Determinants of Virological Failure in HIV Patients on Highly Active Antiretroviral Therapy (HAART): A Retrospective Cross-Sectional Study in the Upper East Region of Ghana
Abstract
:1. Introduction
2. Methods and Materials
2.1. Description of Study Setting
2.2. Study Design
2.3. Inclusion and Exclusion Criteria
2.4. Sample Size Determination
2.5. Data Collection Tools, Procedures, and Data Management
2.6. Study Variables
2.7. Data Analysis
2.8. Ethical Considerations
3. Results
3.1. Socio-Demographic Characteristics of Respondents
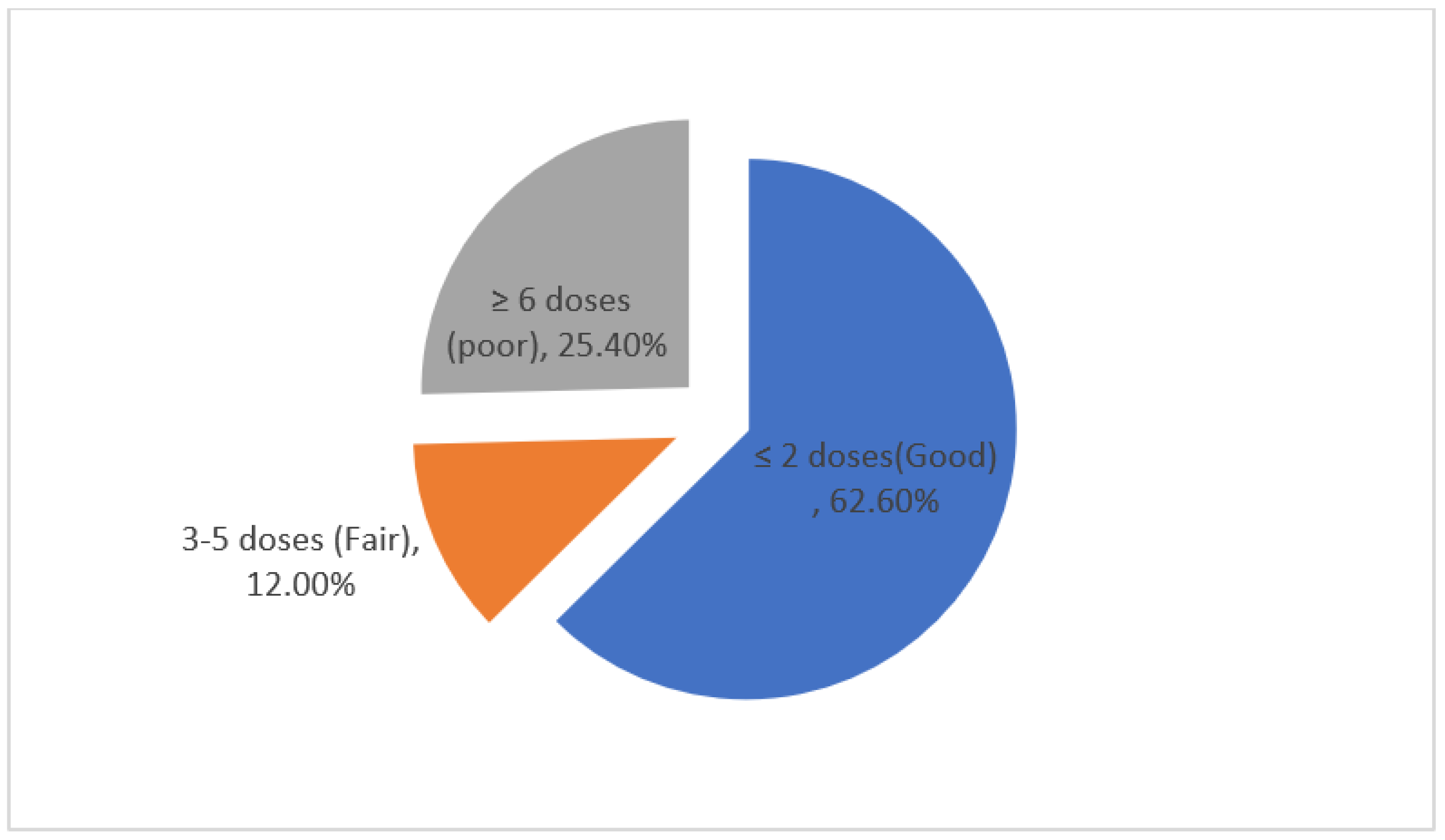
3.2. Antiretroviral Therapy Adherence
3.3. HIV Viral Load Testing of Respondents
3.4. Determinants of Viral Load Failure in HIV Patients on Antiretroviral Therapy (ART)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vlahov, D.; Galai, N.; Safaeian, M.; Galea, S.; Kirk, G.D.; Lucas, G.M.; Sterling, T.R. Effectiveness of highly active antiretroviral therapy among injection drug users with late-stage human immunodeficiency virus infection. Am. J. Epidemiol. 2005, 161, 999–1012. [Google Scholar] [CrossRef] [PubMed]
- Joint United Nations Programme on HIV/AIDS (UNAIDS) African Union (AU). Global HIV AIDS Statistics-Fact Sheet. [Internet]. 2021. Available online: https://www.unaids.org/en/resources/fact-sheet (accessed on 18 September 2022).
- World Health Organization. End HIV/AIDS by 2030: Framework for Action in the WHO African Region, 2016–2020. 2017. Available online: https://apps.who.int/iris/bitstream/handle/10665/259638/EndAIDS-eng.pdf (accessed on 10 September 2022).
- UNAIDS. UNAIDS Goal 90-90-90: An Ambitious Treatment Target to Help End the AIDS Epidemic [Internet]. Switzerland. 2014. Available online: https://www.unaids.org/en/resources/documents/2017/90-90-90 (accessed on 16 September 2022).
- Opoku, S.; Sakyi, S.A.; Ayisi-Boateng, N.K.; Enimil, A.K.; Senu, E.; Ansah, R.O.; Aning, B.D.; Ojuang, D.A.; Wekesa, D.N.; Ahmed, F.O.; et al. Factors associated with viral suppression and rebound among adult HIV patients on treatment: A retrospective study in Ghana. AIDS Res. Ther. 2022, 19, 21. [Google Scholar] [CrossRef] [PubMed]
