New Paradigms for Thoracic Outlet Compression and Thoracic Outlet Syndrome, with or without Complications or Sequelae: A Trans-Continental and Trans-Disciplinary Opinion Paper
Abstract
1. Introduction
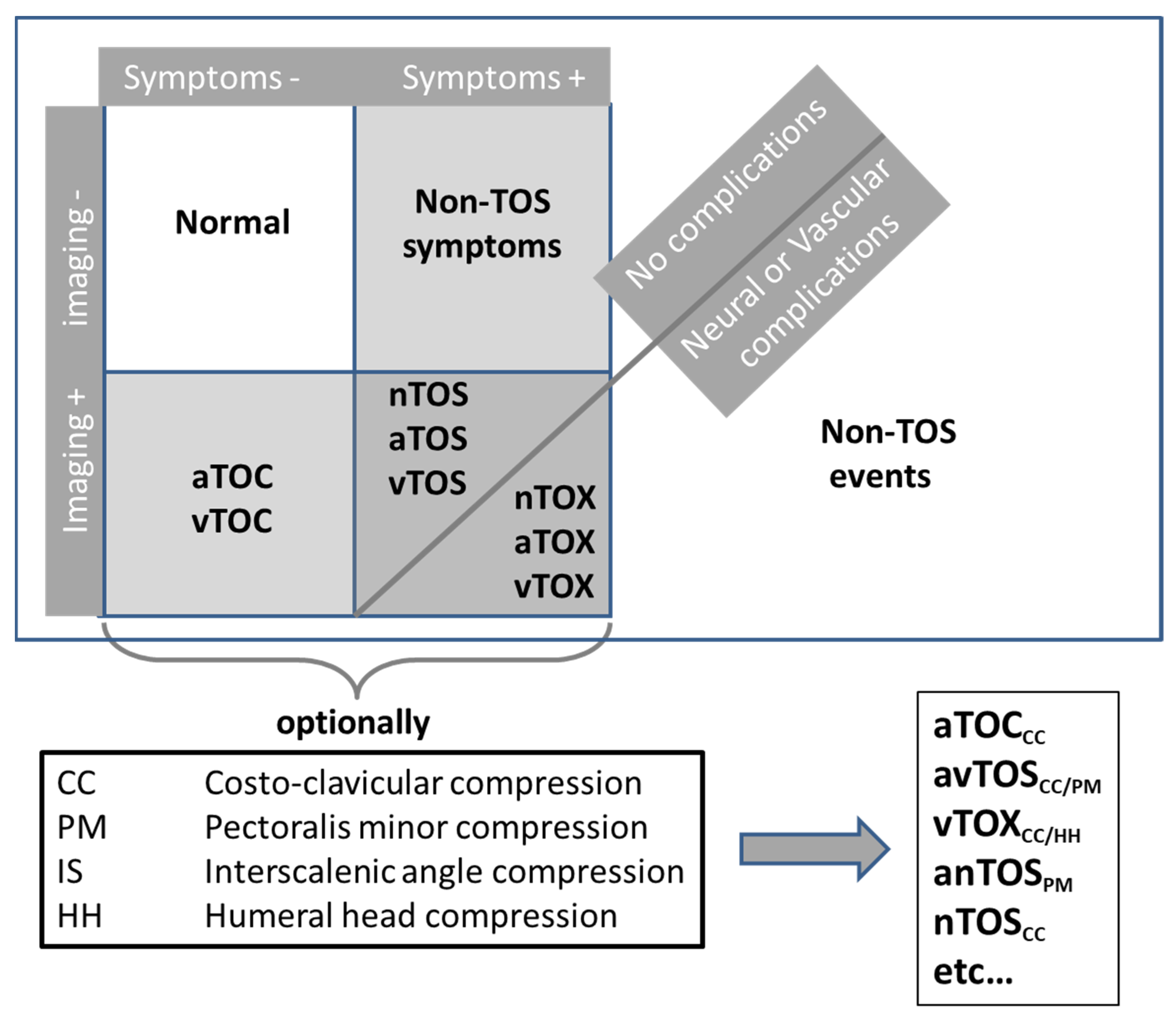
2. New Paradigm for Clinical Classification
3. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Larson, S.G.; Jungers, W.L.; Morwood, M.J.; Sutikna, T.; Jatmiko; Saptomo, E.W.; Due, R.A.; Djubiantono, T. Homo floresiensis and the evolution of the hominin shoulder. J. Hum. Evol. 2007, 53, 718–731. [Google Scholar] [CrossRef]
- Voisin, J.L. Clavicle, a neglected bone: Morphology and relation to arm movements and shoulder architecture in primates. Anat. Rec. A Discov. Mol. Cell Evol. Biol. 2006, 288, 944–953. [Google Scholar] [CrossRef] [PubMed]
- Illig, K.A.; Donahue, D.; Duncan, A.; Freischlag, J.; Gelabert, H.; Johansen, K.; Jordan, S.; Sanders, R.; Thompson, R. Reporting standards of the Society for Vascular Surgery for thoracic outlet syndrome: Executive summary. J. Vasc. Surg. 2016, 64, 797–802. [Google Scholar] [CrossRef] [PubMed]
- Illig, K.A.; Rodriguez-Zoppi, E. How Common Is Thoracic Outlet Syndrome? Thorac. Surg. Clin. 2021, 31, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Wyllie, W.G. Scalenus Anticus Syndrome in a Girl aged 11 Years. Proc. R. Soc. Med. 1939, 32, 218. [Google Scholar] [CrossRef] [PubMed]
- Craig, W.M.; Knepper, P.A. Cervical Rib and the Scalenus Anticus Syndrome. Ann. Surg. 1937, 105, 556–563. [Google Scholar] [CrossRef] [PubMed]
- Falconer, M.A. The costoclavicular syndrome. Br. Med. J. 1947, 2, 69–70. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, E.; Fletcher, A. The costoclavicular syndrome. Br. Med. J. 1947, 1, 465–466. [Google Scholar] [CrossRef]
- Bishop, L.; Bartlett, M. Doppler waveform analysis during provocative manoeuvres in the assessment for arterial thoracic outlet syndrome results in high false-positive rates; a cross-sectional study. JRSM Cardiovasc. Dis. 2021, 10, 20480040211006571. [Google Scholar] [CrossRef]
- Nord, K.M.; Kapoor, P.; Fisher, J.; Thomas, G.; Sundaram, A.; Scott, K.; Kothari, M.J. False positive rate of thoracic outlet syndrome diagnostic maneuvers. Electromyogr. Clin. Neurophysiol. 2008, 48, 67–74. [Google Scholar]
- Li, N.; Dierks, G.; Vervaeke, H.E.; Jumonville, A.; Kaye, A.D.; Myrcik, D.; Paladini, A.; Varrassi, G.; Viswanath, O.; Urits, I. Thoracic Outlet Syndrome: A Narrative Review. J. Clin. Med. 2021, 10, 962. [Google Scholar] [CrossRef] [PubMed]
