A Technological Review of Wearable Cueing Devices Addressing Freezing of Gait in Parkinson’s Disease
Abstract
:1. Introduction
- Cueing may compensate for the defective internal rhythm generator of the basal ganglia, consequently affecting the coordination and execution of movement [31,32]. In this way, the PwP may use auditory, visual or somatosensory cueing to provide temporal information (external rhythm) to which movement can be coupled [33].
- Another theory is that the PwP may use visual cueing to provide spatial information to scale and guide movements, which may allow the PwP to bypass their defective basal ganglia during gait [34].
- Previous studies also have suggested that cognitive/attentional mechanisms might explain the positive effects of cueing on FoG. Namely, auditory, visual or somatosensory cueing may shift the PwP’s attention to the task of walking, helping them to consciously think of what to do next [35].
- Studies indicate that enhanced proprioceptive information processing could be the mechanism underlying the positive effects of cueing on FoG. In this way, the PwP may use visual or somatosensory cueing as an artificial means to stimulate the proprioceptive inputs, providing enhanced information on limb position and movement during gait [36].
- Immediate cueing: the majority of studies have investigated the immediate effect of cueing on FoG [36,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59]. These studies predominantly evaluated the effect of cueing over a single session of use, with the objective of the cueing being to provide an immediate benefit in terms a reduction in the number/duration of FoG episodes.
- Therapeutic cueing: a number of studies have investigated the therapeutic effect of cueing [60,61,62,63,64,65,66,67,68,69,70]. During these studies, the PwP engaged in a number of therapy sessions per week (treatment period). The cueing in this case was only delivered during the therapy sessions. These therapy sessions aimed to provide a therapeutic benefit, which ameliorated FoG when the person was walking at home or in the community without any cueing being provided.
2. Methods
2.1. Review Questions
2.2. Article Search Strategy
2.3. Article Screening
2.4. Quality Assessment
- Each outcome variable was systematically measured and an inter-observer agreement (IOA) was reported for a minimum of 20% of data for each experimental condition. The IOA score must meet or exceeded 80%.
- The study included at least three replication attempts of intervention effects at different points in time or in three different phase repetitions.
- An intervention phase met the minimal data point threshold for the design type as specified by WWC guidelines [74].
3. Results
3.1. Auditory Cueing Devices
3.2. Visual Cueing Devices
3.3. Somatosensory Stimuli Devices
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Pieter, G.; Evelien, N.; Alice, N.; Elke, H. Cueing for people with Parkinson’s disease with freezing of gait: A narrative review of the state-of-the-art and novel perspectives. Ann. Phys. Rehabil. Med. 2017. [Google Scholar] [CrossRef]
- Lim, I.; van Wegen, E.; de Goede, C.; Deutekom, M.; Nieuwboer, A.; Willems, A.; Jones, D.; Rochester, L.; Kwakkel, G. Effects of external rhythmical cueing on gait in patients with Parkinson’s disease: A systematic review. Clin. Rehabil. 2005, 19, 695–713. [Google Scholar] [CrossRef] [PubMed]
- Heremans, E.; Nieuwboer, A.; Vercruysse, S. Freezing of gait in Parkinson’s disease: Where are we now? Curr. Neurol. Neurosci. Rep. 2013, 13, 350. [Google Scholar] [CrossRef] [PubMed]
- Giladi, N.; Horak, F.B.; Hausdorff, J.M. Classification of gait disturbances: Distinguishing between continuous and episodic changes. Mov. Disord. 2013, 28, 1469–1473. [Google Scholar] [CrossRef] [PubMed]
- Moretti, R.; Torre, P.; Antonello, R.M.; Esposito, F.; Bellini, G. The on-freezing phenomenon: Cognitive and behavioral aspects. Parkinson’s Dis. 2011. [Google Scholar] [CrossRef]
- Bloem, B.R.; Hausdorff, J.M.; Visser, J.E.; Giladi, N. Falls and freezing of gait in Parkinson’s disease: A review of two interconnected, episodic phenomena. Mov. Disord. Off. J. Mov. Disord. Soc. 2004, 19, 871–884. [Google Scholar] [CrossRef]
- Hausdorff, J.M.; Balash, Y.; Giladi, N. Time series analysis of leg movements during freezing of gait in Parkinson’s disease: Akinesia, rhyme or reason? Phys. A Stat. Mech. Appl. 2003, 321, 565–570. [Google Scholar] [CrossRef]
