Risk Factors Associated with the Mortality of COVID-19 Patients Aged ≥60 Years Neither Intubated nor Treated with Mechanical Ventilation: A Multicentre Retrospective Cohort Study during the First Wave in Spain
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
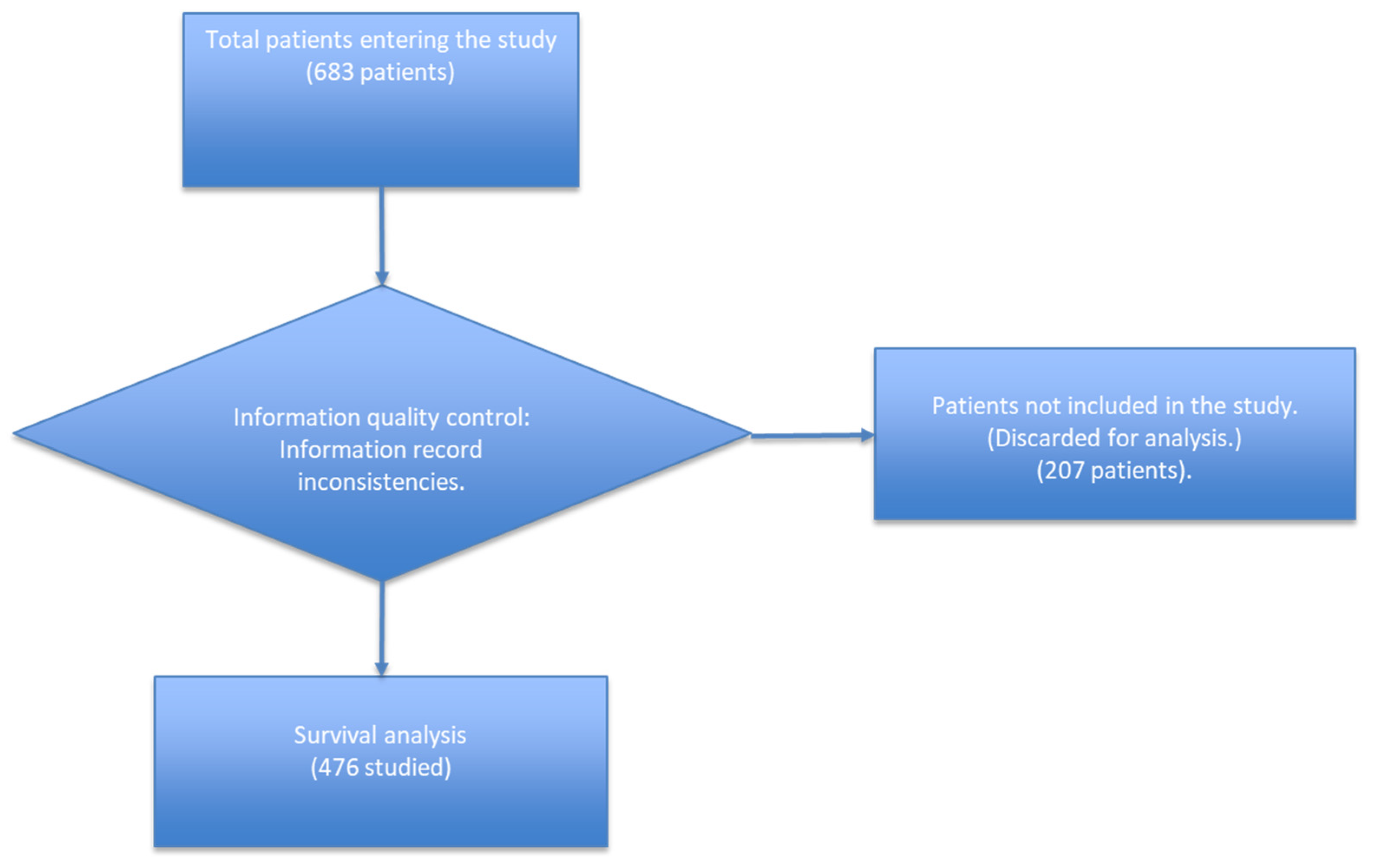
2.2. Sample
2.3. Long-Term Care Facilities
2.4. Variables
2.4.1. Human Biology
- Hypertension, auricular fibrillation, heart failure, ischemic heart disease, other cardiovascular diseases.
- Asthma, bronchitis, chronic obstructive pulmonary disease (COPD), other respiratory diseases.
- Diabetes, obesity, dyslipidaemia, other metabolic conditions.
- The term dyslipidaemia indicates an elevated concentration of lipids in the blood. There are several categories of this disorder, depending on which lipids are altered. The two most important forms are hypercholesterolaemia and hypertriglyceridaemia, although other disorders can be common, such as hyperchylomicronaemia or decreased HDL-cholesterol [9].
- Ictus, migraine, Parkinson’s disease, Alzheimer’s disease, cognitive impairment, other neurological diseases.
- Other conditions:
- −
- Neoplasia;
- −
- Chronic renal failure;
- −
- Low-frequency digestive pathology;
- −
- Anaemia;
- −
- Other.
- Geriatric syndrome: immobility, recurrent falls, pressure ulcers, malnutrition, incontinence, constipation, dysphagia, polypharmacy (more than 5 drugs), cognitive impairment, depression/insomnia and sensory impairment.
- Initial symptoms: fever, cough, malaise, dyspnoea, myalgia, fatigue, diarrhoea, nausea, other initial symptoms.
- The authors confirmed that all information about the whole medical history of these patients to the time of admission to care was confirmed with the patients’ medical records.
2.4.2. Lifestyles
2.4.3. COVID-19 Progression
2.4.4. Treatments:
- Azithromycin, ceftriaxone, other antibiotics.
- Corticoids and inhalers (INH): methylprednisolone, hydrocortisone, dexamethasone, salbutamol, ipratropium bromide, other inhalers.
- Other treatments: hydroxychloroquine (antimalarial), oxygen, antithrombotics, anti-platelet agents, antiviral and ivermectin.
