Abstract
Background: Spontaneous rupture of the liver capsule secondary to the progression of hepatocellular carcinoma is a rare complication with high mortality. Case Description: This article presents the case of a 73-year-old male with no prior HCC diagnosis who presents acute abdominal pain and hemodynamic instability. Computed tomography reveals a heterogeneous liver lesion with capsular rupture and hemoperitoneum. Discussion: Management strategies focus on hemodynamic stabilization and bleeding control through transcatheter arterial embolization (TAE), surgical hemostasis or liver resection, the treatment selection is based on disease severity and patient condition. Conclusions: This case highlights the importance of considering HCC rupture in patients with acute abdominal pain and risk factors for liver disease, as early recognition and appropriate intervention significantly impact survival outcomes.
1. Introduction
Hepatocellular carcinoma (HCC) is the fifth most frequently diagnosed cancer and the most common histological type (90%) of malignant liver tumor [1,2]. It is also the fourth most prevalent cause of cancer-related death [3]. Spontaneous capsular rupture is a rare complication of HCC, with a high mortality rate [4,5]. In Western European countries, the incidence is estimated to be less than 3% [4]. This article presents the case of a 73-year-old male with an unknown history of HCC who presented to an Emergency Department (ED) for abdominal pain. We discuss the risk factors for spontaneous capsular rupture, its associated symptoms, and management options for this rare yet often fatal oncological complication.
2. Case
A 73-year-old male patient presented to the Emergency Department (ED) complaining of left parasternal chest pain, which was of sudden onset and exacerbated by the slightest movement. The patient reported two episodes of malaise, neither of which resulted in loss of consciousness, and each episode was preceded by palpitations and profuse sweating. The patient’s past medical history revealed a preserved ejection fraction, heart failure, essential hypertension, and polyneuropathy of the lower limbs. The patient also reported a history of alcohol abuse. At the time of triage, the patient was hypotensive (mean arterial pressure: 47 mmHg), normocardic (74 beats per minute), and had an oxygen saturation of 97% in room-air conditions. Given these parameters and the symptoms presented, the patient was transferred to the resuscitation bay.