- Schaafsma, J.D.; Balash, Y.; Gurevich, T.; Bartels, A.L.; Hausdorff, J.M.; Giladi, N. Characterization of freezing of gait subtypes and the response of each to levodopa in Parkinson’s disease. Eur. J. Neurol. 2003, 10, 391–398. [Google Scholar] [CrossRef]
- Custodio, N.; Lira, D.; Herrera-Perez, E.; Montesinos, R.; Castro-Suarez, S.; Cuenca-Alfaro, J.; Cortijo, P. Predictive model for falling in Parkinson disease patients. eNeurologicalSci 2016, 5, 20–24. [Google Scholar] [CrossRef]
- Youn, J.; Okuma, Y.; Hwang, M.; Kim, D.; Cho, J.W. Falling Direction can Predict the Mechanism of Recurrent Falls in Advanced Parkinson’s Disease. Sci. Rep. 2017, 7, 3921. [Google Scholar] [CrossRef] [Green Version]
- Okuma, Y.; de Lima, A.L.S.; Fukae, J.; Bloem, B.R.; Snijders, A.H. A prospective study of falls in relation to freezing of gait. Parkinsonism Relat. Disord. 2018, 46, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Lieberman, A.; Deep, A.; Lockhart, T. Falls in Parkinson Disease. J. Alzheimers Dis. Parkinsonism 2016, 6. [Google Scholar] [CrossRef]
- Paul, S.S.; Harvey, L.; Canning, C.G.; Boufous, S.; Lord, S.R.; Close, J.C.T.; Sherrington, C. Fall-related hospitalization in people with Parkinson’s disease. Eur. J. Neurol. 2017, 24, 523–529. [Google Scholar] [CrossRef]
- Moore, O.; Peretz, C.; Giladi, N. Freezing of gait affects quality of life of peoples with Parkinson’s disease beyond its relationships with mobility and gait. Mov. Disord. Off. J. Mov. Disord. Soc. 2007, 22, 2192–2195. [Google Scholar] [CrossRef] [PubMed]
- Redmond, L.; Suddick, K. The lived experience of freezing in people with Parkinson’s: An interpretive phenomenological approach. Int. J. Ther. Rehabil. 2012, 19, 169–177. [Google Scholar] [CrossRef]
- Rahman, S.; Griffin, H.J.; Quinn, N.P.; Jahanshahi, M. Quality of life in Parkinson’s disease: The relative importance of the symptoms. Mov. Disord. Off. J. Mov. Disord. Soc. 2008, 23, 1428–1434. [Google Scholar] [CrossRef]
- Walton, C.C.; Shine, J.M.; Hall, J.M.; O’Callaghan, C.; Mowszowski, L.; Gilat, M.; Szeto, J.Y.; Naismith, S.L.; Lewis, S.J. The major impact of freezing of gait on quality of life in Parkinson’s disease. J. Neurol. 2015, 262, 108–115. [Google Scholar] [CrossRef]
- Ishii, M.; Okuyama, K. Characteristics associated with freezing of gait in actual daily living in Parkinson’s disease. J. Phys. Ther. Sci. 2017, 29, 2151–2156. [Google Scholar] [CrossRef] [Green Version]
- Ishii, M.; Okuyama, K. Influence of Freezing of Gait on Quality of Life in Patients with Parkinson’s disease. J. Fac. Health Sci. 2018, 12, 1–10. [Google Scholar]
- Sarbaz, Y.; Gharibzadeh, S.; Towhidkhah, F. Pathophysiology of freezing of gait and some possible treatments for it. Med. Hypotheses 2012, 78, 258–261. [Google Scholar] [CrossRef]
- Nonnekes, J.; Snijders, A.H.; Nutt, J.G.; Deuschl, G.; Giladi, N.; Bloem, B.R. Freezing of gait: A practical approach to management. Lancet Neurol. 2015, 14, 768–778. [Google Scholar] [CrossRef]
- Zhang, L.L.; Canning, S.D.; Wang, X.P. Freezing of gait in Parkinsonism and its potential drug treatment. Curr. Neuropharmacol. 2016, 14, 302. [Google Scholar] [CrossRef]
- Amboni, M.; Stocchi, F.; Abbruzzese, G.; Morgante, L.; Onofrj, M.; Ruggieri, S.; Tinazzi, M.; Zappia, M.; Attar, M.; Colombo, D.; et al. Prevalence and associated features of self-reported freezing of gait in Parkinson disease: The DEEP FOG study. Parkinsonism Relat. Disord. 2015, 21, 644–649. [Google Scholar] [CrossRef]
- Manson, A.; Stirpe, P.; Schrag, A. Levodopa-induced-dyskinesias clinical features, incidence, risk factors, management and impact on quality of life. J. Parkinson’s Dis. 2012, 2, 189–198. [Google Scholar]
- Chang, F.C.; Tsui, D.S.; Mahant, N.; Wolfe, N.; Kim, S.D.; Ha, A.D.; Drury, M.; Griffith, J.M.; Fung, V.S. 24 h Levodopa–carbidopa intestinal gel may reduce falls and “unresponsive” freezing of gait in Parkinson’s disease. Parkinsonism Relat. Disord. 2015, 21, 317–320. [Google Scholar] [CrossRef]
- Valentino, F.; Cosentino, G.; Brighina, F.; Pozzi, N.G.; Sandrini, G.; Fierro, B.; Savettieri, G.; D’amelio, M.; Pacchetti, C. Transcranial direct current stimulation for treatment of freezing of gait: A cross-over study. Mov. Disord. 2014, 29, 1064–1069. [Google Scholar] [CrossRef] [Green Version]