2.5. Data Analysis
3. Results
4. Discussion
4.1. Demographic Variables
4.2. Geriatric Syndromes
4.3. Cardiovascular, Respiratory, Metabolic and Neurologic Comorbidities
4.4. Initial Symptoms
4.5. Treatment
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Coronavirus Disease 2019 (COVID-19) Situation Report-41; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Cesari, M.; Proietti, M. COVID-19 in Italy: Ageism and Decision Making in a Pandemic. J. Am. Med. Dir. Assoc. 2020, 21, 576–577. [Google Scholar] [CrossRef] [PubMed]
- Diaz, L.F. Vigilancia De Los Excesos De Mortalidad Por Todas Las Causas. MoMo. Available online: https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/MoMo/Documents/InformesMoMo2022/MoMo_Situacion%20a%202%20de%20febrero_CNE.pdf (accessed on 27 June 2022).
- Sezgin, D.; O’Caoimh, R.; Liew, A.; O’Donovan, M.R.; Illario, M.; Salem, M.A.; Kennelly, S.; Carriazo, A.M.; Lopez-Samaniego, L.; Carda, C.A.; et al. The effectiveness of intermediate care including transitional care interventions on function, healthcare utilisation and costs: A scoping review. Eur. Geriatr. Med. 2020, 11, 961–974. [Google Scholar] [CrossRef]
- Mena-Vázquez, N.; Manrique Arija, S.; Rojas-Giménez, M.; Raya-Álvarez, E.; Velloso-Feijoó, M.L.; López-Medina, C.; Ramos-Giraldez, C.; Godoy-Navarrete, F.J.; Redondo-Rodríguez, R.; Cabezas-Lucena, A.M.; et al. Hospitalization and Mortality from COVID-19 of Patients with Rheumatic Inflammatory Diseases in Andalusia. Reumatol. Clin. 2021, in press. [CrossRef] [PubMed]
- Gutiérrez Rodríguez, J.; Montero Muñoz, J.; Jiménez Muela, F.; Guirola García-Prendes, C.; Martínez Rivera, M.; Gómez Armas, L. Variables associated with mortality in a selected sample of patients older than 80 years and with some degree of functional dependence hospitalized for COVID-19 in a Geriatrics Service. Rev. Esp. Geriatr. Gerontol. 2020, 55, 317–325. [Google Scholar] [CrossRef]
- Dever, A.G.E. Epidemiología Y Administración De Servicios De Salud; Organización Panamericana de la Salud/Organización Mundial de la Salud: Washington, DC, USA, 1991. [Google Scholar]
- Ouchi, Y.; Rakugi, H.; Arai, H.; Akishita, M.; Ito, H.; Toba, K.; Kai, I. Redefining the elderly as aged 75 years and older: Proposal from the Joint Committee of Japan Gerontological Society and the Japan Geriatrics Society. Geriatr. Gerontol. Int. 2017, 17, 1045–1047. [Google Scholar] [CrossRef]
- Lozano, J.A. Dislipidemias. Offarm 2005, 24, 100–108. [Google Scholar]
- Cuschieri, S. The STROBE guidelines. Saudi J. Anaesth. 2019, 13, S31–S34. [Google Scholar] [CrossRef] [PubMed]
- Peckham, H.; de Gruijter, N.M.; Raine, C.; Radziszewska, A.; Ciurtin, C.; Wedderburn, L.R.; Rosser, E.C.; Webb, K.; Deakin, C.T. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat. Commun. 2020, 11, 6317. [Google Scholar] [CrossRef]
- Salinas-Escudero, G.; Carrillo-Vega, M.F.; Granados-García, V.; Martínez-Valverde, S.; Toledano-Toledano, F.; Garduño-Espinosa, J. A survival analysis of COVID-19 in the Mexican population. BMC Public Health 2020, 20, 1616. [Google Scholar]
- Kundu, S.; Chauhan, K.; Mandal, D. Survival analysis of patients with COVID-19 in india by demographic factors: Quantitative study. JMIR Form. Res. 2021, 5, e23251. [Google Scholar] [CrossRef]
- Iftimie, S.; López-Azcona, A.F.; Vicente-Miralles, M.; Descarrega-Reina, R.; Hernández-Aguilera, A.; Riu, F.; Simó, J.M.; Garrido, P.; Joven, J.; Camps, J.; et al. Risk factors associated with mortality in hospitalized patients with SARS-CoV-2 infection. A prospective, longitudinal, unicenter study in Reus, Spain. PLoS ONE 2020, 15, e0234452. [Google Scholar] [CrossRef] [PubMed]
- Bertsimas, D.; Lukin, G.; Mingardi, L.; Nohadani, O.; Orfanoudaki, A.; Stellato, B.; Wiberg, H.; Gonzalez-Garcia, S.; Parra-Calderón, C.L.; Robinson, K.; et al. COVID-19 mortality risk assessment: An international multi-center study. PLoS ONE 2020, 15, e0243262. [Google Scholar] [CrossRef] [PubMed]
- Petrilli, C.M.; Jones, S.A.; Yang, J.; Rajagopalan, H.; O’Donnell, L.; Chernyak, Y.; Tobin, K.A.; Cerfolio, R.J.; Francois, F.; Horwitz, L.I. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: Prospective cohort study. BMJ 2020, 369, m1966. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Ding, M.; Dong, X.; Zhang, J.; Kursat Azkur, A.; Azkur, D.; Gan, H.; Sun, Y.; Fu, W.; Li, W.; et al. Risk factors for severe and critically ill COVID-19 patients: A review. Allergy 2021, 76, 428–455. [Google Scholar] [CrossRef]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y.; et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef]
- Searle, S.D.; Mitnitski, A.; Gahbauer, E.A.; Gill, T.M.; Rockwood, K. A standard procedure for creating a frailty index. BMC Geriatr. 2008, 8, 24. [Google Scholar] [CrossRef]
- Sociedad Española de Geriatría y Gerontología Tratado de Geriatría. Available online: https://www.segg.es/tratadogeriatria/main.html (accessed on 23 July 2022).
