Indoor Airborne Microplastics: Human Health Importance and Effects of Air Filtration and Turbulence
Abstract
:1. Aims and Identification of Relevant Literature
2. Introduction
3. Influence of Air Turbulence on Airborne Microplastic Load: Fans and Vacuum Cleaners
4. Domestic Air Filters
4.1. Air Conditioners (ACs)
4.2. Air Purifiers
Plants as Purifiers of Polluted Air (Phytoremediation)
5. Airborne Microplastics as Disseminators of Microorganisms and Disease
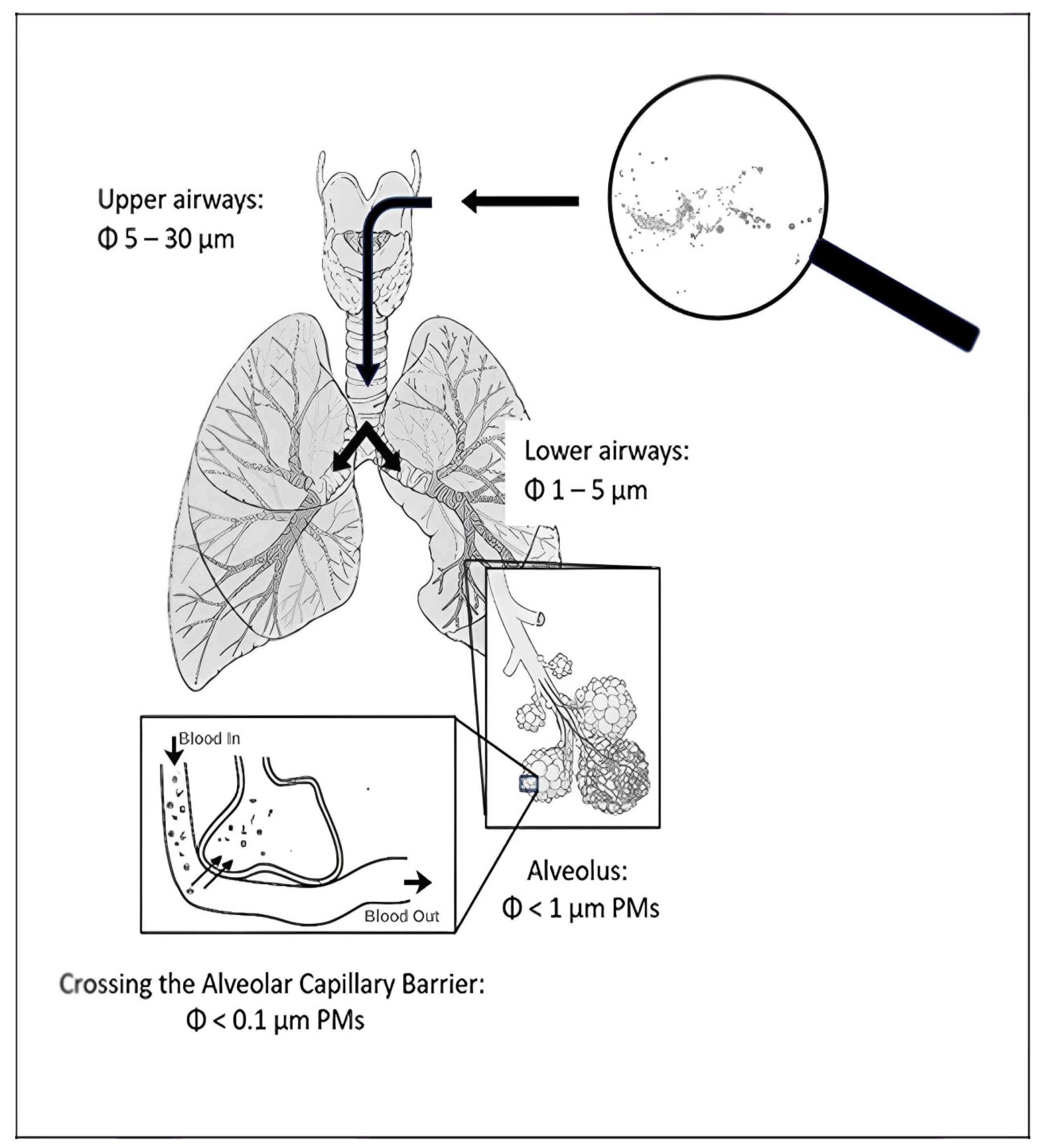
5.1. The Health Impacts of Microplastics in the Air
5.2. Aerial Chemical Pollutants and Microplastics
5.2.1. Inorganic Pollutants
5.2.2. Organic Pollutants
5.2.3. Controversy
6. Conclusions and Perspectives
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Zhao, X.; Zhou, Y.; Liang, C.; Song, J.; Yu, S.; Liao, G.; Zou, P.; Tang, K.H.D.; Wu, C. Airborne microplastics: Occurrence, sources, fate, risks and mitigation. Sci. Total Environ. 2023, 858, 159943. [Google Scholar] [CrossRef] [PubMed]
- Chandrakanthan, K.; Fraser, M.P.; Herckes, P. Airborne microplastics in a suburban location in the desert southwest: Occurrence and identification challenges. Atmos. Environ. 2023, 298, 119617. [Google Scholar] [CrossRef]
- Zhang, K.; Wu, C. Formation of Airborne Microplastics. In Comprehensive Analytical Chemistry; Elsevier: Amsterdam, The Netherlands, 2023; Volume 100, pp. 1–16. [Google Scholar] [CrossRef]
- Alimba, C.G.; Faggio, C. Microplastics in the marine environment: Current trends in environmental pollution and mechanisms of toxicological profile. Environ. Toxicol. Pharmacol. 2019, 68, 61–74. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Shan, E.; Zhao, J.; Teng, J.; Wang, Q. The factors influencing the vertical transport of microplastics in marine environment: A review. Sci. Total Environ. 2023, 870, 161893. [Google Scholar] [CrossRef] [PubMed]
- Nakano, H.; Alfonso, M.B.; Jandang, S.; Imai, K.; Arakawa, H. Microplastic pollution indexes in the coastal and open ocean areas around Japan. Region Stud. Mar. Sci. 2024, 69, 103287. [Google Scholar] [CrossRef]
- Yuan, W.; Liu, X.; Wang, W.; Di, M.; Wang, J. Microplastic abundance, distribution and composition in water, sediments, and wild fish from Poyang Lake, China. Ecotoxicol. Environ. Saf. 2019, 170, 180–187. [Google Scholar] [CrossRef]
- Gong, J.; Xie, P. Research progress in sources, analytical methods, eco-environmental effects, and control measures of microplastics. Chemosphere 2020, 254, 126790. [Google Scholar] [CrossRef]
- Ricciardi, M.; Pironti, C.; Motta, O.; Miele, Y.; Proto, A.; Montano, L. Correction: Ricciardi et al. Microplastics in the Aquatic Environment: Occurrence, Persistence, Analysis, and Human Exposure. Water 2023, 15, 1718. [Google Scholar] [CrossRef]
- Torres, S.; Compa, M.; Box, A.; Pinya, S.; Sureda, A. Presence and Potential Effects of Microplastics in the Digestive Tract of Two Small Species of Shark from the Balearic Islands. Fishes 2024, 9, 55. [Google Scholar] [CrossRef]
- Cox, K.D.; Covernton, G.A.; Davies, H.L.; Dower, J.F.; Juanes, F.; Dudas, S.E. Human consumption of microplastics. Environ. Sci. Technol. 2019, 53, 7068–7074. [Google Scholar] [CrossRef]
- Neves, C.V.; Gaylarde, C.C.; Neto, J.A.B.; Vieira, K.S.; Pierri, B.; Waite, C.C.; Scott, D.C.; da Fonseca, E.M. The transfer and resulting negative effects of nano-and micro-plastics through the aquatic trophic web—A discreet threat to human health. Water Biol. Secur. 2022, 1, 100080. [Google Scholar] [CrossRef]
- Ziani, K.; Ioniță-Mîndrican, C.-B.; Mititelu, M.; Neacșu, S.M.; Negrei, C.; Moroșan, E.; Drăgănescu, D.; Preda, O.-T. Microplastics: A real global threat for environment and food safety: A state of the art review. Nutrients 2023, 15, 617. [Google Scholar] [CrossRef]
- Kadac-Czapska, K.; Knez, E.; Grembecka, M. Food and human safety: The impact of microplastics. Crit. Rev. Food Sci. Nutr. 2024, 64, 3502–3521. [Google Scholar] [CrossRef]
- Catarino, A.I.; Macchia, V.; Sanderson, W.G.; Thompson, R.C.; Henry, T.B. Low levels of microplastics (MP) in wild mussels indicate that MP ingestion by humans is minimal compared to exposure via household fibres fallout during a meal. Environ. Poll. 2018, 237, 675–684. [Google Scholar] [CrossRef]
- Zhao, X.; You, F. Microplastic human dietary uptake from 1990 to 2018 grew across 109 major developing and industrialized countries but can be halved by plastic debris removal. Environ. Sci. Technol. 2024, 58, 8709–8723. [Google Scholar] [CrossRef]
- Zhang, Q.; Xu, E.G.; Li, J.; Chen, Q.; Ma, L.; Zeng, E.Y.; Shi, H. A review of microplastics in table salt, drinking water, and air: Direct human exposure. Environ. Sci. Technol. 2020, 54, 3740–3751. [Google Scholar] [CrossRef]
- Vianello, A.; Jensen, R.L.; Liu, L.; Vollertsen, J. Simulating human exposure to indoor airborne microplastics using a Breathing Thermal Manikin. Sci. Rep. 2019, 9, 8670. [Google Scholar] [CrossRef]
- Prata, J.C. Microplastics and human health: Integrating pharmacokinetics. Crit. Rev. Environ. Sci. Technol. 2023, 53, 1489–1511. [Google Scholar] [CrossRef]
- Ageel, H.K.; Harrad, S.; Abdallah, M.A.E. Occurrence, human exposure, and risk of microplastics in the indoor environment. Environ. Sci. Proc. Imp. 2022, 24, 17–31. [Google Scholar] [CrossRef]
- Farrow, A.; Taylor, H.; Golding, J. Time spent in the home by different family members. Environ. Technol. 1997, 18, 605–613. [Google Scholar] [CrossRef]
- Levy, J.I. Impact of residential nitrogen dioxide exposure on personal exposure: An international study. J. Air Waste Manag. Ass. 1998, 48, 553–560. [Google Scholar] [CrossRef]
- Jenner, L.C.; Sadofsky, L.R.; Danopoulos, E.; Rotchell, J.M. Household indoor microplastics within the Humber region (United Kingdom): Quantification and chemical characterisation of particles present. Atmos. Environ. 2021, 259, 118512. [Google Scholar] [CrossRef]
- Liao, Z.; Ji, X.; Ma, Y.; Lv, B.; Huang, W.; Zhu, X.; Fang, M.; Wang, Q.; Wang, X.; Dahlgren, R.; et al. Airborne microplastics in indoor and outdoor environments of a coastal city in Eastern China. J. Hazard. Mater. 2021, 417, 126007. [Google Scholar] [CrossRef]