- Collins, E.; Orpin, M. Physical Therapy Management of Neurogenic Thoracic Outlet Syndrome. Thorac. Surg. Clin. 2021, 31, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Balderman, J.; Abuirqeba, A.A.; Eichaker, L.; Pate, C.; Earley, J.A.; Bottros, M.M.; Jayarajan, S.N.; Thompson, R.W. Physical therapy management, surgical treatment, and patient-reported outcomes measures in a prospective observational cohort of patients with neurogenic thoracic outlet syndrome. J. Vasc. Surg. 2019, 70, 832–841. [Google Scholar] [CrossRef] [PubMed]
- Pesser, N.; Goeteyn, J.; van der Sanden, L.; Houterman, S.; van Alfen, N.; van Sambeek, M.; van Nuenen, B.F.L.; Teijink, J.A.W. Feasibility and Outcomes of a Multidisciplinary Care Pathway for Neurogenic Thoracic Outlet Syndrome: A Prospective Observational Cohort Study. Eur. J. Vasc. Endovasc. Surg. 2021, 61, 1017–1024. [Google Scholar] [CrossRef] [PubMed]
- Matsubara, T.; Kurokawa, K.; Sakurai, K.; Yasutomi, H.; Yamawaki, T. The Gilliatt-Sumner hand: A diagnostic clue of neurogenic thoracic outlet syndrome. QJM 2018, 111, 831–832. [Google Scholar] [CrossRef] [PubMed]
- McGillicuddy, J.E. Cervical radiculopathy, entrapment neuropathy, and thoracic outlet syndrome: How to differentiate? Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2004. J. Neurosurg. Spine 2004, 1, 179–187. [Google Scholar] [CrossRef] [PubMed]
- Tilki, H.E.; Stalberg, E.; Incesu, L.; Basoglu, A. Bilateral neurogenic thoracic outlet syndrome. Muscle Nerve 2004, 29, 147–150. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Martinez, A.; Arpa, J. Electrophysiological assessment in neurogenic thoracic outlet syndrome. Electromyogr. Clin. Neurophysiol. 2001, 41, 253–256. [Google Scholar]
- Smith, T.; Trojaborg, W. Diagnosis of thoracic outlet syndrome. Value of sensory and motor conduction studies and quantitative electromyography. Arch. Neurol. 1987, 44, 1161–1163. [Google Scholar] [CrossRef]
- Dessureault-Dober, I.; Bronchti, G.; Bussieres, A. Diagnostic Accuracy of Clinical Tests for Neurogenic and Vascular Thoracic Outlet Syndrome: A Systematic Review. J. Manip. Physiol. Ther. 2018, 41, 789–799. [Google Scholar] [CrossRef]
- Hixson, K.M.; Horris, H.B.; McLeod, T.C.V.; Bacon, C.E.W. The Diagnostic Accuracy of Clinical Diagnostic Tests for Thoracic Outlet Syndrome. J. Sport Rehabil. 2017, 26, 459–465. [Google Scholar] [CrossRef] [PubMed]