- Thevathasan, W.; Cole, M.H.; Graepel, C.L.; Hyam, J.A.; Jenkinson, N.; Brittain, J.S.; Coyne, T.J.; Silburn, P.A.; Aziz, T.Z.; Kerr, G.; et al. A spatiotemporal analysis of gait freezing and the impact of pedunculopontine nucleus stimulation. Brain 2012, 135, 1446–1454. [Google Scholar] [CrossRef] [Green Version]
- Rubinstein, T.C.; Giladi, N.; Hausdorff, J.M. The power of cueing to circumvent dopamine deficits: A review of physical therapy treatment of gait disturbances in Parkinson’s disease. Mov. Disord. Off. J. Mov. Disord. Soc. 2002, 17, 1148–1160. [Google Scholar] [CrossRef]
- Nieuwboer, A.; Kwakkel, G.; Rochester, L.; Jones, D.; van Wegen, E.; Willems, A.M.; Chavret, F.; Hetherington, V.; Baker, K.; Lim, I. Cueing training in the home improves gait-related mobility in Parkinson’s disease: The RESCUE trial. J. Neurol. Neurosurg. Psychiatry 2007, 78, 134–140. [Google Scholar] [CrossRef]
- Espay, A.J.; Fasano, A.; Van Nuenen, B.F.L.; Payne, M.M.; Snijders, A.H.; Bloem, B.R. “On” state freezing of gait in Parkinson disease a paradoxical levodopa-induced complication. Neurology 2012, 78, 454–457. [Google Scholar] [CrossRef]
- Azulay, J.P.; Mesure, S.; Amblard, B.; Blin, O.; Sangla, I.; Pouget, J. Visual control of locomotion in Parkinson’s disease. Brain 1999, 122, 111–120. [Google Scholar] [CrossRef]
- Burleigh-Jacobs, A.; Horak, F.B.; Nutt, J.G.; Obeso, J.A. Step initiation in Parkinson’s disease: Influence of levodopa and external sensory triggers. Mov. Disord. 1997, 12, 206–215. [Google Scholar] [CrossRef]
- Janssen, S.; Bolte, B.; Nonnekes, J.; Bittner, M.; Bloem, B.R.; Heida, T.; Zhao, Y.; van Wezel, R.J. Usability of three-dimensional augmented visual cues delivered by smart glasses on (freezing of) gait in Parkinson’s disease. Front. Neurol. 2017, 8, 279. [Google Scholar] [CrossRef]
- Glickstein, M.; Stein, J. Paradoxical movement in Parkinson’s disease. Trends Neurosci. 1991, 14, 480–482. [Google Scholar] [CrossRef]
- Nieuwboer, A. Cueing for freezing of gait in patients with Parkinson’s disease: A rehabilitation perspective. Mov. Disord. Off. J. Mov. Disord. Soc. 2008, 23, S475–S481. [Google Scholar] [CrossRef]
- Pereira, M.P.; Gobbi, L.T.; Almeida, Q.J. Freezing of gait in Parkinson’s disease: Evidence of sensory rather than attentional mechanisms through muscle vibration. Parkinsonism Relat. Disord. 2016, 29, 78–82. [Google Scholar] [CrossRef]
- Dietz, M.A.; Goetz, C.G.; Stebbins, G.T. Evaluation of a modified inverted walking stick as a treatment for parkinsonian freezing episodes. Mov. Disord. Off. J. Mov. Disord. Soc. 1990, 5, 243–247. [Google Scholar] [CrossRef]
- Enzensberger, W.; Oberländer, U.; Stecker, K. Metronome therapy in patients with Parkinson disease. Der. Nervenarzt 1997, 68, 972–977. [Google Scholar] [CrossRef]
- Cubo, E.; Leurgans, S.; Goetz, C.G. Short-term and practice effects of metronome pacing in Parkinson’s disease patients with gait freezing while in the ‘on’state: Randomized single blind evaluation. Parkinsonism Relat. Disord. 2004, 10, 507–510. [Google Scholar] [CrossRef]
- Kompoliti, K.; Goetz, C.G.; Leurgans, S.; Morrissey, M.; Siegel, I.M. “On” freezing in Parkinson’s disease: Resistance to visual cue walking devices. Mov. Disord. Off. J. Mov. Disord. Soc. 2000, 15, 309–312. [Google Scholar] [CrossRef]
- Brichetto, G.; Pelosin, E.; Marchese, R.; Abbruzzese, G. Evaluation of physical therapy in parkinsonian patients with freezing of gait: A pilot study. Clin. Rehabil. 2006, 20, 31–35. [Google Scholar] [CrossRef] [PubMed]
- Buated, W.; Sriyudthsak, M.; Sribunruangrit, N.; Bhidayasiri, R. A low-cost intervention for improving gait in Parknson’s disease patients: A cane providing visual cues. Eur. Geriatr. Med. 2012, 3, 126–130. [Google Scholar] [CrossRef]
- Bryant, M.S.; Rintala, D.H.; Lai, E.C.; Protas, E.J. A pilot study: Influence of visual cue color on freezing of gait in persons with Parkinson’s disease. Disabil. Rehabil. Assist. Technol. 2010, 5, 456–461. [Google Scholar] [CrossRef]
- Arias, P.; Cudeiro, J. Effect of rhythmic auditory stimulation on gait in Parkinsonian patients with and without freezing of gait. PLoS ONE 2010, 5, e9675. [Google Scholar] [CrossRef]
