Manual Reduction for Subacute Osteoporotic Burst and Severe Compression Thoracolumbar Fractures
Abstract
:1. Introduction
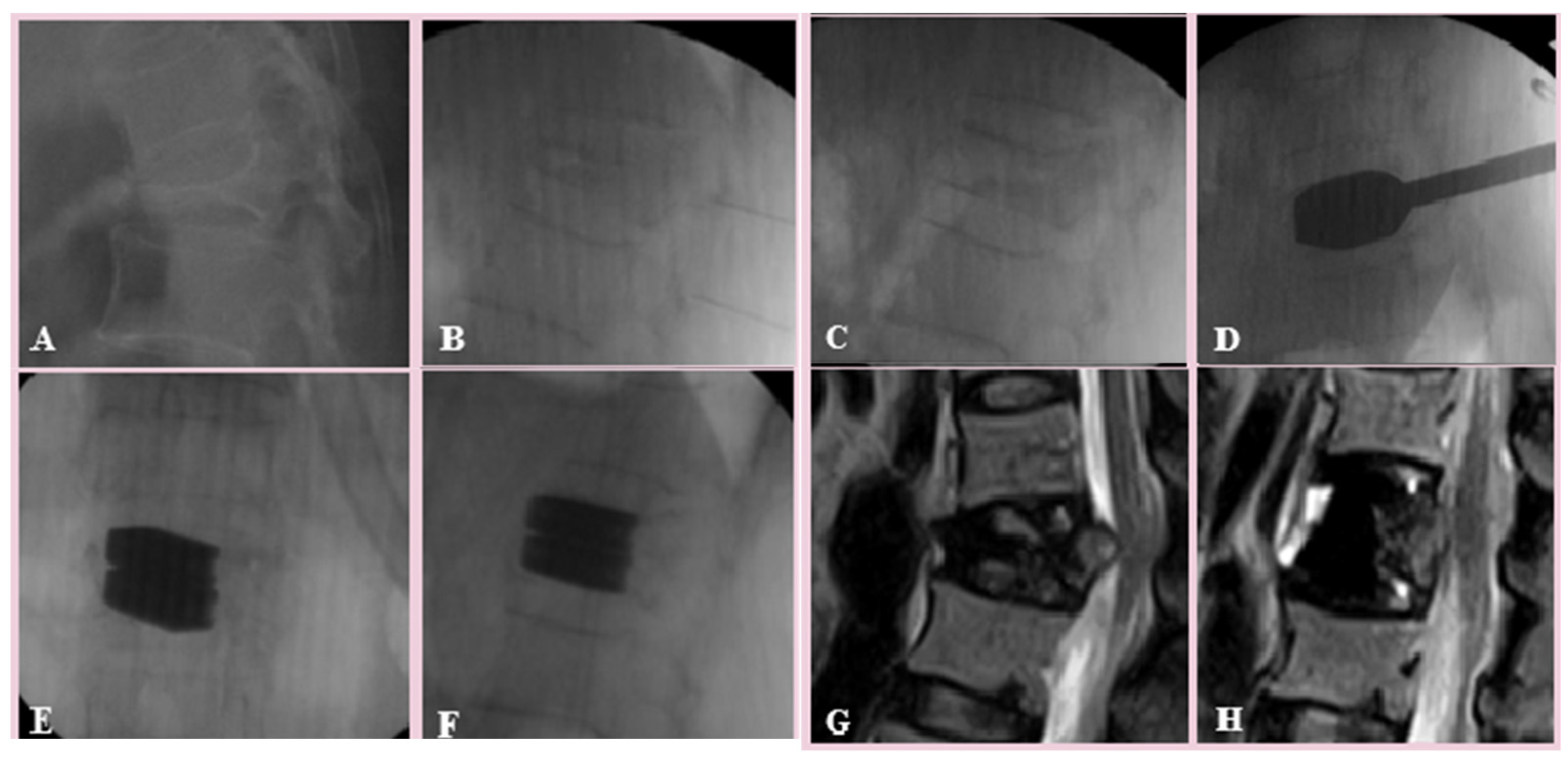
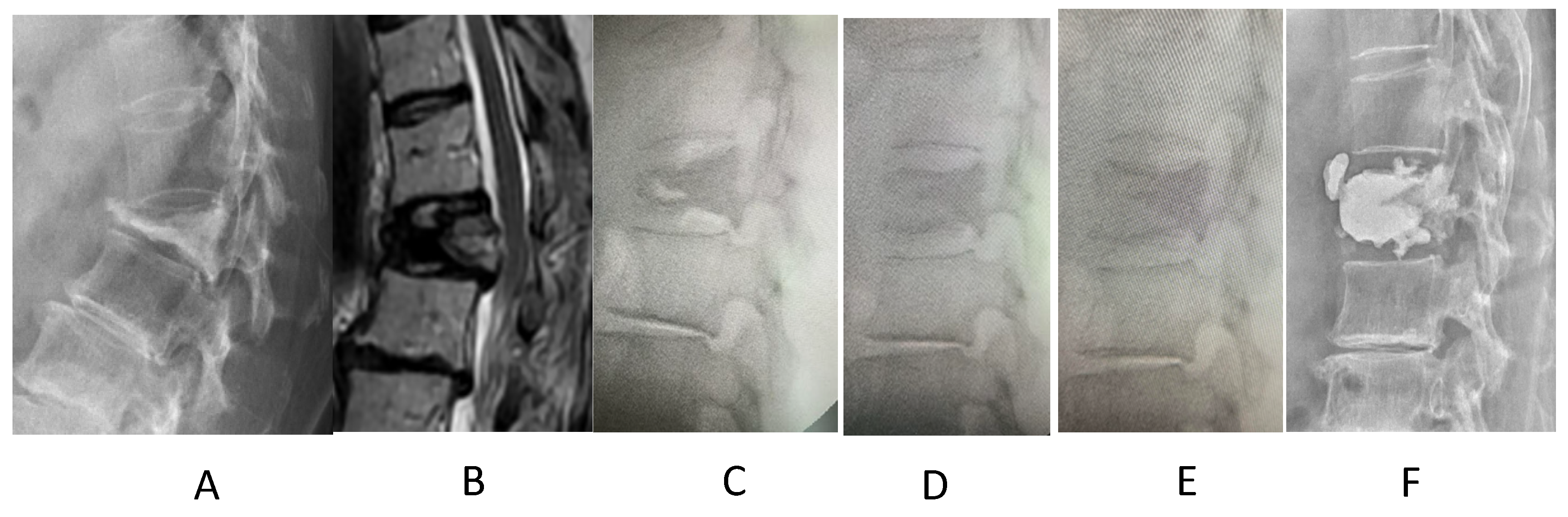
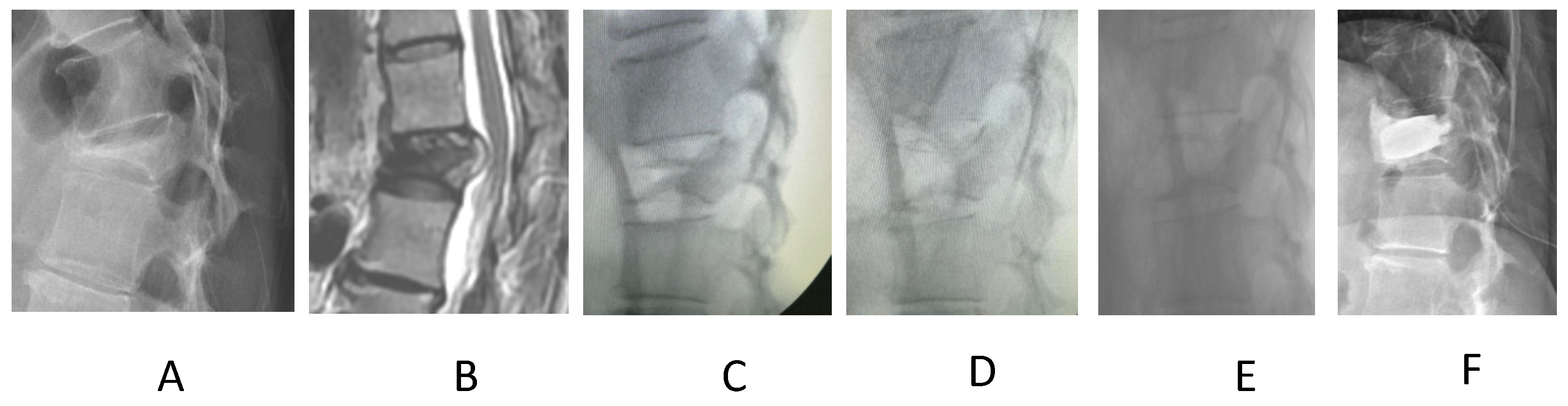
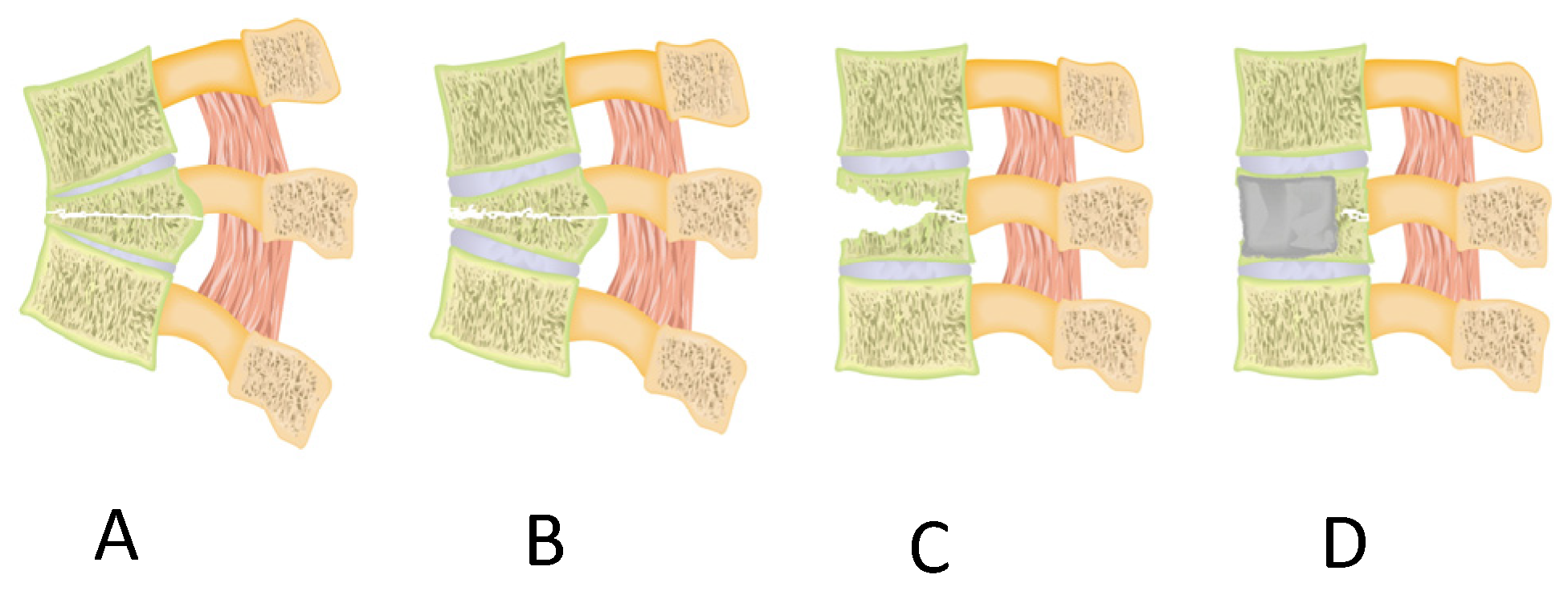
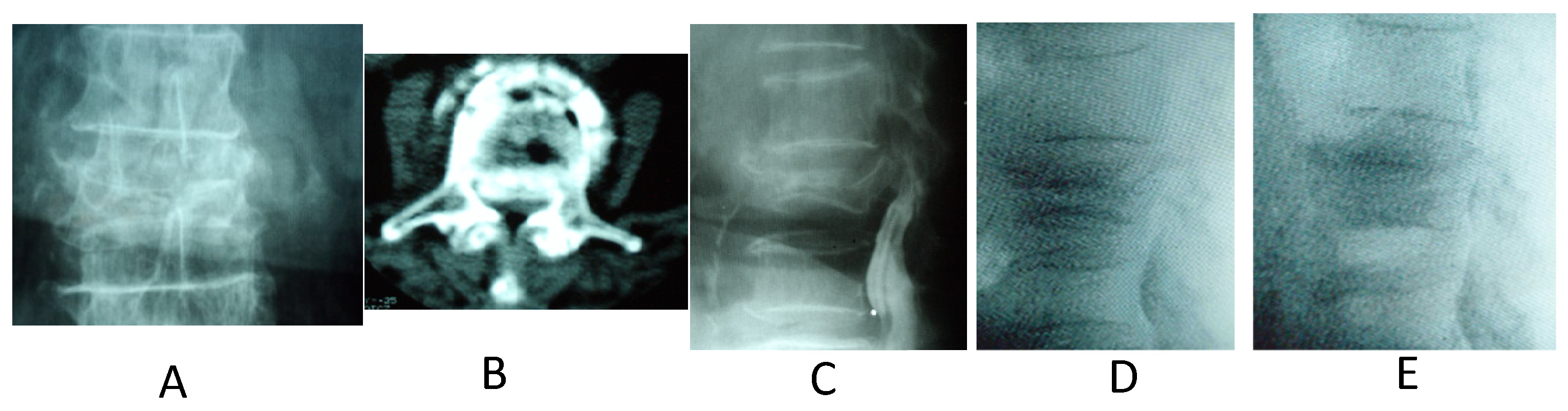
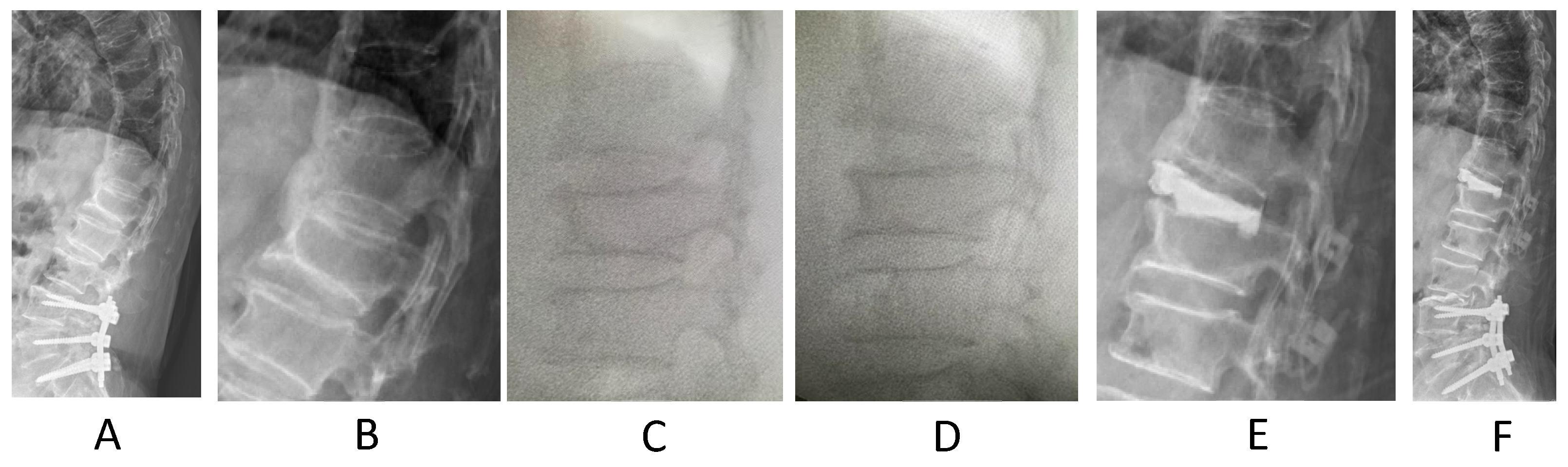
2. Materials and Methods
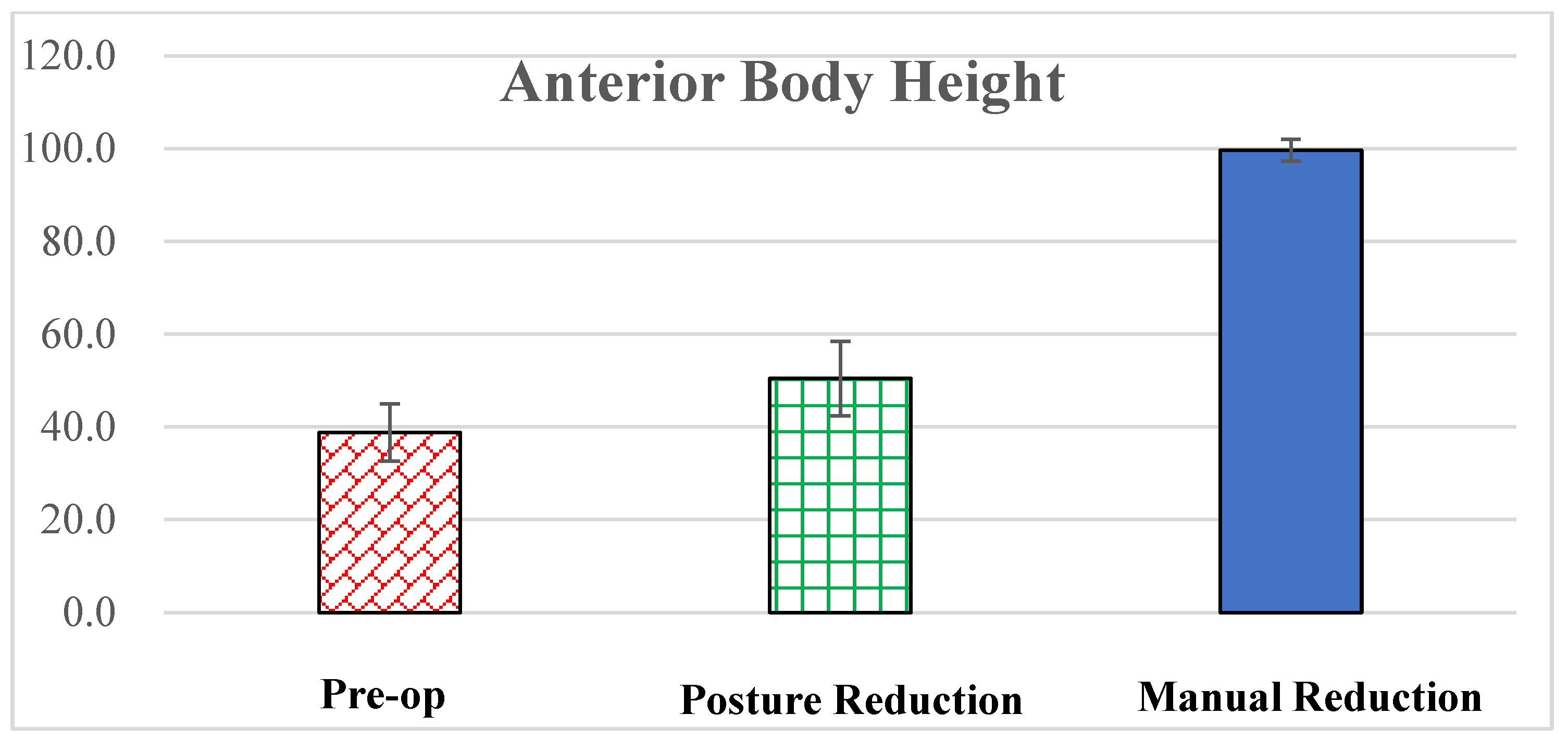
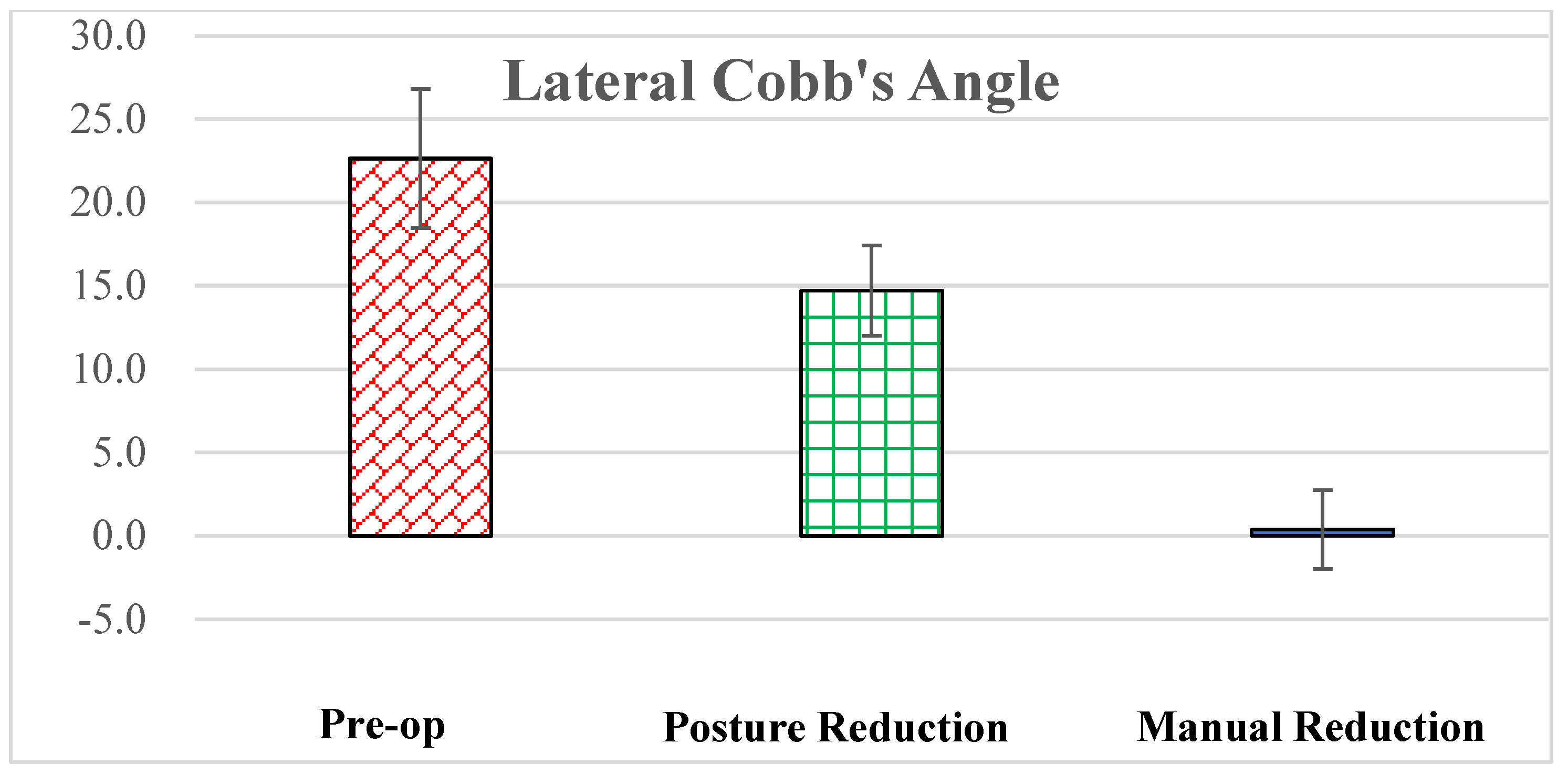
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Buchbinder, R.; Johnston, R.V.; Rischin, K.J.; Homik, J.; Jones, C.A.; Golmohammadi, K.; Kallmes, D.F. Percutaneous vertebroplasty for osteoporotic vertebral compression fracture. Cochrane Database Syst. Rev. 2018, 4, CD006349, Update in Cochrane Database Syst. Rev. 2018, 11, CD006349. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zuo, X.H.; Zhu, X.P.; Bao, H.G.; Xu, C.J.; Chen, H.; Gao, X.Z.; Zhang, Q.X. Network meta-analysis of percutaneous vertebroplasty, percutaneous kyphoplasty, nerve block, and conservative treatment for nonsurgery options of acute/subacute and chronic osteoporotic vertebral compression fractures (OVCFs) in short-term and long-term effects. Medicine 2018, 97, e11544. