Abstract
Background: Over the past few decades, epidemic outbreaks and disease occurrences have become more frequent and widespread in Africa, posing challenges for poor countries in the region and impacting vulnerable populations. Limited resources, inadequate healthcare infrastructure, socioeconomic inequalities, malnutrition, mass gatherings, and lack of proper sanitation and hygiene contribute to Africa’s high burden of epidemics and infectious diseases such as cholera, measles, monkeypox, Ebola viral disease, and COVID-19. This paper reviewed epidemic outbreaks and diseases transmitted through intimate contact in Africa and their impacts on vulnerable populations. Methods: A narrative review approach was adopted to gather and analyze the relevant literature on epidemic outbreaks in African sub-regions. The review encompassed causes, transmission patterns, demographic impact, community susceptibility, preventive measures, and psychosocial risk-taking behaviors. Results: This study emphasizes the importance of addressing the causes of response lapses and the resulting human, material, and economic losses in the region. Effective preventive measures include disease surveillance, early mitigation strategies, contact tracing, personal protective measures, improved political and public health leadership, and socioeconomic equity. However, the review highlights challenges in implementing these measures effectively due to limited resources, delayed detection, and difficulties in scaling up response solutions. Conclusions: There is a need for a comprehensive approach involving health departments, infrastructure development, and addressing socioeconomic factors.
1. Introduction
The management of diseases and infections constitutes a critical determinant that influences health outcomes and life expectancy within a given population [1]. Understanding and mitigating the transmission of diseases necessitates an examination of the determinants influencing behavioral patterns, whether they remain stable or evolve. This overarching objective contributes to the expanding body of literature on the psychosocial impacts of pandemics and epidemics. Over the past decades, the African continent has experienced a surge in the frequency and geographical scale of epidemics and infectious disease outbreaks. These outbreaks exhibit diverse socio-economic focal points across the region, often eliciting political responses and occasionally presenting formidable challenges for marginalized community groups. Specifically, the resurgence of infectious diseases such as diphtheria, influenza, Ebola, monkeypox, and measles poses considerable challenges for economically disadvantaged nations, impeding progress and inflicting severe global consequences [2,3].
Infectious diseases attributed to bacterial, viral, fungal, or parasitic etiologies consistently permeate African society and typically manifest sporadically. However, sporadic outbreaks can precipitate rapid dissemination of novel pathogens affecting a significant proportion of individuals within localized communities. Epidemics occur when specific epidemiological conditions are met, including a critical pool of susceptible hosts, efficient transmission pathways for the pathogen, and adequate availability of infectious agents [3]. Certain health-related behaviors within Africa, particularly substance abuse and addiction, exhibit prevalence rates significantly exceeding anticipated levels, thereby meriting their classification as full-fledged epidemics.
While epidemics are typically associated with pronounced negative consequences and health risks, they tend to follow predictable patterns that facilitate the monitoring and containment of infectious diseases. This predictive capacity is invaluable in mitigating exponential growth and curtailing global adverse effects as exemplified by communicable viral diseases such as influenza. However, Africa’s economy is marked by constrained healthcare infrastructure, insufficient access to intensive care facilities, and various systemic deficiencies in rural communities. These drive the burden of epidemics and infectious diseases disproportionately severe within the continent, with a pronounced impact on the most vulnerable demographic segments [1,3].
This review underscored the contributory factors underlying lapses in response to epidemics and the resultant human, material, and economic toll across the region. A salient area of vulnerability pertains to neonatal and child health, which is frequently relegated in favor of reallocating resources, healthcare personnel, and medical supplies to address the exigencies of affected adults. The economic impacts of epidemics, as seen during the 2014–2016 Ebola outbreak in West Africa, are substantial, leading to extensive infrastructural decay and heightened food insecurity [2]. Approximately 50% of mortality cases in Africa are ascribed to epidemics, with maternal health issues ranking as the second leading cause of fatalities [3]. The problem is further compounded by non-communicable diseases, including stroke, diabetes, obesity, cancer, and cardiovascular maladies which exacerbate the predicament because of healthcare system inadequacies.
Another facet of the epidemic milieu in Africa is the significant increase in zoonotic pathogen outbreaks, with the Ebola virus accounting for over 50% of such incidents [2,4]. Zoonotic diseases such as dengue fever, anthrax, and monkeypox also engender substantial risks. This is primarily due to the consumption of animal-based foods and the prevalence of cultural practices that overlook wildlife conservation [4].
Psychosocial behaviors predicated upon an individual’s inclination to lead a social, interactive existence constitute a pivotal element in epidemic control. These behaviors coalesce psychological and social dynamics and have significantly manifested in past epidemic events, including the Ebola crisis, the COVID-19 pandemic, Lassa fever, cholera, and monkeypox [1,2,4]. Africans, particularly those residing in rural regions, are renowned for their sociable and affectionate disposition, characterized by physical contact, close interpersonal proximity, and diverse manifestations of affection. This communal lifestyle and overcrowding are driving factors behind the growing risk of outbreaks in the African continent.
Notwithstanding the transformative changes in interpersonal interactions brought about by the global impact of the COVID-19 pandemic, rural residents in Africa have continued to demonstrate resilience in preserving these traditional social behaviors. They often disregard recommended health precautions such as maintaining physical distancing and observing stringent hygiene practices, thereby promoting the resurgence of epidemics as exemplified by the recurrence of monkeypox.
This review provides a comprehensive examination of epidemic outbreaks and diseases transmitted through close contact within the African context. It further scrutinizes their modes of transmission, demographic ramifications, community susceptibility, and the psychosocial impacts of epidemic events.