- Kacprzak, S.; Tijing, L.D. Microplastics in indoor environment: Sources, mitigation and fate. J. Environ. Chem. Eng. 2022, 10, 107359. [Google Scholar] [CrossRef]
- O’Brien, S.; Rauert, C.; Ribeiro, F.; Okoffo, E.D.; Burrows, S.D.; O’Brien, J.W.; Wang, X.; Wright, S.L.; Thomas, K.V. There’s something in the air: A review of sources, prevalence and behaviour of microplastics in the atmosphere. Sci. Total Environ. 2023, 874, 162193. [Google Scholar] [CrossRef]
- Perera, K.; Ziajahromi, S.; Nash, S.B.; Leusch, F.D. Microplastics in Australian indoor air: Abundance, characteristics, and implications for human exposure. Sci. Total Environ. 2023, 889, 164292. [Google Scholar] [CrossRef]
- Yang, S.; Bekö, G.; Wargocki, P.; Williams, J.; Licina, D. Human emissions of size-resolved fluorescent aerosol particles: Influence of personal and environmental factors. Environ. Sci. Technol. 2020, 55, 509–518. [Google Scholar] [CrossRef]
- Finkel, D.; Ernsth Bravell, M.; Pedersen, N.L. Role of motor function and lung function in pathways to ageing and decline. Aging Clin. Exp. Res. 2020, 32, 2479–2487. [Google Scholar] [CrossRef]
- Gaston, E.; Woo, M.; Steele, C.; Sukumaran, S.; Anderson, S. Microplastics differ between indoor and outdoor air masses: Insights from multiple microscopy methodologies. Appl. Spectrosc. 2020, 74, 1079–1098. [Google Scholar] [CrossRef]
- Perera, K.; Ziajahromi, S.; Bengtson Nash, S.; Manage, P.M.; Leusch, F.D. Airborne microplastics in indoor and outdoor environments of a developing country in south asia: Abundance, distribution, morphology, and possible sources. Environ. Sci. Technol. 2022, 56, 16676–16685. [Google Scholar] [CrossRef]
- Ouyang, Z.; Mao, R.; Hu, E.; Xiao, C.; Yang, C.; Guo, X. The indoor exposure of microplastics in different environments. Gondwana Res. 2022, 108, 193–199. [Google Scholar] [CrossRef]
- Zhu, J.; Zhang, X.; Liao, K.; Wu, P.; Jin, H. Microplastics in dust from different indoor environments. Sci. Total Environ. 2022, 833, 155256. [Google Scholar] [CrossRef]
- Torres-Agullo, A.; Karanasiou, A.; Moreno, T.; Lacorte, S. Airborne microplastic particle concentrations and characterization in indoor urban microenvironments. Environ. Poll. 2022, 308, 119707. [Google Scholar] [CrossRef]
- Dris, R.; Gasperi, J.; Mirande, C.; Mandin, C.; Guerrouache, M.; Langlois, V.; Tassin, B. A first overview of textile fibers, including microplastics, in indoor and outdoor environments. Environ. Poll. 2017, 221, 453–458. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Wang, L.; Kannan, K. Microplastics in house dust from 12 countries and associated human exposure. Environ. Int. 2020, 134, 105314. [Google Scholar] [CrossRef]
- Yang, H.; He, Y.; Yan, Y.; Junaid, M.; Wang, J. Characteristics, toxic effects, and analytical methods of microplastics in the atmosphere. Nanomaterials 2021, 11, 2747. [Google Scholar] [CrossRef]
- Peng, C.; Zhang, X.; Li, M.; Lu, Y.; Liu, C.; Wang, L. Source apportionment of microplastics in indoor dust: Two strategies based on shape and composition. Environ. Poll. 2023, 334, 122178. [Google Scholar] [CrossRef]
- O’Brien, S.; Okoffo, E.D.; O’Brien, J.W.; Ribeiro, F.; Wang, X.; Wright, S.L.; Samanipour, S.; Rauert, C.; Toapanta, T.Y.A.; Albarracin, R.; et al. Airborne emissions of microplastic fibres from domestic laundry dryers. Sci. Total Environ. 2020, 747, 141175. [Google Scholar] [CrossRef]
- Gaylarde, C.; Baptista-Neto, J.A.; da Fonseca, E.M. Plastic microfibre pollution: How important is clothes’ laundering? Heliyon 2021, 7, e07105. [Google Scholar] [CrossRef]
- Tiffin, L.; Hazlehurst, A.; Sumner, M.; Taylor, M. Reliable quantification of microplastic release from the domestic laundry of textile fabrics. J. Textile Inst. 2022, 113, 558–566. [Google Scholar] [CrossRef]
- Periyasamy, A.P. Environmentally friendly approach to the reduction of microplastics during domestic washing: Prospects for machine vision in microplastics reduction. Toxics 2023, 11, 575. [Google Scholar] [CrossRef]
- Wang, C.; Chen, W.; Zhao, H.; Tang, J.; Li, G.; Zhou, Q.; Sun, J.; Xing, B. Microplastic fiber release by laundry: A comparative study of hand-washing and machine-washing. ACS ES&T Water 2023, 3, 147–155. [Google Scholar] [CrossRef]
- Lim, E.; Tanaka, H.; Ni, Y.; Bai, Y.; Ito, K. Microplastics/microfibers in settled indoor house dust—Exploratory case study for 10 residential houses in the Kanto area of Japan. Jpn. Archit. Rev. 2022, 5, 682–690. [Google Scholar] [CrossRef]
- Nematollahi, M.J.; Zarei, F.; Keshavarzi, B.; Zarei, M.; Moore, F.; Busquets, R.; Kelly, F.J. Microplastic occurrence in settled indoor dust in schools. Sci. Total Environ. 2022, 807, 150984. [Google Scholar] [CrossRef]
- Amato-Lourenço, L.F.; dos Santos Galvão, L.; Wiebeck, H.; Carvalho-Oliveira, R.; Mauad, T. Atmospheric microplastic fallout in outdoor and indoor environments in São Paulo megacity. Sci. Total Environ. 2022, 821, 153450. [Google Scholar] [CrossRef]
- Valdiviezo-Gonzales, L.; Ojeda, P.O.; Morriberón, D.E.; Colombo, C.V.; Rimondino, G.N.; López, A.D.F.; Severini, M.D.F.; Malanca, F.E.; De-la-Torre, G.E. Influence of the geographic location and house characteristics on the concentration of microplastics in indoor dust. Sci. Total Environ. 2024, 917, 170353. [Google Scholar] [CrossRef]
- Suaria, G.; Achtypi, A.; Perold, V.; Lee, J.R.; Pierucci, A.; Bornman, T.G.; Aliani, S.; Ryan, P.G. Microfibers in oceanic surface waters: A global characterization. Sci. Adv. 2020, 6, eaay8493. [Google Scholar] [CrossRef]
- Zhu, X.; Huang, W.; Fang, M.; Liao, Z.; Wang, Y.; Xu, L.; Mu, Q.; Shi, C.; Lu, C.; Deng, H.; et al. Airborne microplastic concentrations in five megacities of northern and southeast China. Environ. Sci. Technol. 2021, 55, 12871–12881. [Google Scholar] [CrossRef]
- Liu, K.; Wang, X.; Fang, T.; Xu, P.; Zhu, L.; Li, D. Source and potential risk assessment of suspended atmospheric microplastics in Shanghai. Sci. Total Environ. 2019, 675, 462–471. [Google Scholar] [CrossRef]
- Xie, Y.; Li, Y.; Feng, Y.; Cheng, W.; Wang, Y. Inhalable microplastics prevails in air: Exploring the size detection limit. Environ. Int. 2022, 162, 107151. [Google Scholar] [CrossRef]