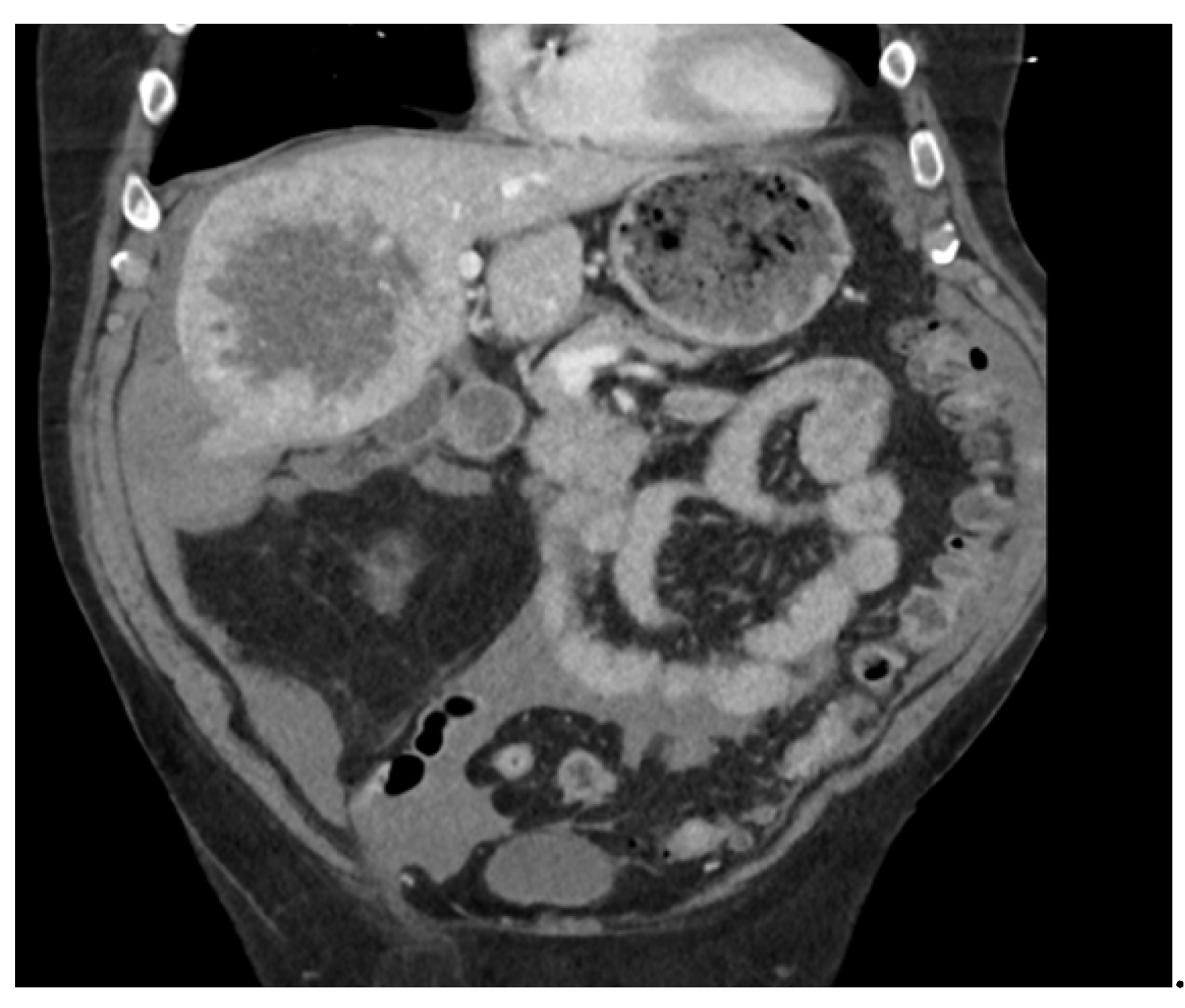
Physical examination revealed an abdominal tenderness in the right hypochondrium, with no indications of peritonism. Paraclinical investigations, including electrocardiography and blood tests, were conducted within three hours of pain onset and showed no evidence of acute coronary syndrome, with troponin I levels at 34 ng/L and lactate levels at 0.9 mmol/L. The patient also exhibited normal levels of creatinine (115 µmol/L), direct bilirubin (3.3 µmol/L), C-reactive protein (6.6 mg/L), and aspartate and alanine aminotransferases. An abdominal computed tomography (CT) scan was performed to rule out aortic dissection and mesenteric ischemia, among other potential diagnoses. The CT scan revealed a voluminous heterogeneous lesion of the right liver measuring 145 × 100 × 100 mm, with a necrotic component in contact with the capsule, and capsular rupture associated with hemoperitoneum. There were no signs of active bleeding. In light of these findings, a diagnosis of hepatocellular carcinoma (HCC) with a ruptured capsule was established (see Figure 1 and Figure 2).

Figure 1.
Axial section of the abdominal CT scan.
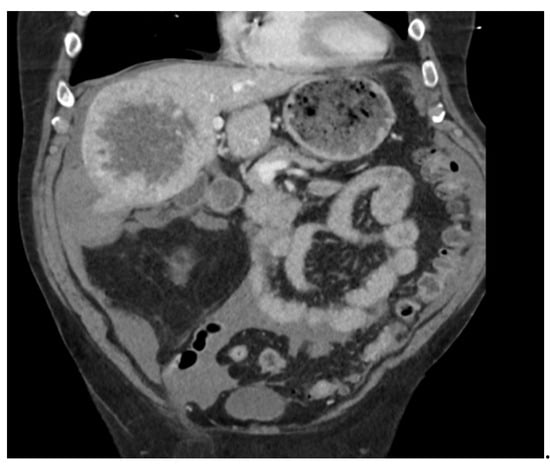
Figure 2.
Coronal section of the abdominal CT scan.
A second hemoglobin test yielded a negative delta of 22 g/L (121 to 99 g/L), indicating active bleeding. Furthermore, a disturbance in hemostasis (INR 1.22) was detected, suggesting acute liver failure. In the absence of a radiologist who could provide a second opinion, the patient was transferred to the nearest tertiary referral center for further evaluation. At this center, diagnostic angiography revealed a liver tumor measuring 14 cm in diameter at its greatest axis. As there was no active bleeding, the patient was kept under nil-by-mouth conditions and observed, with no additional invasive procedures. The patient received his first dose of chemotherapy 48 h after admission, and coiled embolization followed by selective internal radiotherapy was also performed. There was no further deterioration, and the patient was discharged with an outpatient oncological follow-up.
