Periodontal Health as Perceived by Rheumatologists and Rheumatoid Arthritis Patients
Abstract
:1. Introduction
Aims and Objectives
2. Materials and Methods
2.1. Study Design and Data Collection
2.2. Subjects/Samples
2.2.1. Rheumatologists
2.2.2. Rheumatoid Arthritis Patients
2.3. Statistical Analysis
3. Results
3.1. Demographic Characteristics of Rheumatoid Arthiritis Patients
3.2. Rheumatoid Arthitis Patients’ Knowledge of Relationships between Rheumatoid Arthritis and Periodontal Disease
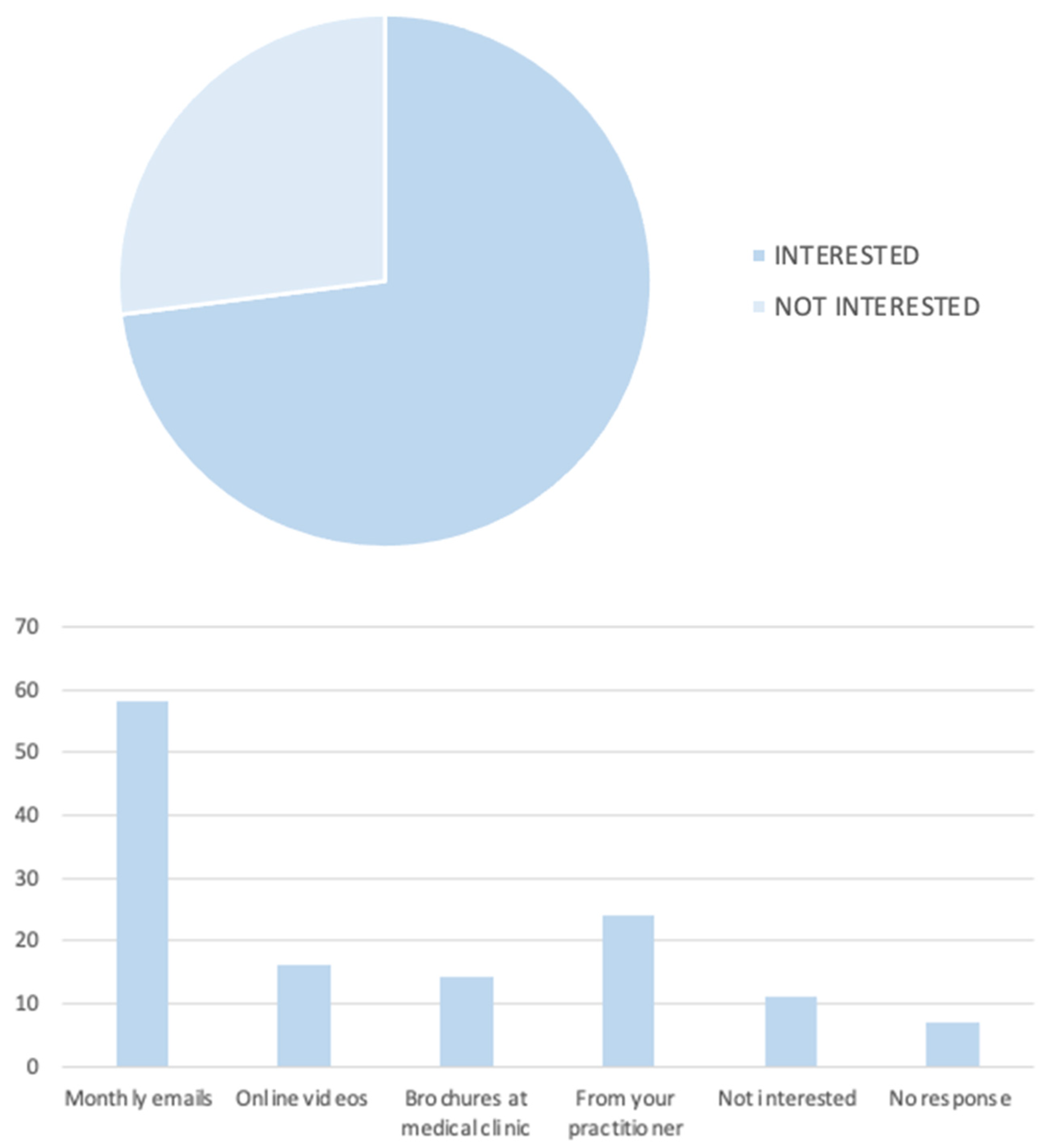
3.3. Rheumatoid Arthiritis Patients’ Attitudes and Behaviours towards Periodontal Disease
3.4. Relationships between Knowledge Regarding Oral Systemic Link and Sociodemographic Characteristics of Rheumatoid Arthritis Patients
3.5. Relationships between Attitudes and Behaviours Regarding Oral Systemic Link and Sociodemographic Characteristics of Rheumatoid Arthritis Patients
3.6. Relationships between Attitudes and Behaviours Regarding Oral Systemic Link and Knowledge of Rheumatoid Arthritis Patients
3.7. Demographic Characteristics of Rheumatologists
3.8. Rheumatologists’ Knowledge of Relationships between Rheumatoid Arthritis and Periodontal Disease
3.9. Rheumatologists’ Attitudes and Behaviours towards Periodontal Disease
3.10. Relationships between Knowledge Regarding Oral Systemic Link and Sociodemographic Characteristics of Rheumatologists
3.11. Relationships between Attitudes and Behaviours Regarding Oral Systemic Link and Sociodemographic Characteristics of Rheumatologists
3.12. Relationships between Attitudes and Behaviours Regarding Oral Systemic Link and Knowledge of Rheumatologists
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- McInnes, I.B.; Schett, G. The pathogenesis of rheumatoid arthritis. N. Engl. J. Med. 2011, 365, 2205–2219. [Google Scholar] [CrossRef] [PubMed]
- Rosenstein, E.D.; Greenwald, R.A.; Kushner, L.J.; Weissmann, G. Hypothesis: The humoral immune response to oral bacteria provides a stimulus for the development of rheumatoid arthritis. Inflammation 2004, 28, 311–318. [Google Scholar] [CrossRef] [PubMed]
- Ha, D.H.; John Spencer, A.; Ju, X.; Do, L.G. Periodontal diseases in the Australian adult population. Aust. Dent. J. 2020, 65 (Suppl. S1), S52–S58. [Google Scholar] [CrossRef] [PubMed]
- Protudjer, J.L.P.; Billedeau, C.; Hurst, K.; Schroth, R.; Stavropoulou, C.; Kelekis-Cholakis, A.; Hitchon, C.A. Oral Health in Rheumatoid Arthritis: Listening to Patients. JDR Clin. Trans. Res. 2022, 7, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Alexia, V.; Chloé, V.; Pierre, B.; Sara, L.D. Periodontal Diseases and Systemic Disorders: What Do Our Doctors Know? A General Practitioner’s Survey Conducted in Southern France. J. Evid. Based Dent. Pract. 2017, 17, 361–369. [Google Scholar] [CrossRef] [PubMed]