2. Methods
This study employed a narrative review, adopting different web search engines and databases and evaluating relevant published reports to provide a comprehensive overview of the recent epidemiology, responses, and resultant risk associated with epidemics within the African sub-region. To retrieve relevant information, we performed a literature search in different electronic databases, including Medline, PubMed, Web of Science, Scopus, and Google Scholar. We used Boelean operators with the following search terms: “Cholera”, “Ebola viral disease”, “measles”, “monkeypox”, “Lassa fever”, “COVID-19”, “infectious disease outbreaks”, “zoonotic disease outbreaks”, “viral haemorrhagic fevers”, “zoonotic pathogen outbreaks”, “disease surveillance systems”, “disease surveillance”, “emerging infectious diseases”, “re-emerging infectious diseases”, “zoonoses”, “health inequalities”, “epidemic response”, “animals”, “environment”, and “Africa sub-region”. This paper included publications that offered insights into the recent epidemiological trends, response strategies, and the resultant risks associated with epidemic outbreaks within the African population. The paper also included publications that were only published in the English language, from peer-reviewed journals and reputable organizational reports. Data on the most recently estimated infectious disease epidemic outbreaks were obtained from the US Centers for Disease Control and Prevention, the Africa Centre for Disease Control and Prevention, and the World Health Organization databases and dashboards. Data from these databases and dashboards provided valuable insights into the epidemiological information and trends on the key recent epidemic outbreaks included in this study. Abstracts and articles not written in English, studies that did not directly explore the most recent epidemic outbreaks in Africa, and studies published in peer-reviewed sources with questionable credibility were excluded from the study. The authors W.B.V., C.W-V., L.K.D., B.M.A., J.N.P., and U.A.E independently verified that the selected studies were of high quality and met the inclusion criteria.
3. Epidemiology of Recent Infectious Disease Outbreaks of Public Health Importance in Africa
While epidemics encompass both infectious and non-communicable outbreaks, the historical focus in Africa has primarily been on communicable outbreaks. Diseases such as yellow fever, Lassa fever, Rift Valley fever, smallpox, measles, polio, influenza, cholera, Ebola, leptospirosis, meningitis, Middle East respiratory syndrome (MERS), plague, Zika, and, most recently, COVID-19 are a few examples of infectious epidemics that are prevalent in the African sub-region and pose a significant threat due to deep cultural and social connections [4]. The most reported epidemic outbreaks in Africa in 2023 and 2024 are shown in Figure 1 and Figure 2, respectively.
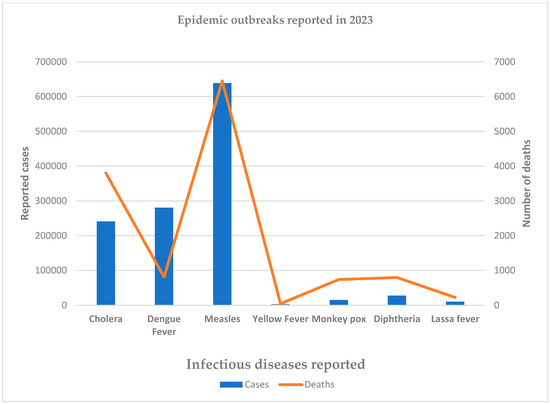
Figure 1.
The most reported epidemic outbreaks in Africa as of December 2023. Data extracted from Africa Centre for Disease Control and Prevention, Africa CDC Epidemic Intelligence Report, 29 March 2024 [5].
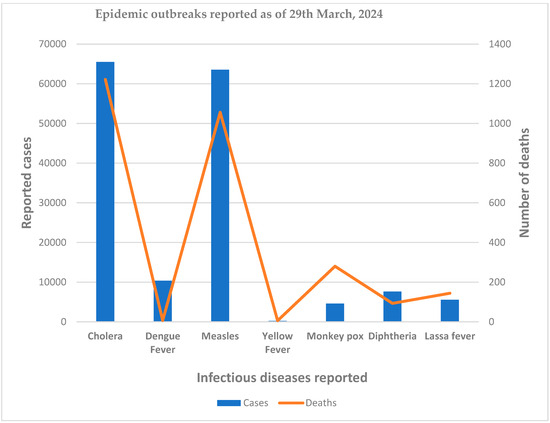
Figure 2.
The most reported epidemic outbreaks in Africa as of March 2024. Data extracted from Africa Centre for Disease Control and Prevention, Epidemic Intelligence Report, 29 March 2024 [5].
3.1. Ebola Viral Disease
Ebola virus disease (EVD) is one of the major infectious diseases of public health importance in the African region. The virus originated from wild animals and is transmitted to the human population through direct contact with the blood, secretions, organs, or other bodily fluids of infected people, and contaminated surfaces. Since the first discovery of the virus in 1976, there have been pockets of EVD outbreaks, but these were restricted to Central Africa [6]. However, the 2014–2016 outbreak in West Africa was the largest and most devastating EVD outbreak spreading from Guinea to Liberia, Sierra Leone, Mali, Senegal, and Nigeria resulting in 28,652 cases and 11,325 deaths [7]. The socioeconomic burden and impacts of the outbreak were approximately USD 54 billion between 2014 and 2016 [8]. In addition, the World Bank put the economic impact of the 2014–2016 Ebola crisis on the three most affected countries at approximately USD 600 million for Guinea, USD 300 million for Liberia, and USD 1.9 billion for Sierra Leone [9]. After the major and devastating 2014–2016 EVD outbreak in West Africa, eight outbreaks have been recorded in the Democratic Republic of Congo (cases: 3691; deaths: 2400), one outbreak in Uganda (cases: 165; deaths: 55), and one outbreak in Guinea (cases: 23; deaths: 12) [10]. This further highlights the lack of public health leadership, inadequacies in the outbreak response mechanisms, persisting vulnerabilities, and substantial inequities in the public health emergency response protocols in the affected countries [7,11,12]
3.2. Monkeypox
Monkeypox, caused by the monkeypox virus, is one of the emerging outbreaks in Africa because of zoonotic pathogens that switched species and infected humans. Monkeypox is common in West, Central, and East Africa with higher endemicity in the Democratic Republic of Congo. However, a multi-country outbreak of monkeypox outside the African continent was reported in May 2022. For the first time, a total of 117 countries reported monkeypox cases within the 2022–2023 period [13]. In 110 non-endemic countries, 83,026 confirmed cases of mpox and 269 deaths were reported in 2022 [14]. During this period, 1176 confirmed cases and 219 deaths of monkeypox were reported in eight endemic African Union Member States [14]. In 2023, a total of 14,837 cases and 738 confirmed deaths of monkeypox were reported from seven African Union member states. As of April 2024, a total of 4594 cases and 280 deaths of monkeypox have been reported from five African Union Member States, including Cameroon, Central African Republic, Congo, Democratic Republic of Congo, and Liberia [5]. From a global perspective, an overview of the mpox epidemiological situation, as reported to WHO as of 31 May 2024, shows a total of 97,745 laboratory-confirmed cases and 203 deaths [15]. The total reported monkeypox cases and deaths according to WHO region are shown in Table 1. Therefore, continuous monitoring, risk assessment, and surveillance of monkeypox in both endemic and non-endemic countries are required to contain the global spread and reduce the direct economic burden and the indirect social impacts.