3. Discussion
The initial presentation of non-ruptured HCC is frequently asymptomatic, with symptoms manifesting only when the disease progresses [4]. These symptoms include diffuse abdominal pain, typically located on the right side of the patient’s abdomen. As the disease advances, symptoms such as icterus, weight loss, loss of appetite, and asthenia may become evident [4]. Spontaneous capsular rupture as a consequence of HCC progression is a rare phenomenon; a retrospective study of 1451 HCC patients identified 57 cases (3.9%) of spontaneous rupture [1]. This complication is associated with a high mortality rate caused by often difficult-to-control hemorrhaging. This condition is frequently diagnosed late due to the absence of symptoms in the early phase of the disease, particularly for patients with no known progressive cirrhosis [6]. The prognosis for HCC that has ruptured is worse than for non-ruptured cases. This is due to the greater extent of intraperitoneal hemorrhaging observed with the ruptured capsules [7]. It is noteworthy that spontaneous capsular rupture ranks as the third leading cause of death among HCC patients, surpassed only by tumor progression and liver failure [4,8,9].
Several predisposing risk factors have been identified, the most common of which are obesity, tumor location, the presence of single tumors, tumor size > 5 cm at diagnosis, portal vein thrombosis, hypertension, and extrahepatic extension of oncological disease [2,4,9]. The literature on the subject is inconclusive about whether concomitant cirrhosis should be considered a risk factor [1,10]. Regarding tumor location, studies have shown that more centrally located tumors have a lower risk of rupturing, whereas those in the left liver (caudate lobe) or subcapsular region present a higher risk [6,10,11]. Capsular rupture has also been observed in the wake of the implementation of specific therapeutic interventions for HCC. The underlying pathophysiological mechanism responsible for this complication remains to be elucidated. Sorafenib (a multi-kinase inhibitor) and trans-arterial chemoembolization are the most prevalent treatment modalities [10]. Table 1 provides a comprehensive overview of the various risk factors associated with capsular rupture.

Table 1.
Risk factors associated with liver capsule rupture in HCC.
In the event of capsular rupture, most cases present with acute abdominal pain [8]. This pain is characterized by a sudden onset, intense discomfort, and a throbbing sensation, typically localized in the right hypochondrium. It may also radiate to the right shoulder due to diaphragmatic irritation. Additional symptoms may include abdominal guarding and signs of peritonism, often accompanied by nausea and vomiting. Fever is reported in some cases, with no evidence of concomitant infection, and anemia may be detected during initial investigations [10]. Unless treated, most cases progress to hemorrhagic shock [5,8], and signs of liver failure may