- McCandless, P.J.; Evans, B.J.; Janssen, J.; Selfe, J.; Churchill, A.; Richards, J. Effect of three cueing devices for people with Parkinson’s disease with gait initiation difficulties. Gait Posture 2016, 44, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Sijobert, B.; Azevedo-Coste, C.; Andreu, D.; Verna, C.; Geny, C. Effects of sensitive electrical stimulation based cueing in Parkinson’s disease: A preliminary study. Eur. J. Transl. Myol. 2016, 26. [Google Scholar] [CrossRef] [PubMed]
- Sijobert, B.; Azevedo, C.; Andreu, D.; Verna, C.; Geny, C. Effects of Sensitive Electrical Stimulation-Based Somatosensory Cueing in Parkinson’s Disease Gait and Freezing of Gait Assessment. Artif. Organs 2017, 41, E222–E232. [Google Scholar] [CrossRef]
- Zhao, Y.; Nonnekes, J.; Storcken, E.J.; Janssen, S.; van Wegen, E.E.; Bloem, B.R.; Dorresteijn, L.D.; van Vugt, J.P.; Heida, T.; van Wezel, R.J. Feasibility of external rhythmic cueing with the Google Glass for improving gait in people with Parkinson’s disease. J. Neurol. 2016, 263, 1156–1165. [Google Scholar] [CrossRef] [Green Version]
- Bunting-Perry, L.; Spindler, M.; Robinson, K.M.; Noorigian, J.; Cianci, H.J.; Duda, J.E. Laser light visual cueing for freezing of gait in Parkinson disease: A pilot study with male participants. J. Rehabil. Res. Dev. 2013, 50, 223–231. [Google Scholar] [CrossRef]
- Lee, S.J.; Yoo, J.Y.; Ryu, J.S.; Park, H.K.; Chung, S.J. The effects of visual and auditory cues on freezing of gait in patients with Parkinson disease. Am. J. Phys. Med. Rehabil. 2012, 91, 2–11. [Google Scholar] [CrossRef]
- Barthel, C.; Nonnekes, J.; van Helvert, M.; Haan, R.; Janssen, A.; Delval, A.; Weerdesteyn, V.; Debû, B.; van Wezel, R.; Bloem, B.R.; et al. The laser shoes: A new ambulatory device to alleviate freezing of gait in Parkinson disease. Neurology 2017, 90, e164–e171. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.H.; Liou, D.J.; Liou, K.C.; Liang, J.L.; Cheng, S.J.; Shaw, J.S. Walking Turns in Parkinson’s Disease Patients with Freezing of Gait: The Short-term Effects of Different Cueing Strategies. Int. J. Gerontol. 2016, 10, 71–75. [Google Scholar] [CrossRef]
- Spildooren, J.; Vercruysse, S.; Meyns, P.; Vandenbossche, J.; Heremans, E.; Desloovere, K.; Vandenberghe, W.; Nieuwboer, A. Turning and unilateral cueing in Parkinson’s disease patients with and without freezing of gait. Neurosciece 2012, 207, 298–306. [Google Scholar] [CrossRef] [PubMed]
- Rosenthal, L.; Sweeney, D.; Cunnington, A.L.; Quinlan, L.R.; ÓLaighin, G. Sensory Electrical Stimulation Cueing May Reduce Freezing of Gait Episodes in Parkinson’s Disease. J. Healthc. Eng. 2018. [Google Scholar] [CrossRef] [PubMed]
- Tang, L.; Gao, C.; Wang, D.; Liu, A.; Chen, S.; Gu, D. Rhythmic laser cue is beneficial for improving gait performance and reducing freezing of turning in Parkinson’s disease patients with freezing of gait. Int. J. Clin. Exp. Med. 2017, 10, 16802–16808. [Google Scholar]
- Ahn, D.; Chung, H.; Lee, H.W.; Kang, K.; Ko, P.W.; Kim, N.S.; Park, T. Smart gait-aid glasses for Parkinson’s disease patients. IEEE Trans. Biomed. Eng. 2017, 64, 2394–2402. [Google Scholar] [CrossRef] [PubMed]
- Donovan, S.; Lim, C.; Diaz, N.; Browner, N.; Rose, P.; Sudarsky, L.R.; Tarsy, D.; Fahn, S.; Simon, D.K. Laserlight cues for gait freezing in Parkinson’s disease: An open-label study. Parkinsonism Relat. Disord. 2011, 17, 240–245. [Google Scholar] [CrossRef]
- Spildooren, J.; Vercruysse, S.; Heremans, E.; Galna, B.; Verheyden, G.; Vervoort, G.; Nieuwboer, A. Influence of cueing and an attentional strategy on freezing of gait in Parkinson disease during turning. J. Neurol. Phys. Ther. 2017, 41, 129–135. [Google Scholar] [CrossRef]
- Young, W.R.; Shreve, L.; Quinn, E.J.; Craig, C.; Bronte-Stewart, H. Auditory cueing in Parkinson’s patients with freezing of gait. What matters most: Action-relevance or cue-continuity? Neuropsychologia 2016, 87, 54–62. [Google Scholar] [CrossRef]
- Plotnik, M.; Shema, S.; Dorfman, M.; Gazit, E.; Brozgol, M.; Giladi, N.; Hausdorff, J.M. A motor learning-based intervention to ameliorate freezing of gait in subjects with Parkinson’s disease. J. Neurol. 2014, 261, 1329–1339. [Google Scholar] [CrossRef]
- Espay, A.J.; Baram, Y.; Dwivedi, A.K.; Shukla, R.; Gartner, M.; Gaines, L.; Duker, A.P.; Revilla, F.J. At-home training with closed-loop augmented-reality cueing device for improving gait in patients with Parkinson disease. J. Rehabil. Res. Dev. 2010, 47, 573–583. [Google Scholar] [CrossRef] [PubMed]