Table 1.
The cumulative monkeypox cases and deaths according to WHO region between January 2022 to May 2024 [15].
3.3. The Coronavirus Disease 2019 (COVID-19)
COVID-19 also constitutes an infectious disease outbreak that has plagued Africa in recent times. The COVID-19 pandemic caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) is considered a major global health threat of the 21st century. The disease was first reported in Wuhan city of Hubei province in China in December 2019 [16] and was declared a pandemic on 11 March 2020 by the World Health Organization [17] because of its global spread and fatality. As of 7 July 2024, 775,673,955 COVID-19 cases and 7,053,524 deaths (Figure 3) have been reported globally, with most fatalities occurring in the USA, Brazil, and India [18]. In the African region, a total of 12,381,836 COVID-19 cases and 259,265 deaths have been reported by the 55 African Union member states as of 28 March 2024 [5]. The COVID-19 pandemic had a devastating social, psychological, and economic impact on the global economy [19]. Unfortunately, the African populations suffered from most of the economic consequences and social and psychological impacts of the COVID-19 pandemic. For instance, it was estimated that the African region lost between USD 37 and USD 79 billion during the COVID-19 pandemic due to the lockdown directive resulting in a reduction in agricultural production, weakening of supply chains, increasing trade deficit, increasing unemployment, and massive job losses [20,21].
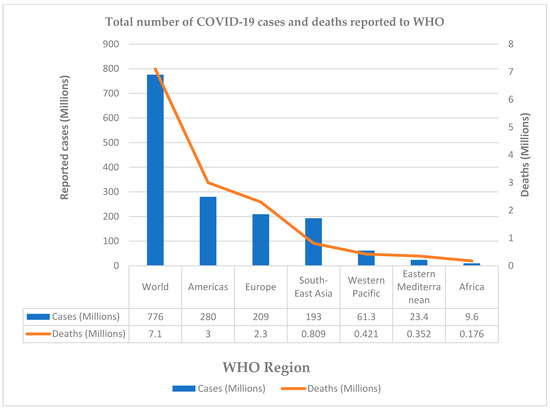
Figure 3.
Cumulative number of COVID-19 cases and deaths reported to WHO from January 2020 to 7 July 2024. Source: WHO 2024 [18].
3.4. Lassa Fever
Lassa fever, caused by the Lassa virus, is spread by the multimammate rat (Mastomys natalensisis) and outbreaks are common in West Africa, including Sierra Leone, Liberia, Guinea, and Nigeria. In 2023, a total of 10,353 cases and 221 deaths of Lassa fever were reported from five African Union member states [5]. However, 5552 cases and 144 deaths of Lassa fever have been reported as of 28 March 2024, from three African Union member states, including Guinea (27 cases; 2 deaths), Liberia (33; 0), and Nigeria (5132; 138) [5]. These infectious disease outbreaks have a major impact on African societies and public health infrastructures highlighting the need to strengthen initiatives for disease outbreak surveillance, emergency response strategies, and control in the region [22]. In addition, more regional-focused research is needed to identify environmental, socioeconomic, and cultural factors that boost the emergence and transmission of epidemic-prone diseases, as well as to better understand the factors that affect the impact and spread of epidemics in the African region.
4. Pattern and Transmission of Epidemics around African Sub-Regions
A recent increase in an infectious agent’s virulence, as well as its introduction into an environment where it has never been found before, can lead to an epidemic. This might be connected to the seasonal nature of specific infectious diseases. Any infectious agent’s epidemic potential has five essential components, including susceptible recruitment through reproduction, transmission, acquired or fading immunity and recovery, natural or disease-induced mortality, and symptomatology and pathology, which can be affected by seasonality [23]. It could also be influenced by variables that enhance host exposure to the agent or involve introduction through new entry points, such as a change in the host’s susceptibility to the agent [24]. Changes in climate can be a contributing factor, as seen in whooping cough and measles during certain periods of seasonal shift, or even exposure to chemicals [23]. More susceptible individuals are exposed to an increased risk of transmission which might be promoted by unfavorable environmental elements such as water, food, and air.
4.1. Epidemics Spread Patterns
Depending on how epidemics spread through a community, they can be grouped into different categories. The proliferation of all these patterns is directly related to the communal African dwellings and settlements. A common-source epidemic occurs when a group of humans are collectively exposed to an infectious agent or toxin from a single source. This type of epidemic can be classified as a point-source outbreak if the group’s exposure happens over a relatively short time frame, resulting in all affected individuals becoming ill within one incubation period. In cases of continuous common-source outbreaks where there is a range of exposures and incubation times, the peaks on the epidemic curve tend to spread out and become less distinct.
There is also the possibility of an outbreak spreading from one person to another. Like syphilis, transmission typically occurs through direct person-to-person contact. Moreover, transmission can occur through a vehicle or a vector such as when exchanging needles to spread HIV or hepatitis B (e.g., transmission of yellow fever by mosquitoes). As an outbreak is propagated, cases develop throughout several incubation periods. Certain diseases share characteristics with both common source and spread epidemics as it is not unusual for an outbreak to have a common source and then spread from person to person; hence it is referred to as mixed epidemics. Certain epidemics do not spread from person to person or have common sources in the traditional sense. There must be sufficient human–vector interaction, enough vector presence, and sufficient prevalence of infection in the host species for zoonotic or vector-borne disease outbreaks to occur.
4.2. Epidemic Transmission Routes in Africa
The following approaches represent various ways in which epidemic diseases propagate among African nations. Any of the following methods can interact with one another to affect the mechanism and promote the transmission of close-contact disease infections.
Airborne transmission: This is the spread of infection through dust or droplet nuclei in the air with the assistance of the wind [25].
Arthropod transmission: An insect can spread disease by an infected proboscis or foot, or it can do so physiologically when an arthropod harbors an organism that is growing or replicating.
Biological transmission: This involves a typical biological process such as the infectious agent progressing through a stage of development in an intermediate host.
Contact transmission: The disease agent is spread either directly through biting, sucking, or chewing, or indirectly through inhaling droplets, drinking tainted water, or riding in tainted vehicles.
Fecal–oral transmission: The infectious agent is dispersed in the feces of the diseased host and is ingested by the susceptible host, who then becomes infected.
Lateral spread to members of the same group and concurrent spread to contemporaries are examples of horizontal transmission [26].
