Improvement in Muscular Strength in HIV-Infected Individuals Receiving Antiretroviral Therapy
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participant Recruitment
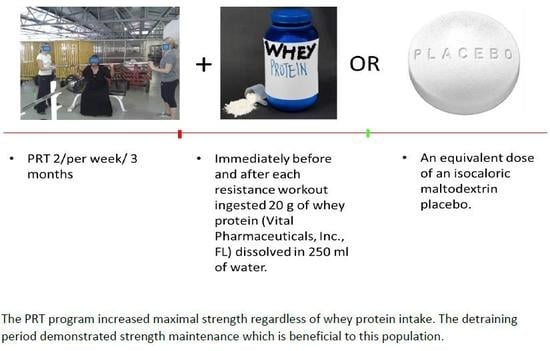
2.2. Resistance Training Program
2.3. Nutritional Supplementation
2.4. Data Analysis
3. Results
4. Discussion
4.1. Limitations
4.2. Strengths
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Botros, D.; Somarriba, G.; Neri, D.; Miller, T.L. Interventions to Address Chronic Disease and HIV: Strategies to Promote Exercise and Nutrition among HIV-Infected Individuals. Curr. HIV/AIDS Rep. 2012, 9, 351–363. [Google Scholar] [CrossRef] [PubMed]
- Gomes-Neto, M.; Conceição, C.S.; Carvalho, V.O.; Brites, C. A systematic review of the effects of different types of therapeutic exercise on physiologic and functional measurements in patients with HIV/AIDS. Clinics 2013, 68, 1157–1167. [Google Scholar] [CrossRef]
- Cioe, P.A.; Guthrie, K.M.; Freiberg, M.S.; Williams, D.M.; Kahler, C.W. Cardiovascular Risk Reduction in Persons Living With HIV: Treatment Development, Feasibility, and Preliminary Results. J. Assoc. Nurses AIDS Care 2018, 29, 163–177. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, S.W.; Torres, T.S.; Santini-Oliveira, M.; Marins, L.M.S.; Veloso, V.G.; Grinsztejn, B. Aging with HIV: A practical review. Braz. J. Infect. Dis. 2013, 17, 464–479. [Google Scholar] [CrossRef] [PubMed]
- Montoya, J.L.; Jankowski, C.M.; O’Brien, K.K.; Webel, A.R.; Oursler, K.K.; Henry, B.L.; Moore, D.J.; Erlandson, K.M. Evidence-informed practical recommendations for increasing physical activity among persons living with HIV. Aids 2019, 33, 931–939. [Google Scholar] [CrossRef] [PubMed]
- Capili, B.; Anastasi, J.K.; Ogedegbe, O. HIV and General Cardiovascular Risk. J. Assoc. Nurses AIDS Care 2011, 22, 362–375. [Google Scholar] [CrossRef] [PubMed]
- Sattler, F.R.; Schroeder, E.T.; Dubé, M.P.; Jaque, S.V.; Martínez, C.; Blanche, P.J.; Azen, S.; Krauss, R.M. Metabolic effects of nandrolone decanoate and resistance training in men with HIV. Am. J. Physiol. Metab. 2002, 283, E1214–E1222. [Google Scholar] [CrossRef] [PubMed]
- Chaparro, C.G.A.P.; Zech, P.; Schuch, F.; Wolfarth, B.; Rapp, M.; Heiβel, A. Effects of aerobic and resistance exercise alone or combined on strength and hormone outcomes for people living with HIV. A meta-analysis. PLoS ONE 2018, 13, e0203384. [Google Scholar]
- O’Brien, K.; Tynan, A.-M.; Nixon, S.; Glazier, R. Effects of progressive resistive exercise in adults living with HIV/AIDS: Systematic review and meta-analysis of randomized trials. AIDS Care 2008, 20, 631–653. [Google Scholar] [CrossRef]
- Medeiros, R.C.D.S.C.; Medeiros, J.A.D.; Silva, T.A.L.D.; Andrade, R.D.D.; Medeiros, D.C.D.; Araújo, J.D.S.; Oliveira, A.M.G.D.; Costa, M.A.D.A.; Cabral, B.G.D.A.T.; Dantas, P.M.S. Quality of life, socioeconomic and clinical factors, and physical exercise in persons living with HIV/AIDS. Revis. Saúde Pública 2017, 51, 66. [Google Scholar] [CrossRef]