- Dubar, M.; Delatre, V.; Moutier, C.; Sy, K.; Agossa, K. Awareness and practices of general practitioners towards the oral-systemic disease relationship: A regionwide survey in France. J. Eval. Clin. Pract. 2019, 26, 1722–1730. [Google Scholar] [CrossRef] [PubMed]
- Serban, S.; Dietrich, T.; Lopez-Oliva, I.; de Pablo, P.; Raza, K.; Filer, A.; Chapple, I.L.C.; Hill, K. Attitudes towards Oral Health in Patients with Rheumatoid Arthritis: A Qualitative Study Nested within a Randomized Controlled Trial. JDR Clin. Trans. Res. 2019, 4, 360–370. [Google Scholar] [CrossRef] [PubMed]
- Mühlberg, S.; Jäger, J.; Krohn-Grimberghe, B.; Patschan, S.; Mausberg, R.F.; Schmalz, G.; Haak, R.; Ziebolz, D. Oral health-related quality of life depending on oral health in patients with rheumatoid arthritis. Clin. Oral. Investig. 2017, 21, 2661–2670. [Google Scholar] [CrossRef] [PubMed]

| Rheumatoid Patients | Rheumatologists | ||||
|---|---|---|---|---|---|
| Variables | n | % | Variables | n | % |
| Demographic Information | Demographic Information | ||||
| Gender | Gender | ||||
| Female | 72 | 94.74 | Female | 1 | 14.3 |
| Male | 3 | 3.95 | Male | 5 | 71.4 |
| Other/Not specified | 0 | 0 | Other/Not specified | 1 | 14.3 |
| Age, y | Age, y | ||||
| 21–30 | 3 | 3.95 | 21–30 | 0 | 0 |
| 31–40 | 3 | 3.95 | 31–40 | 0 | 0 |
| 41–50 | 6 | 7.89 | 41–50 | 3 | 42.9 |
| 51–60 | 22 | 28.95 | 51–60 | 0 | 0 |
| 61–70 | 17 | 22.37 | 61–70 | 1 | 14.3 |
| >70 | 17 | 22.37 | >70 | 3 | 42.9 |
| Identity | Identity | ||||
| Caucasian | 72 | 94.74 | Caucasian | 3 | 42.9 |
| Aboriginal or Torres Strait Islander | 0 | 0 | Aboriginal or Torres Strait Islander | 0 | 0 |
| Asian | 0 | 0 | Asian | 4 | 57.1 |
| Other | 3 | 3.95 | Other | 0 | 0 |
| Marital Status | Professional Career | ||||
| Never married | 19 | 25 | Years practising | ||
| Married | 37 | 48.68 | <5 | 0 | 0 |
| Separated | 5 | 6.58 | 6–10 | 3 | 42.9 |
| Divorced | 9 | 11.84 | >10 | 4 | 57.1 |
| Widowed | 5 | 6.58 | Up to date with literature | ||
| Highest level of education | Yes | 7 | 100 | ||
| Less than high school | 3 | 3.95 | No | 0 | 0 |
| Highschool graduate | 17 | 22.37 | |||
| TAFE or diploma | 24 | 31.58 | |||
| Undergraduate degree | 10 | 13.16 | |||
| Postgraduate degree | 10 | 13.16 | |||
| Masters degree | 10 | 13.16 | |||
| Doctorate | 1 | 1.32 | |||
| Current employment status | |||||
| Full time | 18 | 23.68 | |||
| Part time | 15 | 19.74 | |||
| Not working due to disability | 7 | 9.21 | |||
| Retired | 29 | 38.16 | |||
| Unemployed and not looking for work | 2 | 2.63 | |||