5. Epidemics Preventive Measures and Mitigating Responses in Africa
Having the capacity to promptly and efficiently deploy emergency personnel, particularly local responders, along with a legal framework to guarantee the safety and well-being of healthcare professionals, are crucial elements in preparing for disease prevention during an epidemic, particularly for contagious diseases transmitted through close contact [27]. A system for disease surveillance constitutes several layers. For instance, Tanzania has a national laboratory that manages testing at 200 health facilities and monitors the spread of infectious illnesses. Moreover, techniques based on machine learning and artificial intelligence have demonstrated very high performance, reaching up to 99% accuracy in categorization and computation performance [28]. Additionally, researchers have created weather-based forecasting methods for infectious diseases, particularly dengue and malaria, utilizing meteorological variables such as temperature and rainfall [28,29]. This agrees with other researchers who have demonstrated that many of these innovations will help in the diagnosis, classification, risk forecasting, and prediction of future disease outbreaks if properly adopted [30,31]. Additionally, prevention and control measures such as vaccinations can be planned for and implemented before disease outbreak seasons, and this can improve a community’s herd immunity and resilience towards infectious disease.
The genuine response to an epidemic outbreak emergency requires an additional layer. To achieve what is commonly known as “flattening the epidemic curve”, it is necessary to implement early and proactive mitigation measures that utilize non-pharmacological therapies, such as social and physical isolation, aggressive contact tracing, issuing “stay-at-home” orders, providing the appropriate personal protective equipment, and other physical barriers to prevent the spread of the infectious agent. The rising number of high-threat infectious hazards in Africa is a direct result of these outbreaks of vaccine-preventable infectious diseases. This is due to the lack of sufficient healthcare infrastructure and resources, delayed detection, and challenges in implementing appropriate responses. Research has shown that there is a lack of understanding of case definitions and the identification of high-risk patients among a significant portion of African healthcare professionals [32]. These gaps have negative impacts on support and care efforts, hampering efforts to identify suspected cases [32,33]. Therefore, developing effective national health systems and combating epidemics in African populations requires a multifaceted approach. Additionally, managing health issues, especially epidemics, is not solely the responsibility of health departments or professionals; it also depends on the actions of departments in charge of providing clean water and sanitation, ensuring that food is nutritious and of high quality (including immune status), housing, and population management.
The typical “fire brigade service approach”, which allows situations to escalate to the point where immediate treatment should have been given, has often been used as a response measure to combat diseases in Africa. The capacity to contain transmission spread has generally not been able to keep up with the surge at peak levels, making it difficult to scale up large-scale response solutions. Even when suppression measures are included, there are still constraints such as a lack of beds for effective monitoring and management at health centers, a shortage of personal protective equipment, and a scarcity of medical supplies and essential management medications [34,35].
Although the lockdown technique may be a very effective response tactic in Africa where the more persistent problem of economic viability exists, individuals would prefer to die of sickness rather than from a hunger strike. This hunger effect was significantly responsible for a major breakdown of law and order in Nigeria in 2020 when warehouses were broken into by youths in crowded environments despite the COVID-19 risk while seeking food to survive after an unending lockdown strategy. Lockdown tactics may only yield short-term delays in transmission due to economic viability difficulties, and if these issues are not resolved by economic packages made accessible by global financing actors, poverty may worsen [36,37]. The political approach of granting the upper socioeconomic classes special treatment in isolation methods during resource allocation, such as priority for bed space, oxygen, and other essentials, presents a particularly concerning aspect that could jeopardize the success of epidemics response efforts in African countries. In most cases, this political influence also affects the pattern of disease transmission. Instead of being isolated in designated facilities for proper monitoring—as is the usual practice for those in the lower socioeconomic status and less privileged population—those in higher socioeconomic classes were advised to self-isolate, leading to an increased number of infections spreading within their communities.
African populations are known to be highly socially bonded, which is always observable in the way they exchange pleasantries by hugging and shaking hands, and the way they work together within close family bonds. This poses a serious challenge in managing outbreaks of close-contact infections. General physical distancing, a strategy employed during the COVID-19 pandemic for a reduction in all contact outside the household, was not very effective in the African scenario. It must be highlighted that although physical separation can result in a significant decrease in the epidemic peak, this is temporary since the impact on the rural population may be socioculturally detrimental and result in intolerable limitations on jobs, education, and/or other aspects of public life and fulfilling, engaging activities. As a result, it is advisable to prioritize within-household shielding over other solutions, especially if it can be organized and led by the communities themselves [38,39]. This approach is considered feasible and can achieve a suggested target of reducing high-risk individuals’ contact by 70%, though raising awareness about the risks remains a challenge [38,39]. It is crucial to assess each strategy in consideration of the specific needs of the community residents to prevent exacerbating issues or triggering the outbreak of a riot crisis while addressing the public health crisis. This situation was observed during the 2014–2015 Ebola period in parts of Niger, Liberia, Kenya, Uganda, Ethiopia, South Africa, and Nigeria when certain intervention measures, particularly the distribution of government and donor-provided relief aid, were poorly managed.
6. Demographic Factors and Assessing Psycho-Social Effects on Epidemics in the African Population
Epidemiology and demography work in conjunction to produce the overall disease and death trends of the African sub-region where infectious diseases and epidemics predominate [4].
6.1. Migration
People are at a high risk of bringing epidemic pathogens into other nations when they cross the continent by land, water, or air. This could result in people moving from places with a higher prevalence of infection to areas with lower prevalence, which would further the spread of illness [40]. For example, the spread of the 2014–2016 EVD outbreak in West Africa to Nigeria was because of intercontinental migration [9].
6.2. Rapid Urbanization
Physical separation is difficult in densely populated urban regions, especially in sub-Saharan Africa where urbanization is accelerating at the fastest rate in the world with an expected 65 million new urban residents annually [41]. In addition, a high percentage of city dwellers lack access to clean water and detergents for frequent hand washing which are essential preventative measures against some of these epidemics, as typically advised by the World Health Organization. More than half of the region’s urban residents reside in slums or informal housing, which are known for their unhygienic and crowded conditions.
6.3. Large Households
Multigenerational households are more common in the African population than in most other continents, with an average household size of 6.9 people [42]. Such living arrangements where children and working adults reside in proximity can potentially elevate the risk of close-contact infections and the spread of epidemics, particularly among the most vulnerable and the elderly population.