- Jahandari, A. Microplastics in the urban atmosphere: Sources, occurrences, distribution, and potential health implications. J. Hazard. Mat. Adv. 2023, 12, 100346. [Google Scholar] [CrossRef]
- Kim, J.J.; Hann, T.; Lee, S.J. Effect of flow and humidity on indoor deposition of particulate matter. Environ. Pollut. 2019, 255, 113263. [Google Scholar] [CrossRef]
- Boakes, L.C.; Patmore, I.R.; Bancone, C.E.; Rose, N.L. High temporal resolution records of outdoor and indoor airborne microplastics. Environ. Sci. Poll. Res. 2023, 30, 39246–39257. [Google Scholar] [CrossRef]
- Zhai, X.; Zheng, H.; Xu, Y.; Zhao, R.; Wang, W.; Guo, H. Characterization and quantification of microplastics in indoor environments. Heliyon 2023, 9, e15901. [Google Scholar] [CrossRef]
- Kim, J.J.; Kim, H.; Kim, J.; Lee, I.; Kim, H.; Lee, S.J. Effect of the flow structure on the indoor deposition of particulate matter. J. Vis. 2022, 25, 741–750. [Google Scholar] [CrossRef]
- Prata, J.C. Airborne microplastics: Consequences to human health? Environ. Poll. 2018, 234, 115–126. [Google Scholar] [CrossRef]
- Lewis, R.D.; Ong, K.H.; Emo, B.; Kennedy, J.; Kesavan, J.; Elliot, M. Resuspension of house dust and allergens during walking and vacuum cleaning. J. Occup. Environ. Hyg. 2018, 15, 235–245. [Google Scholar] [CrossRef]
- Wang, B.; Tang, Z.; Li, Y.; Cai, N.; Hu, X. Experiments and simulations of human walking-induced particulate matter resuspension in indoor environments. J. Clean. Prod. 2021, 295, 126488. [Google Scholar] [CrossRef]
- Soltani, N.S.; Taylor, M.P.; Wilson, S.P. Quantification and exposure assessment of microplastics in Australian indoor house dust. Environ. Poll. 2021, 283, 117064. [Google Scholar] [CrossRef]
- Soltani, N.S.; Taylor, M.P.; Wilson, S.P. International quantification of microplastics in indoor dust: Prevalence, exposure and risk assessment. Environ. Poll. 2022, 312, 119957. [Google Scholar] [CrossRef]
- Wu, C.; Chao, C.Y.H.; Wan, M.; Chan, T.C. Ultrafine Particle Resuspension During Vacuum Cleaning in a Household Environment. In Proceedings of the 10th International Conference of Healthy Buildings, Brisbane, Australia, 8–12 July 2012; p. 1002. Available online: https://repository.hkust.edu.hk/ir/bitstream/1783.1-56151/1/611310-ConfP-3-fulltext-pre.pdf (accessed on 22 May 2024).
- Vicente, E.D.; Vicente, A.M.; Evtyugina, M.; Calvo, A.I.; Oduber, F.; Alegre, C.B.; Castro, A.; Fraile, R.; Nunes, T.; Lucarelli, F.; et al. Impact of vacuum cleaning on indoor air quality. Build. Environ. 2020, 180, 107059. [Google Scholar] [CrossRef]
- Besis, A.; Katsoyiannis, A.; Botsaropoulou, E.; Samara, C. Concentrations of polybrominated diphenyl ethers (PBDEs) in central air-conditioner filter dust and relevance of non-dietary exposure in occupational indoor environments in Greece. Environ. Pollut. 2014, 188, 64–70. [Google Scholar] [CrossRef]
- Abad-López, A.P.; Orozco-Pérez, K.K.; Arana, V.A.; Grande-Tovar, C.D. Microplastics suspended in dust from different indoor environments in Barranquilla, Colombia: Predominant microparticles? Environ. Pollut. 2024, 350, 124023. [Google Scholar] [CrossRef]
- Fang, C.; Awoyemi, O.S.; Saianand, G.; Xu, L.; Niu, J.; Naidu, R. Characterising microplastics in indoor air: Insights from Raman imaging analysis of air filter samples. J. Hazard. Mater. 2024, 464, 132969. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, S.; Hu, J.; Wu, B.; Huang, C.; He, C.; Zheng, Z.; Gao, P. Bioaccessibility of polycyclic aromatic hydrocarbons in central air conditioner filter dust and its occupational exposure to shopping mall employees. Environ. Pollut. 2019, 246, 896–903. [Google Scholar] [CrossRef]
- Winiarska, E.; Jutel, M.; Zemelka-Wiacek, M. The potential impact of nano-and microplastics on human health: Understanding human health risks. Environ. Res. 2024, 251, 118535. [Google Scholar] [CrossRef]
- Vonberg, R.-P.; Gastmeier, P.; Kenneweg, B.; Holdack-Janssen, H.; Sohr, D.; Chaberny, I.F. The microbiological quality of air improves when using air conditioning systems in cars. BMC Infect. Dis. 2010, 10, 146. [Google Scholar] [CrossRef]
- Chen, Y.; Li, X.; Zhang, X.; Zhang, Y.; Gao, W.; Wang, R.; He, D. Air conditioner filters become sinks and sources of indoor microplastics fibers. Environ. Poll. 2022, 292, 118465. [Google Scholar] [CrossRef]
- Watanabe, K.; Yanagi, U.; Shiraishi, Y.; Harada, K.; Ogino, F.; Asano, K. Bacterial communities in various parts of air-conditioning units in 17 Japanese houses. Microorganisms 2022, 10, 2246. [Google Scholar] [CrossRef]
- Argyropoulos, C.D.; Skoulou, V.; Efthimiou, G.; Michopoulos, A.K. Airborne transmission of biological agents within the indoor built environment: A multidisciplinary review. Air Qual. Atmos. Health 2023, 16, 477–533. [Google Scholar] [CrossRef]
- Shiraishi, Y.; Harada, K.; Maeda, C.; Ogino, F.; Suzuki, Y.; Okada, N.; Tomomatsu, K.; Sekine, Y.; Yanagi, U.; Imanishi, T.; et al. A method to evaluate and eliminate fungal contamination in household air conditioners. Indoor Air 2023, 2023, 8984619. [Google Scholar] [CrossRef]
- Boccia, P.; Mondellini, S.; Mauro, S.; Zanellato, M.; Parolini, M.; Sturchio, E. Potential effects of environmental and occupational exposure to microplastics: An overview of air contamination. Toxics 2024, 12, 320. [Google Scholar] [CrossRef] [PubMed]
- Burridge, H.C.; Liu, S.; Mohamed, S.; Wood, S.G.; Noakes, C.J. The CHEPA model: Assessing the impact of HEPA filter units in classrooms using a fast-running coupled indoor air quality and dynamic thermal model. arXiv 2024, arXiv:2404.10837. [Google Scholar] [CrossRef]
- Forgione, G.; Izzo, F.; Mercurio, M.; Cicchella, D.; Dini, L.; Giancane, G.; Paolucci, M. Microplastics pollution in freshwater fishes in the South of Italy: Characterization, distribution, and correlation with environmental pollutants. Sci. Total Environ. 2023, 864, 161032. [Google Scholar] [CrossRef]
- Klein, M.; Bechtel, B.; Brecht, T.; Fischer, E.K. Spatial distribution of atmospheric microplastics in bulk-deposition of urban and rural environments–A one-year follow-up study in northern Germany. Sci. Total Environ. 2023, 901, 165923. [Google Scholar] [CrossRef]
