- Brief Report
Exploratory Pilot Study of Mobile Phone Use During Emergency Department Triage and Hospital Admission
- Jacopo Davide Giamello,
- Bianca Miclaus and
- Giuseppe Lauria
- + 5 authors
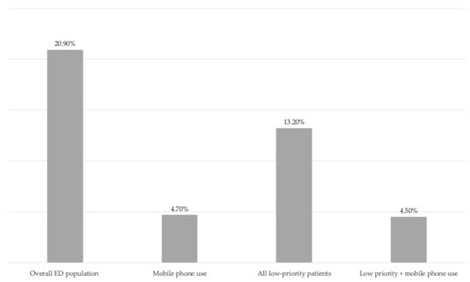
Background: Behavioural cues observed during emergency department (ED) triage may provide additional information on patient acuity. We conducted an exploratory pilot study to investigate whether mobile phone use observed during ED triage was associated with hospital admission. Methods: We performed a retrospective, single-centre study including all adult ED attendances between 1 January 2019 and 30 June 2025. Demographics, triage category, mobile phone use documented by nursing staff during waiting time, and hospital admission were extracted from the electronic health record. The primary outcome was hospital admission, with a secondary analysis restricted to low-priority triage categories. Results: Among 423,267 ED visits, the overall admission rate was 20.9%. Mobile phone use was documented in 171 patients (0.04%), of whom 4.7% were admitted (p < 0.001). In low-priority patients (n = 336,160), admission was 4.5% among those using a phone compared with 13.2% overall (p = 0.001). Conclusions: Mobile phone use observed during ED triage was associated with lower hospital admission rates and may represent a simple behavioural adjunct to conventional triage assessment.
30 January 2026