6.4. Cultural Beliefs and Behavioral Practices
High-risk practices related to following ancestral funeral and burial ceremonies have been identified as the cause of significant spikes in newly re-emerging epidemic cases. However, funeral and burial customs in West Africa have been identified by medical anthropologists as unusually high-risk vectors of infectious illnesses. Examples of such traditions include the bathing of bodies, or anointing others with rinsed water from the washing of corpses (often extremely contagious corpses).
The recent outbreaks of COVID-19 and monkeypox have introduced the “new normal”, which has provided social and psychological burden and adversely affected social solidarity. The status of harmonious and closely knit community-based relationships in small groups where individuals disregard hygiene, as people in the rural areas would otherwise do, can be used to assess the psychosocial effects of epidemics on the rural inhabitants of Africa as noted [43]. This social solidarity stresses the interdependence between individuals in a community and allows individuals to feel that they can enhance the lives of others [44].
The current situation demonstrates that while some of the behaviors observed during the peak of the pandemic have been largely preserved, others have been only partially adhered to or have been completely abandoned. One hygienic measure that is reported to be consistently maintained in daily activities and human interactions is the habit of handwashing. In contrast to the previous practice in the pre-Ebola and pre-COVID-19 era where people consumed fruits without washing them, individuals now consciously and regularly wash their hands after most interactions involving physical contact with others (e.g., handshakes), touching surfaces like handrails, elevator buttons, tools, doorknobs, and mobile devices, and even before eating. The anomaly in this behavioral adaptation, however, lies in the ineffectiveness of not washing the hands with detergents to thoroughly rinse away any gum traces that have penetrated deeply into the hand, as well as the abandonment of public washing areas that had previously been established during the peak of the COVID-19 pandemic at specific public institutions like places of worship, schools, and government offices.
In the area of respiratory hygiene, it is observed that the habits developed at the height of epidemics are mostly not practiced, as evidenced by the failure to use an elbow or disposable material when sneezing, coughing, or washing one’s hands, and wearing face masks only when required as a condition of receiving specific community services or access. People converge in social gatherings and events like town hall meetings, ceremonies, and business centers without worrying about the virus spreading quickly within the community because of the recommended minimum 2 cm physical distancing gap. This factor of not managing close-contact relationships has always contributed to the re-emerging secondary crisis seen during outbreaks. On self-isolation, people are seen to disregard signs of suspicion of any possible symptoms, preferring instead to self-administer local herb mixtures that could relieve symptoms and make them feel better. Data and information gathered on those who were infected, tested for, and treated have been significantly affected by this since most rural residents rely on their own daily wages and businesses. In such a situation, a government-enforced order would not stand because these residents do not receive social assistance or government benefits. For instance, most citizens experienced the hardships associated with food insecurity, unemployment, and poverty during the COVID-19 pandemic lockdown order [45]. This is because approximately 9 in 10 rural and urban workers in Africa rely on the informal sector for their daily income and wages [46].
7. Addiction Tendencies and the Risk of Becoming Epidemic in Africa
Recent observations indicate a concerning increase in the prevalence of substance use and abuse among various demographic groups within the African population. Different types of substances are being used, and dependence on these substances has become so strong that many individuals struggle to maintain their regular behavior and mental well-being when they attempt to discontinue use. The subsequent impact on their mental health, cardiovascular health, renal health, and eventual death when taken in an overdose is a cause for concern. In recent research conducted in Africa, the prevalence of substance use disorders is among the leading factors contributing to disability-adjusted life years [47]. According to one report [48], some substances that are abused are responsible for 1 in 10 cases of the spread of hepatitis C, endocarditis, and cellulitis in addition to creating intoxication, which impairs judgment. In addition, Eluwa and colleagues [49] reported that the citizens in 48 out of Africa’s 54 nations had acknowledged opioid use as an HIV risk factor. As a result of the long-term negative effects of these abused substances, Africa is currently home to a sizable population of mentally disturbed youths and mentally ill people who can be seen on nearly every street in city centers. Because most of these drugs were prescribed for clinical case management, but are increasingly being used for non-medical purposes, it is clear why there has been an increase in drug abuse. According to a study [50], many young people on the African continent are increasingly “getting high” on a variety of unorthodox substances, including smoking animal dung and sniffing fermented sewage with resultant serious negative health effects. Since most of these substances are readily available, young people from all socioeconomic groups and genders use them, including heroin, cannabis, cocaine, marijuana, and opioids, even though the UN’s drug agency believes that in 2016 there were 1.8 million cocaine users and more than 34 million cannabis users in West and Central Africa, as noted [50]. In a different study [51], the total prevalence of teenage substance use in sub-Saharan Africa was assessed to be 41.6%. For instance, 13.2% of pregnant adolescents (aged 14 to 18) in Kenya were found to have an alcohol use disorder [52]. In Uganda, 60–71% of school-age youth (12–24 years) use addictive substances, with alcohol accounting for the highest percentage (19.3%), according to a study [53].
Efforts to combat these substance addiction issues have not proven successful, primarily due to the failure to address the underlying causes and risk factors. Some of these risk factors arise from the inadequate management culture common among many African leaders resulting in the absence of a conducive environment and essential infrastructure necessary to alleviate widespread poverty and foster creativity. Consequently, many young people divert their attention to coping with their anxieties in what they perceive as a struggling continent. A drastic change in the lifestyle of most individuals due to the lockdown experience coupled with the resultant economic difficulties it brought on an already challenged populace has contributed to this overdependence on substances, as noted by [54,55]. The growing epidemic concern about these substances has been significantly exacerbated by accessibility. In a previous study on the use of psychoactive substances and risk factors, Vidona et al. [56] observed that the accessibility of these substances, psychological factors such as the desire to feel high and relieve stress, and parental influence were very responsible for the indulgence, especially students in these substances. It is noteworthy that only a few African states have passed laws governing the inspection and regulation of products crossing borders, but these policies have also encountered numerous obstacles due to dishonest government officials and organizations. A few nations in the African sub-region, including Kenya, Tanzania, and Mauritius, have begun to investigate treatment options for specific misused substances [57,58,59].
8. Study Strengths and Limitations
This study has provided a detailed evaluation of several literature and data sources such as epidemiological studies, population-based studies, and international public health databases and dashboards with particular interest in the African sub-region. The narrative review has focused on the epidemiology, responses, and the resultant risk associated with epidemics within the African context, and epidemiological evidence highlights the current epidemic trends in the WHO African region. This narrative review puts emphasis on the call for a review of actions/responses to avoid the almost endemic infectious state plaguing the African population, which is a major public health concern. It must be stated that public health issues are a routine challenge with emerging and re-emerging disease outbreaks persistent in Africa, hence the narrative review has contributed to the recent advancements that have been made in this field. However, this study has a limitation due to the lack of a detailed systematic review which would have minimized publication selection bias, thereby improving the interpretation and conclusions.