- Cai, J.; Yu, W.; Li, B.; Yao, R.; Zhang, T.; Guo, M.; Wang, H.; Cheng, Z.; Xiong, J.; Meng, Q.; et al. Particle removal efficiency of a household portable air cleaner in real-world residences: A single-blind cross-over field study. Energy Build. 2019, 203, 109464. [Google Scholar] [CrossRef]
- Chen, R.; Zhao, A.; Chen, H.; Zhao, Z.; Cai, J.; Wang, C.; Yang, C.; Li, H.; Xu, X.; Ha, S.; et al. Cardiopulmonary benefits of reducing indoor particles of outdoor origin: A randomized, double-blind crossover trial of air purifiers. J. Amer Coll. Cardiol. 2015, 65, 2279–2287. [Google Scholar] [CrossRef]
- Lee, W.C.; Catalano, P.J.; Yoo, J.Y.; Park, C.J.; Koutrakis, P. Validation and application of the mass balance model to determine the effectiveness of portable air purifiers in removing ultrafine and submicrometer particles in an apartment. Environ. Sci. Technol. 2015, 49, 9592–9599. [Google Scholar] [CrossRef]
- Sundbæk, K.B.; Koch, I.D.W.; Villaro, C.G.; Rasmussen, N.S.; Holdt, S.L.; Hartmann, N.B. Sorption of fluorescent polystyrene microplastic particles to edible seaweed Fucus vesiculosus. J. Appl. Phycol. 2018, 30, 2923–2927. [Google Scholar] [CrossRef]
- Masiá, P.; Sol, D.; Ardura, A.; Laca, A.; Borrell, Y.J.; Dopico, E.; Laca, A.; Machado-Schiaffino, G.; Díaz, M.; Garcia-Vazquez, E. Bioremediation as a promising strategy for microplastics removal in wastewater treatment plants. Mar. Poll. Bull. 2020, 156, 111252. [Google Scholar] [CrossRef]
- Rozman, U.; Kokalj, A.J.; Dolar, A.; Drobne, D.; Kalčíková, G. Long-term interactions between microplastics and floating macrophyte Lemna minor: The potential for phytoremediation of microplastics in the aquatic environment. Sci. Total Environ. 2022, 831, 154866. [Google Scholar] [CrossRef] [PubMed]
- Biswal, B.K.; Bolan, N.; Zhu, Y.G.; Balasubramanian, R. Nature-based systems (NbS) for mitigation of stormwater and air pollution in urban areas: A review. Resour. Conserv. Recycl. 2022, 186, 106578. [Google Scholar] [CrossRef]
- dos Santos, N.; Clyde-Smith, D.; Qi, Y.; Gao, F.; Busquets, R.; Campos, L.C. A study of microfiber phytoremediation in vertical hydroponics. Sustainability 2023, 15, 2851. [Google Scholar] [CrossRef]
- Prathima, Y.; Venkatanarasaiah, D.; Akhil, D.; Pallerla, R.R. Restoration of Micro-/Nano Plastics: Contaminated Soil by Phytoremediation. In Micro and Nanoplastics in Soil: Threats to Plant-Based Food; Springer International Publishing: Cham, Switzerland, 2023; pp. 295–302. [Google Scholar] [CrossRef]
- Mudgal, V.; Raninga, M.; Patel, D.; Ankoliya, D.; Mudgal, A. A review on phytoremediation: Sustainable method for removal of heavy metals. Mater. Today Proc. 2023, 77, 201–208. [Google Scholar] [CrossRef]
- Xie, C.; Kan, L.; Guo, J.; Jin, S.; Li, Z.; Chen, D.; Li, X.; Che, S. A dynamic processes study of PM retention by trees under different wind conditions. Environ. Poll. 2018, 233, 315–322. [Google Scholar] [CrossRef]
- Kończak, B.; Cempa, M.; Deska, M. Assessment of the ability of roadside vegetation to remove particulate matter from the urban air. Environ. Poll. 2021, 268, 115465. [Google Scholar] [CrossRef]
- Prigioniero, A.; Postiglione, A.; Zuzolo, D.; Niinemets, Ü.; Tartaglia, M.; Scarano, P.; Mercurio, M.; Germinario, C.; Izzo, F.; Trifuoggi, M.; et al. Leaf surface functional traits influence particulate matter and polycyclic aromatic hydrocarbons air pollution mitigation: Insights from Mediterranean urban forests. J. Clean. Product. 2023, 418, 138158. [Google Scholar] [CrossRef]
- Ryu, J.; Kim, J.J.; Byeon, H.; Go, T.; Lee, S.J. Removal of fine particulate matter (PM2. 5) via atmospheric humidity caused by evapotranspiration. Environ. Poll. 2019, 245, 253–259. [Google Scholar] [CrossRef]
- Han, Y.; Hu, Y.; Qian, F. Effects of air temperature and humidity on particle deposition. Chem. Eng. Res. Des. 2011, 89, 2063–2069. [Google Scholar] [CrossRef]
- Kristanti, R.A.; Tirtalistyani, R.; Tang, Y.Y.; Thao, N.T.T.; Kasongo, J.; Wijayanti, Y. Phytoremediation Mechanism for Emerging Pollutants: A Review. Trop. Aquat. Soil Pollut. 2023, 3, 88–108. [Google Scholar] [CrossRef]
- Guo, K.; Yan, L.; He, Y.; Li, H.; Lam, S.S.; Peng, W.; Sonne, C. Phytoremediation as a potential technique for vehicle hazardous pollutants around highways. Environ. Poll. 2023, 322, 121130. [Google Scholar] [CrossRef] [PubMed]
- Baptista Neto, J.A.; Gaylarde, C.C.; de Carvalho, D.G.; Lourenço, M.F.; da Fonseca, E.M. Occurrence of microplastics derived from tyres in bottom sediments of Guanabara Bay, Brazil: A form of pollution that is neglected or difficult to detect? Water Emerg. Contam. Nanoplastics 2023, 2, 1–14. [Google Scholar] [CrossRef]
- Zhang, M.; Yin, H.; Tan, J.; Wang, X.; Yang, Z.; Hao, L.; Du, T.; Niu, Z.; Ge, Y. A comprehensive review of tyre wear particles: Formation, measurements, properties, and influencing factors. Atmos. Environ. 2023, 297, 119597. [Google Scholar] [CrossRef]
- Gaylarde, C.C.; Neto, J.A.B.; da Fonseca, E.M. Paint fragments as polluting microplastics: A brief review. Mar. Pollut. Bull. 2021, 162, 111847. [Google Scholar] [CrossRef]
- Burghardt, T.E.; Pashkevich, A. Road markings and microplastics—A critical literature review. Transp. Res. Part. D Transp. Environ. 2023, 119, 103740. [Google Scholar] [CrossRef]
- Gong, X.; Shi, G.; Zou, D.; Wu, Z.; Qin, P.; Yang, Y.; Hu, X.; Zhou, L.; Zhou, Y. Micro-and nano-plastics pollution and its potential remediation pathway by phytoremediation. Planta 2023, 257, 35. [Google Scholar] [CrossRef]
- Leonard, J.; Borthakur, A.; Koutnik, V.S.; Brar, J.; Glasman, J.; Cowger, W.; Dittrich, T.M.; Mohanty, S.K. Challenges of using leaves as a biomonitoring system to assess airborne microplastic deposition on urban tree canopies. Atmos. Pollut. Res. 2023, 14, 101651. [Google Scholar] [CrossRef]
- Budaniya, M.; Rai, A.C. Effectiveness of plants for passive removal of particulate matter is low in the indoor environment. Build. Environ. 2022, 222, 109384. [Google Scholar] [CrossRef]
- Perera, K.; Ziajahromi, S.; Nash, S.B.; Leusch, F.D. Evaluating the retention of airborne microplastics on plant leaf: Influence of leaf morphology. Environ. Poll. 2024, 346, 123673. [Google Scholar] [CrossRef]