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fredrickson, B.; Edwards, W.; Rauschning, W.; Bayley, J.; Yuan, H. Volvo award in experimental studies vertebral burst fractures: An experimental, morphologic, and radiographic study. Spine 1992, 17, 1012–1021. [Google Scholar] [CrossRef] [PubMed]
- Fredrickson, B.E.; Mann, K.A.; Yuan, H.A.; Lubicky, J.P. Reduction of the intracanal fragment in experimental burst fractures. Spine 1988, 13, 267–271. [Google Scholar] [CrossRef] [PubMed]
- Frankel, H.L.; O Hancock, D.; Hyslop, G.; Melzak, J.; Michaelis, L.S.; Ungar, G.H.; Vernon, J.D.S.; Walsh, J.J. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. Spinal Cord. 1969, 7, 179–192. [Google Scholar] [CrossRef] [PubMed]
- Tropiano, P.; Huang, R.C.; Louis, C.A.; Poitout, D.G.; Louis, R.P. Functional and radiographic outcome of thoracolumbar and lumbar burst fractures managed by closed orthopaedic reduction and casting. Spine 2003, 28, 2459–2465. [Google Scholar] [CrossRef] [PubMed]
- Li, K.-C.; Hsieh, C.-H.; Lee, C.-Y.; Chen, T.-H. Transpedicle body augmenter: A further step in treating burst fractures. Clin. Orthop. Relat. Res. (1976–2007) 2005, 436, 119–125. [Google Scholar] [CrossRef]
- Li, K.-C.; Li, A.F.-Y.; Hsieh, C.-H.; Chen, H.-H. Transpedicle body augmenter in painfulo steoporotic compression fractures. Eur. Spine J. 2007, 16, 589–598. [Google Scholar] [CrossRef] [PubMed]
- Carlo, P.; Francesco, C. Preoperative manual on-table-traction for the reduction of thoracolumbar burst fractures: A technical note. J. Craniovertebral Junction Spine 2018, 9, 73. [Google Scholar] [CrossRef]
- Li, Y.; Du, Y.; Ji, A.; Wang, Q.; Li, L.; Wu, X.; Wang, P.; Chen, F. The clinical effect of manual reduction combined with internal fixation through Wiltse Paraspinal approach in the treatment of thoracolumbar fracture. Orthop. Surg. 2021, 13, 2206–2215. [Google Scholar] [CrossRef]
- Huang, J.; Zhou, L.; Yan, Z.; Zhou, Z.; Gou, X. Effect of manual reduction and indirect decompression on thoracolumbar burst fracture: A comparison study. J. Orthop. Surg. Res. 2020, 15, 532. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rousing, R.; Andersen, M.O.; Jespersen, S.M.; Thomsen, K.; Lauritsen, J. Percutaneous vertebroplasty compared to conservative treatment in patients with painful acute or subacute osteoporotic vertebral fractures: Three-months follow-up in a clinical randomized study. Spine 2009, 34, 1349–1354. [Google Scholar] [CrossRef] [PubMed]
- Li, K.C. IntechOpen: Manual Reduction, Subpedicle Approach, and Body Cage to Treat Burst Fracture. IntechOpen 2023. Available online: https://www.intechopen.com/profiles/518621 (accessed on 1 June 2023).
- Khan, M.R.; Mirdad, T.M. Ipsilateral dislocation of the shoulder and elbow. Saudi Med. J. 2001, 22, 1019–1021. [Google Scholar] [PubMed]
- Bohlman, H.H.; Ducker, T.B. Spine and Spine Cord Injuries. In Rothman-Simeone the Spine, 4th ed.; Herkowitz, H.N., Garfin, S.R., Balderston, R.A., Eismont, F.J., Bell, G.R., Eds.; WB Saunders Company: Philadelphia, PA, USA, 1999; Volume 2, pp. 889–1002. [Google Scholar]
- Harrington, R.; Budorick, T.; Hoyt, J.; Anderson, P.; Tencer, A. Biomechanics of indirect reduction of bone retropulsed into the spinal canal in vertebral fracture. Spine 1993, 18, 692–699. [Google Scholar] [CrossRef]