- Rubenstein, L.Z. Geriatric assessment: An overview of its impacts. Clin. Geriatr. Med. 1987, 3, 1–15. [Google Scholar] [CrossRef]
- Salgado Alba, A.; Guillem Llera, F.; Ruipérez Cantera, I. Manual De Geriatría; Masson: Barcelona, Spain, 2003. [Google Scholar]
- Aprahamian, I.; Cesari, M. Geriatric Syndromes and SARS-CoV-2: More than Just Being Old. J. Frailty Aging 2020, 9, 127–129. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, L.K.; Jakobsen, L.H.; Hollensberg, L.; Ryg, J.; Midttun, M.; Frederiksen, H.; Glenthøj, A.; Kodahl, A.R.; Secher-Johnsen, J.; Nielsen, L.K.; et al. Clinical presentation and mortality in hospitalized patients aged 80+ years with COVID-19—A retrospective cohort study. Arch. Gerontol. Geriatr. 2021, 94, 104335. [Google Scholar] [CrossRef]
- Knopp, P.; Miles, A.; Webb, T.E.; Mcloughlin, B.C.; Mannan, I.; Raja, N.; Wan, B.; Davis, D. Presenting features of COVID-19 in older people: Relationships with frailty, inflammation and mortality. Eur. Geriatr. Med. 2020, 11, 1089–1094. [Google Scholar] [CrossRef] [PubMed]
- Williamson, E.J.; Walker, A.J.; Bhaskaran, K.; Bacon, S.; Bates, C.; Morton, C.E.; Curtis, H.J.; Mehrkar, A.; Evans, D.; Inglesby, P.; et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 2020, 584, 430–436. [Google Scholar] [CrossRef]
- Trecarichi, E.M.; Mazzitelli, M.; Serapide, F.; Pelle, M.C.; Tassone, B.; Arrighi, E.; Perri, G.; Fusco, P.; Scaglione, V.; Davoli, C.; et al. Clinical characteristics and predictors of mortality associated with COVID-19 in elderly patients from a long-term care facility. Sci. Rep. 2020, 10, 20834. [Google Scholar] [CrossRef] [PubMed]
- De Smet, R.; Mellaerts, B.; Vandewinckele, H.; Lybeert, P.; Frans, E.; Ombelet, S.; Lemahieu, W.; Symons, R.; Ho, E.; Frans, J.; et al. Frailty and Mortality in Hospitalized Older Adults With COVID-19: Retrospective Observational Study. J. Am. Med. Dir. Assoc. 2020, 21, 928–932.e1. [Google Scholar] [CrossRef]
- Chang, T.I.; Park, H.; Kim, D.W.; Jeon, E.K.; Rhee, C.M.; Kalantar-Zadeh, K.; Kang, E.W.; Kang, S.W.; Han, S.H. Polypharmacy, hospitalization, and mortality risk: A nationwide cohort study. Sci. Rep. 2020, 10, 18964. [Google Scholar] [CrossRef] [PubMed]
- Iaccarino, G.; Grassi, G.; Borghi, C.; Ferri, C.; Salvetti, M.; Volpe Massimo, M. Age and multimorbidity predict death among COVID-19 Patients: Results of the SARS-RAS study of the Italian society of hypertension. Hypertension 2020, 76, 366–372. [Google Scholar] [CrossRef] [PubMed]
- Turgeon, J.; Michaud, V.; Steffen, L. The dangers of polypharmacy in elderly patients. JAMA Intern. Med. 2017, 177, 1544. [Google Scholar] [CrossRef] [PubMed]
- Izcovich, A.; Ragusa, M.A.; Tortosa, F.; Marzio, M.A.L.; Agnoletti, C.; Bengolea, A.; Ceirano, A.; Espinosa, F.; Saavedra, E.; Sanguine, V.; et al. Prognostic factors for severity and mortality in patients infected with COVID-19: A systematic review. PLoS ONE 2020, 15, e0241955. [Google Scholar] [CrossRef]
- Zheng, Z.; Peng, F.; Xu, B.; Zhao, J.; Liu, H.; Peng, J.; Li, Q.; Jiang, C.; Zhou, Y.; Liu, S.; et al. Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. J. Infect. 2020, 81, e16–e25. [Google Scholar] [PubMed]
- Deng, G.; Yin, M.; Chen, X.; Zeng, F. Clinical determinants for fatality of 44,672 patients with COVID-Crit. Care 2020, 24, 179. [Google Scholar]
- Sanchis-Gomar, F.; Perez-Quilis, C.; Lavie, C.J. Should atrial fibrillation be considered a cardiovascular risk factor for a worse prognosis in COVID-19 patients? Eur. Heart J. 2020, 41, 3092–3093. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.K.; Gillies, C.L.; Singh, R.; Singh, A.; Chudasama, Y.; Coles, B.; Seidu, S.; Zaccardi, F.; Davies, M.J.; Khunti, K. Prevalence of co-morbidities and their association with mortality in patients with COVID-19: A systematic review and meta-analysis. Diabetes Obes. Metab. 2020, 22, 1915–1924. [Google Scholar] [CrossRef] [PubMed]
- Iftimie, S.; López-Azcona, A.F.; Vallverdú, I.; Hernández-Flix, S.; de Febrer, G.; Parra, S.; Hernández-Aguilera, A.; Riu, F.; Joven, J.; Andreychuk, N.; et al. First and second waves of coronavirus disease-19: A comparative study in hospitalized patients in Reus, Spain. PLoS ONE 2021, 16, e0248029. [Google Scholar] [CrossRef] [PubMed]
- Cangiano, B.; Fatti, L.M.; Danesi, L.; Gazzano, G.; Croci, M.; Vitale, G.; Gilardini, L.; Bonadonna, S.; Chiodini, I.; Caparello, C.F.; et al. Mortality in an Italian nursing home during COVID-19 pandemic: Correlation with gender, age, ADL, vitamin D supplementation, and limitations of the diagnostic tests. Aging 2020, 12, 24522–24534. [Google Scholar] [CrossRef]
- Rubio-Rivas, M.; Corbella, X.; Mora-Luján, J.M.; Loureiro-Amigo, J.; López Sampalo, A.; Yera Bergua, C.; Esteve Atiénzar, P.J.; Díez García, L.F.; Gonzalez Ferrer, R.; Plaza Canteli, S.; et al. Predicting Clinical Outcome with Phenotypic Clusters in COVID-19 Pneumonia: An Analysis of 12,066 Hospitalized Patients from the Spanish Registry SEMI-COVID-19. J. Clin. Med. 2020, 9, 3488. [Google Scholar] [CrossRef] [PubMed]
- Lippi, G.; Plebani, M. Laboratory abnormalities in patients with COVID-2019 infection. Clin. Chem. Lab. Med. 2020, 58, 1131–1134. [Google Scholar] [CrossRef] [PubMed]