| Unemployed and looking for work | 1 | 1.32 | |||
| Student | 3 | 3.95 | |||
| Rheumatoid Arthritis | |||||
| Length of diagnosis, y | |||||
| <1 | 6 | 7.89 | |||
| 1–5 | 20 | 26.32 | |||
| 6–10 | 10 | 13.16 | |||
| >10 | 32 | 42.11 | |||
| Type of RA known | |||||
| Yes | 32 | 42.11 | |||
| No | 37 | 48.68 | |||
| Periodontal disease | |||||
| Yes | 14 | 18.42 | |||
| No | 51 | 67.11 | |||
| Rheumatoid Patients | ||
| Variables | n | % |
| Knows there is a Link between oral and systemic diseases | ||
| Yes | 33 | 43.42 |
| No | 43 | 56.58 |
| Experiences one or more signs of periodontal disease | ||
| Yes | 45 | 59.21 |
| No | 31 | 40.79 |
| Knows they are more susceptible to poor dental health | ||
| Yes | 33 | 43.42 |
| No | 43 | 56.58 |
| Knows that oral hygiene can impact rheumatoid arthritis | ||
| Yes | 16 | 21.05 |
| No | 60 | 78.95 |
| Rheumatologist’s | ||
| Variables | n | % |
| Good oral health is important to overall health? | ||
| Strongly agree | 6 | 85.7 |
| Agree | 1 | 14.3 |
| Neutral | 0 | 0 |
| Disagree | 0 | 0 |
| Strongly disagree | 0 | 0 |
| No response | 1 | 0 |
| Oral disease (periodontal disease) can be linked to systemic disease and vice versa | ||
| Strongly agree | 2 | 28.6 |
| Agree | 3 | 42.9 |
| Neutral | 2 | 28.6 |
| Disagree | 0 | 0 |
| Strongly disagree | 0 | 0 |
| No response | 1 | 0 |
| Patients with rheumatoid arthritis are at an increased risk of severe periodontal disease | ||
| Strongly agree | 2 | 28.6 |
| Agree | 5 | 71.4 |
| Neutral | 0 | 0 |
| Disagree | 0 | 0 |
| Strongly Disagree | 0 | |
| No response | 1 | 0 |
| Rheumatoid Patients | ||
| Variables | n | % |
| How often attends the dentist (65 responses) | ||
| Never | 1 | 1.54 |
| Only when a problem arises | 17 | 26.15 |
| 1–2 times per year | 27 | 41.54 |
| >2 times per year | 20 | 30.78 |
| Receiving treatment for periodontal disease (65 responses) | ||
| Yes | 16 | 24.62 |
| No | 49 | 75.38 |
| Importance of maintaining good oral hygiene (66 responses) | ||
| Not at all important | 0 | 0 |
| Slightly-moderately important | 12 | 18.18 |
| Very-extremely important | 54 | 81.82 |
| Rheumatologist’s | ||
| Variables | n | % |
| How often do you ask about your patient’s oral hygiene or oral health status | ||
| Always | 1 | 14.3 |
| Most of the time | 0 | 0 |
| About half the time | 0 | 0 |
| Sometimes | 5 | 71.4 |
| Never | 1 | 14.3 |
| No response | 0 | 0 |
| How often do you perform an oral exam on your patients? | ||
| Always | 1 | 14.3 |
| Most of the time | 0 | 0 |
| About half the time | 0 | 0 |
| Sometimes | 3 | 42.9 |
| Never | 3 | 42.9 |
| No response | 1 | 0 |
| How often do you refer your patients to a dental specialist | ||
