- Article
Autophagy Activation in Mesenchymal Stem Cells with Lithium Chloride and Trehalose: Implications for Regenerative Medicine
- Ali Fouad,
- Yasser ElSherbini and
- Mohamed Abdraboh
- + 1 author
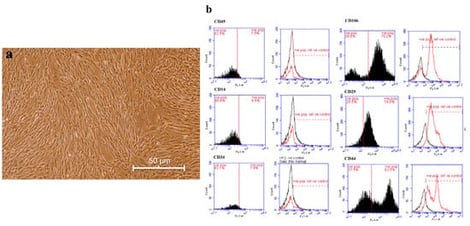
Background/Objectives: Mesenchymal stem cells (MSCs) are deemed to be a highly safe model for autologous and allogeneic cellular therapy, owing to their inherent lack of HLA-DR expression, immunomodulatory properties, homing ability, and plasticity allowing differentiation into different cell types. The interest in activating autophagic signaling in MSCs has recently grown due to its significant potential in maintaining stemness, enhancing paracrine signaling, and providing therapeutic benefits for cancer and neurodegenerative diseases. This study aimed to explore the impact of autophagy induction on enhancing the therapeutic potential of MSCs by maintaining their plasticity and to assess different induction agents. Methods: In this study, MSCs were first extracted from the fat tissue of Sprague–Dawley (SD) rats and characterized phenotypically and molecularly by their positive expression of stemness markers CD29, CD106, and CD44, and their negative expression of hematopoietic surface markers CD14, CD34, and CD45, using a flow cytometry approach. Isolated MSCs were then treated separately with two FDA-approved autophagy inducers: Lithium Chloride and Trehalose, following assessment of autophagy activity. Results: Treated MSCs showed significant increases in autophagic activity at both the transcriptional and translational levels. The successful induction of autophagy in MSCs was confirmed through the elevated expression of autophagy-related genes such as ATG3, ATG13, ATG14, P62, and ULK1. These data were confirmed by the significant upregulation in LC3 protein expression and the formation of autophagosomes, which was detected using a transmission electron microscope. Furthermore, the expression of Oct4, Sox2, and Nanog genes was significantly enhanced after treatment with Trehalose and Lithium Chloride compared with untreated control MSCs which may indicate an upregulation of pluripotency. Meanwhile, Lithium Chloride and Trehalose did not significantly induce cellular apoptosis, indicated by the Bax/Bcl-2 expression ratio, and significantly decreased the expression of the antioxidant markers SOD and GPx. Conclusions: Treatment of MSCs with Trehalose and, in particular, Lithium Chloride significantly activated autophagic signaling, which showed a profound effect in enhancing cells’ pluripotency, reinforcing the usage of treated MSCs for autologous and/or allogenic cellular therapy. However, further in vivo studies for activating autophagy in cellular grafts should be conducted before their use in clinical trials.
16 January 2026



![Imaging and endoscopic findings of intramural esophageal abscess secondary to suspected fish bone injury. (A) Chest radiograph showing no evidence of pneumomediastinum. (B) Contrast-enhanced CT of the neck demonstrating circumferential thickening of the cervical esophageal wall with a well-demarcated, low-attenuation intramural collection and mild adjacent fat stranding (arrow). (C) Upper endoscopy revealing submucosal bulging and a pinpoint mucosal defect with active pus discharge in the upper esophagus (arrow), without signs of transmural perforation or a retained foreign body. (D) Water-soluble contrast esophagogram showing smooth passage of contrast without extravasation, obstruction, or double-lumen sign, consistent with an intramural lesion. (E) Follow-up CT on day 7 indicating an interval reduction of the intramural fluid collection. The etiology of esophageal abscess, which is a rare intramural infection caused by mucosal breach without full-thickness perforation [1,2], includes iatrogenic trauma and contiguous spread, and fish bone ingestion is a leading trigger in East Asia [1,2,3,4]. The symptoms of esophageal abscess are nonspecific, and early radiographs are often normal; therefore, contrast-enhanced computed tomography (CT) should be prioritized in cases with suspicious esophageal injury [2,3,5,6,7]. Here, we report the case of a patient diagnosed with cervical esophageal abscess following fish bone impaction to underscore the need for early CT and increased clinical vigilance for the timely diagnosis of this under-recognized condition. The patient was a 57-year-old man. His medical history was notable for hypertension treated with amlodipine; he had no prior surgical history, reported a 33-year smoking history, and denied alcohol use. He presented with a 1-day history of fever and progressive odynophagia that began 3 days after a suspected fish bone impaction. Upon arrival, his vital signs were as follows: temperature, 37.7 °C; heart rate, 107 beats/min; respiratory rate, 18 breaths/min; and blood pressure, 135/66 mmHg. Neck erythema, swelling, and subcutaneous emphysema were absent on physical examination. Laboratory tests revealed leukocytosis (17,400/µL) and an elevated C-reactive protein level (8.93 mg/dL). Chest radiography was normal, ruling out pneumomediastinum (A). Contrast-enhanced CT of the neck showed circumferential thickening of the cervical esophageal wall with a well-demarcated, intramural collection with low attenuation and mild fat stranding in adjacent tissue in the absence of extraluminal air, supporting the diagnosis of intramural esophageal abscess (B). Upper endoscopy revealed submucosal bulging with a pinpoint mucosal defect that was actively discharging pus in the upper esophagus without transmural perforation or a clear sign of a retained foreign body (C). Water-soluble contrast esophagogram confirmed smooth passage without extravasation, obstruction, or the double-lumen sign, supporting the diagnosis of an intramural lesion (D). Blood cultures and pus cultures obtained during