- Barry, O.; Powell, J.; Renner, L.; Bonney, E.Y.; Prin, M.; Ampofo, W.; Paintsil, E. Effectiveness of first-line antiretroviral therapy and correlates of longitudinal changes in CD4 and viral load among HIV-infected children in Ghana. BMC Infect. Dis. 2013, 13, 476. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bulage, L.; Ssewanyana, I.; Nankabirwa, V.; Nsubuga, F.; Kihembo, C.; Pande, G.; Ario, A.R.; Matovu, J.K.; Wanyenze, R.K.; Kiyaga, C. Factors Associated with Virological Non-suppression among HIV-Positive Patients on Antiretroviral Therapy in Uganda, August 2014–July 2015. BMC Infect. Dis. 2017, 17, 326. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jobanputra, K.; Parker, L.A.; Azih, C.; Okello, V.; Maphalala, G.; Kershberger, B.; Khogali, M.; Lujan, J.; Antierens, A.; Teck, R.; et al. Factors Associated with Virological Failure and Suppression after Enhanced Adherence Counselling, in Children, Adolescents and Adults on Antiretroviral Therapy for HIV in Swaziland. PLoS ONE 2015, 10, e0116144. [Google Scholar] [CrossRef] [Green Version]
- Chawana, T.D.; Reid, A.; Bwakura, T.; Gavi, S.; Nhachi, C.F.B. Factors influencing treatment failure in HIV positive adult patients on first line antiretroviral therapy. Central Afr. J. Med. 2016, 60, 29–36. [Google Scholar]
- Ansah, D.; Kumah, E.; Bawontuo, V.; Agyei-Baffour, P.; Afriyie, E.K. Determinants of viral load non-suppression among people living with HIV on antiretroviral therapy in Kumasi, Ghana. Ghana Med. J. 2021, 55, 111–117. [Google Scholar]
- Lailulo, Y.; Kitenge, M.; Jaffer, S.; Aluko, O.; Nyasulu, P.S. Factors associated with antiretroviral treatment failure among people living with HIV on antiretroviral therapy in resource-poor settings: A systematic review and metaanalysis. Syst. Rev. 2020, 9, 292. [Google Scholar] [CrossRef]