- Kadivar, Z.; Corcos, D.M.; Foto, J.; Hondzinski, J.M. Effect of step training and rhythmic auditory stimulation on functional performance in Parkinson patients. Neurorehabil. Neural Repair 2011, 25, 626–635. [Google Scholar] [CrossRef] [PubMed]
- Murgia, M.; Pili, R.; Corona, F.; Sors, F.; Agostini, T.A.; Bernardis, P.; Casula, C.; Cossu, G.; Guicciardi, M.; Pau, M. The Use of Footstep Sounds as rhythmic auditory Stimulation for Gait rehabilitation in Parkinson’s Disease: A randomized Controlled Trial. Front. Neurol. 2018, 9. [Google Scholar] [CrossRef] [PubMed]
- Martin, T.; Weatherall, M.; Anderson, T.J.; MacAskill, M.R. A randomized controlled feasibility trial of a specific cueing program for falls management in persons with Parkinson disease and freezing of gait. J. Neurol. Phys. Ther. 2015, 39, 179–184. [Google Scholar] [CrossRef] [PubMed]
- Morris, M.E.; Iansek, R.; Kirkwood, B. A randomized controlled trial of movement strategies compared with exercise for people with Parkinson’s disease. Mov. Disord. 2009, 24, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Frazzitta, G.; Pezzoli, G.; Bertotti, G.; Maestri, R. Asymmetry and freezing of gait in parkinsonian patients. J. Neurol. 2013, 260, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Frazzitta, G.; Bertotti, G.; Riboldazzi, G.; Turla, M.; Uccellini, D.; Boveri, N.; Guaglio, G.; Perini, M.; Comi, C.; Balbi, P.; et al. Effectiveness of intensive inpatient rehabilitation treatment on disease progression in parkinsonian patients: A randomized controlled trial with 1-year follow-up. Neurorehabil. Neural Repair 2012, 26, 144–150. [Google Scholar] [CrossRef] [PubMed]
- Frazzitta, G.; Abbruzzese, G.; Bertotti, G.; Boveri, N.; Pezzoli, G.; Maestri, R. Effectiveness of an intensive rehabilitation treatment on different Parkinson’s disease subtypes. NeuroRehabilitation 2013, 33, 299–303. [Google Scholar]
- Fietzek, U.M.; Schroeteler, F.E.; Ziegler, K.; Zwosta, J.; Ceballos-Baumann, A.O. Randomized cross-over trial to investigate the efficacy of a two-week physiotherapy programme with repetitive exercises of cueing to reduce the severity of freezing of gait in patients with Parkinson’s disease. Clin. Rehabil. 2014, 28, 902–911. [Google Scholar] [CrossRef]
- Georgy, E.; Barsnley, S.; Chellappa, R. Effect of physical exercise-movement strategies programme on mobility, falls, and quality of life in Parkinson’s disease. Int. J. Ther. Rehabil. 2012, 19, 88–96. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The prisma statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef] [PubMed]
- Wendt, O.; Miller, B. Quality appraisal of single-subject experimental designs: An overview and comparison of different appraisal tools. Educ. Treat. Child. 2012, 35, 235–268. [Google Scholar] [CrossRef]
- Lobo, M.A.; Moeyaert, M.; Cunha, A.B.; Babik, I. Single-case design, analysis, and quality assessment for intervention research. J. Neurol. Phys. Ther. JNPT 2017, 41, 187. [Google Scholar] [CrossRef] [PubMed]
- Kratochwill, T.R.; Hitchcock, J.; Horner, R.H.; Levin, J.R.; Odom, S.L.; Rindskopf, D.M.; Shadish, W.R. Single-case designs technical documentation. In What Works Clearinghouse; ERIC: Seoul, Korea, 2010. [Google Scholar]
- Bächlin, M.; Plotnik, M.; Roggen, D.; Giladi, N.; Hausdorff, J.M.; Tröster, G. A wearable system to assist walking of Parkinson s disease patients. Methods Inf. Med. 2010, 49, 88–95. [Google Scholar]
- Bachlin, M.; Plotnik, M.; Roggen, D.; Maidan, I.; Hausdorff, J.M.; Giladi, N.; Troster, G. Wearable assistant for Parkinson’s disease patients with the freezing of gait symptom. IEEE Trans. Inf. Technol. Biomed. 2010, 14, 436–446. [Google Scholar] [CrossRef] [PubMed]
- Moore, S.T.; MacDougall, H.G.; Ondo, W.G. Ambulatory monitoring of freezing of gait in Parkinson’s disease. J. Neurosci. Methods 2008, 167, 340–348. [Google Scholar] [CrossRef] [PubMed]
- Whittle, M.W. Gait Analysis: An Introduction; Elselvier: Edinburgh, UK, 2007. [Google Scholar]
- Baram, Y.; Miller, A. Virtual reality cues for improvement of gait in patients with multiple sclerosis. Neurology 2006, 66, 178–181. [Google Scholar] [CrossRef] [PubMed]
- Ghai, S.; Ghai, I.; Schmitz, G.; Effenberg, A.O. Effect of rhythmic auditory cueing on parkinsonian gait: A systematic review and meta-analysis. Sci. Rep. 2018, 8, 506. [Google Scholar] [CrossRef] [Green Version]