- Rabaan, A.A.; Al-Ahmed, S.H.; Muhammad, J.; Khan, A.; Sule, A.A.; Tirupathi, R.; Al Mutair, A.; Alhumaid, S.; Al-Omari, A.; Dhawan, M.; et al. Role of Inflammatory Cytokines in COVID-19 Patients: A Review on Molecular Mechanisms, Immune Functions, Immunopathology and Immunomodulatory Drugs to Counter Cytokine Storm. Vaccines 2021, 9, 436. [Google Scholar] [CrossRef] [PubMed]
- Matli, K.; Farah, R.; Maalouf, M.; Chamoun, N.; Costanian, C.; Ghanem, G. Role of combining anticoagulant and antiplatelet agents in COVID-19 treatment: A rapid review. Open Heart 2021, 8, 1628. [Google Scholar] [CrossRef]
- Tang, N.; Bai, H.; Chen, X.; Gong, J.; Li, D.; Sun, Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J. Thromb. Haemost. 2020, 18, 1094–1099. [Google Scholar] [CrossRef] [PubMed]
- Paranjpe, I.; Fuster, V.; Lala, A.; Russak, A.J.; Glicksberg, B.S.; Levin, M.A.; Charney, A.W.; Narula, J.; Fayad, Z.A.; Bagiella, E.; et al. Association of Treatment Dose Anticoagulation with In-Hospital Survival among Hospitalized Patients with COVID-19. J. Am. Coll. Cardiol. 2020, 76, 122–124. [Google Scholar] [CrossRef] [PubMed]
- Billett, H.H.; Reyes-Gil, M.; Szymanski, J.; Ikemura, K.; Stahl, L.R.; Lo, Y.; Rahman, S.; Gonzalez-Lugo, J.D.; Kushnir, M.; Barouqa, M.; et al. Anticoagulation in COVID-19: Effect of Enoxaparin, Heparin, and Apixaban on Mortality. Thromb. Haemost. 2020, 120, 1691–1699. [Google Scholar] [PubMed]
- Hanif, A.; Khan, S.; Mantri, N.; Hanif, S.; Saleh, M.; Alla, Y.; Chinta, S.; Shrestha, N.; Ji, W.; Attwood, K.; et al. Thrombotic complications and anticoagulation in COVID-19 pneumonia: A New York City hospital experience. Ann. Hematol. 2020, 99, 2323–2328. [Google Scholar] [CrossRef]
- Fröhlich, G.M.; Jeschke, E.; Eichler, U.; Thiele, H.; Alhariri, L.; Reinthaler, M.; Kastrati, A.; Leistner, D.M.; Skurk, C.; Landmesser, U.; et al. Impact of oral anticoagulation on clinical outcomes of COVID-19: A nationwide cohort study of hospitalized patients in Germany. Clin. Res. Cardiol. 2021, 110, 1041–1050. [Google Scholar] [CrossRef] [PubMed]
- Bikdeli, B.; Madhavan, M.V.; Jimenez, D.; Chuich, T.; Dreyfus, I.; Driggin, E.; Der Nigoghossian, C.; Ageno, W.; Madjid, M.; Guo, Y.; et al. COVID-19 and Thrombotic or Thromboembolic Disease: Implications for Prevention, Antithrombotic Therapy, and Follow-Up: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2020, 75, 2950–2973. [Google Scholar] [CrossRef] [PubMed]
- Corrochano, M.; Acosta-Isaac, R.; Mojal, S.; Miqueleiz, S.; Rodriguez, D.; Quijada-Manuitt, M.Á.; Fraga, E.; Castillo-Ocaña, M.; Amaro-Hosey, K.; Albiol, N.; et al. Impact of pre-admission antithrombotic therapy on disease severity and mortality in patients hospitalized for COVID-19. J. Thromb. Thrombolysis 2022, 53, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Rossi, R.; Coppi, F.; Talarico, M.; Boriani, G. Protective role of chronic treatment with direct oral anticoagulants in elderly patients affected by interstitial pneumonia in COVID-19 era. Eur. J. Intern. Med. 2020, 77, 158–160. [Google Scholar] [CrossRef] [PubMed]
- Saifi, E.S.; Giorgi-Pierfranceschi, M.; Salvetti, M.; Maninetti, L.; Cavalli, I.; Muiesan, M.L. Factors associated with survival in older patients affected by COVID-19: A retrospective cohort study. Arch. Gerontol. Geriatr. 2021, 94, 104349. [Google Scholar] [CrossRef] [PubMed]
- Albani, F.; Fusina, F.; Granato, E.; Capotosto, C.; Ceracchi, C.; Gargaruti, R.; Santangelo, G.; Schiavone, L.; Taranto, M.S.; Tosati, C.; et al. Corticosteroid treatment has no effect on hospital mortality in COVID-19 patients. Sci. Rep. 2021, 11, 1015. [Google Scholar] [CrossRef]
- Monreal, E.; Sainz de la Maza, S.; Natera-Villalba, E.; Beltrán-Corbellini, Á.; Rodríguez-Jorge, F.; Fernández-Velasco, J.I.; Walo-Delgado, P.; Muriel, A.; Zamora, J.; Alonso-Canovas, A.; et al. High versus standard doses of corticosteroids in severe COVID-19: A retrospective cohort study. Eur. J. Clin. Microbiol. Infect. Dis. 2021, 40, 761–769. [Google Scholar] [CrossRef]
- Jeronimo, C.M.P.; Farias, M.E.L.; Val, F.F.A.; Sampaio, V.S.; Alexandre, M.A.A.; Melo, G.C.; Safe, I.P.; Borba, M.G.S.; Netto, R.L.A.; Maciel, A.B.S.; et al. Methylprednisolone as Adjunctive Therapy for Patients Hospitalized With Coronavirus Disease 2019 (COVID-19; Metcovid): A Randomized, Double-blind, Phase IIb, Placebo-controlled Trial. Clin. Infect. Dis. 2021, 72, E373–E381. [Google Scholar] [CrossRef]
- Piniella-Ruiz, E.; Bellver-Álvarez, M.T.; Mestre-Gómez, B.; Escolano-Fernández, B.; Vinat-Prado, S.; Cabezas-Olea, R.; Acedo-Gutiérrez, M.S.; Akasbi-Montalvo, M.; Ryan-Murua, P.; Bustamante-Fermosel, A.; et al. Impact of Systemic Corticosteroids on Mortality in Older Adults with Critical COVID-19 Pneumonia. J. Gerontol.-Ser. A Biol. Sci. Med. Sci. 2021, 76, E127–E132. [Google Scholar] [CrossRef]
- Fadel, R.; Morrison, A.R.; Vahia, A.; Smith, Z.R.; Chaudhry, Z.; Bhargava, P.; Miller, J.; Kenney, R.M.; Alangaden, G.; Ramesh, M.S.; et al. Early Short-Course Corticosteroids in Hospitalized Patients with COVID-19. Clin. Infect. Dis. 2020, 71, 2114–2120. [Google Scholar] [CrossRef] [PubMed]
- Pfizer Zithromax. Available online: https://www.pfizer.com/products/product-detail/zithromax (accessed on 23 July 2022).