- Meshesha, H.M.; Nigussie, Z.M.; Asrat, A.; Mulatu, K. Determinants of virological failure among adults on first-line highly active antiretroviral therapy at public health facilities in Kombolcha town, Northeast, Ethiopia: A case–control study. BMJ Open 2020, 10, e036223. [Google Scholar] [CrossRef]
- Yuan, D.; Liu, M.; Jia, P.; Li, Y.; Huang, Y.; Ye, L.; Api, L.; Chen, M.; Yao, L.; Wang, Z.; et al. Prevalence and determinants of virological failure, genetic diversity and drug resistance among people living with HIV in a minority area in China: A population-based study. BMC Infect. Dis. 2020, 20, 443. [Google Scholar] [CrossRef]
- Emagnu, A.; Abay, Z.; Bulti, A.B.; Animut, Y. Determinants of Virologic Failure among Adult HIV Patients on First-Line Antiretroviral Therapy at Waghimra Zone, Northern Ethiopia: A Case-Control Study. Adv. Public Health 2020, 2020, 1929436. [Google Scholar] [CrossRef]
- Owusu, M.; Mensah, E.; Enimil, A.; Mutocheluh, M. Prevalence and Risk Factors of Virological Failure Among Children on Antiretroviral Therapy. BMJ Glob. Health 2017, 2, A9. [Google Scholar] [CrossRef]
- Lokpo, S.Y.; Ofori-Attah, P.J.; Ameke, L.S.; Obirikorang, C.; Orish, V.N.; Kpene, G.E.; Agboli, E.; Kye-Duodu, G.; Deku, J.G.; Awadzi, B.K.; et al. Viral Suppression and Its Associated Factors in HIV Patients on Highly Active Antiretroviral Therapy (HAART): A Retrospective Study in the Ho Municipality, Ghana. AIDS Res. Treat. 2020, 2020, 9247451. [Google Scholar] [CrossRef] [Green Version]
- Ghana AIDS Commission. GHANA’S HIV FACT SHEET_2019 [Internet]. 2019. Available online: https://www.ghanaids.gov.gh/mcadmin/Uploads/2019%20FACT%20SHEET%2022%2006%202020%20revised(1).pdf (accessed on 7 September 2022).
- Ghana AIDS Commission. National and Sub-National HIV and AIDS Estimates and Projections: 2020 Report; [Internet]; Ghana Aids Commission: Accra, Ghana, 2020. Available online: https://www.ghanaids.gov.gh/mcadmin/Uploads/2020%20HIV%20and%20AIDS%20Estimates%20and%20Projections%20PDF.pdf (accessed on 8 September 2022).
