Abstract
Obstetric trauma refers to injuries that occur to the newborn during the birth process and can occur despite proper perinatal care. Limiting risk factors could reduce its incidence and avoid significant morbidity and mortality to the infant. The aim of our study was to determine the incidence of birth injury in our setting and to discover its associated risks factors. For this case–control study, all births that took place in our center during the year 2021 were systematically reviewed. A total of 231 full-term newborns, with 77 cases and 154 controls, were included. For each case, two controls of similar sex and gestational age, born during the same shift before and after the case were selected. Preterm infants, outborn patients, twins, and infants with major congenital anomalies were excluded. The incidence of birth injury was 22.8‰ of singleton births. The most frequent injuries were cephalohematoma, peripheral facial paralysis, and clavicle fracture. After the adjusted logistic regression analysis, the variables that were independently associated with obstetric trauma were (aOR; 95% CI) breech presentation: 10.6 (1.2, 92.6), p = 0.032; dystocia: 7.8 (3.8, 16.2), p < 0.001; forceps instrumentation: 3.1 (1.0, 9.1), p = 0.043; induced labor: 3.0 (1.6, 5.5), p < 0.001; and newborn birthweight (per each 100 g): 1.1 (1.0, 1.2), p = 0.004. In conclusion, the incidence of birth trauma in our setting was 22.8‰ of singletons. The most frequent injuries were cephalohematoma, peripheral facial paralysis, and clavicle fracture. There was an independent association between birth trauma and breech presentation, dystocia, forceps instrumentation, labor induction, and infant birthweight.
1. Introduction
Childbirth is a natural and physiological process that, in most cases, culminates in the birth of a live and healthy newborn. During childbirth, trauma to the fetus can occur, which in most cases does not present complications and resolves spontaneously. However, some injuries persist over time and give rise to significant neonatal morbidity and mortality [1,2,3]. These injuries can occur despite proper perinatal care, but with new technologies and advances in maternal–fetal care techniques, obstetric trauma has decreased in incidence and severity worldwide. Some factors have contributed to this reduction. These include the increase in the number of caesarean sections when adverse fetal conditions are detected, the limitations in the use of instruments in the delivery process (forceps, vacuum, spatulas, etc.), and the near eradication of the Kristeller maneuver, among others. Birth trauma can cause important morbidity and mortality to the newborn that can be minimized with good peripartum care and the use of updated techniques. Therefore, it is important to recognize the main predisposing factors in order to prevent its appearance. The objective of our study was to determine the incidence of birth injury in our setting and to discover the potential independent risk factors associated with it. We hypothesized that obstetric trauma is still significantly present in the context of modern perinatology and that breech presentation, labor induction, instrumental delivery, and fetal weight increase the risk of birth injury.
2. Methods
We performed a case–control study of births that took place from 1 January to 31 December 2021 in our maternity hospital. The clinical records of mothers and infants were reviewed to record all the sociodemographic and clinical variables of interest and to detect the presence of birth trauma to the infant. Births were assisted by the obstetrical and neonatal teams according to their respective local protocols and under the guidance of the attending clinicians. Birth trauma was defined as any injury that occurred to the fetus or newborn during labor. In this study, caput succedaneum was not included because, given its low severity and its rapid resolution during the first hours of life in most cases, these cases are not systematically collected in the clinical records. As controls, infants of the same sex and gestational age (GA) born immediately before and after a case were selected.
The following set of variables was recorded:
- Maternal variables. Characteristics of the mother: age, height, weight, body mass index (BMI), and toxic habits. Maternal personal history: diabetes mellitus and arterial hypertension. Obstetric history: the number of pregnancies and previous vaginal deliveries, the gestational control, infectious risk factors, etc.
- Delivery variables. Characteristics of childbirth and its complications: onset of labor (spontaneous or induced); type of delivery (vaginal or caesarean section); delivery time, instrumentation, and type; fetal presentation; premature rupture membrane; chorioamnionitis; altered cardiotocographic record (CTGR); placental abruption; vasa previa rupture; umbilical cord knot or prolapse; etc. Dystocic end of labor was defined as any arrest in the normal progression of labor due to abnormally slow dilation of the cervix, delay in the normal descent of the fetus during active labor, entrapment of the fetal shoulders after delivery of the head, etc., requiring urgent intervention to finish labor.