| Factors | Variables | Mortality Rate | Total | Lethality Rate | From 60–74 | From 75 to 90 | From 91 to More | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Deaths | Total | Lethality Rate | Deaths | Total | Lethality Rate | Deaths | Total | Lethality Rate | |||||||||||||
| n | % | N | % | n | % | N | % | n | % | N | % | n | % | N | % | ||||||
| Total number of patients | 227 | 33% | 683 | 100% | 33% | 20 | 9% | 95 | 14% | 21% | 137 | 60% | 423 | 62% | 32% | 70 | 31% | 165 | 24% | 42% | |
| Intermediate care hospitals (social-health centers (HAI)) | Isabel Roig | 115 | 17% | 315 | 46% | 37% | 5 | 5% | 38 | 40% | 13% | 69 | 16% | 193 | 46% | 36% | 41 | 25% | 84 | 51% | 49% |
| Dolors Aleu | 52 | 8% | 195 | 29% | 27% | 7 | 7% | 34 | 36% | 21% | 30 | 7% | 118 | 28% | 25% | 15 | 9% | 43 | 26% | 35% | |
| Reus Hospital | 20 | 3% | 46 | 7% | 43% | 5 | 5% | 11 | 12% | 45% | 12 | 3% | 31 | 7% | 39% | 3 | 2% | 4 | 2% | 75% | |
| Centre Fòrum del Parc de Salut Mar. | 40 | 6% | 127 | 19% | 31% | 3 | 3% | 12 | 13% | 25% | 26 | 6% | 81 | 19% | 32% | 11 | 7% | 34 | 21% | 32% | |
| Gender | Male | 115 | 17% | 274 | 40% | 42% | 15 | 16% | 55 | 58% | 27% | 75 | 18% | 168 | 40% | 45% | 25 | 15% | 51 | 31% | 49% |
| Feminine | 112 | 16% | 409 | 60% | 27% | 5 | 5% | 40 | 42% | 13% | 62 | 15% | 255 | 60% | 24% | 45 | 27% | 114 | 69% | 39% | |
| Age group | 60–74 | 20 | 3% | 95 | 14% | 21% | |||||||||||||||
| 75–90 | 137 | 20% | 423 | 62% | 32% | ||||||||||||||||
| 91 to more | 70 | 10% | 165 | 24% | 42% | ||||||||||||||||
| Geriatric Syndromes | Immobility | 131 | 19% | 325 | 49% | 40% | 10 | 11% | 44 | 47% | 23% | 79 | 19% | 197 | 48% | 40% | 42 | 25% | 84 | 53% | 50% |
| Recurrent falls | 48 | 7% | 145 | 22% | 33% | 3 | 3% | 14 | 15% | 21% | 34 | 8% | 104 | 25% | 33% | 11 | 7% | 27 | 17% | 41% | |
| Pressure ulcers | 36 | 5% | 120 | 18% | 30% | 3 | 3% | 22 | 24% | 14% | 25 | 6% | 75 | 18% | 33% | 8 | 5% | 23 | 15% | 35% | |
| Malnutrition | 37 | 5% | 110 | 17% | 34% | 3 | 3% | 14 | 15% | 21% | 26 | 6% | 69 | 17% | 38% | 8 | 5% | 27 | 17% | 30% | |
| Incontinence | 137 | 20% | 397 | 59% | 35% | 11 | 12% | 44 | 47% | 25% | 74 | 17% | 235 | 57% | 31% | 52 | 32% | 118 | 73% | 44% | |
| Constipation | 86 | 13% | 288 | 44% | 30% | 6 | 7% | 29 | 31% | 21% | 50 | 12% | 182 | 45% | 27% | 30 | 18% | 77 | 48% | 39% | |
| Dysphagia | 44 | 6% | 105 | 19% | 42% | 0 | 0% | 14 | 16% | 0% | 30 | 7% | 67 | 19% | 45% | 14 | 8% | 24 | 18% | 58% | |
| Polypharmacy (+5 drugs) | 179 | 26% | 503 | 75% | 36% | 14 | 15% | 62 | 67% | 23% | 112 | 27% | 319 | 76% | 35% | 53 | 33% | 122 | 75% | 43% | |
| Cognitive impairment | 107 | 16% | 323 | 48% | 33% | 9 | 10% | 31 | 33% | 29% | 66 | 16% | 202 | 48% | 33% | 32 | 20% | 90 | 56% | 36% | |
| Depression/Anxiety | 77 | 11% | 265 | 40% | 29% | 10 | 11% | 38 | 41% | 26% | 42 | 10% | 162 | 39% | 26% | 25 | 15% | 65 | 40% | 38% | |
| Sensory Alterations | 88 | 13% | 267 | 42% | 33% | 6 | 7% | 26 | 29% | 23% | 52 | 12% | 168 | 42% | 31% | 30 | 18% | 73 | 47% | 41% | |
| Cardiovascular Diseases | Ischemic heart disease | 31 | 5% | 83 | 12% | 37% | 4 | 4% | 9 | 10% | 44% | 14 | 3% | 49 | 12% | 29% | 13 | 8% | 25 | 15% | 52% |
| Atrial Fibrillation | 72 | 11% | 166 | 24% | 43% | 3 | 3% | 11 | 12% | 27% | 43 | 10% | 108 | 26% | 40% | 26 | 16% | 47 | 29% | 55% | |
| Hypertension | 180 | 26% | 526 | 77% | 34% | 15 | 16% | 63 | 66% | 24% | 105 | 25% | 326 | 77% | 32% | 60 | 36% | 137 | 83% | 44% | |
| Heart failure | 56 | 8% | 140 | 21% | 40% | 2 | 2% | 7 | 7% | 29% | 32 | 8% | 93 | 22% | 34% | 23 | 14% | 42 | 26% | 55% | |
| Other Cardiovascular Diseases | 25 | 4% | 111 | 16% | 23% | 1 | 1% | 11 | 12% | 9% | 16 | 4% | 74 | 18% | 22% | 8 | 5% | 26 | 16% | 31% | |
| Peripheral Vascular Disease | 6 | 1% | 30 | 4% | 20% | 1 | 1% | 6 | 6% | 17% | 4 | 1% | 19 | 5% | 21% | 1 | 1% | 5 | 3% | 20% | |
| Non-Coronary Heart Disease | 3 | 0% | 25 | 100% | 12% | 2 | 2% | 3 | 3% | 67% | 2 | 1% | 15 | 4% | 13% | 0 | 0% | 7 | 4% | 0% | |