- Stapleton, C.; Herrington, L.; George, K. Sonographic evaluation of the subclavian artery during thoracic outlet syndrome shoulder manoeuvres. Man. Ther. 2009, 14, 19–27. [Google Scholar] [CrossRef] [PubMed]
- DiFiore, J.W.; Reid, J.R.; Drummond-Webb, J. Thoracic outlet syndrome in a child—Transaxillary resection of anomalous first rib. J. Pediatr. Surg. 2002, 37, 1220–1222. [Google Scholar] [CrossRef] [PubMed]
- Franklin, G.M. Work-Related Neurogenic Thoracic Outlet Syndrome: Diagnosis and Treatment. Phys. Med. Rehabil. Clin. N. Am. 2015, 26, 551–561. [Google Scholar] [CrossRef] [PubMed]
- Sanders, R.J.; Hammond, S.L. Outcome of surgery for thoracic outlet syndrome in Washington state workers’ compensation. Neurology 2000, 55, 1594–1595. [Google Scholar] [CrossRef] [PubMed]
- Ritter, A.; Sensat, M.L.; Harn, S.D. Thoracic outlet syndrome: A review of the literature. J. Dent. Hyg. 1999, 73, 205–207. [Google Scholar] [PubMed]
- Abraham, P.; Henni, S. Symptoms and absence of symptoms while using a telephone: The paradox of thoracic outlet syndrome. Musculoskelet. Sci. Pract. 2021, 51, 102266. [Google Scholar] [CrossRef]
- Hammacher, E.R.; Eikelboom, B.C.; van Lier, H.J.; Skotnicki, S.H.; Wijn, P.F. Brachial artery lesions after cardiac catheterisation. Eur. J. Vasc. Surg. 1988, 2, 145–149. [Google Scholar] [CrossRef]
- Huber, T.S.; Brown, M.P.; Seeger, J.M.; Lee, W.A. Midterm outcome after the distal revascularization and interval ligation (DRIL) procedure. J. Vasc. Surg. 2008, 48, 926–932; discussion 932–923. [Google Scholar] [CrossRef][Green Version]
- Zhang, T.; Xu, Z.; Chen, J.; Liu, Z.; Wang, T.; Hu, Y.; Shen, L.; Xue, F. A Novel Approach for Imaging of Thoracic Outlet Syndrome Using Contrast-Enhanced Magnetic Resonance Angiography (CE-MRA), Short Inversion Time Inversion Recovery Sampling Perfection with Application-Optimized Contrasts Using Different Flip Angle Evolutions (T2-STIR-SPACE), and Volumetric Interpolated Breath-Hold Examination (VIBE). Med. Sci. Monit. 2019, 25, 7617–7623. [Google Scholar] [CrossRef]
- Magill, S.T.; Brus-Ramer, M.; Weinstein, P.R.; Chin, C.T.; Jacques, L. Neurogenic thoracic outlet syndrome: Current diagnostic criteria and advances in MRI diagnostics. Neurosurg. Focus 2015, 39, E7. [Google Scholar] [CrossRef] [PubMed]
- Haghighi, S.S.; Baradarian, S.; Bagheri, R. Sensory and motor evoked potentials findings in patients with thoracic outlet syndrome. Electromyogr. Clin. Neurophysiol. 2005, 45, 149–154. [Google Scholar] [PubMed]