appear at a later stage, indicating an unfavorable prognosis [10]. The diagnosis of this condition primarily depends on imaging procedures, with abdominal CT scanning with contrast injection being the preferred modality [1]. This approach allows visualization of the tumor, hemoperitoneum, and extravasation of the contrast medium, indicating active bleeding [1]. Ultrasound also plays a pivotal role in the rapid and early detection of hemoperitoneum. It can be performed before hospital arrival or upon arrival at the ED. The clinical picture is often paucisymptomatic and unspecific, and due to the rarity of this diagnosis, it is frequently excluded from the differential diagnosis, particularly if the patient does not have a known history of HCC.
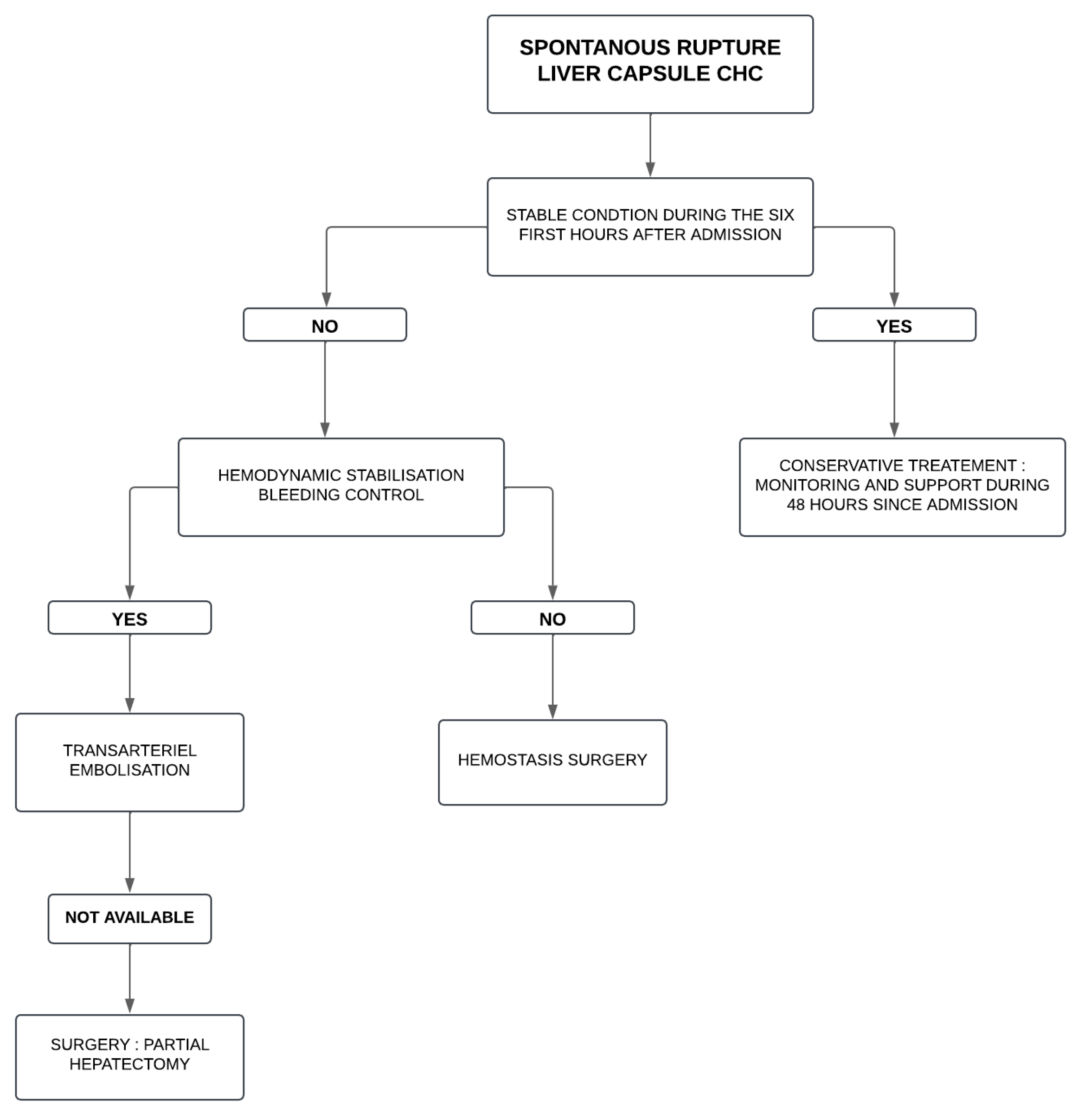
Initial patient management consists of restoring hemodynamic stability—with the administration of volemic resuscitation—and bleeding control. The management of hemorrhagic shock and specific HCC treatment are beyond the scope of this article. Once the patient has been stabilized, the following treatment options may be considered to halt the progression of the active bleeding caused by the capsular rupture. These include transcatheter arterial embolization (TAE), hemostasis surgery, and liver resection [1]. In two recent studies by Kang et al. and Kirihata et al., the two reference treatments were TAE followed by surgery [6,7]. Other treatments cited in the literature include radiofrequency or Yttrium-90 embolization, cryosurgery, and percutaneous ethanol injection (PEI) [10]. Current data do not allow for any conclusions to be drawn regarding the benefits of these treatments. Treatment choice depends on the severity of the clinical picture, the progression of the oncological disease, and the patient’s general condition. A conservative attitude can be advisable based on hemodynamic, clinical, and biological monitoring [10]. In the event of deterioration during the initial phase—arbitrarily set at between 6 and 48 h after the onset of capsular rupture—TAE is frequently the primary treatment if the patient is hemodynamically stable [11]. The serum bilirubin level, the presence of shock, liver deficiency, and tumor characteristics have been identified as prognostic factors for survival following TAE [6]. When TAE is not an option, hemostatic surgery can be considered as a viable alternative. This approach involves surgical resection at a subsequent date (first-look versus definitive), contingent on the tumor’s size and extension as well as the surgeon’s expertise [8]. Liver transplantation does not seem to be a rational alternative given such patients’ generally fragile state at the time of presentation and the frequently advanced stage of the disease at the time of diagnosis [10]. As illustrated in Figure 3, a decision-making algorithm has been developed for managing liver capsule rupture in HCC progression, emphasizing the need for a multidisciplinary approach.