| Coronary Cardiopathy | 6 | 1% | 19 | 3% | 32% | 1 | 1.1% | 2 | 2.1% | 50% | 4 | 1% | 13 | 2% | 31% | 1 | 1% | 4 | 2% | 25% | |
| Electrical Conduction Disorder | 5 | 1% | 20 | 3% | 25% | 0 | 0.0% | 1 | 1.0% | 0% | 3 | 1% | 13 | 3% | 23% | 2 | 1% | 6 | 4% | 33% | |
| Respiratory Diseases | Asthma | 10 | 2% | 32 | 5% | 31% | 0 | 0% | 2 | 2% | 0% | 8 | 2% | 24 | 6% | 33% | 2 | 1% | 6 | 4% | 33% |
| Chronic Obstructive Pulmonary Disease (COPD) | 39 | 6% | 111 | 16% | 35% | 8 | 8% | 19 | 20% | 42% | 23 | 5% | 71 | 17% | 32% | 8 | 5% | 21 | 13% | 38% | |
| Other Respiratory Diseases | 15 | 2% | 50 | 7% | 30% | 2 | 2% | 7 | 7% | 29% | 10 | 2% | 33 | 8% | 30% | 3 | 2% | 10 | 6% | 30% | |
| Metabolic Diseases | Diabetes | 59 | 9% | 171 | 25% | 35% | 9 | 10% | 36 | 38% | 25% | 35 | 8% | 105 | 25% | 33% | 15 | 9% | 30 | 18% | 50% |
| Obesity | 19 | 3% | 82 | 12% | 23% | 1 | 1% | 15 | 16% | 7% | 10 | 2% | 54 | 13% | 19% | 8 | 5% | 13 | 8% | 62% | |
| Other Metabolic Diseases | 38 | 6% | 182 | 27% | 21% | 2 | 2% | 25 | 26% | 8% | 27 | 6% | 115 | 27% | 23% | 9 | 6% | 42 | 26% | 21% | |
| Dyslipidemia | 22 | 3% | 119 | 17% | 18% | 1 | 1% | 15 | 16% | 7% | 18 | 4% | 80 | 19% | 23% | 3 | 2% | 24 | 15% | 13% | |
| Osteoporosis | 3 | 0% | 30 | 4% | 10% | 1 | 1% | 3 | 3% | 33% | 2 | 1% | 21 | 5% | 10% | 0 | 0% | 6 | 4% | 0% | |
| Hypothyroidism | 12 | 2% | 33 | 5% | 36% | 0 | 0% | 3 | 3% | 0% | 8 | 2% | 20 | 5% | 40% | 4 | 2% | 10 | 6% | 40% | |
| Neurological Diseases | Ictus | 40 | 6% | 111 | 16% | 36% | 3 | 3% | 15 | 16% | 20% | 24 | 6% | 70 | 17% | 34% | 13 | 8% | 26 | 16% | 50% |
| Migraine | 7 | 1% | 24 | 4% | 29% | 2 | 2% | 5 | 5% | 40% | 5 | 1% | 18 | 4% | 28% | 0 | 0% | 1 | 1% | 0% | |
| Parkinson’s | 13 | 2% | 27 | 4% | 48% | 1 | 1% | 3 | 3% | 33% | 10 | 2% | 20 | 5% | 50% | 2 | 1% | 4 | 2% | 50% | |
| Alzheimer’s | 23 | 3% | 67 | 10% | 34% | 1 | 1% | 5 | 5% | 20% | 11 | 3% | 42 | 10% | 26% | 11 | 7% | 20 | 12% | 55% | |
| Other dementias | 48 | 7% | 137 | 20% | 35% | 1 | 1% | 10 | 11% | 10% | 28 | 7% | 88 | 21% | 32% | 19 | 12% | 39 | 24% | 49% | |
| Other Neurological Diseases | 32 | 5% | 92 | 14% | 35% | 3 | 3% | 23 | 24% | 13% | 23 | 5% | 53 | 13% | 43% | 6 | 4% | 16 | 10% | 38% | |
| Other Dementias 1a | 68 | 10% | 192 | 28% | 35% | 2 | 2% | 14 | 15% | 14% | 42 | 10% | 128 | 30% | 33% | 24 | 15% | 50 | 30% | 48% | |
| Other Pathologies | Other Pathologies | 96 | 14% | 380 | 56% | 25% | 10 | 11% | 56 | 59% | 18% | 64 | 15% | 236 | 56% | 27% | 22 | 13% | 88 | 53% | 25% |
| Neoplasia b | 30 | 4% | 107 | 16% | 28% | 6 | 6% | 17 | 18% | 35% | 20 | 5% | 70 | 17% | 29% | 4 | 2% | 20 | 12% | 20% | |
| Chronic renal failure | 21 | 3% | 85 | 12% | 25% | 1 | 1% | 8 | 8% | 13% | 16 | 4% | 53 | 13% | 30% | 4 | 2% | 24 | 15% | 17% | |
| Lower Frequency Digestive Pathology c | 3 | 0% | 28 | 4% | 11% | 0 | 0% | 5 | 5% | 0% | 3 | 1% | 18 | 4% | 17% | 0 | 0% | 5 | 3% | 0% | |
| Anemia | 2 | 0% | 22 | 3% | 9% | 0 | 0% | 1 | 1% | 0% | 1 | 0% | 13 | 3% | 8% | 1 | 1% | 8 | 5% | 13% | |
| Initial Symptoms | Fever | 157 | 23% | 392 | 57% | 40% | 17 | 18% | 60 | 63% | 28% | 97 | 23% | 244 | 58% | 40% | 43 | 26% | 88 | 53% | 49% |
| Cough | 64 | 9% | 230 | 34% | 28% | 2 | 2% | 27 | 28% | 7% | 39 | 9% | 143 | 34% | 27% | 23 | 14% | 60 | 36% | 38% | |
| General discomfort | 95 | 14% | 240 | 35% | 40% | 8 | 8% | 33 | 35% | 24% | 61 | 14% | 159 | 38% | 38% | 26 | 16% | 48 | 29% | 54% | |
| Dyspnoea | 133 | 19% | 298 | 44% | 45% | 12 | 13% | 35 | 37% | 34% | 78 | 18% | 181 | 43% | 43% | 43 | 26% | 82 | 50% | 52% | |
| Myalgia | 10 | 2% | 45 | 7% | 22% | 0 | 0% | 5 | 5% | 0% | 4 | 1% | 31 | 7% | 13% | 6 | 4% | 9 | 6% | 67% | |
| Fatigue | 33 | 5% | 82 | 12% | 40% | 3 | 3% | 10 | 11% | 30% | 19 | 5% | 53 | 13% | 36% | 11 | 7% | 19 | 12% | 58% | |
| Diarrhea | 9 | 1% | 73 | 11% | 12% | 1 | 1% | 13 | 14% | 8% | 4 | 1% | 44 | 10% | 9% | 4 | 2% | 16 | 10% | 25% | |