| Always | 0 | 0 |
| Most of the time | 0 | 0 |
| About half of the time | 1 | 14.3 |
| Sometimes | 6 | 85.7 |
| Never | 0 | 0 |
| No response | 1 | 0 |
| Sociodemographics | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gender | Age | Highest Level of Education | Employment Status | Length of RA Diagnosis | Type of RA Diagnosis | |||||||||||||||
| Female | Male | p-Value | £40 | 40–60 | >60 | p-Value | High School or Less | Undergraduate Qualification | Postgraduate Qualification | p-Value | Employed or Retired | Unemployed or Student | p-Value | 0–5 Years | >5 Years | p-Value | Known | Unknown | p-Value | |
| Knowledge | ||||||||||||||||||||
| Link between oral and systemic diseases | 33 (46) | 0 | 0.2508 | 4 (67) | 13 (46) | 15 (47) | 0.6457 | 8 (38) | 15 (44) | 10 (50) | 0.4410 | 27 (44) | 6 (46) | 0.8634 | 11 (42) | 20 (48) | 0.6691 | 19 (59) | 13 (35) | 0.0441 |
| Experience one or more signs of periodontal disease | 44 (61) | 1 (33) | 0.5602 | 3 (50) | 17 (61) | 19 (59) | 0.8884 | 11 (52) | 23 (68) | 11 (55) | 0.6383 | 36 (58) | 9 (69) | 0.4549 | 13 (50) | 31 (74) | 0.0459 | 20 (63) | 24 (65) | 0.8285 |
| Susceptibility for poor dental health due to existing rheumatoid arthritis condition | 33 (46) | 0 | 0.2562 | 4 (67) | 12 (43) | 14 (44) | 0.5481 | 8 (38) | 15 (44) | 10 (50) | 0.2959 | 25 (40) | 7 (54) | 0.3701 | 11 (42) | 20 (48) | 0.6691 | 17 (53) | 15 (41) | 0.2959 |
| Oral hygiene impact on rheumatoid arthritis | 16 (22) | 0 | 1 | 1 (17) | 5 (18) | 9 (21) | 0.5962 | 3 (14) | 9 (26) | 4 (20) | 0.2661 | 14 (23) | 2 (15) | 0.5647 | 2 (50) | 13 (31) | 0.1515 | 6 (19) | 10 (27) | 0.4166 |
| Attitudes & Behaviours | ||||||||||||||||||||
| Attends dentist regularly | 46 (64) | 1 (33) | 0.2837 | 3 (50) | 16 (57) | 23 (72) | 0.3808 | 12 (60) | 22 (65) | 13 (62) | 0.9387 | 43 (69) | 4 (31) | 0.0089 | 15 (58) | 30 (71) | 0.2446 | 22 (69) | 25 (68) | 0.9163 |
| Receiving treatment for periodontal disease | 16 (22) | 0 | 1 | 1 (17) | 4 (14) | 6 (19) | 0.8983 | 3 (15) | 9 (26) | 4 (19) | 0.5833 | 15 (24) | 1 (8) | 0.1867 | 3 (12) | 12 (29) | 0.0997 | 5 (16) | 11 (30) | 0.1662 |
| Importance of maintaining good oral hygiene | 51 (71) | 2 (67) | 0.8766 | 2 (33) | 21 (75) | 24 (75) | 0.0993 | 14 (70) | 23 (68) | 9 (43) | 0.1208 | 48 (77) | 6 (46) | 0.0224 | 19 (73) | 34 (81) | 0.4466 | 27 (84) | 27 (73) | 0.2522 |
| Attitudes & Behaviours | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Dentist Attendance | Receiving Periodontal Treatment | Oral Health Importance to Patient | |||||||
| Regularly >1–2 Times/Year (47) | Never/Only When There Is a Problem (18) | p-Value | Yes (16) | No (49) | p-Value | Extremely/Very Important (54) | Moderately/Not at All Important (12) | p-Value | |