- Newborn variables. Sex, weight, height, head circumference, first and five-minute Apgar scores, arterial and venous cord pH, and neonatal resuscitation. Intrauterine growth restriction (IUGR). If admission to the neonatal unit was required, age at admission and reason were recorded to determine its possible relationship with obstetric trauma. Type of birth injury was also included.
Statistical Analysis
The normality of the quantitative variables was studied using the Kolmogorov–Smirnov or Shapiro–Wilk tests. Results are presented as means or proportions and 95% confidence intervals. Variables with normal distribution were compared using the Student’s t test, and those with non-normal distribution are presented as median and interquartile range (IQR) and were compared with the Mann–Whitney U test. Qualitative variables are expressed as proportions (%) and were analyzed with the Pearson’s chi-square or Fisher’s exact test when appropriate. We used causal diagrams or Bayesian networks with directed acyclic graphs (DAGs) to study causal inference [4]. Birth trauma was the outcome variable, and as exposure variables, we tested risk factors known from the literature or from our bivariate analysis, considering their biological plausibility. Different variables were tested as potential confounders or intermediate variables. To avoid overadjustment, only true confounders (Supplementary Figure S1) were included in the logistic regression analysis [5]. Results are shown as odds ratios (ORs) and adjusted ORs (aORs) with 95% confidence intervals. All hypotheses were two-tail tested and p-values < 0.05 were considered significant. Statistical analyses were carried out using SPSS.v25 software (SPSS Inc., Chicago, IL, USA).