| Nausea and vomiting | 7 | 1% | 29 | 4% | 24% | 0 | 0% | 2 | 2% | 0% | 4 | 1% | 22 | 5% | 18% | 3 | 2% | 5 | 3% | 60% | |
| Other Symptoms | 13 | 2% | 40 | 6% | 33% | 2 | 2% | 6 | 6% | 33% | 10 | 2% | 25 | 6% | 40% | 1 | 1% | 9 | 6% | 11% | |
| Administered Therapies | Antibiotics | ||||||||||||||||||||
| Hydroxychloroquine | 102 | 15% | 296 | 43% | 34% | 7 | 7% | 33 | 35% | 21% | 64 | 15% | 192 | 45% | 33% | 31 | 19% | 71 | 43% | 44% | |
| Azithromycin | 127 | 19% | 387 | 57% | 33% | 8 | 8% | 43 | 45% | 19% | 80 | 19% | 240 | 57% | 33% | 39 | 24% | 104 | 63% | 38% | |
| Ceftriaxone | 90 | 13% | 234 | 34% | 38% | 9 | 10% | 22 | 23% | 41% | 49 | 12% | 138 | 33% | 36% | 32 | 19% | 74 | 45% | 43% | |
| Other Antibiotics | 71 | 10% | 159 | 23% | 45% | 4 | 4% | 22 | 23% | 18% | 50 | 12% | 95 | 23% | 53% | 17 | 10% | 42 | 26% | 40% | |
| Hydroxychloroquine-Azithromycin d | 141 | 21% | 433 | 63% | 33% | 9 | 10% | 53 | 56% | 17% | 88 | 21% | 266 | 63% | 33% | 44 | 27% | 114 | 69% | 39% | |
| Hydroxychloroquine and Azithromycin e | 88 | 13% | 250 | 37% | 35% | 6 | 6% | 23 | 24% | 26% | 56 | 13% | 166 | 39% | 34% | 26 | 16% | 61 | 37% | 43% | |
| Corticosteroids and inhalers | |||||||||||||||||||||
| Methylprednisolone | 86 | 13% | 192 | 28% | 45% | 5 | 5% | 18 | 19% | 28% | 58 | 14% | 131 | 31% | 44% | 23 | 14% | 43 | 26% | 53% | |
| Prednisone | 5 | 1% | 22 | 3% | 23% | 0 | 0% | 5 | 5% | 0% | 5 | 1% | 10 | 2% | 50% | 0 | 0% | 7 | 4% | 0% | |
| Hydrocortisone | 6 | 1% | 14 | 2% | 43% | 0 | 0% | 1 | 1% | 0% | 5 | 1% | 10 | 2% | 50% | 1 | 1% | 3 | 2% | 33% | |
| Dexamethasone f | 11 | 2% | 28 | 22% | 39% | 0 | 0% | 1 | 8% | 0% | 6 | 7% | 16 | 20% | 38% | 5 | 3% | 11 | 32% | 45% | |
| Salbutamol | 49 | 7% | 97 | 14% | 51% | 4 | 4% | 10 | 11% | 40% | 32 | 8% | 65 | 15% | 49% | 13 | 8% | 22 | 13% | 59% | |
| Ipratropium bromide | 78 | 11% | 168 | 25% | 46% | 7 | 7% | 20 | 21% | 35% | 47 | 11% | 102 | 24% | 46% | 24 | 15% | 46 | 28% | 52% | |
| Other inhalers | 15 | 2% | 63 | 9% | 24% | 0 | 0% | 10 | 11% | 0% | 12 | 3% | 46 | 11% | 26% | 3 | 2% | 7 | 4% | 43% | |
| Others | |||||||||||||||||||||
| Use of Antinthrombotic and/or Antiplatelet | 103 | 15% | 391 | 57% | 26% | 10 | 11% | 54 | 57% | 19% | 64 | 15% | 248 | 59% | 26% | 29 | 18% | 89 | 54% | 33% | |
| Antithrombotic Agent | 111 | 16% | 376 | 55% | 30% | 20 | 21% | 95 | 100% | 21% | 40 | 10% | 168 | 40% | 24% | 51 | 31% | 113 | 69% | 45% | |
| Platelet Antiplatelet | 25 | 4% | 37 | 5% | 68% | 0 | 0% | 0 | 0% | 0% | 7 | 2% | 7 | 2% | 100% | 18 | 11% | 30 | 18% | 60% | |
| Antivirals | 8 | 1% | 46 | 7% | 17% | 1 | 1% | 10 | 11% | 10% | 6 | 1% | 28 | 7% | 21% | 1 | 1% | 8 | 5% | 13% | |
| Variables | Frequency | Deaths | Mean | |||
|---|---|---|---|---|---|---|
| Limit Product Estimator or Kaplan–Meier | Desv. Error | 95% Confidence Interval (CI) | ||||
| Lower Limit | Upper Limit | |||||
| General | 475 | 186 | 21.92 | 0.48 | 20.98 | 22.86 |
| Male | 279 | 95 | 23.01 | 0.61 | 21.81 | 24.22 |
| Feminine | 196 | 91 | 20.37 | 0.75 | 18.90 | 21.84 |
| From 60 to 74 | 55 | 17 | 22.20 | 1.37 | 19.51 | 24.89 |
| From 75 to 90 | 296 | 107 | 22.34 | 0.60 | 21.15 | 23.52 |
| From 91 to more | 124 | 62 | 20.63 | 0.93 | 18.80 | 22.45 |
| Factors | Variables | Total Population (N = 475) (adjusted) | Population 60–74 (n = 55) | Population 75–90 (n = 296) | Population 91 to More (n = 124) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| p. Value | HR | * IC | p. Value | HR | * IC | p. Value | HR | * IC | p. Value | HR | * IC | ||
| Sex | Male | NS | NS | NS | NS | NS | NS | 0.003 | 1.77 | (1.215–2.599) | NS | NS | NS |
| Feminine | |||||||||||||
| Age | 60–74 | NS | REF | REF | |||||||||
| 75–90 | NS | 1082 | (0.65–1.80) | ||||||||||
| 91 to more | NS | 1488 | (0.87–2.55) | ||||||||||
| Geriatric Syndromes | Urinary incontinence | NS | NS | NS | 0.034 | 17.15 | (1.25–236.0) | NS | NS | NS | NS | NS | NS |
| Constipation | NS | NS | NS | 0.048 | 4.36 | (1.01–18.85) | NS | NS | NS | NS | NS | NS | |