| Knowledge | |||||||||
| Link between oral and systemic diseases | 27 (57) | 6 (33) | 0.0818 | 8 (50) | 25 (51) | 0.9435 | 40 (74) | 8 (67) | 0.6022 |
| Experience one or more signs of periodontal disease | 30 (64) | 13 (72) | 0.5222 | 14 (88) | 30 (61) | 0.0510 | 35 (65) | 9 (75) | 0.4984 |
| Susceptibility for poor dental health due to existing rheumatoid arthritis condition | 24 (51) | 9 (50) | 0.9388 | 9 (56) | 24 (49) | 0.6135 | 26 (48) | 7 (58) | 0.5232 |
| Oral hygiene impact on rheumatoid arthritis | 13 (28) | 3 (17) | 0.3572 | 7 (44) | 9 (18) | 0.0407 | ‘13 (24) | 3 (25) | 0.9460 |
| Sociodemographic | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Gender | Age | Years Practicing | |||||||
| Male (5) | Female (1) | p Value | <60 (3) | 60+ (4) | p Value | 6–10 (3) | 10+ (4) | p Value | |
| Knowledge | |||||||||
| Is good oral health important to overall health? | 5 (100) | 1 (100) | 1 | 3 (100) | 4 (100) | 1 | 3 (100) | 4 (100) | 1 |
| Oral disease (periodontal disease) can be linked to systemic disease and vice versa | 4 (80) | 0 | 0.33 | 3 (100) | 2 (50) | 0.4286 | 3 (100) | 2 (50) | 0.4286 |
| Patients with rheumatoid arthritis are at an increased risk of severe periodontal disease | 5 (100) | 1 (100) | 1 | 3 (100) | 4 (100) | 1 | 3 (100) | 4 (100) | 1 |
| Attitudes & Behavior | |||||||||
| Ask about patient’s oral hygiene or oral health status | 4 (80) | 1 (100) | 1 | 3 (100) | 3 (75) | 1 | 3 (100) | 3 (75) | 1 |
| Perform an oral exam on their patients | 2 (40) | 1 (100) | 1 | 2 (67) | 2 (50) | 1 | 2 (67) | 2 (50) | 1 |
| Refers patients to a dental specialist | 5 (100) | 1 (100) | 1 | 3 (100) | 4 (100) | 1 | 3 (100) | 4 (100) | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Proud, N.; Hughes, G.; McCashney, C.; Algarves Miranda, L. Periodontal Health as Perceived by Rheumatologists and Rheumatoid Arthritis Patients. Rheumato 2023, 3, 118-131. https://doi.org/10.3390/rheumato3020010
Proud N, Hughes G, McCashney C, Algarves Miranda L. Periodontal Health as Perceived by Rheumatologists and Rheumatoid Arthritis Patients. Rheumato. 2023; 3(2):118-131. https://doi.org/10.3390/rheumato3020010
Chicago/Turabian StyleProud, Natasha, Grace Hughes, Cohen McCashney, and Letícia Algarves Miranda. 2023. "Periodontal Health as Perceived by Rheumatologists and Rheumatoid Arthritis Patients" Rheumato 3, no. 2: 118-131. https://doi.org/10.3390/rheumato3020010
APA StyleProud, N., Hughes, G., McCashney, C., & Algarves Miranda, L. (2023). Periodontal Health as Perceived by Rheumatologists and Rheumatoid Arthritis Patients. Rheumato, 3(2), 118-131. https://doi.org/10.3390/rheumato3020010