- Ghana AIDS Commission. Update on National HIV AIDS Response; Eastern Premier Hotel: Koforidua, CA, USA, 2021. [Google Scholar]
- Afrane, A.K.A.; Goka, B.Q.; Renner, L.; Yawson, A.E.; Alhassan, Y.; Owiafe, S.N.; Agyeman, S.; Sagoe, K.W.C.; Kwara, A. HIV virological non-suppression and its associated factors in children on antiretroviral therapy at a major treatment centre in Southern Ghana: A cross-sectional study. BMC Infect. Dis. 2021, 21, 731. [Google Scholar] [CrossRef]
- Yamane, T. Statistics: An Introductory Analysis, 2nd ed.; Harper and Row: New YorK, NY, USA, 1967. [Google Scholar]
- World Health Organization. Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection: Recommendations for a Public Health Approach; World Health Organization: Genève, Switzerland, 2016. [Google Scholar]
- World Health Organization. Antiretroviral Therapy for HIV Infection in Infants and Children: Towards Universal Access. Recomm a Public Heal Approach; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Byrd, K.; Hou, J.G.; Hazen, R.; Kirkham, H.; Suzuki, S.; Clay, P.G.; Bush, T.; Camp, N.M.; Weidle, P.J.; Delpino, A.; et al. Antiretroviral Adherence Level Necessary for HIV Viral Suppression Using Real-World Data. Am. J. Ther. 2019, 82, 245–251. [Google Scholar] [CrossRef]
- Ritchie, A.V.; Ushiro-Lumb, I.; Edemaga, D.; Joshi, H.A.; De Ruiter, A.; Szumilin, E.; Lee, H.H. SAMBA HIV semiquantitative test, a new point-of-care viral-load-monitoring assay for resource-limited settings. J. Clin. Microbiol. 2014, 52, 3377–3383. [Google Scholar] [CrossRef] [Green Version]
- Ochodo, E.A.; Olwanda, E.E.; Deeks, J.J.; Mallett, S. Point-of-care viral load tests to detect high HIV viral load in people living with HIV/AIDS attending health facilities. Cochrane Database Syst. Rev. 2022, 2022, CD013208. [Google Scholar] [CrossRef]
- Bokretsion, G.B.; Endalkachew, N.; Getachew, K.A. HIV/AIDS treatment failure and its determinant factors among first line HAART patients at Felege-Hiwot Referral Hospital, Bahir Dar, Northwest Ethiopia. J. AIDS Clin. Res. 2017, 8, 744. [Google Scholar]
- Raghupathi, V.; Raghupathi, W. The influence of education on health: An empirical assessment of OECD countries for the period 1995–2015. Arch. Public Health 2020, 78, 20. [Google Scholar] [CrossRef] [Green Version]
- Shacham, E.; Nurutdinova, D.; Onen, N.; Stamm, K.; Overton, E.T. The Interplay of Sociodemographic Factors on Virologic Suppression Among a U.S. Outpatient HIV Clinic Population. AIDS Patient Care STDs 2010, 24, 229–235. [Google Scholar] [CrossRef] [Green Version]
- Leigh, J.P.; De Vogli, R. Low wages as occupational health hazards. J. Occup. Environ. Med. 2016, 58, 444–447. [Google Scholar] [CrossRef] [PubMed]
- Joseph Davey, D.; Abrahams, Z.; Feinberg, M.; Prins, M.; Serrao, C.; Medeossi, B.; Darkoh, E. Factors associated with recent unsuppressed viral load in HIV-1-infected patients in care on first-line antiretroviral therapy in South Africa. Int. J. STD AIDS 2018, 29, 603–610. [Google Scholar] [CrossRef] [PubMed]
- Rangarajan, S.; Colby, D.J.; Giang, L.T.; Bui, D.D.; Nguyen, H.H.; Tou, P.B.; Danh, T.T.; Tran, N.B.C.; Nguyen, D.A.; Nguyen, B.T.H.; et al. Factors associated with HIV viral load suppression on antiretroviral therapy in Vietnam. J. Virus Erad. 2016, 2, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Fokam, J.; Billong, S.C.; Jogue, F.; Moyo Tetang Ndiang, S.; Nga Motaze, A.C.; Paul, K.N.; Njom Nlend, A.E. Immuno-virological response and associated factors amongst HIV-1 vertically infected adolescents in Yaoundé-Cameroon. PLoS ONE 2017, 12, e0187566. [Google Scholar] [CrossRef] [Green Version]