endoscopy showed no bacterial growth. The patient was initially kept nil per os and maintained with intravenous fluids for 5 days. He was treated conservatively with intravenous piperacillin/tazobactam and close observation, leading to improvement in symptoms and inflammatory marker levels. For pain control, he required only intermittent NSAID injections. The follow-up CT on day 7 of admission revealed a decline in the intramural fluid accumulation (E). He completed a 10-day course of intravenous piperacillin/tazobactam and was discharged without complications, with an additional 5-day course of oral amoxicillin/clavulanate prescribed after discharge. The patient was followed in the outpatient clinic at 1 week, 3 weeks, and 3 months. He reported no persistent or recurrent symptoms at all follow-up visits. Laboratory tests at 1 week and 3 months demonstrated normal WBC and CRP levels. Repeat CT or endoscopy was discussed, but the patient declined further evaluation because he remained asymptomatic. Esophageal abscess, an uncommon presentation, results from a mucosal laceration that enables intraluminal infection to extend into the submucosa, leading to longitudinal intramural collection without causing full-thickness perforation [1,2]. Esophageal abscesses are most commonly reported in older women and after iatrogenic manipulation or anticoagulation treatment [2]. Although rare, descending infection from parapharyngeal or tonsillar sources has also been documented [1]. In East Asia, fish bones are the predominant cause of esophageal foreign bodies, reported as the cause in 46–72% of all reported esophageal abscesses, and delayed presentation beyond 24 h increases the risk of perforation and the development of mediastinal abscesses [4]. Typically, fish bones lodge in the cervical or upper thoracic esophagus, whereas meat boluses tend to impact at more distal sites with physiologic narrowing, such as the esophageal hiatus [3,5]. Patients with esophageal abscesses typically present with retrosternal chest pain, odynophagia, dysphagia, and occasionally hematemesis [2]. Early chest or neck radiographs are often unremarkable, which can delay diagnosis [2]. CT is the most sensitive modality for detecting fish bones and intramural collections [3,5,8]. Differential diagnosis includes intramural dissection, characterized by a mucosal flap and the double-lumen sign on esophagography [7,9,10], and phlegmonous esophagitis, defined as a diffuse suppurative mural infection with rapid systemic deterioration [1]. In the present case, CT revealed a localized submucosal cavity, endoscopy showed a pinpoint draining defect, and contrast esophagogram excluded leaks and the double-lumen sign, consistent with the diagnosis of an intramural abscess. The management of esophageal abscesses centers on early sepsis control, withholding oral intake, administration of broad-spectrum intravenous antibiotics targeting oral aerobic and anaerobic flora, early nutritional support, and cross-sectional CT to determine the extent of involvement and plan intervention [1,6]. Conservative management is appropriate when the patient is hemodynamically stable without clinical sepsis, and imaging suggests a contained intramural lesion without extraluminal air or contrast leak and without extensive mediastinal or pleural contamination [1,6]. In patients with intramural collections without transmural perforation, endoscopic mucosal incision/intraluminal drainage achieves rapid decompression with clinical and radiologic resolution, and is increasingly preferred as the first-line therapeutic option [11,12]. In patients with an extensive esophageal abscess and those for whom endoscopic therapy is not feasible, surgical drainage with thoracotomy and placement of intramural and pleural drains may be necessary, while percutaneous catheter drainage can control persistent mediastinal or abdominal sepsis [1,4]. Cultures commonly yield oral streptococci [4,6], and antibiotic regimens should be tailored and de-escalated based on culture results, when feasible [4,6,13]. The constellation of imaging findings in the present case, including the presence of an intramural, low-attenuation collection without extraluminal air on CT images and the absence of a leak and the double-lumen sign on contrast esophagogram, mirrors patterns highlighted in radiologic and emergency guidelines and reliably distinguishes intramural abscess from free perforation and intramural dissection [5,7,10]. In conclusion, esophageal abscess is a rare but potentially life-threatening complication of fish bone impaction. Early CT-based diagnosis and timely antibiotic therapy are critical for favorable outcomes.](https://mdpi-res.com/cdn-cgi/image/w=281,h=192/https://mdpi-res.com/biomed/biomed-06-00002/article_deploy/html/images/biomed-06-00002-g001-550.jpg)
![“Happy heart syndrome” is associated with a higher rate of the midventricular morphological variant of TTS than “broken heart syndrome”, as assessed by imaging modalities (i.e., echocardiography, cardiac computerized tomography/angiography, and cardiac magnetic resonance imaging); however, this literature finding is based on data from a limited number of patients with “happy heart syndrome”, and thus, this association needs confirmation by further experience. Figure. 1 is reproduced from [29], and reveals 5 different TTS morphological variants (a = apical; b = mid-ventricular; c = basal [aka reverse or inverse]; d = right ventricular in association with apical; e = focal) from left and right systolic ventriculographic images. Left ventricular ejection fraction (LVEF) of patients with the a, b, and c variant is similar, while patients with the e variant have a higher LVEF [30].](https://mdpi-res.com/cdn-cgi/image/w=281,h=192/https://mdpi-res.com/biomed/biomed-06-00001/article_deploy/html/images/biomed-06-00001-g001-550.jpg)