- Abraham, P.; Hersant, J.; Ramondou, P.; Thouveny, F.; Feuilloy, M.; Picquet, J.; Henni, S. Comparison of transcutaneous oximetry with symptoms and arteriography in thoracic outlet syndrome. Clin. Hemorheol. Microcirc. 2020, 75, 107–119. [Google Scholar] [CrossRef] [PubMed]
- Henni, S.; Hersant, J.; Ammi, M.; Mortaki, F.E.; Picquet, J.; Feuilloy, M.; Abraham, P. Microvascular Response to the Roos Test Has Excellent Feasibility and Good Reliability in Patients With Suspected Thoracic Outlet Syndrome. Front. Physiol. 2019, 10, 136. [Google Scholar] [CrossRef] [PubMed]
- Hersant, J.; Ramondou, P.; Chavignier, V.; Chavanon, A.; Feuilloy, M.; Picquet, J.; Henni, S.; Abraham, P. Forearm Volume Changes Estimated by Photo-Plethysmography During an Original Candlestick/Prayer Maneuver in Patients with Suspected Thoracic Outlet Syndrome. Front. Physiol. 2021, 12, 652456. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abraham, P.; Wennberg, P.W.; Bauer, P.; Gu, Y.; Ouedraogo, N.; Guo, L.; Tew, G.; Mazzolai, L.; Martini, R.; Henni, S. New Paradigms for Thoracic Outlet Compression and Thoracic Outlet Syndrome, with or without Complications or Sequelae: A Trans-Continental and Trans-Disciplinary Opinion Paper. J. Vasc. Dis. 2023, 2, 413-418. https://doi.org/10.3390/jvd2040032
Abraham P, Wennberg PW, Bauer P, Gu Y, Ouedraogo N, Guo L, Tew G, Mazzolai L, Martini R, Henni S. New Paradigms for Thoracic Outlet Compression and Thoracic Outlet Syndrome, with or without Complications or Sequelae: A Trans-Continental and Trans-Disciplinary Opinion Paper. Journal of Vascular Diseases. 2023; 2(4):413-418. https://doi.org/10.3390/jvd2040032
Chicago/Turabian StyleAbraham, Pierre, Paul W. Wennberg, Pascal Bauer, Yongquan Gu, Nafi Ouedraogo, Lianrui Guo, Garry Tew, Lucia Mazzolai, Romeo Martini, and Samir Henni. 2023. "New Paradigms for Thoracic Outlet Compression and Thoracic Outlet Syndrome, with or without Complications or Sequelae: A Trans-Continental and Trans-Disciplinary Opinion Paper" Journal of Vascular Diseases 2, no. 4: 413-418. https://doi.org/10.3390/jvd2040032
APA StyleAbraham, P., Wennberg, P. W., Bauer, P., Gu, Y., Ouedraogo, N., Guo, L., Tew, G., Mazzolai, L., Martini, R., & Henni, S. (2023). New Paradigms for Thoracic Outlet Compression and Thoracic Outlet Syndrome, with or without Complications or Sequelae: A Trans-Continental and Trans-Disciplinary Opinion Paper. Journal of Vascular Diseases, 2(4), 413-418. https://doi.org/10.3390/jvd2040032