- Lee, S.C.; Chang, M. Indoor and outdoor air quality investigation at schools in Hong Kong. Chemosphere 2000, 41, 109–113. [Google Scholar] [CrossRef]
- Dacarro, C.; Picco, A.M.; Grisoli, P.; Rodolfi, M. Determination of aerial microbiological contamination in scholastic sports environments. J. Appl. Microbiol. 2003, 95, 904–912. [Google Scholar] [CrossRef] [PubMed]
- Tringe, S.G.; Zhang, T.; Liu, X. The airborne metagenome in an indoor urban environment. PLoS ONE 2008, 20, e1862. [Google Scholar] [CrossRef]
- Kotzias, D. Indoor air and human exposure assessment—Needs and approaches. Exp. Toxicol. Pathol. 2005, 57, 5–7. [Google Scholar] [CrossRef] [PubMed]
- Gawrońska, H.; Bakera, B. Phytoremediation of particulate matter from indoor air by Chlorophytum comosum L. plants. Air Qual. Atmos. Health 2015, 8, 265–272. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO Global Air Quality Guidelines: Particulate Matter (PM2. 5 and PM10), Ozone, Nitrogen Dioxide, Sulfur Dioxide and Carbon Monoxide; World Health Organization: Geneva, Switzerland, 2021; ISBN 978-92-4-003421-1. [Google Scholar]
- Jiayu, C.; Qiaoqiao, R.; Feilong, C.; Chen, L.; Jiguo, W.; Zhendong, W.; Lingyun, C.; Liu, R.; Guoxia, Z. Microbiology community structure in bioaerosols and the respiratory diseases. J. Environ. Sci. Public. Health 2019, 3, 347–357. [Google Scholar] [CrossRef]
- Adhikari, A.; Reponen, T.; Grinshpun, S.A.; Martuzevicius, D.; Lemasters, G. Correlation of ambient inhalable bioaerosols with particulate matter and ozone: A two-year study. Environ. Poll. 2006, 140, 16–28. [Google Scholar] [CrossRef]
- Brągoszewska, E.; Biedroń, I. Indoor air quality and potential health risk impacts of exposure to antibiotic resistant bacteria in an office rooms in Southern Poland. Int. J. Environ. Res. Public Health 2018, 15, 2604. [Google Scholar] [CrossRef]
- Tolabi, Z.; Alimohammadi, M.; Hassanvand, M.S.; Nabizadeh, R.; Soleimani, H.; Zarei, A. The investigation of type and concentration of bioaerosols in the air of surgical rooms: A case study in Shariati Hospital, Karaj. MethodsX 2019, 6, 641–650. [Google Scholar] [CrossRef]
- Amato-Lourenço, L.F.; Costa, N.D.S.X.; Dantas, K.C.; dos Santos Galvão, L.; Moralles, F.N.; Lombardi, S.C.F.S.; Júnior, A.M.; Lindoso, J.A.L.; Ando, R.A.; Lima, F.G.; et al. Airborne microplastics and SARS-CoV-2 in total suspended particles in the area surrounding the largest medical centre in Latin America. Environ. Pollut. 2022, 292, 18299. [Google Scholar] [CrossRef]
- Wang, C.; Wu, W.; Pang, Z.; Liu, J.; Qiu, J.; Luan, T.; Deng, J.; Fang, Z. Polystyrene microplastics significantly facilitate influenza A virus infection of host cells. J. Hazard. Mater. 2023, 446, 130617. [Google Scholar] [CrossRef]
- Lu, J.; Yu, Z.; Ngiam, L.; Guo, J. Microplastics as potential carriers of viruses could prolong virus survival and infectivity. Water Res. 2022, 225, 119115. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.; Li, Y.; Boraschi, D. Association between microorganisms and microplastics: How does it change the host–pathogen interaction and subsequent immune response? Int. J. Mol. Sci. 2023, 24, 4065. [Google Scholar] [CrossRef] [PubMed]
- Kutralam-Muniasamy, G.; Shruti, V.C.; Pérez-Guevara, F. Plastisphere-hosted viruses: A review of interactions, behavior, and effects. J. Hazard. Mater. 2024, 472, 134533. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.; Shao, L.; Li, Y.; Jones, T.; Cao, Y.; Yang, C.X.; Zhang, M.; Santosh, M.; Feng, X.; BéruBé, K. Microplastic atmospheric dustfall pollution in urban environment: Evidence from the types, distribution, and probable sources in Beijing, China. Sci. Total Environ. 2022, 838, 155989. [Google Scholar] [CrossRef]
- Wright, S.L.; Ulke, J.; Font, A.; Chan, K.L.A.; Kelly, F.J. Atmospheric microplastic deposition in an urban environment and an evaluation of transport. Environ. Int. 2020, 136, 105411. [Google Scholar] [CrossRef]
- Chen, G.L.; Feng, Q.Y.; Wang, J. Mini-review of microplastics in the atmosphere and their risks to humans. Sci. Total Environ. 2020, 703, 135504. [Google Scholar] [CrossRef]
- Mbachu, O.; Jenkins, G.; Pratt, C.; and Kaparaju, P. A new contaminant superhighway? A review of sources, measurement techniques and fate of atmospheric microplastics. Water Air Soil Poll. 2020, 231, 85. [Google Scholar] [CrossRef]
- Kaya, A.T.; Yurtsever, M.; Bayraktar, S.C. Ubiquitous exposure to microfiber pollution in the air. Eur. Phys. J. Plus 2018, 133, 488. [Google Scholar] [CrossRef]
- Yuan, Z.; Li, H.X.; Lin, L.; Pan, Y.F.; Liu, S.; Hou, R.; Xu, X.R. Occurrence and human exposure risks of atmospheric microplastics: A review. Gondwana Res. 2020, 108, 200–212. [Google Scholar] [CrossRef]
- Rist, S.; Almroth, B.C.; Hartmann, N.B.; Karlsson, T.M. A critical perspective on early communications concerning human health aspects of microplastics. Sci. Total Environ. 2018, 626, 720–726. [Google Scholar] [CrossRef]
- Atis, S.; Tutluoglu, B.; Levent, E.; Ozturk, C.; Tunaci, A.; Sahin, K.; Saral, A.; Oktay, I.; Kanik, A.; Nemery, B. The respiratory effects of occupational polypropylene flock exposure. Eur. Resp. J. 2005, 25, 110–117. [Google Scholar] [CrossRef] [PubMed]
- Gasperi, J.; Wright, S.L.; Dris, R.; Collard, F.; Mandin, C.; Guerrouache, M.; Langlois, V.; Kelly, F.J.; Tassin, B. Microplastics in air: Are we breathing it in? Curr. Opin. Environ. Sci. Health 2018, 1, 1–5. [Google Scholar] [CrossRef]
- WHO. Determination of Airborne Fiber Number Concentrations: A Recommended Method, by Phase-Contrast Optical Microscopy (Membrane Filter Method); World Health Organization: Geneva, Switzerland, 1997; pp. 1–53. ISBN 92-4-154496-1. [Google Scholar]
- Law, B.D.; Bunn, W.B.; Hesterberg, T.W. Solubility of polymeric organic fibers and manmade vitreous fibers in Gambles solution. Inhal. Toxicol. 1990, 2, 321–339. [Google Scholar] [CrossRef]
- Smith, M.; Love, D.C.; Rochman, C.M.; Neff, R.A. Microplastics in seafood and the implications for human health. Curr. Environ. Health Rep. 2018, 5, 375–386. [Google Scholar] [CrossRef] [PubMed]