- Roubenoff, R. Exercise and HIV Infection. Nutr. Clin. Care 2000, 3, 230–236. [Google Scholar] [CrossRef]
- Shah, K.N.; Majeed, Z.; Yoruk, Y.B.; Yang, H.; Hilton, T.N.; McMahon, J.M.; Hall, W.J.; Walck, D.; Luque, A.E.; Ryan, R.M. Enhancing physical function in HIV-infected older adults: A randomized controlled clinical trial. Health Psychol. 2016, 35, 563–573. [Google Scholar] [CrossRef] [PubMed]
- Dudgeon, W.; Phillips, K.; Carson, J.; Brewer, R.; Durstine, J.; Hand, G.; Carson, J. Counteracting muscle wasting in HIV-infected individuals. HIV Med. 2006, 7, 299–310. [Google Scholar] [CrossRef] [PubMed]
- Dolan, S.E.; Frontera, W.; Librizzi, J.; Ljungquist, K.; Juan, S.; Dorman, R.; Cole, M.E.; Kanter, J.R.; Grinspoon, S. Effects of a Supervised Home-Based Aerobic and Progressive Resistance Training Regimen in Women Infected With Human Immunodeficiency Virus. Arch. Intern. Med. 2006, 166, 1225–1231. [Google Scholar] [CrossRef] [PubMed]
- Hulmi, J.J.; Myllymäki, T.; Tenhumäki, M.; Mutanen, N.; Puurtinen, R.; Paulsen, G.; Mero, A.A. Effects of resistance exercise and protein ingestion on blood leukocytes and platelets in young and older men. Graefe’s Arch. Clin. Exp. Ophthalmol. 2010, 109, 343–353. [Google Scholar] [CrossRef]
- Sattler, F.R.; Rajicic, N.; Mulligan, K.; Yarasheski, K.E.; Koletar, S.L.; Zolopa, A.; Smith, B.A.; Zackin, R.; Bistrian, B. Evaluation of high-protein supplementation in weight-stable HIV-positive subjects with a history of weight loss: A randomized, double-blind, multicenter trial123. Am. J. Clin. Nutr. 2008, 88, 1313–1321. [Google Scholar]
- Hulmi, J.J.; Lockwood, C.M.; Stout, J.R. Effect of protein/essential amino acids and resistance training on skeletal muscle hypertrophy: A case for whey protein. Nutr. Metab. 2010, 7, 1–11. [Google Scholar] [CrossRef]
- Souza, P.M.L.D.; Jacob-Filho, W.; Santarém, J.M.; Silva, A.R.D.; Li, H.Y.; Burattini, M.N. Progressive Resistance Training on Elderly HIV+ Patients: Does it Work? Am. J. Infect. Dis. 2008, 4, 215–219. [Google Scholar] [CrossRef]
- Dobs, A. Role of testosterone in maintaining lean body mass and bone density in HIV-infected patients. Int. J. Impot. Res. 2003, 15 (Suppl. 4), S21–S25. [Google Scholar] [CrossRef]
- Srikanthan, P.; Karlamangla, A.S. Muscle Mass Index as a Predictor of Longevity in Older Adults. Am. J. Med. 2014, 127, 547–553. [Google Scholar] [CrossRef]
- Kaufmann, G.R.; Furrer, H.; Ledergerber, B.; Perrin, L.; Opravil, M.; Vernazza, P.; Cavassini, M.; Bernasconi, E.; Rickenbach, M.; Hirschel, B.; et al. Characteristics, Determinants, and Clinical Relevance of CD4 T cell Recovery to <500 Cells/ÂμL in HIV Type 1-Infected Individuals Receiving Potent Antiretroviral Therapy. Clin. Infect. Dis. 2005, 41, 361–372. [Google Scholar] [CrossRef] [PubMed]