- Lin, R.M.; Panjabi, M.M.; Oxland, T.R. Functional radiographs of acute thoracolumbar burst fractures: A biomechanical study. Spine 1993, 18, 2431–2437. [Google Scholar] [CrossRef] [PubMed]
- Mumford, J.; Weinstein, J.N.; Spratt, K.F.; Goel, V.K. Thoracolumbar burst fractures: The clinical efficacy and outcome of nonoperative management. Spine 1993, 18, 955–970. [Google Scholar] [CrossRef] [PubMed]
- Deramond, H.; Depriester, C.; Galibert, P.; Le Gars, D. Percutaneous vertebroplasty with polymethylmethacrylate: Technique, indications, and results. Radiol. Clin. N. Am. 1998, 36, 533–546. [Google Scholar] [CrossRef] [PubMed]
- Lindsey, R.W.; Dick, W. The fixateur interne in the reduction and stabilization of thoracolumbar spine fractures in patients with neurologic deficit. Spine 1991, 16 (Suppl. S3), S140–S145. [Google Scholar] [CrossRef]
- Duan, Y.; Feng, D.; Chen, J.; Wu, Y.; Li, T.; Jiang, L.; Huang, Y. Anterior, Posterior and Anterior-Posterior Approaches for the Treatment of Thoracolumbar Burst Fractures: A Network Meta-Analysis of Randomized Controlled Trials. J. Investig. Surg. 2024, 37, 2301794. [Google Scholar] [CrossRef] [PubMed]