- Liégeois, F.; Vella, C.; Eymard-Duvernay, S.; Sica, J.; Makosso, L.; Mouinga-Ondémé, A.; Rouet, F. Virological failure rates and HIV-1 drug resistance patterns in patients on first-line antiretroviral treatment in semirural and rural Gabon. J. Int. AIDS Soc. 2012, 15, 17985. [Google Scholar] [CrossRef]
- Rupérez, M.; Pou, C.; Maculuve, S.; Cedeño, S.; Luis, L.; Rodríguez, J.; Letang, E.; Moltó, J.; Macete, E.; Clotet, B.; et al. Determinants of virological failure and antiretroviral drug resistance in Mozambique. J. Antimicrob. Chemother. 2015, 70, 2639–2647. [Google Scholar] [CrossRef] [Green Version]
- Mamo, A.; Assefa, T.; Negash, W.; Takelign, Y.; Sahiledinigl, B.; Teferu, Z.; Atilaw, D. Virological and Immunological Antiretroviral Treatment Failure and Predictors Among HIV Positive Adult and Adolescent Clients in Southeast Ethiopia. HIV/AIDS (Auckl. NZ) 2022, 14, 73. [Google Scholar]
- Fong, R.; Cheng, A.C.; Vujovic, O.; Hoy, J.F. Factors associated with virological failure in a cohort of combination antiretroviral therapy-treated patients managed at a tertiary referral centre. Sex. Health 2013, 10, 442–447. [Google Scholar] [CrossRef]
- Kyaw, N.T.T.; Harries, A.D.; Kumar, A.M.V.; Oo, M.M.; Kyaw, K.W.Y.; Win, T.; Aung, T.K.; Min, A.C.; Oo, H.N. High rate of virological failure and low rate of switching to second-line treatment among adolescents and adults living with HIV on first-line ART in Myanmar, 2005–2015. PLoS ONE 2017, 12, e0171780. [Google Scholar] [CrossRef]
- Potchoo, Y.; Tchamdja, K.; Balogou, A.; Pitche, V.P.; Guissou, I.P.; Kassang, E.K. Knowledge and adherence to antiretroviral therapy among adult people living with HIV/AIDS treated in the health care centers of the association Espoir Vie Togo" in Togo, West Africa. BMC Clin. Pharmacol. 2010, 10, 11. [Google Scholar] [CrossRef] [Green Version]
- Morowatisharifabad, M.A.; Movahed, E.; Farokhzadian, J.; Nikooie, R.; Hosseinzadeh, M.; Askarishahi, M.; Bidaki, R. Antiretroviral therapy adherence and its determinant factors among people living with HIV/AIDS: A case study in Iran. BMC Notes 2019, 12, 162. [Google Scholar] [CrossRef]
- de Fatima Bonolo, P.; Ceccato, M.D.G.B.; Rocha, G.M.; de Assis Acúrcio, F.; Campos, L.N.; Guimarães, M.D.C. Gender differences in non-adherence among Brazilian patients initiating antiretroviral therapy. Clinics 2013, 68, 612–620. [Google Scholar] [CrossRef]
- Uzochukwu, B.S.C.; Onwujekwe, O.E.; Onoka, A.C.; Okoli, C.; Uguru, N.P.; Chukwuogo, O.I. Determinants of non-adherence to subsidized anti-retroviral treatment in southeast Nigeria. Health Policy Plan. 2009, 24, 189–196. [Google Scholar] [CrossRef] [Green Version]
- Diress, G.; Dagne, S.; Alemnew, B.; Adane, S.; Addisu, A. Viral Load Suppression after Enhanced Adherence Counseling and Its Predictors among High Viral Load HIV Seropositive People in North Wollo Zone Public Hospitals, Northeast Ethiopia, 2019: Retrospective Cohort Study. AIDS Res. Treat. 2020, 2020, 8909232. [Google Scholar] [CrossRef]
- Ridgeway, K.; Dulli, L.S.; Murray, K.R.; Silverstein, H.; Santo, L.D.; Olsen, P.; de Mora, D.D.; McCarraher, D.R. Interventions to improve antiretroviral therapy adherence among adolescents in low- and middle-income countries: A systematic review of the literature. PLoS ONE 2018, 13, e0189770. [Google Scholar] [CrossRef]
- Ghana AIDS Commission. Ghana May Not Meetthe 90-90-90 Target by 2020—AIDS Commission [Internet]. 2019. Available online: https://www.ghanaids.gov.gh/pages/ghana-may-not-meet-the-90-90-90-target-by-2020-aids-commission (accessed on 10 August 2022).