9. Conclusions
In the past few decades, epidemic outbreaks and disease occurrences have become more frequent and widespread in Africa, posing challenges for poor countries and impacting vulnerable populations. The recent epidemiological data from this study demonstrates that the WHO African region continues to face a growing risk of epidemic disease outbreaks such as monkeypox, Ebola viral disease, measles, cholera, Dengue fever, Lassa fever, and other viral hemorrhagic fevers. Several factors, including limited resources, poor epidemic response strategies, inadequate healthcare infrastructure, socio-economic inequalities, malnutrition, cultural norms, mass gatherings, and lack of proper sanitation and hygiene contribute to Africa’s high burden of epidemics and infectious diseases. Providing effective preventive measures such as regional disease surveillance, early mitigation strategies, cultural and behavioral changes, contact tracing, and personal protective measures will help reduce the human, material, and economic losses attributed to epidemic outbreaks in the region. This study further highlights the importance of reviewing and adapting strategies to the cultural context and involving local communities in designing and implementing these preventive measures. Attention should also be paid to drugs and substance abuse with its associated mental health and psychosocial issues which is becoming common among young people in Africa. In addition, more regional-focused research is urgently needed to identify the environmental, socio-economic, and cultural factors that promote the emergence and transmission of epidemic diseases in the African population.
Author Contributions
Conceptualization, W.B.V. and C.W.-V.; methodology, W.B.V., C.W.-V., L.K.D., B.M.A., J.N.P., and U.A.E.; software, W.B.V. and U.A.E.; validation, W.B.V., C.W.-V. and U.A.E.; formal analysis, W.B.V. and U.A.E.; investigation, W.B.V., C.W.-V., L.K.D., B.M.A., J.N.P. and U.A.E.; resources, W.B.V. and C.W.-V.; data curation, W.B.V., C.W.-V. and U.A.E.; writing—original draft preparation, W.B.V., C.W.-V., L.K.D., B.M.A. and J.N.P.; writing—review and editing, W.B.V., C.W.-V. and U.A.E.; supervision, W.B.V. and U.A.E.; project administration, W.B.V. and C.W.-V. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Hopman, J.; Allegranzi, B.; Mehtar, S. Managing COVID-19 in low- and middle-income countries. J. Am. Med. Assoc. 2020, 323, 1549–1550. [Google Scholar] [CrossRef]
- World Bank. Summary on the Ebola Recovery Plan: Sierra Leone External Icon; World Bank: Washington, DC, USA, 2015. [Google Scholar]
- Madhav, N.; Oppenheim, B.; Gallivan, M.; Mulembakani, P.; Rubin, E.; Wolfe, N. Pandemics: Risks, Impacts, and Mitigation. In Disease Control Priorities: Improving Health and Reducing Poverty, 3rd ed.; Jamison, D.T., Gelband, H., Horton, S., Eds.; International Bank for Reconstruction and Development/The World Bank: Washington, DC, USA, 2017. Available online: https://www.ncbi.nlm.nih.gov/books/NBK525302/ (accessed on 5 December 2023).
- WHO. African Region. In Animal-to-Human Diseases on the Rise in Africa, Warns UN Health Agency; WHO: Geneva, Switzerland, 2022. [Google Scholar]
- Africa Centre for Disease Control and Prevention. Africa CDC Epidemic Intelligence Report, Africa CDC. 2024. Available online: https://africacdc.org/download/africa-cdc-weekly-event-based-surveillance-report-march-2024/ (accessed on 19 July 2024).
- Ohimain, E.I.; Silas-Olu, D. The 2013–2016 Ebola virus disease outbreak in West Africa. Curr. Opin. Pharmacol. 2021, 60, 360–365. [Google Scholar] [CrossRef] [PubMed]
- Bosa, H.K.; Kamara, N.; Aragaw, M.; Wayengera, M.; Talisuna, A.; Bangura, J.; Mwebesa, H.G.; Katoto, P.D.; Agyarko, R.K.; Ihekweazu, C.; et al. The west Africa Ebola virus disease outbreak: 10 years on. Lancet Glob. Health 2024, 12, e1081–e1083. [Google Scholar] [CrossRef]
- Onyekuru, N.A.; Ihemezie, E.J.; Ezea, C.P.; Apeh, C.C.; Onyekuru, B.O. Impacts of Ebola disease outbreak in West Africa: Implications for government and public health preparedness and lessons from COVID-19. Sci. Afr. 2023, 19, e01513. [Google Scholar] [CrossRef]
- Nyaruaba, R.; Okoye, C.O.; Akan, O.D.; Mwaliko, C.; Ebido, C.C.; Ayoola, A.; Ayeni, E.A.; Odoh, C.K.; Abi, M.E.; Adebanjo, O.; et al. Socio-economic impacts of emerging infectious diseases in Africa. Infect. Dis. 2022, 54, 315–324. [Google Scholar] [CrossRef] [PubMed]
- US Centers for Disease Control and Prevention. History of Ebola Disease Outbreaks. 2024. Available online: https://www.cdc.gov/ebola/outbreaks/ (accessed on 19 July 2024).
- Guetiya Wadoum, R.E.; Sevalie, S.; Minutolo, A.; Clarke, A.; Russo, G.; Colizzi, V.; Mattei, M.; Montesano, C. The 2018–2020 Ebola outbreak in the Democratic Republic of Congo: A better response had been achieved through inter-state coordination in Africa. Risk Manag. Healthc. Policy 2021, 14, 4923–4930. [Google Scholar] [CrossRef] [PubMed]
- Ndembi, N.; Aluso, A.; Habtemariam, M.K. African leadership is critical in responding to public health threats. Nat. Commun. 2024, 15, 877. [Google Scholar] [CrossRef]
- World Health Organisation, WHO. Surveillance, Case Investigation and Contact Tracing for Mpox (Monkeypox): Interim Guidance, 20 March 2024. Reference Number: WHO/MPX/Surveillance/2024.1. WHO, 2024. Available online: https://www.who.int/publications/i/item/WHO-MPX-Surveillance-2024.1 (accessed on 19 July 2024).