Given that all the maternal and infant records were systematically reviewed during the study period, all variables of interest were appropriately collected and there were no missing values. A complete-case analysis was performed. For sensitivity analysis, we carried out determination of the E-values for the estimated aOR and for the limit of the CI closest to the null (Supplementary Table S1) [6,7,8].
The study was approved by the Centre’s Research Ethics Committee (number: 2021:177-1). Patient informed consent was not deemed necessary due to the anonymity of the data and the non-interventional nature of the study.
3. Results
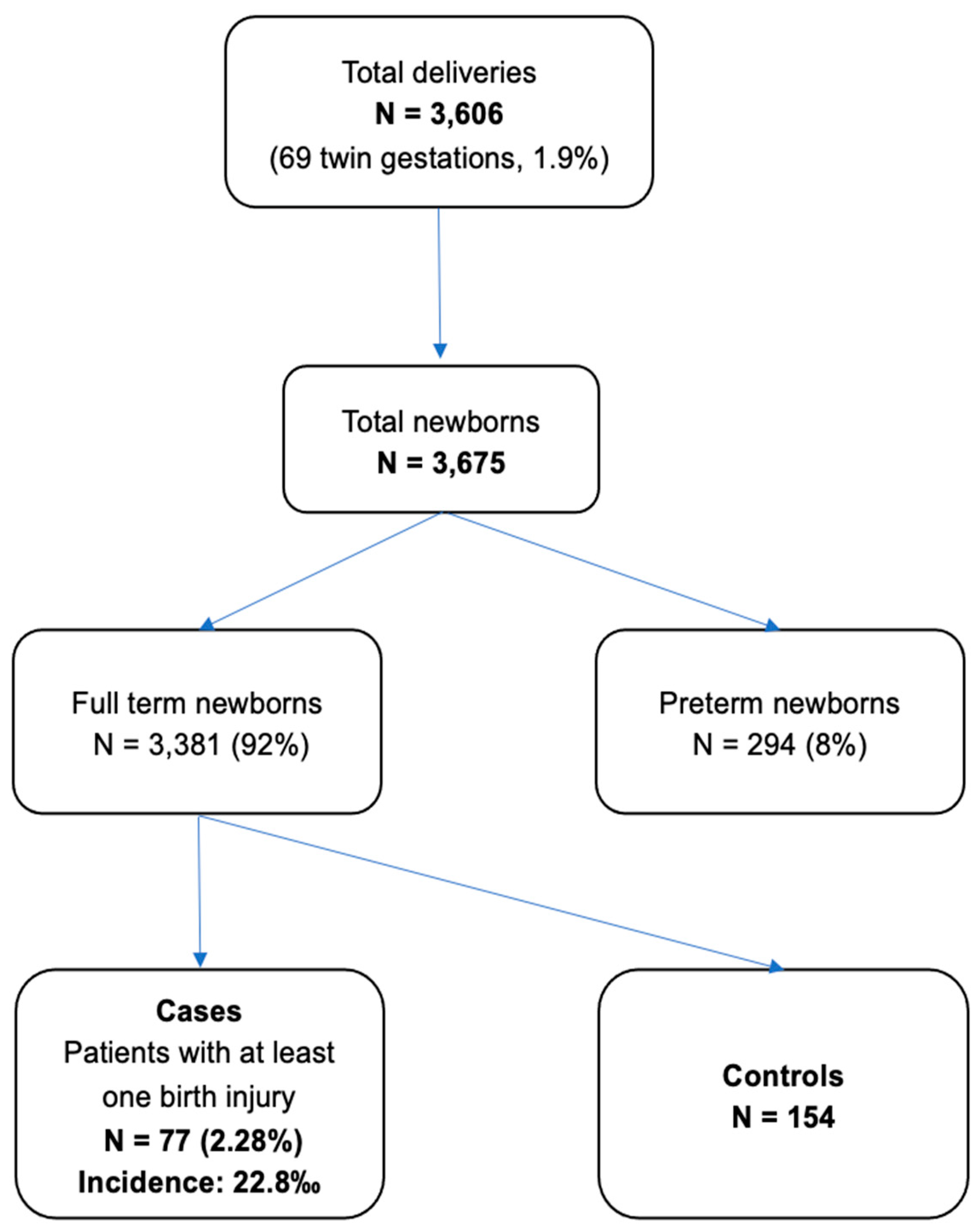
During the year 2021, a total of 3606 deliveries were registered with a final number of 3675 newborns, of which 3381 (93.8%) were full-term infants. A total of 231 newborns were included in the study, with 77 cases and 154 controls. The final number of birth injuries was 96 injuries in 77 patients, which represents an incidence of 22.8‰ of term newborns (Figure 1).
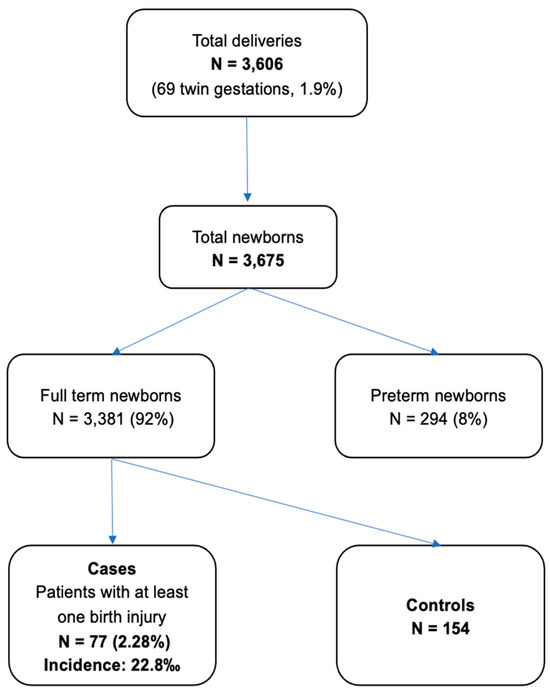
Figure 1.
Patient flow chart. Flow chart of total deliveries assisted in our maternity hospital during 2021, with the total number of newborns, full-term newborns, patients with birth trauma (cases), and controls included in the study.