| Name of Facility | Total ART Active Clients with Viral Load Test | Sample Size |
|---|---|---|
| Regional Hospital, Bolgatanga | 1274 | 108 |
| War Memorial Hospital | 759 | 64 |
| Bongo Hospital | 737 | 63 |
| Zebilla Hospital | 426 | 36 |
| Sandema Hospital | 379 | 32 |
| Tongo Hospital | 268 | 23 |
| Kongo-Logre Health Centre | 267 | 23 |
| Paga Hospital | 205 | 17 |
| Total | 4315 | 366 |
| Variables | Frequency (n) | Percentage (%) |
|---|---|---|
| Age group (years) | ||
| 15–24 | 46 | 12.6 |
| 25–34 | 136 | 37.2 |
| 35–44 | 107 | 29.2 |
| 45–54 | 55 | 15.0 |
| ≥55 | 22 | 6.0 |
| Gender | ||
| Male | 98 | 26.8 |
| Female | 268 | 73.2 |
| Marital Status | ||
| Married | 208 | 56.8 |
| Never married | 62 | 16.9 |
| Divorced/Separated/Widowed | 96 | 26.2 |
| Educational Status | ||
| No formal education | 192 | 52.5 |
| Basic | 78 | 21.3 |
| SHS/Voc/Tech | 70 | 19.1 |
| Tertiary | 26 | 7.1 |
| Occupation | ||
| Public/Private employment | 46 | 12.6 |
| Self-employed | 229 | 62.6 |
| Unemployed | 91 | 24.9 |
| Salary/Income Level | ||
| <GHS 375.00 | 222 | 60.7 |
| GHS 375–1000 | 99 | 27.0 |
| >GHS 1000 | 45 | 12.3 |
| Alcohol Intake | ||
| Yes | 99 | 27.0 |
| No | 267 | 73.0 |
| Variables | Frequency (n) | Percentage (%) |
|---|---|---|
| Age at HIV Diagnosis | ||
| 15–24 | 155 | 42.3 |
| 25–34 | 180 | 49.2 |
| 35–44 | 31 | 8.5 |
| Adherence Counseling | ||
| Yes | 356 | 97.3 |
| No | 10 | 2.7 |
| ART Duration | ||
| <1 year | 36 | 9.8 |
| 1–3 years | 115 | 31.4 |
| ≥3 years | 215 | 58.7 |
| ARV Combination | ||
| Tenofovir + Lamivudine + Efavirenz | 65 | 17.8 |
| Tenofovir + Lamivudine + Dolutegravir | 280 | 76.5 |
| Zidovudine + Lamivudine + Dolutegravir | 21 | 5.7 |
| Ease of taking ART | ||
| Easy | 326 | 89.1 |
| Difficult | 40 | 10.9 |
| Issues with Receiving ART in Timely Manner | ||
| Yes | 58 | 15.8 |
| No | 308 | 84.2 |
| Reasons Doses Missed | ||
| Stigma | 22 | 6.0 |
| Felt sick/ill | 44 | 12.0 |
| Side effects | 38 | 10.4 |
| Forgot to take | 67 | 18.3 |
| Ran out of pills | 181 | 49.5 |
| ART Side Effects | ||
| Yes | 38 | 10.4 |
| No | 328 | 89.6 |
| Variables | Frequency (n) | Percentage (%) |
|---|---|---|
| Received Enhanced Adherence Counseling | ||
| Yes | 356 | 97.3 |
| No | 10 | 2.7 |
| Number of Viral Load (VL) Tests Done | ||
| 1 time | 253 | 69.1 |
| 2 times | 105 | 28.7 |
| 3 times | 8 | 2.2 |
| Reasons for checking VL test * | ||
| Check disease progression | 144 | 39.3 |
| Monitor response to ART | 333 | 91.0 |
| Check infectious level | 48 | 13.1 |
| Viral Load Results | ||