- Africa Centre for Disease Control and Prevention. Outbreak Brief 23: Mpox in Africa Union Member States. Africa CDC, 2022. Available online: https://africacdc.org/disease-outbreak/outbreak-brief-23-mpox-in-africa-union-member-states/ (accessed on 19 July 2024).
- World Health Organization. 2022–2024 Mpox Outbreak: Global Trends; WHO: Geneva, Switzerland, 2024; Available online: https://worldhealthorg.shinyapps.io/mpx_global/ (accessed on 19 July 2024).
- Wan, Y.; Shang, J.; Graham, R.; Baric, R.S.; Li, F. Receptor recognition by the novel coronavirus from Wuhan: An analysis based on decade-long structural studies of SARS coronavirus. J. Virol. 2020, 94, e00127-20. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020; WHO: Geneva, Switzerland. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 19 July 2024).
- World Health Organization. WHO Dashboard for COVID-19; WHO Health Emergencies Programme, WHO: Geneva, Switzerland, 2024. Available online: https://data.who.int/dashboards/covid19/cases?n=c (accessed on 19 July 2024).
- Cutler, D.M.; Summers, L.H. The COVID-19 pandemic and the $16 trillion virus. JAMA 2020, 324, 1495–1496. [Google Scholar] [CrossRef]
- Farayibi, A.; Asongu, S. The economic consequences of the COVID-19 pandemic in Nigeria; AGDI Working Paper, No. WP/20/042. African Governance and Development Institute (AGDI): Yaoundé, Cameroon, 2020. Available online: http://hdl.handle.net/10419/228019 (accessed on 19 July 2024).
- Oyejobi, G.K.; Olaniyan, S.O.; Awopetu, M.J. COVID-19 in Nigeria: Matters arising. Curr. Med. Issues 2020, 18, 210–212. [Google Scholar] [CrossRef]
- Moyo, E.; Mhango, M.; Moyo, P.; Dzinamarira, T.; Chitungo, I.; Murewanhema, G. Emerging infectious disease outbreaks in Sub-Saharan Africa: Learning from the past and present to be better prepared for future outbreaks. Front. Public Health 2023, 11, 1049986. [Google Scholar] [CrossRef] [PubMed]
- Martinez, M.E. The calendar of epidemics: Seasonal cycles of infectious diseases. PLoS Pathog. 2018, 14, e1007327. [Google Scholar] [CrossRef]
- Kelsey, J.L.; Thompson, W.D.; Evans, A.S. Methods in Observational Epidemiology; Oxford University Press: New York, NY, USA, 1986; Volume 216. [Google Scholar]
- Stawicki, S.P.; Jeanmonod, R.; Miller, A.C.; Paladino, L.; Gaieski, D.F.; Yaffee, A.Q. The 2019–2020 Novel Corona-virus (Severe Acute Respiratory Syndrome Coronavirus 2) Pandemic: A Joint American College of Academic International Medicine-World Academic Council of Emergency Medicine Multidisciplinary COVID-19 Working Group Consensus Paper. J. Glob. Infect. Dis. 2020, 12, 47–93. [Google Scholar] [CrossRef]
- Studdert, V.P.; Gay, C.C.; Charles Blood, D.C. (Eds.) Transmission. In Saunders Comprehensive Veterinary Dictionary, 4th ed.; Elsevier Health Sciences: Philadelphia, PA, USA, 2012; ISBN 978-0-7020-3231-8. [Google Scholar]
- David, E.; Eric, W. What a Population’s Age Structure Means for COVID-19’s Impact in Low-Income Countries. Center for Global Development, 2020. Available online: https://www.cgdev.org/blog/what-populations-age-structure-means-covid-19s-impact-low-income-countries (accessed on 7 December 2023).
- Thakur, S.; Dharavath, R. Artificial neural network based prediction of malaria abundances using big data: A knowledge capturing approach. Clin. Epidemiol. Glob. Health 2019, 7, 121–126. [Google Scholar] [CrossRef]
- Darkoh, E.; Larbi, J.A.; Lawer, E.A. A Weather-Based Prediction Model of Malaria Prevalence in Amenfi West District, Ghana. Malar. Res. Treat. 2017, 2017, 7820454. [Google Scholar] [CrossRef]
- Sarkar, B.K.; Sana, S.S. An e-healthcare system for disease prediction using hybrid data mining technique. J. Model. Manag. 2019, 14, 628–661. [Google Scholar] [CrossRef]
- Baldominos, A.; Puello, A.; Ogul, H.; Asuroglu, T.; Colomo-Palacios, R. Predicting Infections Using Computational Intelligence—A Systematic Review. IEEE Access 2000, 8, 31083–31102. [Google Scholar] [CrossRef]
- WHO. Coronavirus Disease (COVID-19) Advice for the Public. 2019. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public (accessed on 19 July 2024).
- Semaan, A.; Audet, C.; Huysmans, E. Voices from the frontline: Findings from a thematic analysis of a rapid online global survey of maternal and newborn health professionals facing the COVID-19 pandemic. BMJ Glob. Health 2020, 5, 520093393. [Google Scholar] [CrossRef]
- Wood, G. Think 168,000 ventilators is too few? Try three. Atlantic 2020, 6, 434–436. [Google Scholar]
- Dahab, M.; Van Zandvoort, K.; Flasche, S.; Warsame, A.; Spiegel, P.; Waldman, R.J.; Ratnayake, R.; Favas, C.; Checchi, F. COVID-19 control in low-income settings and displaced populations: What can realistically be done? Long Sch. Hyg. Trop. Med. 2020, 14, 54. [Google Scholar] [CrossRef]
- United Nations News. COVID-19: Impact Could Cause Equivalent of 195 Million Job Losses, Says ILO Chief. UN News. 2020. Available online: https://news.un.org/en/story/2020/04/1061322 (accessed on 19 July 2024).