Table 1 shows the different types of birth trauma found. The most frequent injuries were cephalohematoma (35/77 = 45.5%), followed by facial paralysis (17/77 = 22.1%) and clavicle fracture (15/77 = 19.5%). No cases of subgaleal hemorrhage, intraparenchymal hemorrhage, epidural hemorrhage, or skull fractures were detected in our series.

Table 1.
Classification of birth trauma (ICD 11). Number of reported injuries and incidence per 1000 live-born, full-term infants (n = 3381).
Table 2 shows the distribution of maternal and delivery characteristics in both study groups. The maternal age was significantly higher in the case group, but we did not find any other significant differences in the sociodemographic characteristics. Induced labor was more frequent in cases, and the second stage of labor was longer in these mothers.

Table 2.
Maternal demographic characteristics and perinatal interventions in cases and controls.
Table 3 shows the infants’ demographic characteristics and postnatal interventions in cases and controls. Infants with birth trauma were significantly heavier and larger. In comparison with cephalic presentation, breech presentation ended more frequently with a dystocic delivery (83.3% vs. 23.3%); p = 0.001), and these patients had a higher incidence of birth injury. Patients with birth injury were delivered more frequently by forceps, and this group of patients also exhibited lower Apgar scores at one and five minutes. Forceps instrumentation was also associated with a higher maternal age (mean, SD): 33.8 (6.2) vs. 31.6 (6.3) years (p = 0.043), and induced labor was associated with a higher maternal BMI: 32.1 (6.2) vs. 30.6 (5.3) kg/m2 (p = 0.049) and dystocia: 33.3% vs. 16.4% (p = 0.003).

Table 3.
Infants’ demographic characteristics and postnatal interventions in cases and controls.
Table 4 shows the aOR for the main variables and interventions associated with birth injury. For the selection of confounders for each variable, we used causal diagrams or Bayesian networks by means of DAG (graphs and codes in Supplementary Figure S1). No true confounders for breech presentation were found, and the unadjusted OR is shown. Forceps instrumentation was adjusted for dystocic end of labor and maternal age. Dystocia was adjusted for infant birthweight, breech presentation, and induced labor. Induced labor, in turn, was adjusted for maternal BMI and neonatal birthweight. Finally, birthweight was adjusted for maternal BMI and induced labor. All these factors were independently associated with birth trauma (Table 4).

Table 4.
Variables with independent association with birth trauma (OR and aOR).
Among patients with birth trauma, four (5.2%) required hospitalization for specialized care, while none required hospitalization in the control group. One death occurred in the group of cases due to spinal cord injury, and two infants were additionally diagnosed with severe hypoxic–ischemic encephalopathy (HIE).
4. Discussion
In our setting, the incidence of birth trauma was 22.8‰ of full-term newborns, and the most frequent injuries were cephalohematoma, facial paralysis, and clavicle fracture. This incidence and distribution of injuries was similar to that reported in other developed countries [1,2,3]. Gestation control and delivery care have improved worldwide, but birth-related injury is still present, and it cannot be considered a minor problem. After adjusting for confounders, the principal risk factors associated with obstetric trauma were breech presentation, forceps instrumentation, dystocia, induced labor, and birthweight. We could not demonstrate an association between birth injury and other traditional risk factors, such as maternal age, maternal BMI, infant sex, etc.
We found the highest odds for birth trauma with breech presentation (Table 4), although with a large 95% CI due to the small number of patients with this presentation. It is well known that fetal positions other than cephalic are associated with an increased risk of birth trauma. In our study, five out of six infants in breech presentation were delivered vaginally. Overall, in vaginal deliveries, the duration of the second stage in breech was longer than in cephalic presentations, with a mean (SD) of 122 (64) vs. 74 (74) min (p = 0.155). A duration of more than 40 min and the use of epidural anesthesia have been associated with adverse neonatal outcomes in previous studies [9]. In breech deliveries, the wishes of the patient and the experience of professionals must be taken into account. External cephalic version could be an alternative to planned cesarean section in cases of single term breech fetuses, but always under strict supervision and with the possibility of performing an urgent cesarean section if necessary. The American Academy of Obstetrics and Gynecology (ACOG) recommends documenting detailed informed consent, including relaying that the risk of short-term perinatal or neonatal mortality or serious neonatal morbidity may be greater than if a cesarean delivery is planned [10].