| ˂1000 copies/mL | 131 | 35.8 |
| ≥1000 copies/mL | 172 | 47.0 |
| Target Not Detected | 63 | 17.2 |
| Results Interpreted to Respondent | ||
| Yes | 339 | 92.6 |
| No | 27 | 7.4 |
| Viral Load Result Status | ||
| VL Suppressed | 194 | 53.0 |
| VL Failed (Unsuppressed) | 172 | 47.0 |
| Implication of VL Failure * | ||
| Can cause further infection | 129 | 35.2 |
| Increase to stage 3/AIDS | 116 | 31.7 |
| Opportunistic infection | 130 | 35.5 |
| Drug resistance | 20 | 5.5 |
| Reduce survival rate | 121 | 33.1 |
| Variables | Categories | Viral Load (VL) Status | p-Value | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|---|---|
| VL Suppressed | VL Failed (Unsuppressed) | |||||
| Gender | 0.232 | |||||
| Male | 57 (58.2%) | 41 (41.8%) | Ref * | Ref * | ||
| Female | 137 (51.1%) | 131 (48.9%) | 1.33 (0.83–2.12) | 1.04 (0.56–1.95) | ||
| Age | 0.016 | |||||
| 15–24 | 28 (60.9%) | 18 (39.1%) | Ref * | Ref * | ||
| 25–34 | 59 (43.3%) | 77 (56.6%) | 2.03 (1.02–4.01) * | 1.79 (0.62–5.16) | ||
| 35–44 | 66 (61.7%) | 41 (38.2%) | 0.97 (0.48–1.96) | 1.28 (0.44–3.79) | ||
| 45–54 | 26 (47.3%) | 29 (52.7%) | 1.74 (0.78–3.84) | 1.81 (0.54–6.08) | ||
| ≥55 | 15 (68.2%) | 7 (31.8%) | 0.73 (0.25–2.13) | 1.01 (0.22–4.71) | ||
| Marital status | 0.374 | omitted | ||||
| Married | 115 (55.3%) | 93 (44.7%) | Ref * | omitted | ||
| Never married | 34 (58.4%) | 28 (45.2%) | 1.02 (0.58–1.80) | omitted | ||
| Divorced/Separated/Widowed | 45 (46.9%) | 51 (53.1%) | 1.40 (0.86–2.28) | omitted | ||
| Education | p < 0.001 | |||||
| No formal education | 89 (46.4%) | 103 (53.6%) | 8.8 (2.57–30.54) ** | 4.30 (0.94–34.34) | ||
| Basic | 40 (51.3%) | 38 (48.7%) | 7.28 (2.02–26.25) ** | 7.36 (4.91–59.71) * | ||
| SHS/Vocational/Technical | 42 (60.0%) | 28 (40.0%) | 5.11 (1.40–18.65) * | 4.70 (1.90–9.69) * | ||
| Tertiary | 23 (88.5%) | 3 (11.5%) | Ref * | Ref * | ||
| Occupation | 0.019 | |||||
| Public/Private employment | 33 (71.7%) | 13 (28.3%) | 0.35 (0.16–0.76) ** | 2.05 (0.52–8.09) | ||
| Self-employed | 118 (51.5%) | 111 (48.5%) | 0.84 (0.52–1.37) | 1.28 (0.63–2.64) | ||
| Unemployed | 43 (47.3%) | 48 (52.7%) | Ref * | Ref * | ||
| Monthly salary/income | p < 0.001 | |||||
| <GHS 375.00 | 95 (42.8%) | 127 (57.2%) | 6.18 (2.75–13.88) *** | 7.20 (1.73–29.95) ** | ||
| GHS 375–1000 | 62 (62.6%) | 37 (37.4%) | 2.76 (1.16–6.56) ** | 2.02 ((0.51–7.91) | ||
| >GHS 1000 | 37 (82.2%) | 8 (17.8%) | Ref * | Ref * | ||
| Alcohol intake | 0.719 | Omitted | ||||
| Yes | 54 (54.5%) | 45 (45.5%) | 1.09 (0.69–1.73) | Omitted | ||