- Stock, V.; Böhmert, L.; Lisicki, E.; Block, R.; Cara-Carmona, J.; Pack, L.K.; Selb, R.; Lichtenstein, D.; Voss, L.; Henderson, C.J.; et al. Uptake and effects of orally ingested polystyrene microplastic particles in vitro and in vivo. Arch. Toxicol. 2019, 93, 1817–1833. [Google Scholar] [CrossRef]
- Van Cauwenberghe, L.; Janssen, C.R. Microplastics in bivalves cultured for human consumption. Environ. Poll. 2014, 193, 65–70. [Google Scholar] [CrossRef]
- Liao, Y.; Yang, J. Microplastic serves as a potential vector for Cr in an in vitro human digestive model. Sci. Total Environ. 2020, 703, 134805. [Google Scholar] [CrossRef]
- Enyoh, C.E.; Verla, A.W.; Verla, E.N.; Ibe, F.C.; Amaobi, C.E. Airborne microplastics: A review study on method for analysis, occurrence, movement and risks. Environ. Monit. Assess. 2019, 191, 668. [Google Scholar] [CrossRef]
- Chen, Y.; Meng, Y.; Liu, G.; Huang, X.; Chai, G. Probabilistic estimation of airborne micro- and nanoplastic intake in humans. Environ. Sci. Technol. 2024, 58, 9071–9081. [Google Scholar] [CrossRef] [PubMed]
- Eberhard, T.; Casillas, G.; Zarus, G.M.; Barr, D.B. Systematic review of microplastics and nanoplastics in indoor and outdoor air: Identifying a framework and data needs for quantifying human inhalation exposures. J. Expo. Sci. Environ. Epidemiol. 2024, 34, 185–196. [Google Scholar] [CrossRef]
- Huang, Y.; Qing, X.; Wang, W.; Han, G.; Wang, J. Mini-review on current studies of airborne microplastics: Analytical methods, occurrence, sources, fate and potential risk to human beings. TrAC Trends Anal. Chem. 2020, 125, 115821. [Google Scholar] [CrossRef]
- Marfella, R.; Prattichizzo, F.; Sardu, C.; Fulgenzi, G.; Graciotti, L.; Spadoni, T.; D’Onofrio, N.; Scisciola, L.; La Grotta, R.; Frigé, C.; et al. Microplastics and nanoplastics in atheromas and cardiovascular events. N. Eng. J. Med. 2024, 390, 900–910. [Google Scholar] [CrossRef] [PubMed]
- Campen, M.; Nihart, A.; Garcia, M.; Liu, R.; Olewine, M.; Castillo, E.; Bleske, B.; Scott, J.; Howard, T.; Gonzalez-Estrella, J.; et al. Bioaccumulation of microplastics in decedent human brains assessed by pyrolysis gas chromatography-mass spectrometry. Res. Sq. 2024. [Google Scholar] [CrossRef]
- Facciolà, A.; Visalli, G.; Pruiti Ciarello, M.; Di Pietro, A. Newly emerging airborne pollutants: Current knowledge of health impact of micro and nanoplastics. Int. J. Environ. Res. Public. Health 2021, 18, 2997. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- López, A.P.A.; Trilleras, J.; Arana, V.A.; Garcia-Alzate, L.S.; Grande-Tovar, C.D. Atmospheric microplastics: Exposure, toxicity, and detrimental health effects. RSC Adv. 2023, 13, 7468–7489. [Google Scholar] [CrossRef]
- Amato-Lourenço, L.F.; Carvalho-Oliveira, R.; Júnior, G.R.; dos Santos Galvão, L.; Ando, R.A.; Mauad, T. Presence of airborne microplastics in human lung tissue. J. Hazard. Mater. 2021, 416, 126124. [Google Scholar] [CrossRef]
- Jenner, L.C.; Rotchell, J.M.; Bennett, R.T.; Cowen, M.; Tentzeris, V.; Sadofsky, L.R. Detection of microplastics in human lung tissue using μFTIR spectroscopy. Sci. Total Environ. 2022, 831, 154907. [Google Scholar] [CrossRef]
- Huang, S.; Huang, X.; Bi, R.; Guo, Q.; Yu, X.; Zeng, Q.; Huang, Z.; Liu, T.; Wu, H.; Chen, Y.; et al. Detection and analysis of microplastics in human sputum. Environ. Sci. Technol. 2022, 56, 2476–2486. [Google Scholar] [CrossRef]
- Choudhury, A.; Simnani, F.Z.; Singh, D.; Patel, P.; Sinha, A.; Nandi, A.; Ghosh, A.; Saha, U.; Kumari, K.; Jaganathan, S.K.; et al. Atmospheric microplastic and nanoplastic: The toxicological paradigm on the cellular system. Ecotoxicol. Environ. Saf. 2023, 259, 115018. [Google Scholar] [CrossRef]
- Borgatta, M.; Breider, F. Inhalation of Microplastics—A Toxicological Complexity. Toxics 2024, 12, 358. [Google Scholar] [CrossRef]
- Amato-Lourenço, L.F.; Dos Santos Galvão, L.; de Weger, L.A.; Hiemstra, P.S.; Vijver, M.G.; Mauad, T. An emerging class of air pollutants: Potential effects of microplastics to respiratory human health? Sci. Total Environ. 2020, 749, 141676. [Google Scholar] [CrossRef] [PubMed]
- Ullah, S.; Ahmad, S.; Guo, X.; Ullah, S.; Nabi, G.; Wanghe, K. A review of the endocrine disrupting effects of micro and nano plastic and their associated chemicals in mammals. Front. Endocrinol. 2023, 13, 1084236. [Google Scholar] [CrossRef] [PubMed]
- Darbre, P.D. Chemical components of plastics as endocrine disruptors: Overview and commentary. Birth Defects Res. 2020, 112, 1300–1307. [Google Scholar] [CrossRef] [PubMed]
- Jewett, E.; Arnott, G.; Connolly, L.; Vasudevan, N.; Kevei, E. Microplastics and their impact on reproduction—Can we learn from the C. elegans model? Front. Toxicol. 2022, 4, 748912. [Google Scholar] [CrossRef]
- Yuan, Z.; Xu, X.R. Surface characteristics and biotoxicity of airborne microplastics. Compr. Anal. Chem. 2023, 100, 117–164. [Google Scholar] [CrossRef]
- Luo, H.; Liu, C.; He, D.; Xu, J.; Sun, J.; Li, J.; Pan, X. Environmental behaviors of microplastics in aquatic systems: A systematic review on degradation, adsorption, toxicity and biofilm under aging conditions. J. Hazard. Mater. 2022, 423, 126915. [Google Scholar] [CrossRef]
- Li, T.; Liu, R.; Wang, Q.; Rao, J.; Liu, Y.; Dai, Z.; Gooneratne, R.; Wang, J.; Xie, Q.; Zhang, X. A review of the influence of environmental pollutants microplastics, pesticides, antibiotics, air pollutants, viruses and bacteria on animal viruses. J. Hazard. Mater. 2024, 468, 133831. [Google Scholar] [CrossRef]
- Geng, Y.; Zhang, Z.; Zhou, W.; Shao, X.; Li, Z.; Zhou, Y. Individual exposure to microplastics through the inhalation route: Comparison of microplastics in inhaled indoor aerosol and exhaled breath air. Environ. Sci. Technol. Lett. 2023, 10, 464–470. [Google Scholar] [CrossRef]
- Costigan, E.; Collins, A.; Hatinoglu, M.D.; Bhagat, K.; MacRae, J.; Perreault, F.; Apul, O. Adsorption of organic pollutants by microplastics: Overview of a dissonant literature. J. Hazard. Mater. Adv. 2022, 6, 100091. [Google Scholar] [CrossRef]
- Budhiraja, V.; Urh, A.; Horvat, P.; Krzan, A. Synergistic adsorption of organic pollutants on weathered polyethylene microplastics. Polymers 2022, 14, 2674. [Google Scholar] [CrossRef]