The second most relevant risk factor in our setting was forceps instrumentation (Table 4). Previous studies have shown a higher incidence of birth injuries with the use of forceps or vacuum-assisted delivery compared with non-surgical vaginal delivery or C-section before labor [11,12,13]. In our setting, vacuum is not used, but the use of forceps is involved in around 10–12% of all deliveries, and in the present study, it was associated with a threefold increase in the risk of birth injury. Even with the use of an adequate technique, the maximum traction force exerted on the fetal cephalic pole seems to be a determining factor in the production of injuries, both in standing and sitting positions [14]. Although they are in declining use in many countries, both forceps and vacuum are considered appropriate interventions in expert hands for specific indications [15]. In cases of high risk of hypoxia/asphyxia, the benefits of instrumentation outweigh the risk of minor injuries such as lacerations to the scalp or caput. However, other, more serious injuries can be associated with instrumental delivery. During the short observation period of our study (one year), we observed no skull fractures and only two cases of subdural hemorrhage, but other authors have described an increase in intracranial hemorrhages of about three times in operative vaginal deliveries [11]. Recommendations for when to stop a forceps delivery attempt include difficulty applying the blades and lack of appreciable descent of the fetal head on each attempt after three failed pulls from a correctly applied instrument or if the baby has not been delivered after 15 to 20 min, although the latter may vary depending on local protocols [16].
Mortality related to obstetric trauma is low, and it is estimated that it contributes to less than 2% of overall neonatal mortality [17]. The only patient who died in our study was an infant with severe upper spinal cord injury after laborious traction and rotator forceps, who developed tetraplegia and lack of spontaneous respiration, with permanent dependence on mechanical ventilation. Though not always, it has been described that spinal cord injury is usually the consequence of excessive traction or rotational force on the spine during a difficult delivery [18].
Birth injuries can also occur during C-sections, but their frequency, at least for C-sections without labor, is estimated to be about half that of vaginal deliveries [19]. C-section rates have increased significantly in Western countries in recent decades, while instrumental deliveries have decreased. In the United States, for example, cesarean deliveries rose from about 23% to more than 30%, while forceps use fell from 2.1 to 0.6% during slightly over than the first decade of the present century [20]. One of the probable indications for elective C-section to avoid adverse outcomes could be an estimated fetal weight greater than 4500 g in diabetic mothers or greater than 5000 g in non-diabetic mothers [21]. In fact, it has been suggested that the decrease in major birth trauma could be related to the performance of C-sections in cases of fetal malposition, breech presentation, and/or fetal macrosomia [3,20]. Adequate control of the gestation with a timely diagnosis of risk situations is the obstetrician’s fundamental tool for shared decision making with the family. Considering the individual maternal and fetal risk factors could favor the election of the optimal method for delivery in each particular situation. The current measurements of birth injuries cannot be considered valid indicators of the quality of obstetric care due to a lack of precision and reliability. Nevertheless, the continuous monitoring and evaluation of their incidence and characteristics could be an important tool to evaluate care and influence clinical practice in a particular setting. In the long run, they could be useful in developing valid measures of quality of care, which contribute to reducing the incidence of preventable birth injuries [22].
Our study has limitations. This is a single-center study conducted over a short period of time, which could certainly limit the generalizability of our results. In our study, we could not find an association between birth trauma and some traditional risk factors, such as maternal age or maternal BMI. Perhaps the small sample size could have prevented us from detecting these associations. On the other hand, it has been recognized that birth trauma may not be visible immediately after birth, with some types of injury being diagnosed post-discharge. For example, it was previously reported that up to about 14% of clavicle fractures are diagnosed after discharge [23]. This means that the incidence of obstetric trauma in our setting could be higher than that reported in this study.