- Li, K.-C.; Li, A.F.; Hsieh, C.-H.; Liao, T.-H.; Chen, C.-H. Another option to treat Kümmell’s disease with cord compression. Eur. Spine J. 2007, 16, 1479–1487. [Google Scholar] [CrossRef]
- Van Eenenaam, D.P.; Georges, Y. Delayed post-traumatic vertebral collapse (Kummell’s disease): Case report with serial radiographs, computed tomographic scans, and bone scans. Spine 1993, 18, 1236–1241. [Google Scholar] [CrossRef] [PubMed]
- Golimbu, C.; Firooznia, H.; Rafii, M. The intravertebral vacuum sign. Spine 1986, 11, 1040–1043. [Google Scholar] [CrossRef] [PubMed]
- Osterhouse, M.D.; Kettner, N.W. Delayed posttraumatic vertebral collapse with intravertebral vacuum cleft. J. Manip. Physiol. Ther. 2002, 25, 270–275. [Google Scholar] [CrossRef] [PubMed]
- Garfin, S.R.; Yuan, H.A.; Reiley, M.A. New technologies in spine: Kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine 2001, 26, 1511–1515. [Google Scholar] [CrossRef] [PubMed]
- Hiwatashi, A.; Moritani, T.; Numaguchi, Y.; Westesson, P.-L. Increase in vertebral body height after vertebroplasty. Am. J. Neuroradiol. 2003, 24, 185–189. [Google Scholar] [PubMed]