- Xia, Y.; Niu, S.; Yu, J. Microplastics as vectors of organic pollutants in aquatic environment: A review on mechanisms, numerical models, and influencing factors. Sci. Total Environ. 2023, 887, 164008. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Li, Y.; Wang, J. Human health effects of airborne microplastics. Comp. Anal. Chem. 2023, 100, 185–223. [Google Scholar] [CrossRef]
- Barboza, L.G.A.; Cózar, A.; Gimenez, B.C.; Barros, T.L.; Kershaw, P.J.; Guilhermino, L. Macroplastics Pollution in the Marine Environment. In World Seas: An Environmental Evaluation; Academic Press: Cambridge, MA, USA, 2019; pp. 305–328. [Google Scholar] [CrossRef]
- Cooray, A.T.; Walpita, J.; Koliyabandara, P.A.; Soyza, I.U. Interaction of Chemical Contaminants with Microplastics. In Microplastics in the Ecosphere; Vithanage, M., Prasad, M.N.V., Eds.; John Wiley & Sons Ltd.: Hoboken, NJ, USA, 2023. [Google Scholar] [CrossRef]
- da Costa, J.P.; Avellan, A.; Tubić, A.; Duarte, A.C.; Rocha-Santos, T. Understanding interface exchanges for assessing environmental sorption of additives from microplastics: Current knowledge and perspectives. Molecules 2024, 29, 333. [Google Scholar] [CrossRef]
- Dong, Y.; Gao, M.; Song, Z.; Qiu, W. As (III) adsorption onto different-sized polystyrene microplastic particles and its mechanism. Chemosphere 2020, 239, 124792. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Zhao, M.; Ma, X.; Song, Y.; Zuo, S.; Li, H.; Deng, W. A critical review on the interactions of microplastics with heavy metals: Mechanism and their combined effect on organisms and humans. Sci. Total Environ. 2021, 788, 147620. [Google Scholar] [CrossRef]
- Li, K.; Wang, F. Global hotspots and trends in interactions of microplastics and heavy metals: A bibliometric analysis and literature review. Environ. Sci. Poll. Res. 2023, 30, 93309–93322. [Google Scholar] [CrossRef]
- Acarer, S. Microplastics in wastewater treatment plants: Sources, properties, removal efficiency, removal mechanisms, and interactions with pollutants. Water Sci. Technol. 2023, 87, 685–710. [Google Scholar] [CrossRef]
- Huang, W.; Deng, J.; Liang, J.; Xia, X. Comparison of lead adsorption on the aged conventional microplastics, biodegradable microplastics and environmentally-relevant tire wear particles. Chem. Eng. J. 2023, 460, 141838. [Google Scholar] [CrossRef]
- Adeleye, A.T.; Bahar, M.M.; Megharaj, M.; Fang, C.; Rahman, M.M. The unseen threat of the synergistic effects of microplastics and heavy metals in aquatic environments: A critical review. Curr. Pollut. Rep. 2024, 10, 478–497. [Google Scholar] [CrossRef]
- Chenappan, N.K.; Ibrahim, Y.S.; Anuar, S.T.; Yusof, K.M.K.K.; Jaafar, M.; Ahamad, F.; Sulaiman, W.Z.W.; Mohamad, N. Quantification and characterization of airborne microplastics in the coastal area of Terengganu, Malaysia. Environ. Monit. Assess. 2024, 196, 242. [Google Scholar] [CrossRef]
- Tang, S.; Lin, L.; Wang, X.; Yu, A.; Sun, X. Interfacial interactions between collected nylon microplastics and three divalent metal ions (Cu(II), Ni(II), Zn(II)) in aqueous solutions. J. Hazard. Mater. 2021, 403, 123548. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.; Lin, L.; Wang, X.; Feng, A.; Yu, A. Pb (II) uptake onto nylon microplastics: Interaction mechanism and adsorption performance. J. Hazard. Mater. 2020, 386, 121960. [Google Scholar] [CrossRef] [PubMed]
- Ho, W.K.; Law, J.C.F.; Lo, J.C.W.; Chng, I.K.X.; Hor, C.H.H.; Leung, K.S.Y. Sorption behavior, speciation, and toxicity of microplastic-bound chromium in multisolute systems. Environ. Sci. Technol. Lett. 2022, 10, cv27–cv32. [Google Scholar] [CrossRef]
- Fu, L.; Li, J.; Wang, G.; Luan, Y.; Dai, W. Adsorption behavior of organic pollutants on microplastics. Ecotoxicol. Environ. Saf. 2021, 217, 112207. [Google Scholar] [CrossRef]
- Ding, L.; Mao, R.; Ma, S.; Guo, X.; Zhu, L. High temperature depended on the ageing mechanism of microplastics under different environmental conditions and its effect on the distribution of organic pollutants. Water Res. 2020, 174, 115634. [Google Scholar] [CrossRef]
- Sharma, M.D.; Elanjickal, A.I.; Mankar, J.S.; Krupadam, R.J. Assessment of cancer risk of microplastics enriched with polycyclic aromatic hydrocarbons. J. Hazard. Mater. 2020, 398, 122994. [Google Scholar] [CrossRef]
- Srogi, K. Monitoring of environmental exposure to polycyclic aromatic hydrocarbons: A review. Environ. Chem. Lett. 2007, 5, 169–195. [Google Scholar] [CrossRef]
- Fussell, J.C.; Franklin, M.; Green, D.C.; Gustafsson, M.; Harrison, R.M.; Hicks, W.; Kelly, F.J.; Kishta, F.; Miller, M.R.; Mudway, I.S.; et al. A review of road traffic-derived non-exhaust particles: Emissions, physicochemical characteristics, health risks, and mitigation measures. Environ. Sci. Technol. 2022, 56, 6813–6835. [Google Scholar] [CrossRef]
- Hyötyläinen, T.; Oikari, A. Bioaccumulation of PAHs from creosote-contaminated sediment in a laboratory-exposed freshwater oligochaete, Lumbriculus variegates. Chemosphere 2004, 57, 159–164. [Google Scholar] [CrossRef]
- Luo, D.; Wang, Z.; Liao, Z.; Chen, G.; Ji, X.; Sang, Y.; Qu, L.; Chen, Z.; Wang, Z.; Dahlgren, R.A.; et al. Airborne microplastics in urban, rural and wildland environments on the Tibetan Plateau. J. Hazard. Mater. 2024, 465, 133177. [Google Scholar] [CrossRef]
- Xu, L.; Bai, X.; Li, K.; Zhang, G.; Zhang, M.; Hu, M.; Huang, Y. Human exposure to ambient atmospheric microplastics in a megacity: Spatiotemporal ariation and associated microorganism-related health risk. Environ. Sci. Technol. 2024, 58, 3702–3713. [Google Scholar] [CrossRef] [PubMed]
- Akhbarizadeh, R.; Dobaradaran, S.; Torkmahalleh, M.A.; Saeedi, R.; Aibaghi, R.; Ghasemi, F.F. Suspended fine particulate matter (PM2.5), microplastics (MPs), and polycyclic aromatic hydrocarbons (PAHs) in air: Their possible relationships and health implications. Environ. Res. 2021, 192, 110339. [Google Scholar] [CrossRef] [PubMed]
- Prata, J.C.; da Costa, J.P.; Lopes, I.; Duarte, A.C.; Rocha-Santos, T. Environmental exposure to microplastics: An overview on possible human health effects. Sci. Total Environ. 2020, 702, 134455. [Google Scholar] [CrossRef] [PubMed]
- Campanale, C.; Dierkes, G.; Massarelli, C.; Bagnuolo, G.; Uricchio, V.F. A relevant screening of organic contaminants present on freshwater and pre-production microplastics. Toxics 2020, 8, 100. [Google Scholar] [CrossRef] [PubMed]