Our study has also some strengths. All maternal and infant histories during a continuous period of time were systematically reviewed, detecting all major birth injury cases and choosing controls of the same GA and sex, as close in time as possible. The strict protocolization of delivery care in our center reduces possible biases in the management derived from the attending care team. On the other hand, from the methodological point of view, we carried out a study of risk factors adjusted for possible confounding factors specific to each variable of interest, following a Bayesian method. Other studies have carried out “one fits all” adjustments, which could lead to “over-fitting” or even open up potential paths of bias in causal inference (Supplementary Figure S1) [4,5,6].
5. Conclusions
Our study showed that the incidence of birth trauma is still significant, affecting 22.8‰ of full-term singletons in our setting. The most frequent injuries were cephalohematoma, peripheral facial paralysis, and clavicular fracture. There was an independent association between birth trauma and breech presentation, dystocia, forceps instrumentation, labor induction, and infant birthweight. Early diagnosis and prevention of risk situations, along with expert and prudent management of interventional alternatives to help finalize delivery, could be essential in reducing the incidence of birth trauma. Continuous monitoring of the incidence and its characteristics is essential in order to reduce maternal–neonatal morbidity and to continuously improve the quality of care.
Supplementary Materials
This supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/future2030010/s1, Figure S1. Directed acyclic graphs (DAG) for the study of causal inference. Table S1. Sensitivity analysis carried out by the determination of the E-values for the estimated aOR and for the limit of the CI closest to the null.
Author Contributions
Conceptualization, P.C.V. and F.G.-M.R.; methodology, P.C.V. and F.G.-M.R.; software, L.U.M. and F.G.-M.R.; validation, P.C.V. and F.G.-M.R.; formal analysis, F.G.-M.R.; investigation, P.C.V., G.C.C., D.R.S., M.S.O. and M.B.L.; resources, L.U.M. and F.G.-M.R.; data curation, F.G.-M.R.; writing—original draft preparation, G.C.C. and P.C.V.; writing—review and editing, D.R.S., L.U.M., O.R.G. and F.G.-M.R.; visualization, L.U.M. and F.G.-M.R.; supervision, L.U.M. and F.G.-M.R.; project administration, D.R.S., L.U.M. and F.G.-M.R.; funding acquisition, no fundings. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was approved by the Centre’s Research Ethics Committee (number: 2021:177-1).
Informed Consent Statement
Patient informed consent was not deemed necessary due to the anonymity of the data and the non-interventional nature of the study.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Sauber-Schatz, E.K.; Markovic, N.; Weiss, H.B.; Bodnar, L.M.; Wilson, J.W.; Pearlman, M.D. Descriptive epidemiology of birth trauma in the United States in 2003. Paediatr. Perinat. Epidemiol. 2010, 24, 116–124. [Google Scholar] [CrossRef] [PubMed]
- Linder, N.; Linder, I.; Fridman, E.; Kouadio, F.; Lubin, D.; Merlob, P.; Yogev, Y.; Melamed, N. Birth trauma-risk factors and short-term neonatal outcome. J. Matern. Fetal. Neonatal Med. 2013, 26, 1491–1495. [Google Scholar] [CrossRef]
- Gupta, R.; Cabacungan, E.T. Neonatal Birth Trauma: Analysis of Yearly Trends, Risk Factors, and Outcomes. J. Pediatr. 2021, 238, 174–180.e3. [Google Scholar] [CrossRef] [PubMed]
- Textor, J.; van der Zander, B.; Gilthorpe, M.S.; Liśkiewicz, M.; Ellison, G.T. Robust causal inference using directed acyclic graphs: The R package ‘dagitty’. Int. J. Epidemiol. 2016, 45, 1887–1894. [Google Scholar] [CrossRef] [PubMed]