- Roberts, L. Polio, Measles, Other Diseases Set to Surge as COVID-19 Forces Suspension of Vaccination Campaigns |Science|; AAAS: Washington, DC, USA, 2020. [Google Scholar]
- Abramowitz, S.A.; McLean, K.E.; McKune, S.L.; Bardosh, K.L.; Fallah, M.; Monger, J.; Tehoungue, K.; Omidian, P.A. Community-centered responses to Ebola in urban Liberia: The view from below. PLoS Negl. Trop. Dis. 2015, 9, e0003706. [Google Scholar] [CrossRef]
- Van Zandvoort, K.; Jarvis, C.I.; Pearson, C.A.B.; Davies, G.N.; Ratnayake, R.; Russell, W.T.; Kucharski, J.A.; Jit, M.; Flasche, S.; Eggo, M.R.; et al. Response strategies for COVID-19 epidemics in African settings: A mathematical modelling study. BMC Med. 2020, 18, 324. [Google Scholar] [CrossRef] [PubMed]
- Toshiko, K.; Lori, S.A. Sub-Saharan Africa’s Demographic and Health Characteristics Will Influence the Course of the COVID-19 Pandemic; Population Reference Bureau: Washington, DC, USA, 2000. [Google Scholar]
- Jamal, S. Urbanization in Sub-Saharan Africa. Center for Strategic International Studies, 2018. Available online: https://www.csis.org/analysis/urbanization-sub-saharan-africa (accessed on 5 December 2023).
- Pew Research Center (PRC). Religion and Living Arrangements around the World. 2019. Available online: https://www.pewforum.org/2019/12/12/religion-and-living-arrangements-around-the-world (accessed on 5 December 2023).
- Igwe, P.A.; Ochinanwata, C.; Ochinanwata, N.; Adeyeye, J.O.; Ikpor, I.M.; Nwakpu, S.E.; Egbo, O.P.; Onyishi, I.E.; Vincent, O.; Nwekpa, K.C.; et al. Solidarity and Social Behavior: How did this help communities to manage COVID-19 pandemic? Int. J. Sociol. Soc. Policy 2020, 40, 1183–1200. [Google Scholar] [CrossRef]
- Douwes, R.; Stuttaford, M.; London, L. Social Solidarity, Human Rights, and Collective Action: Considerations in the Implementation of the National Health Insurance in South Africa. Health Hum. Rights 2018, 20, 185–196. [Google Scholar]
- Vincent, O. COVID-19: Compelling Case for Withdrawal from Employees’ RSA. 2020. Available online: https://businessday.ng/opinion/article/covid-19-compelling-case-for-withdrawal-from-employees-rsa/ (accessed on 10 November 2023).
- African Development Bank, AfDB. Recognizing Africa’s Informal Sector. 2023. Available online: https://blogs.afdb.org/afdb-championing-inclusive-growth-across-africa/post/recognizing-africas-informal-sector-11645 (accessed on 10 June 2020).
- Charlson, F.J.; Diminic, S.; Lund, C.; Degenhardt, L.; Whiteford, H.A. Mental and substance use disorders in Sub-Saharan Africa: Predictions of epidemiological changes and mental health workforce requirements for the next 40 years. PLoS ONE 2014, 9, e110208. [Google Scholar] [CrossRef]
- Cone, E.J.; Bigelow, G.E.; Herrmann, E.S.; Mitchell, M.J.; LoDico, C.; Flegel, R.; Vandrey, R. Non-smoker exposure to secondhand cannabis smoke. I. Urine screening and confirmation results. J. Anal. Toxicol. 2015, 39, 1–12. [Google Scholar] [CrossRef]
- Eluwa, G.I.; Strathdee, S.A.; Adebayo, S.B.; Ahonsi, B.; Adebajo, S.B. A profile on HIV prevalence and risk behaviors among injecting drug users in Nigeria: Should we be alarmed? Drug Alcohol Depend. 2023, 127, 5–71. [Google Scholar] [CrossRef]
- Yomi, K. Nigeria Has Become the Poverty Capital of the World. Quartz Africa Weekly Brief. 2018. Available online: https://qz.com/africa/1313380/nigerias-has-the-highest-rate-of-extreme-poverty-globally/ (accessed on 10 November 2023).
- Kaggwa, M.M.; Abaatyo, J.; Alol, E.; Muwanguzi, M.; Najjuka, S.M.; Favina, A.; Rukundo, G.Z.; Ashaba, S.; Mamun, M.A. Substance use disorder among adolescents before and during the COVID-19 pandemic in Uganda: Retrospective findings from a psychiatric ward registry. PLoS ONE 2022, 26, e0269044. [Google Scholar] [CrossRef] [PubMed]
- Olawole-Isaac, A.; Ogundipe, O.; Amoo, E.O.; Adeloye, D. Substance use among adolescents in sub-Saharan Africa: A systematic review and meta-analysis. S. Afr. J. Child. Health 2018, 12, 79–83. [Google Scholar] [CrossRef]
- Kimbui, E.; Kuria, M.; Yator, O.; Kumar, M.A. Cross-sectional study of depression with comorbid substance use de-pendency in pregnant adolescents from an informal settlement of Nairobi: Drawing implications for treatment and prevention work. Ann. Gen. Psychiatry 2018, 17, 53. [Google Scholar] [CrossRef]
- Enns, A.; Pinto, A.; Venugopal, J.; Grywacheski, V.; Gheorghe, M.; Kakkar, T.; Farmanara, N.; Deb, B.; Noon, A.; Orpana, H. Substance use and related harms in the context of COVID-19: A conceptual model. Health Promot. Chronic Dis. Prev. Can. 2020, 40, 342–349. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.Q.; Kaelber, D.C.; Xu, R.; Volkow, N.D. COVID-19 risk and outcomes in patients with substance use disorders: Analyses from electronic health records in the United States. Mol. Psychiatry 2021, 26, 30–39. [Google Scholar] [CrossRef]
- Vidona, W.B.; Wadioni, A.; Okeke, S.N.; Bodo, T. Evaluation of Psychoactive Substance use and its risk factors among Public School Students of Rivers State, Nigeria. Asian J. Pharm. Res. 2017, 7, 175–182. [Google Scholar] [CrossRef]
- Petersen, Z.; Myers, B.; Van Hout, M.C.; Pluddemann, A.; Parry, C. Availability of HIV prevention and treatment services for people who inject drugs: Findings from 21 countries. Harm Reduct. J. 2013, 10, 13. [Google Scholar] [CrossRef] [PubMed]
- Ratliff, S.A.; Mbwambo, J.K.; Lambdin, B.H.; Voets, A.; Pont, S.; Maruyama, H.; Kilonzo, G.P. An Overview of HIV Prevention Interventions for People Who Inject Drugs in Tanzania. Adv. Prev. Med. 2013, 183187. [Google Scholar] [CrossRef]
- Ndimbii, J.; Guise, A.; Ayon, S.; Kalama, M.; McLean, S.; Rhodes, T. Implementing needle and syringe programmes in Kenya: Changes, opportunities and challenges in HIV prevention. Afr. J. Drug Alcohol. Stud. 2015, 14, 95–103. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).