- McKiernan, F.; Jensen, R.; Faciszewski, T. The dynamic mobility of vertebral compression fractures. J. Bone Miner. Res. 2003, 18, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Fukuta, S.; Miyamoto, K.; Masuda, T.; Hosoe, H.; Kodama, H.; Nishimoto, H.; Sakaeda, H.; Shimizu, K. Two-stage (posterior and anterior) surgical treatment using posterior spinal instrumentation for pyogenic and tuberculotic spondylitis. Spine 2003, 28, E302–E308. [Google Scholar] [CrossRef]
- Perrin, R.G.; McBroom, R.J. Spinal fixation after anterior decompression for symptomatic spinal metastasis. Neurosurgery 1988, 22, 324–327. [Google Scholar] [CrossRef]
- Walker, M.P.; Yaszemski, M.J.; Kim, C.W.; Talac, R.; Currier, B.L. Metastatic disease of the spine: Evaluation and treatment. Clin. Orthop. Relat. Res. (1976–2007) 2003, 415, S165–S175. [Google Scholar] [CrossRef]
- Sieradzki, J.P.; Sarwark, J.F. Thoracolumbar fracture-dislocation in child abuse: Case report, closed reduction technique and review of the literature. Pediatr. Neurosurg. 2008, 44, 253–257. [Google Scholar] [CrossRef]
- Li, K.-C.; Hsieh, C.-H.; Liao, T.-H. Clinical outcome-supported advance of cement lumber interbody fusion for degenerative lumbar scoliosis. J. Surg. 2023, 8, 1697. [Google Scholar] [CrossRef]