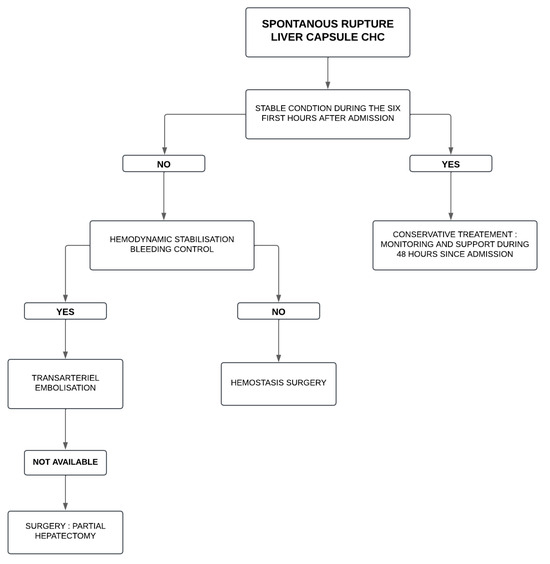
Figure 3.
Decision algorithm for managing liver capsule rupture in HCC progression.
4. Conclusions
Spontaneous capsular rupture is a rare and serious complication of hepatocellular carcinoma, which is often associated with a high mortality rate due to hemorrhaging. The case presented in this manuscript highlights the importance of considering this diagnosis for patients presenting with abrupt abdominal or chest pain, particularly in the context of an underlying liver disease or HCC risk factors. Rapid imaging and multidisciplinary management are essential to stabilize the patient and improve prognosis. Early recognition and appropriate interventions can significantly impact the patient’s survival and quality of life.
Author Contributions
H.A.S. and R.A.Z. contributed as co-authors. H.O.Z. assisted with proofreading. E.P.H. and C.S. supervised this article and participated in its writing. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study. Case report describe existing clinical data and to not pose additional risks beyond standard medical care. In addition, our institution do not require ethics approval for case reports.
Informed Consent Statement
Informed consent was obtained from the patient.
Data Availability Statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author/s.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Obeidat, A.E.; Wong, L.L. Spontaneous Rupture of Hepatocellular Carcinoma: New Insights. J. Clin. Exp. Hepatol. 2022, 12, 483–491. [Google Scholar] [CrossRef] [PubMed]
- Llovet, J.M.; Zucman-Rossi, J.; Pikarsky, E.; Sangro, B.; Schwartz, M.; Scherman, M.; Gores, G. Hepatocellular carcinoma. Nat. Rev. Dis. Primers 2016, 2, 16018. [Google Scholar] [CrossRef] [PubMed]
- Marrero, J.A.; Ahn, J.; Reddy, R.K.; on behalf of the Practice Parameters Committee of the American College of Gastroenterology. ACG clinical guideline: The diagnosis and management of focal liver lesions. Am. J. Gastroenterol. 2014, 109, 1328–1347. [Google Scholar] [CrossRef] [PubMed]
- European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2018, 69, 182–236. [Google Scholar] [CrossRef] [PubMed]
- Forner, A.; Reig, M.; Bruix, J. Hepatocellular carcinoma. Lancet 2018, 391, 1301–1314. [Google Scholar] [CrossRef] [PubMed]
- Kirihata, N.; Nakano, Y.; Moriyoshi, K.; Miyamoto, S. Ruptured hepatocellular carcinoma developed in a normal liver in a young patient with a body mass index of 33 kg/m2. BMJ Case Rep. 2024, 17, e262841. [Google Scholar] [CrossRef] [PubMed]
- Xu, K.; Ryu, D.; Choi, H.; Choi, J.-W.; Lee, J. Prognosis and recurrence of spontaneously ruptured hepatocellular carcinoma treated after hepatectomy: A single institution experience. Medicine 2024, 103, e38555. [Google Scholar] [CrossRef] [PubMed]
- Lai, E.C.; Lau, W.Y. Spontaneous rupture of hepatocellular carcinoma: A systematic review. Arch. Surg. 2006, 141, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Q.; Li, J.; Yan, J.-J.; Huang, L.; Wu, M.-C.; Yan, Y.-Q. Predictors and clinical outcomes for spontaneous rupture of hepatocellular carcinoma. World J. Gastroenterol. 2012, 18, 7302–7307. [Google Scholar] [CrossRef] [PubMed]
- Sahu, S.K.; Chawla, Y.K.; Dhiman, R.K.; Singh, V.; Duseja, A.; Taneja, S.; Kalra, N.; Gorsi, U. Rupture of Hepatocellular Carcinoma: A Review of Literature. J. Clin. Exp. Hepatol. 2019, 9, 245–256. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.L.; Fan, S.T.; Lo, C.M.; Tso, W.K.; Poon, R.T.; Lam, C.M.; Wong, J. Management of spontaneous rupture of hepatocellular carcinoma: Single-center experience. J. Clin. Oncol. 2001, 19, 3725–3732. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).