- Willems, A.M.; Nieuwboer, A.; Chavret, F.; Desloovere, K.; Dom, R.; Rochester, L.; Jones, D.; Kwakkel, G.; Van Wegen, E. The use of rhythmic auditory cues to influence gait in patients with Parkinson’s disease, the differential effect for freezers and non-freezers, an explorative study. Disabil. Rehabil. 2006, 28, 721–728. [Google Scholar] [CrossRef]
- Samà, A.; Pérez-López, C.; Rodríguez-Martín, D.; Moreno-Aróstegui, J.M.; Rovira, J.; Ahlrichs, C.; Castro, R.; Cevada, J.; Graça, R.; Guimarães, V.; et al. A double closed loop to enhance the quality of life of Parkinson’s Disease patients: REMPARK system. Innov. Med. Healthc. 2015, 207, 115–124. [Google Scholar]
- Ahlrichs, C.; Samà, A.; Lawo, M.; Cabestany, J.; Rodríguez-Martín, D.; Pérez-López, C.; Sweeney, D.; Quinlan, L.R.; Laighin, G.Ò.; Counihan, T.; et al. Detecting freezing of gait with a tri-axial accelerometer in Parkinson’s disease patients. Med. Biol. Eng. Comput. 2016, 54, 223–233. [Google Scholar] [CrossRef]
- Nunes, F.; Silva, P.A.; Cevada, J.; Barros, A.C.; Teixeira, L. User interface design guidelines for smartphone applications for people with Parkinson’s disease. Univ. Access Inf. Soc. 2016, 15, 659–679. [Google Scholar] [CrossRef]
- Mazilu, S.; Blanke, U.; Dorfman, M.; Gazit, E.; Mirelman, A.; Hausdorff, J.M.; Tröster, G. A wearable assistant for gait training for Parkinson’s disease with freezing of gait in out-of-the-lab environments. ACM Trans. Interact. Intell. Syst. 2015, 5, 5. [Google Scholar] [CrossRef]
- Mazilu, S.; Blanke, U.; Hardegger, M.; Troster, G.; Gazit, E.; Dorfman, M.; Hausdorff, J.M. GaitAssist: A wearable assistant for gait training and rehabilitation in Parkinson’s disease. In Proceedings of the 2014 IEEE International Conference on Pervasive Computing and Communications Workshops (PERCOM Workshops), Budapest, Hungary, 24–28 March 2014; pp. 135–137. [Google Scholar]
- Baram, Y.; Aharon-Peretz, J.; Simionotici, Y.; Ron, L. Walking on virtual tiles. Neural Proc. Lett. 2002, 16, 227–233. [Google Scholar] [CrossRef]
- Giladi, N.; Shabtai, H.; Simon, E.S.; Biran, S.; Tal, J.; Korczyn, A.D. Construction of freezing of gait 1296 questionnaire for patients with Parkinsonism. Parkinsonism Relat. Disord. 2000, 6, 165–170. [Google Scholar] [CrossRef]
- Ferrarin, M.; Brambilla, M.; Garavello, L.; Di Candia, A.; Pedotti, A.; Rabuffetti, M. Microprocessor-controlled optical stimulating device to improve the gait of patients with Parkinson’s disease. Med. Biol. Eng. Comput. 2004, 42, 328–332. [Google Scholar] [CrossRef] [PubMed]
- Azevedo Coste, C.; Sijobert, B.; Pissard-Gibollet, R.; Pasquier, M.; Espiau, B.; Geny, C. Detection of freezing of gait in Parkinson disease: Preliminary results. Sensors 2014, 14, 6819–6827. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar]
- Gonçalves, H.; Moreira, R.; Rodrigues, A.; Santos, C. Finding Parameters around the Abdomen for a Vibrotactile System: Healthy and Patients with Parkinson’s Disease. J. Med. Syst. 2018, 42, 232. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, H.; Minas, G.; Rodrigues, A.; Santos, C. Literature review of vibrotactile systems addressing freezing of gait in parkinsonians. In Proceedings of the 2017 IEEE International Conference on Autonomous Robot Systems and Competitions (ICARSC), Coimbra, Portugal, 26–28 April 2017; pp. 104–109. [Google Scholar]
- Mancini, M.; Smulders, K.; Harker, G.; Stuart, S.; Nutt, J.G. Assessment of the ability of open-and closed-loop cueing to improve turning and freezing in people with Parkinson’s disease. Sci. Rep. 2018, 8, 12773. [Google Scholar] [CrossRef]
- Harrington, W.; Greenberg, A.; King, E.; McNames, J.; Holmstrom, L.; Horak, F.B.; Mancini, M. Alleviating freezing of gait using phase-dependent tactile biofeedback. In Proceedings of the 2016 IEEE 38th Annual International Conference of the Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 16–20 August 2016; pp. 5841–5844. [Google Scholar]
- Mancini, M.; Smulders, K.; Cohen, R.G.; Horak, F.B.; Giladi, N.; Nutt, J.G. The clinical significance of freezing while turning in Parkinson’s disease. Neuroscience 2017, 343, 222–228. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kwon, Y.; Park, S.H.; Kim, J.W.; Ho, Y.; Jeon, H.M.; Bang, M.J.; Jung, G.I.; Lee, S.M.; Eom, G.M.; Koh, S.B.; et al. A practical method for the detection of freezing of gait in patients with Parkinson’s disease. Clin. Interv. Aging 2014, 9, 1709. [Google Scholar] [PubMed]