| No | 140 (52.4%) | 127 (47.6%) | Ref * | Omitted | ||
| Age at HIV diagnosis (years) | 0.071 | |||||
| 15–24 | 87 (56.1%) | 68 (43.9%) | 1.64 (0.72–3.72) | 1.74 (0.51–5.86) | ||
| 25–34 | 86 (47.6%) | 94 (52.2%) | 2.30 (1.02–5.15) * | 2.42 (0.77–7.61) | ||
| 35–44 | 21 (67.7%) | 10 (32.3%) | Ref * | Ref * | ||
| ART duration | 0.017 | |||||
| <1 year | 27 (75.0%) | 9 (25.0%) | 0.32 (0.15–0.72) ** | 0.27 (0.10–0.75) * | ||
| 1–3 years | 61 (53.0%) | 54 (47.0%) | 0.86 (0.55–1.35) | 0.70 (0.39–1.27) | ||
| >3 years | 106 (49.3%) | 109 (50.7%) | Ref * | Ref * | ||
| ART combination | p < 0.001 | |||||
| Tenofovir + Lamivudine + Efavirenz | 20 (30.8%) | 45 (69.2%) | 3.66 (1.31–1.21) * | 3.26 (1.95–11.25) ** | ||
| Tenofovir + Lamivudine + Dolutegravir | 161 (57.5%) | 119 (42.5%) | 1.20 (0.48–2.99) | 1.20 (0.39–3.72) | ||
| Zidovudine + Lamivudine + Dolutegravir | 13 (61.9%) | 8 (38.1%) | Ref * | Ref * | ||
| Missed doses/ART adherence | p < 0.001 | |||||
| <2 doses (good) | 161 (70.3%) | 68 (29.7%) | Ref * | Ref * | ||
| 3–5 doses (fair) | 22 (50.0%) | 22 (50.0%) | 2.37 (1.23–4.56) ** | 2.86 (1.34–6.08) ** | ||
| ≥6 doses (poor) | 11 (11.8%) | 82 (88.2%) | 17.65 (8.85–35.20) *** | 23.87 (10.57–53.92) *** | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abubakari, A.; Issah, H.; Mutaka, M.A.O.; Asumah, M.N. Determinants of Virological Failure in HIV Patients on Highly Active Antiretroviral Therapy (HAART): A Retrospective Cross-Sectional Study in the Upper East Region of Ghana. Venereology 2023, 2, 16-29. https://doi.org/10.3390/venereology2010002
Abubakari A, Issah H, Mutaka MAO, Asumah MN. Determinants of Virological Failure in HIV Patients on Highly Active Antiretroviral Therapy (HAART): A Retrospective Cross-Sectional Study in the Upper East Region of Ghana. Venereology. 2023; 2(1):16-29. https://doi.org/10.3390/venereology2010002
Chicago/Turabian StyleAbubakari, Abdulai, Habibu Issah, M. Awell Olives Mutaka, and Mubarick Nungbaso Asumah. 2023. "Determinants of Virological Failure in HIV Patients on Highly Active Antiretroviral Therapy (HAART): A Retrospective Cross-Sectional Study in the Upper East Region of Ghana" Venereology 2, no. 1: 16-29. https://doi.org/10.3390/venereology2010002
APA StyleAbubakari, A., Issah, H., Mutaka, M. A. O., & Asumah, M. N. (2023). Determinants of Virological Failure in HIV Patients on Highly Active Antiretroviral Therapy (HAART): A Retrospective Cross-Sectional Study in the Upper East Region of Ghana. Venereology, 2(1), 16-29. https://doi.org/10.3390/venereology2010002