- Sridharan, S.; Kumar, M.; Singh, L.; Bolan, N.S.; Saha, M. Microplastics as an emerging source of particulate air pollution: A critical review. J. Hazard. Mater. 2021, 418, 126245. [Google Scholar] [CrossRef]
- Hirai, H.; Takada, H.; Ogata, Y.; Yamashita, R.; Mizukawa, K.; Saha, M.; Kwan, C.; Moore, C.; Gray, H.; Laursen, D.; et al. Organic micropollutants in marine plastics debris from the open ocean and remote and urban beaches. Mar. Pollut. Bull. 2011, 62, 1683–1692. [Google Scholar] [CrossRef]
- Benedetti, B.; Di Carro, M.; Magi, E. Multivariate optimization of an extraction procedure based on magnetic molecular imprinted polymer for the determination of polycyclic aromatic hydrocarbons in sea water. Microchem. J. 2019, 145, 1199–1206. [Google Scholar] [CrossRef]
- Conesa, J.A. Adsorption of PAHs and PCDD/Fs in microplastics: A review. Microplastics 2022, 1, 346–358. [Google Scholar] [CrossRef]
- Moorchilot, V.S.; Aravind, U.K.; Aravindakumar, C.T. Occurrence of azo-dyes, plasticizers, and PAH-bound microplastics: An emerging source and sink for hazardous compounds in indoor environments? Air Qual. Atmos. Health 2024, 17, 425–438. [Google Scholar] [CrossRef]
- Chen, L.; Shao, H.; Ren, Y.; Mao, C.; Chen, K.; Wang, H.; Jing, S.; Xu, C.; Xu, G. Investigation of the adsorption behavior and adsorption mechanism of pollutants onto electron beam-aged microplastics. Sci. Total Environ. 2024, 917, 170298. [Google Scholar] [CrossRef]
- Rafa, N.; Ahmed, B.; Zohora, F.; Bakya, J.; Ahmed, S.; Ahmed, S.F.; Mofijur, M.; Chowdhury, A.A.; Almomani, F. Microplastics as carriers of toxic pollutants: Source, transport, and toxicological effects. Environ. Poll. 2023, 343, 123190. [Google Scholar] [CrossRef] [PubMed]
- Gomiero, A.; Strafella, P.; Pellini, G.; Salvalaggio, V.; Fabi, G. Comparative effects of ingested PVC micro particles with and without adsorbed benzo (a) pyrene vs. spiked sediments on the cellular and sub cellular processes of the benthic organism Hediste diversicolor. Front. Mar. Sci. 2018, 5, 99. [Google Scholar] [CrossRef]
- Wang, Z.; Dong, H.; Wang, Y.; Ren, R.; Qin, X.; Wang, S. Effects of microplastics and their adsorption of cadmium as vectors on the cladoceran Moina monogolica Daday: Implications for plastic-ingesting organisms. J. Hazard. Mater. 2020, 400, 123239. [Google Scholar] [CrossRef] [PubMed]
- Magara, G.; Khan, F.R.; Pinti, M.; Syberg, K.; Inzirillo, A.; Elia, A.C. Effects of combined exposures of fluoranthene and polyethylene or polyhydroxybutyrate microplastics on oxidative stress biomarkers in the blue mussel (Mytilus edulis). J. Toxicol. Environ. Health 2019, 82 Pt A, 616–625. [Google Scholar] [CrossRef]
- Hanslik, L.; Huppertsberg, S.; Kämmer, N.; Knepper, T.P.; Braunbeck, T. Rethinking the relevance of microplastics as vector for anthropogenic contaminants: Adsorption of toxicants to microplastics during exposure in a highly polluted stream-Analytical quantification and assessment of toxic effects in zebrafish (Danio rerio). Sci. Total Environ. 2022, 816, 151640. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.T.; Ding, J.; Xiong, C.; Zhu, D.; Li, G.; Jia, X.Y.; Zhu, Y.G.; Xue, X.M. Exposure to microplastics lowers arsenic accumulation and alters gut bacterial communities of earthworm Metaphire californica. Environ. Poll. 2019, 251, 110–116. [Google Scholar] [CrossRef]
- Lin, W.; Jiang, R.; Xiong, Y.; Wu, J.; Xu, J.; Zheng, J.; Zhu, F.; Ouyang, G. Quantification of the combined toxic effect of polychlorinated biphenyls and nano-sized polystyrene on Daphnia magna. J. Hazard. Mater. 2019, 364, 531–536. [Google Scholar] [CrossRef]
- Akanyange, S.N.; Lyu, X.; Zhao, X.; Li, X.; Zhang, Y.; Crittenden, J.C.; Anning, C.; Chen, T.; Jiang, T.; Zhao, H. Does microplastic really represent a threat? A review of the atmospheric contamination sources and potential impacts. Sci. Total Environ. 2021, 777, 146020. [Google Scholar] [CrossRef]
- Abbasi, S.; Keshavarzi, B.; Moore, F.; Turner, A.; Kelly, F.J.; Dominguez, A.O.; Jaafarzadeh, N. Distribution and potential health impacts of microplastics and microrubbers in air and street dusts from Asaluyeh County, Iran. Environ. Pollut. 2019, 244, 153–164. [Google Scholar] [CrossRef]
- Ganzleben, C.; Antignac, J.P.; Barouki, R.; Castaño, A.; Fiddicke, U.; Klánová, J.; Lebret, E.; Olea, N.; Sarigiannis, D.; Schoeters, G.R.; et al. Human biomonitoring as a tool to support chemicals regulation in the European Union. Int. J. Hyg. Environ. Health 2017, 220, 94–97. [Google Scholar] [CrossRef] [PubMed]
- Louro, H.; Heinälä, M.; Bessems, J.; Buekers, J.; Vermeire, T.; Woutersen, M.; van Engelen, J.; Borges, T.; Rousselle, C.; Ougier, E.; et al. Human biomonitoring in health risk assessment in Europe: Current practices and recommendations for the future. Int. J. Hyg. Environ. Health 2019, 222, 727–737. [Google Scholar] [CrossRef] [PubMed]
- Zuri, G.; Karanasiou, A.; Lacorte, S. Human biomonitoring of microplastics and health implications: A review. Environ. Res. 2023, 237, 116966. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gaylarde, C.C.; Baptista Neto, J.A.; da Fonseca, E.M. Indoor Airborne Microplastics: Human Health Importance and Effects of Air Filtration and Turbulence. Microplastics 2024, 3, 653-670. https://doi.org/10.3390/microplastics3040040
Gaylarde CC, Baptista Neto JA, da Fonseca EM. Indoor Airborne Microplastics: Human Health Importance and Effects of Air Filtration and Turbulence. Microplastics. 2024; 3(4):653-670. https://doi.org/10.3390/microplastics3040040
Chicago/Turabian StyleGaylarde, Christine C., José Antonio Baptista Neto, and Estefan M. da Fonseca. 2024. "Indoor Airborne Microplastics: Human Health Importance and Effects of Air Filtration and Turbulence" Microplastics 3, no. 4: 653-670. https://doi.org/10.3390/microplastics3040040
APA StyleGaylarde, C. C., Baptista Neto, J. A., & da Fonseca, E. M. (2024). Indoor Airborne Microplastics: Human Health Importance and Effects of Air Filtration and Turbulence. Microplastics, 3(4), 653-670. https://doi.org/10.3390/microplastics3040040