| Polypharmacy | NS | NS | NS | NS | NS | NS | 0.045 | 1.79 | (1.01–3.16) | NS | NS | NS | |
| Cardiovascular Diseases | Atrial Fibrillation | 0.035 | 1452 | (1.03–2.05) | NS | NS | NS | 0.006 | 1.86 | (1.20–2.89) | NS | NS | NS |
| Respiratory Diseases | Chronic Obstructive Pulmonary Disease (COPD) | NS | NS | NS | 0.029 | 3.08 | (1.12–8.44) | NS | NS | NS | NS | NS | NS |
| Metabolic Diseases | Dyslipidemia | 0.007 | 0.474 | (0.28–0.82) | NS | NS | NS | NS | NS | NS | 0.048 | 0.16 | (0.03–0.99) |
| Neurological Diseases | Migraine | NS | NS | NS | 0.011 | 23.14 | (2.04–262.83) | NS | NS | NS | NS | NS | NS |
| Other Pathologies | Neoplasia | NS | NS | NS | 0.007 | 5768 | (1.62–20.52) | NS | NS | NS | NS | NS | NS |
| Initial Symptoms | Fever | 0.024 | 1500 | (1.06–2.13) | NS | NS | NS | 0.003 | 2.00 | (1.27–3.13) | NS | NS | NS |
| Cough | 0.023 | 0.656 | (0.46–0.94) | NS | NS | NS | 0.034 | 0.62 | (0.40–0.97) | NS | NS | NS | |
| General discomfort | 0.028 | 1437 | (1.04–1.99) | NS | NS | NS | 0.007 | 1.77 | (1.17–2.69) | NS | NS | NS | |
| Dyspnoea | p < 0.001 | 1984 | (1.41–2.79) | 0.013 | 4.75 | (1.39–16.20) | p < 0.001 | 2.27 | (1.51–3.41) | 0.002 | 2.52 | (1.40–4.57) | |
| Diarrhea | 0.027 | 0.459 | (0.23–0.92) | NS | NS | NS | 0.014 | 0.27 | (0.10–0.77) | NS | NS | NS | |
| Antibiotic treatments | Azithromycin | NS | NS | NS | NS | NS | NS | NS | NS | NS | 0.043 | 0.50 | (0.23–0.98) |
| Ceftriaxone | 0.055 | 1455 | (0.99–2.13) | 0.005 | 4.49 | (1.58–12.70) | NS | NS | NS | NS | NS | NS | |
| Corticosteroid treatments | Methylprednisolone | NS | NS | NS | NS | NS | NS | 0.034 | 1.60 | (1.04–2.53) | NS | NS | NS |
| Other treatments | Antithrombotic agent | 0.001 | 0.559 | (0.40–0.78) | NS | NS | NS | 0.001 | 0.53 | (0.36–0.78) | 0.007 | 0.488 | (0.29–0.82) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Culqui, D.R.; Ortega Segura, J.; Da Costa-Venancio, E.; Renom-Guiteras, A.; Roquer, E.; Muñoz Tejada, S.M.; Rodriguez, P.; Alba Travieso, A.L.; Medrano, I.; Canchucaja-Gutarra, L.; et al. Risk Factors Associated with the Mortality of COVID-19 Patients Aged ≥60 Years Neither Intubated nor Treated with Mechanical Ventilation: A Multicentre Retrospective Cohort Study during the First Wave in Spain. BioMed 2022, 2, 341-358. https://doi.org/10.3390/biomed2030027
Culqui DR, Ortega Segura J, Da Costa-Venancio E, Renom-Guiteras A, Roquer E, Muñoz Tejada SM, Rodriguez P, Alba Travieso AL, Medrano I, Canchucaja-Gutarra L, et al. Risk Factors Associated with the Mortality of COVID-19 Patients Aged ≥60 Years Neither Intubated nor Treated with Mechanical Ventilation: A Multicentre Retrospective Cohort Study during the First Wave in Spain. BioMed. 2022; 2(3):341-358. https://doi.org/10.3390/biomed2030027
Chicago/Turabian StyleCulqui, Dante R., Josep Ortega Segura, Elisabeth Da Costa-Venancio, Anna Renom-Guiteras, Esther Roquer, Sherly Melissa Muñoz Tejada, Patricia Rodriguez, Adilis L. Alba Travieso, Isis Medrano, Lizzeth Canchucaja-Gutarra, and et al. 2022. "Risk Factors Associated with the Mortality of COVID-19 Patients Aged ≥60 Years Neither Intubated nor Treated with Mechanical Ventilation: A Multicentre Retrospective Cohort Study during the First Wave in Spain" BioMed 2, no. 3: 341-358. https://doi.org/10.3390/biomed2030027
APA StyleCulqui, D. R., Ortega Segura, J., Da Costa-Venancio, E., Renom-Guiteras, A., Roquer, E., Muñoz Tejada, S. M., Rodriguez, P., Alba Travieso, A. L., Medrano, I., Canchucaja-Gutarra, L., Herrero-Torrus, M., Jurado-Marín, P., Marín-Casino, M., Sabaté-Garcia, R. A., Roqueta, C., Martinez, M. d. C., De Febrer, G., López-Bueno, J. A., Navas-Martín, M., ... Cayla, J. A. (2022). Risk Factors Associated with the Mortality of COVID-19 Patients Aged ≥60 Years Neither Intubated nor Treated with Mechanical Ventilation: A Multicentre Retrospective Cohort Study during the First Wave in Spain. BioMed, 2(3), 341-358. https://doi.org/10.3390/biomed2030027