| Items | Data |
|---|---|
| Gender | 73 females |
| 28 males | |
| (Total: 101) | |
| Age | 77.4 ± 8.5 |
| (61 to 94) | |
| DEXA | 3.2 ± 4.5 |
| (2.9 to 4.2) | |
| Injury mechanism | Fall: 54 cases |
| RTA: 13 cases | |
| Minor trauma 1: 34 cases | |
| Fracture level | T10: 5 |
| T11: 19 | |
| T12: 29 | |
| L1: 31 | |
| L2: 17 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, K.-C.; Hsieh, C.-H.; Liao, T.-H.; Chen, C.-H. Manual Reduction for Subacute Osteoporotic Burst and Severe Compression Thoracolumbar Fractures. BioMed 2024, 4, 136-145. https://doi.org/10.3390/biomed4020011
Li K-C, Hsieh C-H, Liao T-H, Chen C-H. Manual Reduction for Subacute Osteoporotic Burst and Severe Compression Thoracolumbar Fractures. BioMed. 2024; 4(2):136-145. https://doi.org/10.3390/biomed4020011
Chicago/Turabian StyleLi, Kung-Chia, Ching-Hsiang Hsieh, Ting-Hua Liao, and Chih-Hung Chen. 2024. "Manual Reduction for Subacute Osteoporotic Burst and Severe Compression Thoracolumbar Fractures" BioMed 4, no. 2: 136-145. https://doi.org/10.3390/biomed4020011