- Young, W.R.; Rodger, M.W.; Craig, C.M. Auditory observation of stepping actions can cue both spatial and temporal components of gait in Parkinson’s disease patients. Neuropsychologia 2014, 57, 140–153. [Google Scholar] [CrossRef] [PubMed]
- Harte, R.; Quinlan, L.R.; Glynn, L.; Rodríguez-Molinero, A.; Baker, P.M.; Scharf, T.; ÓLaighin, G. Human-centered design study: Enhancing the usability of a mobile phone app in an integrated falls risk detection system for use by older adult users. JMIR mHealth uHealth 2017, 5. [Google Scholar] [CrossRef] [PubMed]
- Harte, R.; Glynn, L.; Broderick, B.; Rodriguez-Molinero, A.; Baker, P.; McGuiness, B.; O’Sullivan, L.; Diaz, M.; Quinlan, L.; ÓLaighin, G. Human centred design considerations for connected health devices for the older adult. J. Personal. Med. 2014, 4, 245–281. [Google Scholar] [CrossRef] [PubMed]
- Harte, R.; Glynn, L.; Rodríguez-Molinero, A.; Baker, P.M.; Scharf, T.; Quinlan, L.R.; ÓLaighin, G. A human-centered design methodology to enhance the usability, human factors, and user experience of connected health systems: A three-phase methodology. JMIR Hum. Factors 2017, 4. [Google Scholar] [CrossRef] [PubMed]
- Stara, V.; Harte, R.; Di Rosa, M.; Glynn, L.; Casey, M.; Hayes, P.; Rossi, L.; Mirelman, A.; Baker, P.M.; Quinlan, L.R.; et al. Does culture affect usability? A trans-European usability and user experience assessment of a falls-risk connected health system following a user-centred design methodology carried out in a single European country. Maturitas 2018, 114, 22–26. [Google Scholar] [CrossRef] [PubMed]












| FoG Subtype | Off-Medication State | On-Medication State |
|---|---|---|
| Dopaminergic-Responsive FoG | FoG Occurs | No FoG |
| Dopaminergic-Induced FoG | No FoG | FoG Occurs |
| Dopaminergic-Resistant FoG | FoG Occurs | FoG Occurs |
| Ref. | Cueing Technology | Cueing Mode | Cueing Trigger | Cueing Stimuli Type, Sound (Frequency, Duration) | Cueing Tempo Configuration | Effectiveness |
|---|---|---|---|---|---|---|
| [75] | Custom-built: Small Bluetooth enabled Linux based wearable computer and Bluetooth enabled movement sensor. Commercial: Wired headphones. | O. | FoG detection algorithm (73.1%, 81.6%, <2 s) 1. | Rhythmic, ticking (NR, NR). | Fixed (60 bpm). |  Frequency and duration of Off-FoG 4. Frequency and duration of Off-FoG 4.↓ Frequency and duration of Off-FoG 5. ↓ Frequency of On-FoG 4. ↓ Duration of On-FoG 3. ↑ Duration of On-FoG 3. |
| [44] | Custom-built: Metronome. Commercial: Headphones. | C. | NA. | Rhythmic, tone (4625 Hz, 50 ms). | Adjustable (NR). | ↓ Frequency of EoD-FoG. ↓ Duration of EoD-FoG. |
| [50] | Commercial: Metronome (SDM300 SAMICK). | C. | NA. | Rhythmic, tone (45–440 Hz, NR). | Adjustable (40–216 bpm). | ↑ Frequency of Off-FoG. |
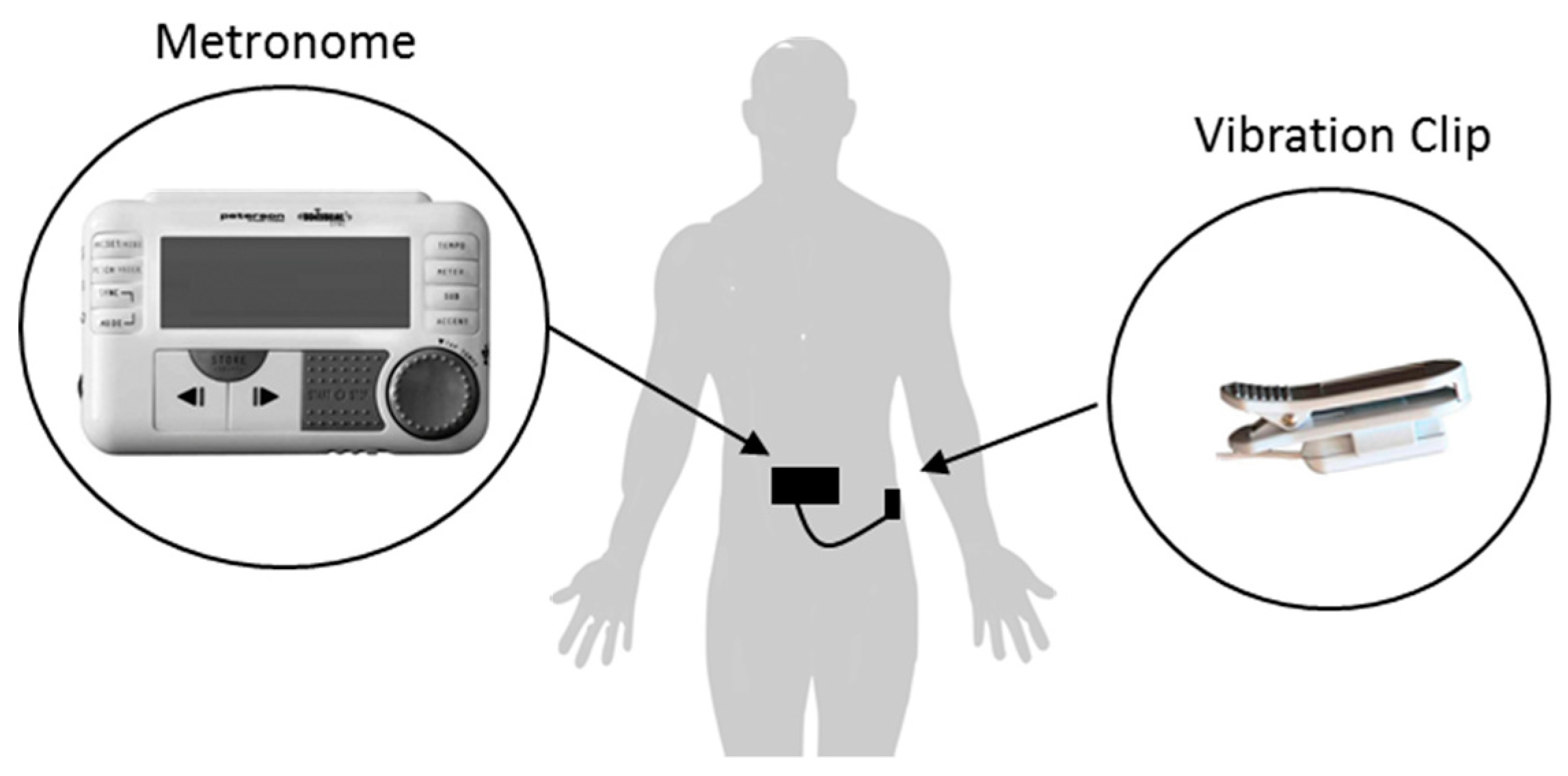
| [45] | Commercial: Metronome (Peterson BodyBeat). | C. | NA. | Rhythmic, rimshot, clave, wood Block or beep (NR, NR). | Adjustable (10–280 bpm). | ↓ Percentage of Off-FoG per walking task. |
| [82] | Custom-built: FoG detection device and Android application. Commercial: Smartphone and wireless ear-set. | O. | FoG detection algorithm (82.2%, 92.8%, 3.2 s) 1. | Rhythmic, ticking, musical beats, clapping or verbal (NR, NR). | Adjustable (NR). | NR. |
| [85] | Custom-built: Two movement sensors devices and Android application. Commercial: Smartphone and wired headphones. (GaitAssist) | O. | FoG detection algorithm (97.1%, 26.5%, 0.5 s) 2. | Rhythmic, ticking (NR, NR). | Adjustable (NR). | ↓ Frequency of FoG. ↓ Duration of FoG. |
| [48] | Custom-built: Android application. Commercial: Google Glass. | O. | NA. | Rhythmic, NR (NR, NR). | Adjustable (NR). |  Frequency and duration of EoD-FoG. Frequency and duration of EoD-FoG.↓ Frequency of EoD-FoG 6. |
 = no change. 1 sensitivity, specificity, lag time. 2 sensitivity, false negative, lag time. 3 For one participant. 4 For two participants. 5 For three participants. 6 Only during complex 360° turns.
= no change. 1 sensitivity, specificity, lag time. 2 sensitivity, false negative, lag time. 3 For one participant. 4 For two participants. 5 For three participants. 6 Only during complex 360° turns.| Ref | Cueing Technology | Cueing Mode | Cueing Trigger | Cueing Stimuli Type, Visual (Color) | Cueing Tempo Configuration | Effectiveness |
|---|---|---|---|---|---|---|
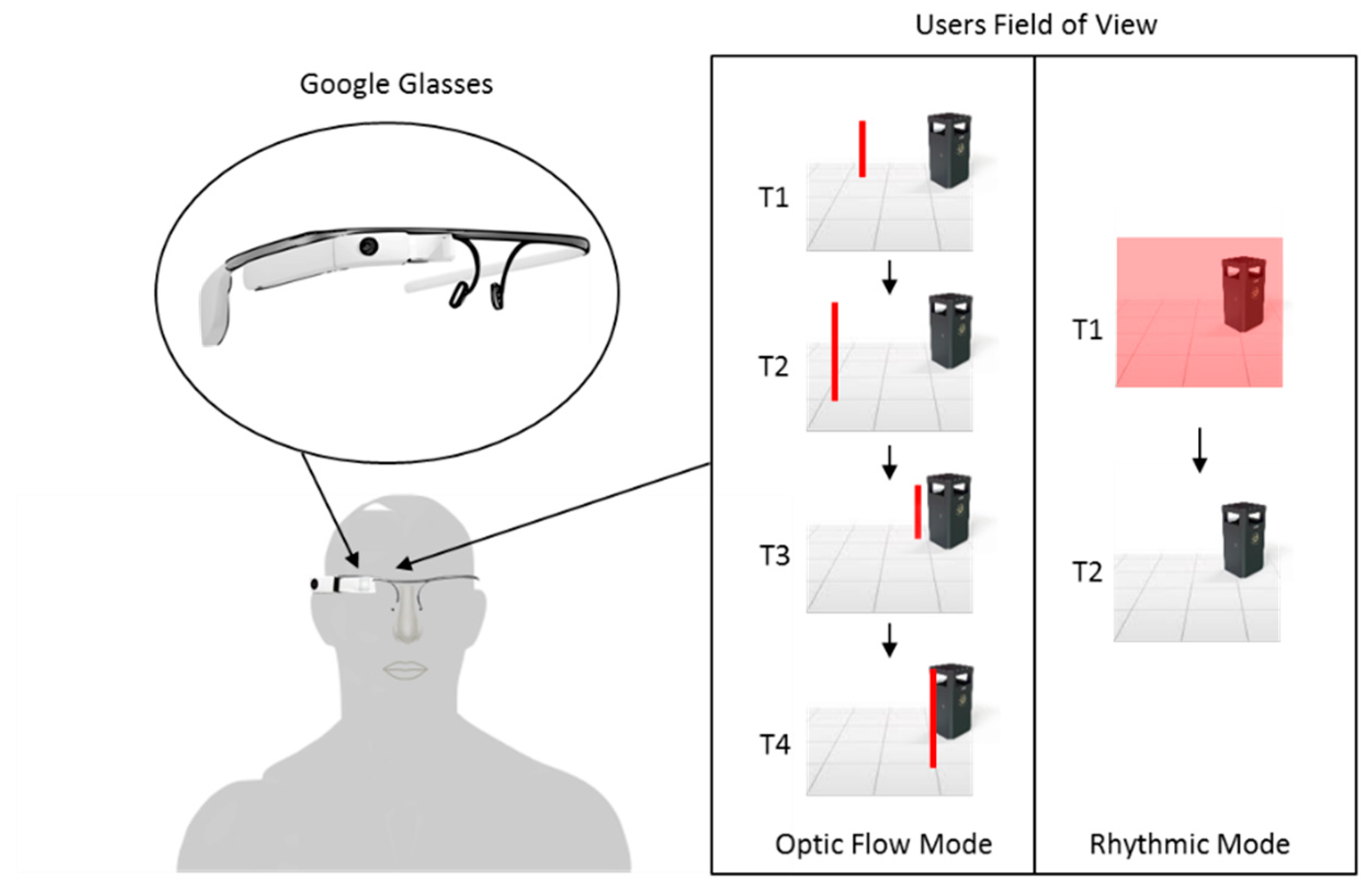
