yawn, R.J.; Nassiri, A.M.; Rivas, A. Auditory Neuropathy: Bridging the Gap Between Hearing Aids and Cochlear Implants. Otolaryngol. Clin. N. Am. 2019, 52, 349–355. [Google Scholar] [CrossRef]
- Bourn, S.S.; Goldstein, M.R.; Morris, S.A.; Jacob, A. Cochlear Implant Outcomes in the Very Elderly. Am. J. Otolaryngol. 2022, 43, 103200. [Google Scholar] [CrossRef] [PubMed]
- Shabashev, S.; Fouad, Y.; Huncke, T.K.; Roland, J.T. Cochlear Implantation Under Conscious Sedation with Local Anesthesia: Safety, Efficacy, Costs, and Satisfaction. Cochlear Implant. Int. 2017, 18, 297–303. [Google Scholar] [CrossRef]
- Spałek, J.; Ociepa, P.; Deptuła, P.; Piktel, E.; Daniluk, T.; Król, G.; Góźdź, S.; Bucki, R.; Okła, S. Biocompatible Materials in Otorhinolaryngology and Their Antibacterial Properties. Int. J. Mol. Sci. 2022, 23, 2575. [Google Scholar] [CrossRef] [PubMed]
- Bae, S.H.; Jung, Y.; Hur, J.H.; Kim, J.H.; Choi, J.Y. Feasibility of Speech Testing Using Wireless Connection in Single-Sided Cochlear Implant Users. J. Audiol. Otol. 2023, 27, 133–138. [Google Scholar] [CrossRef]
- Waltzman, S.B.; Kelsall, D.C. The Use of Artificial Intelligence to Program Cochlear Implants. Otol. Neurotol. 2020, 41, 452–457. [Google Scholar] [CrossRef] [PubMed]
- Trudel, M.; Morris, D.P. The Remaining Obstacles for a Totally Implantable Cochlear Implant. Curr. Opin. Otolaryngol. Head Neck Surg. 2022, 30, 298–302. [Google Scholar] [CrossRef]
- Forli, F.; Lazzerini, F.; Bruschini, L.; Danti, S.; Berrettini, S. Recent and future developments in cochlear implant technology: Review of the literature. Otorhinolaryngology 2021, 71, 196–207. [Google Scholar] [CrossRef]
- Lee, M.Y.; Park, Y.H. Potential of Gene and Cell Therapy for Inner Ear Hair Cells. Biomed. Res. Int. 2018, 2018, 8137614. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Athanasopoulos, M.; Samara, P.; Athanasopoulos, I. A Journey to Hear: The Evolution of Cochlear Implants. Encyclopedia 2024, 4, 125-136. https://doi.org/10.3390/encyclopedia4010011
Athanasopoulos M, Samara P, Athanasopoulos I. A Journey to Hear: The Evolution of Cochlear Implants. Encyclopedia. 2024; 4(1):125-136. https://doi.org/10.3390/encyclopedia4010011
Chicago/Turabian StyleAthanasopoulos, Michail, Pinelopi Samara, and Ioannis Athanasopoulos. 2024. "A Journey to Hear: The Evolution of Cochlear Implants" Encyclopedia 4, no. 1: 125-136. https://doi.org/10.3390/encyclopedia4010011
APA StyleAthanasopoulos, M., Samara, P., & Athanasopoulos, I. (2024). A Journey to Hear: The Evolution of Cochlear Implants. Encyclopedia, 4(1), 125-136. https://doi.org/10.3390/encyclopedia4010011