- Pearl, J. An introduction to causal inference. Int. J. Biostat. 2010, 6. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mathur, M.B.; Ding, P.; Riddell, C.A.; VanderWeele, T.J. Web Site and R Package for Computing E-values. Epidemiology 2018, 29, e45–e47. [Google Scholar] [CrossRef]
- VanderWeele, T.J.; Ding, P. Sensitivity Analysis in Observational Research: Introducing the E-Value. Ann. Intern. Med. 2017, 167, 268–274. [Google Scholar] [CrossRef]
- VanderWeele, T.; Ding, P.; Mathur, M. Technical Considerations in the Use of the E-Value. J. Causal Inference 2019, 7, 20180007. [Google Scholar] [CrossRef]
- Macharey, G.; Ulander, V.M.; Heinonen, S.; Kostev, K.; Nuutila, M.; Väisänen-Tommiska, M. Risk factors and outcomes in “well-selected” vaginal breech deliveries: A retrospective observational study. J. Perinat. Med. 2017, 45, 291–297. [Google Scholar] [CrossRef] [PubMed]
- ACOG Committee Opinion No. 745: Mode of Term Singleton Breech Delivery. Obstet. Gynecol. 2018, 132, e60–e63. [CrossRef] [PubMed]
- Towner, D.; Castro, M.A.; Eby-Wilkens, E.; Gilbert, W.M. Effect of mode of delivery in nulliparous women on neonatal intracranial injury. N. Engl. J. Med. 1999, 341, 1709–1714. [Google Scholar] [CrossRef] [PubMed]
- Demissie, K.; Rhoads, G.G.; Smulian, J.C.A.; Balasubramanian, B.; Gandhi, K.; Joseph, K.S.; Kramer, M. Operative vaginal delivery and neonatal and infant adverse outcomes: Population based retrospective analysis. BMJ 2004, 329, 24–29, Erratum in BMJ 2004, 329, 547. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Alexander, J.M.; Leveno, K.J.; Hauth, J.; Landon, M.B.; Thom, E.; Spong, C.Y.; Varner, M.W.; Moawad, A.H.; Caritis, S.N.; Harper, M.; et al. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Fetal injury associated with cesarean delivery. Obstet. Gynecol. 2006, 108, 885–890. [Google Scholar] [CrossRef] [PubMed]
- Leslie, K.K.; Dipasquale-Lehnerz, P.; Smith, M. Obstetric forceps training using visual feedback and the isometric strength testing unit. Obstet. Gynecol. 2005, 105, 377–382. [Google Scholar] [CrossRef] [PubMed]
- Committee on Practice Bulletins—Obstetrics. ACOG Practice Bulletin No. 154 Summary: Operative Vaginal Delivery. Obstet. Gynecol. 2015, 126, 1118–1119. [Google Scholar] [CrossRef] [PubMed]
- Edozien, L.C. Towards safe practice in instrumental vaginal delivery. Best Pract. Res. Clin. Obstet. Gynaecol. 2007, 21, 639–655. [Google Scholar] [CrossRef] [PubMed]
- Reichard, R. Birth injury of the cranium and central nervous system. Brain Pathol. 2008, 18, 565–570. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lee, C.C.; Chou, I.J.; Chang, Y.J.; Chiang, M.C. Unusual Presentations of Birth Related Cervical Spinal Cord Injury. Front. Pediatr. 2020, 8, 514. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Baskett, T.F.; Allen, V.M.; O’connell, C.M.; Allen, A.C. Fetal trauma in term pregnancy. Am. J. Obstet. Gynecol. 2007, 197, e1–e7. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, B.E.; Martin, J.A.; Osterman, M.J.; Curtin, S.C.; Mathews, T.J. Births: Final Data for 2014. Natl. Vital. Stat. Rep. 2015, 64, 1–64. [Google Scholar] [PubMed]
- Macrosomia: ACOG Practice Bulletin Summary, Number 216. Obstet. Gynecol. 2020, 135, 246–248. [CrossRef] [PubMed]
- Kumar, P.; Papile, L.A.; Watterberg, K. Are current measures of neonatal birth trauma valid indicators of quality of care? J. Perinatol. 2015, 35, 903–906. [Google Scholar] [CrossRef] [PubMed]
- Ahn, E.S.; Jung, M.S.; Lee, Y.K.; Ko, S.Y.; Shin, S.M.; Hahn, M.H. Neonatal clavicular fracture: Recent 10 year study. Pediatr. Int. 2015, 57, 60–63. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).