| [61] | Custom-built: Binocular Smartglasses. (Visual-auditory walker) | C. | NA. | Optical Flow, moving virtual checkerboard-tiled (NR). | Dynamic (Automatically adjusts to gait speed). | ↓ FOGQ score. |
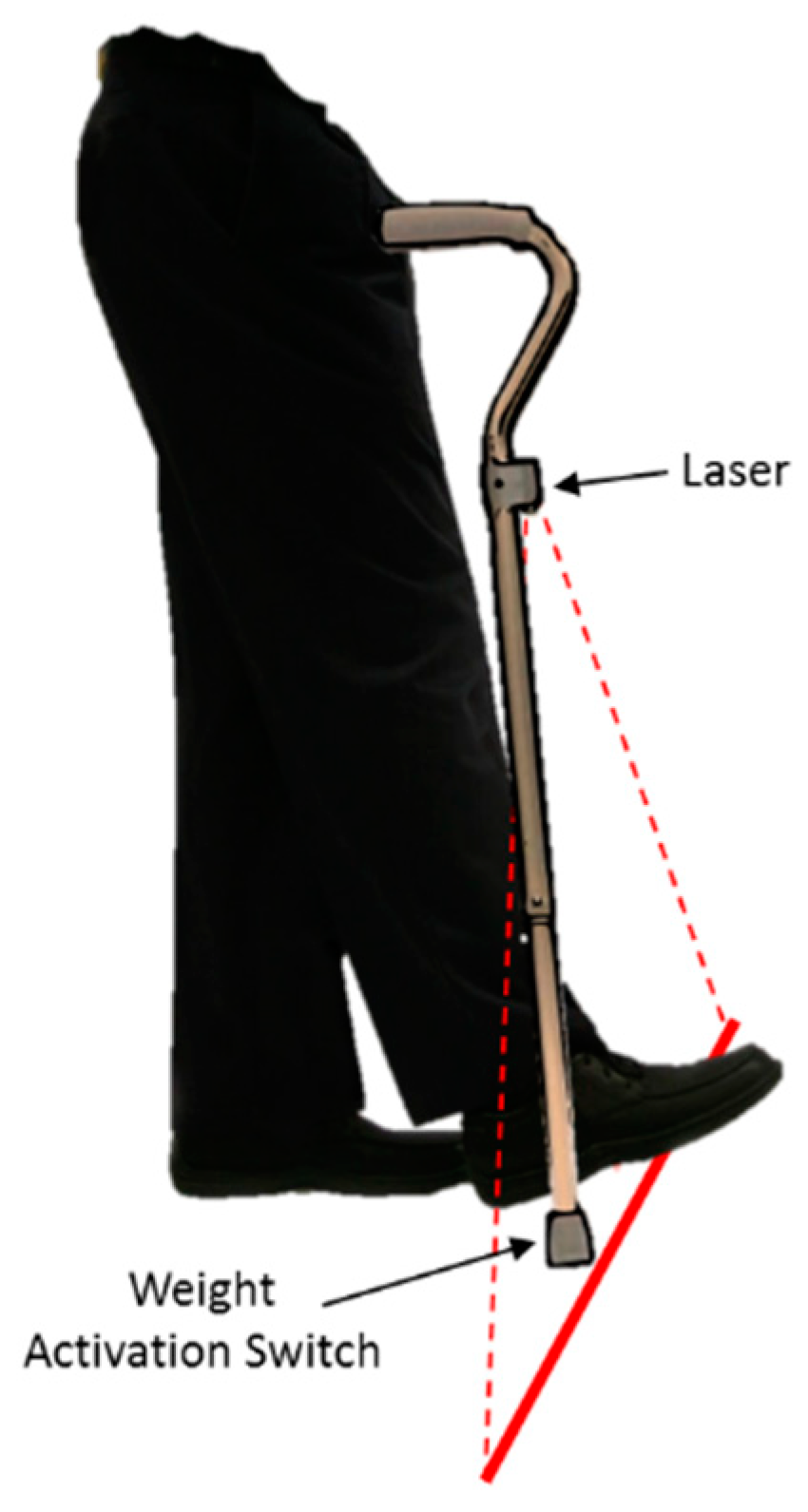
| [43] | Custom-built: Walking cane with attached laser. | C. | NA. | Static, horizontal laser line (green or red). | NA. | ↓ Frequency of On-FoG and Off-FoG (green laser). ↓ Frequency of On-FoG (red laser). ↑↓ Frequency of Off-FoG (red laser). 1 |
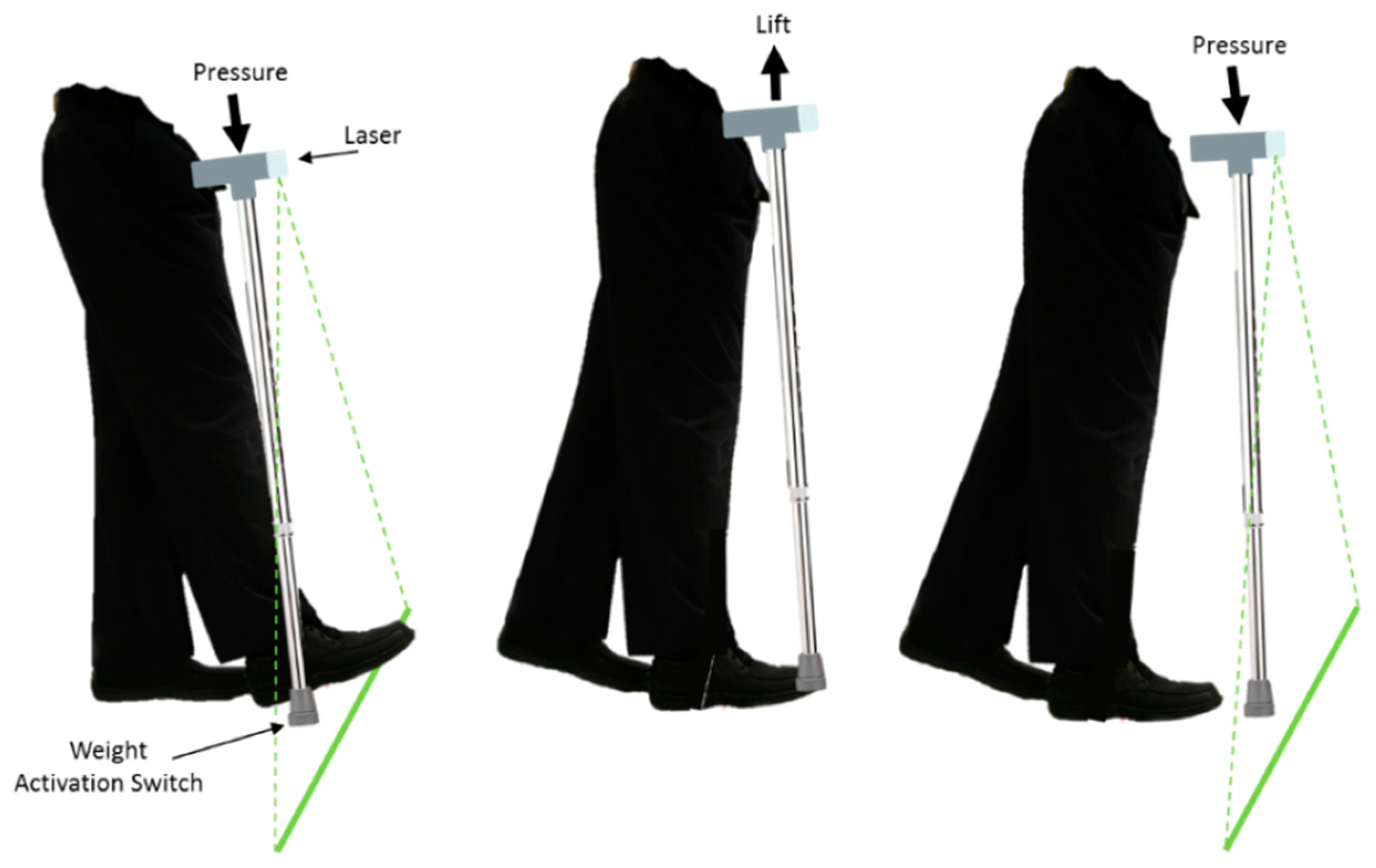
| [45,57] | Commercial: U-Step walking cane. | C. | Weight-activated switch. | Static, horizontal laser line (red). | NA. | ↓ Percentage of Off-FoG per walking task. |
| [49,57] | Commercial: U-Step walking stabilizer. | O. | Push button switch. | Static, horizontal laser line (red). | NA. | ↑↓ Frequency of On-FoG. 2 |
| [42] | Custom-built: Walking cane with attached laser. (LaserCane) | C. | Weight-activated switch. | Static, horizontal laser line (green). | NA. | ↓ Frequency of On-FoG and Off-FoG steps |
| [48] | Custom-built: Android app. Commercial: Google Glass monocular smartglasses. | C. | NA. | Optical Flow or Rhythmic, moving virtual vertically oriented lines or flashing virtual screen (red). | Adjustable. |  Frequency and duration of EoD-FoG. Frequency and duration of EoD-FoG. |
| [55] | Custom-built: Chest worn laser. | C. | NA. | Static or Rhythmic, horizontal laser line or flashing horizontal laser line (NR). | Adjustable. | ↓ Frequency of On-FoG. |
| [56] | Custom-built: Android app. Commercial: Epson’s Moverio BT-200 binocular smartglasses. (Smart Gait-Aid) | O. | FoG detection algorithm (97%, 88%, 1.1 s). | Optical Flow, moving virtual horizontal lines (blue). | Dynamic (Automatically adjusts to gait speed). | NR. |
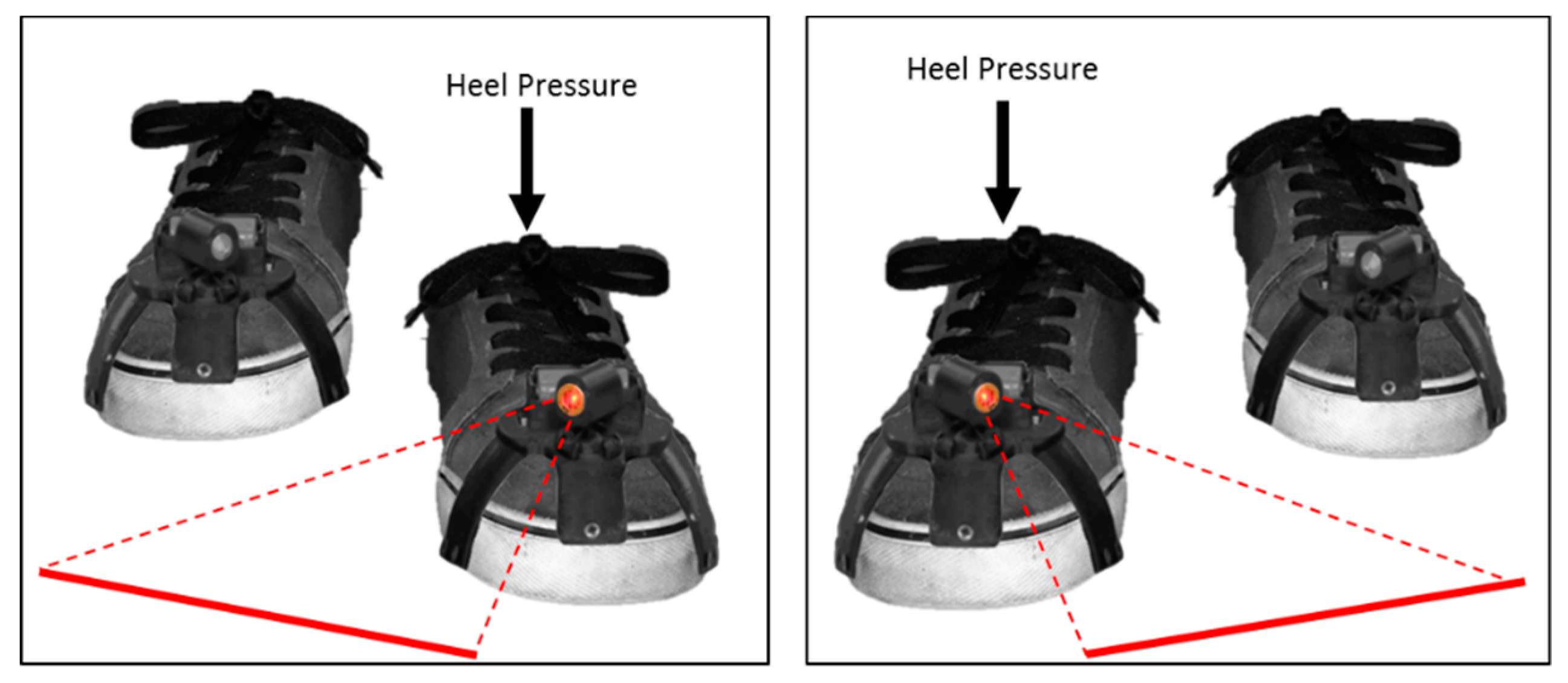
| [51] | Custom-built: Shoe attachment with laser (Laser Shoes). | C. | Heel strike switch. | Static, horizontal laser line (red). | NA. | ↓ Frequency of On-FoG and Off-FoG. ↓ Percentage of time in On-FoG and Off-FoG. |
 = no change. 1 Negative effect during 15.2 m task and positive effect during turning task. 2 Negative effect during walking task 1 and 2 and positive effect during walking task 3.
= no change. 1 Negative effect during 15.2 m task and positive effect during turning task. 2 Negative effect during walking task 1 and 2 and positive effect during walking task 3.| Ref. | Cueing Technology | Cueing Mode | Cueing Trigger | Cueing Stimuli Type, Somatosensory (Frequency, Duration) | Cueing Tempo Configuration | Effectiveness |
|---|---|---|---|---|---|---|
| [45] | Commercial: Metronome (Peterson BodyBeat). | C. | NA. | Rhythmic, vibrations (NR, NR). | Adjustable (10–280 bpm). | ↓ Percentage of walking task with Off-FoG. |
| [54] | Custom-built: Two channel electrical stimulator (cueStim). | C. | NA. | Rhythmic, Biphasic electrical pulses (NR, 500 ms). | Fixed (86 bpm) | ↓ Frequency of On-FoG. |
| [92] | Custom-built: Vibrating waistband. | C. | NA. | Rhythmic, vibrations (NR, 100–1000 ms). | Adjustable (80–250 Hz). | NA |
| [94] | Custom-built: Vibrating system (VibroGait). | C. | NA. | Rhythmic, vibrations (200–300 Hz, NR) | Dynamic (Automatically adjusts to gait speed). | ↓ Frequency of and time spent in Off-FoG. |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sweeney, D.; Quinlan, L.R.; Browne, P.; Richardson, M.; Meskell, P.; ÓLaighin, G. A Technological Review of Wearable Cueing Devices Addressing Freezing of Gait in Parkinson’s Disease. Sensors 2019, 19, 1277. https://doi.org/10.3390/s19061277
Sweeney D, Quinlan LR, Browne P, Richardson M, Meskell P, ÓLaighin G. A Technological Review of Wearable Cueing Devices Addressing Freezing of Gait in Parkinson’s Disease. Sensors. 2019; 19(6):1277. https://doi.org/10.3390/s19061277
Chicago/Turabian StyleSweeney, Dean, Leo R. Quinlan, Patrick Browne, Margaret Richardson, Pauline Meskell, and Gearóid ÓLaighin. 2019. "A Technological Review of Wearable Cueing Devices Addressing Freezing of Gait in Parkinson’s Disease" Sensors 19, no. 6: 1277. https://doi.org/10.3390/s19061277
APA StyleSweeney, D., Quinlan, L. R., Browne, P., Richardson, M., Meskell, P., & ÓLaighin, G. (2019). A Technological Review of Wearable Cueing Devices Addressing Freezing of Gait in Parkinson’s Disease. Sensors, 19(6), 1277. https://doi.org/10.3390/s19061277