- Patil, R.; Shimpi, A.; Rairikar, S.; Shyam, A.; Sancheti, P. Effects of fitness training on physical fitness parameters and quality of life in human immunodeficiency virus-positive Indian females. Indian J. Sex. Transm. Dis. AIDS 2017, 38, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Hulmi, J.J.; Tannerstedt, J.; Selanne, H.; Kainulainen, H.; Kovanen, V.; Mero, A.A. Resistance execise with whey protein ingestion affects mTOR signaling pathway and myostatin in men. J. Appl. Physiol. 2009, 106, 1720–1729. [Google Scholar] [CrossRef] [PubMed]
- Morton, R.W.; McGlory, C.; Phillips, S.M. Nutritional interventions to augment resistance training-induced skeletal muscle hypertrophy. Front. Physiol. 2015, 6, 245. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, C.J.; McGregor, R.A.; D’Souza, R.F.; Thorstensen, E.B.; Markworth, J.F.; Fanning, A.C.; Poppitt, S.D.; Cameron-Smith, D. Consumption of Milk Protein or Whey Protein Results in a Similar Increase in Muscle Protein Synthesis in Middle Aged Men. Nutrients 2015, 7, 8685–8699. [Google Scholar] [CrossRef] [PubMed]
- Bauer, J.; Biolo, G.; Cederholm, T.; Cesari, M.; Cruz-Jentoft, A.J.; Morley, J.E.; Phillips, S.; Sieber, C.; Stehle, P.; Teta, D.; et al. Evidence-Based Recommendations for Optimal Dietary Protein Intake in Older People: A Position Paper From the PROT-AGE Study Group. J. Am. Med Dir. Assoc. 2013, 14, 542–559. [Google Scholar] [CrossRef] [PubMed]
- Woldeyohannes, M.T.; Kaestel, P.; Olsen, M.F.; Girma, T.; Yilma, D.; Abdissa, A.; Ritz, C.; Michaelsen, K.F.; Hanlon, C.; Friis, H. The effect of nutritional supplementation on quality of life in people living with HIV: A randomized controlled trial. Trop. Med. Int. Health 2016, 21, 735–742. [Google Scholar] [CrossRef]
- Olsen, M.F.; Abdissa, A.; Kæstel, P.; Tesfaye, M.; Yilma, D.; Girma, T.; Wells, J.C.K.; Ritz, C.; Mølgaard, C.; Michaelsen, K.F.; et al. Effects of nutritional supplementation for HIV patients starting antiretroviral treatment: Randomised controlled trial in Ethiopia. BMJ 2014, 348, g3187. [Google Scholar] [CrossRef] [PubMed]
- Benton, M.J.; Swan, P.D.; Peterson, M.D. Evaluation of Multiple One Repetition Maximum Strength Trials in Untrained Women. J. Strength Cond. Res. 2009, 23, 1503–1507. [Google Scholar] [CrossRef] [PubMed]
- Barrett, B.; Locken, K.; Maberry, R.; Schwamman, J.; Brown, R.; Bobula, J.; Stauffacher, E.A. The Wisconsin upper respiratory symptom survey (WURSS). J. Fam. Pract. 2002, 51, 265. [Google Scholar] [PubMed]
- Leyes, P.; Martínez, E.; Forga, M.D.T. Use of diet, nutritional supplements and exercise in HIV-infected patients recieving combination antiretroviral therapies: A systematic review. Antivir. Ther. 2008, 13, 149–159. [Google Scholar] [PubMed]
- Driscoll, S.D.; Meininger, G.E.; Ljungquist, K.; Hadigan, C.; Torriani, M.; Klibanski, A.; Frontera, W.R.; Grinspoon, S. Differential Effects of Metformin and Exercise on Muscle Adiposity and Metabolic Indices in Human Immunodeficiency Virus-Infected Patients. J. Clin. Endocrinol. Metab. 2004, 89, 2171–2178. [Google Scholar] [CrossRef] [PubMed]
- Sakkas, G.K.; Mulligan, K.; DaSilva, M.; Doyle, J.W.; Khatami, H.; Schleich, T.; Kent-Braun, J.A.; Schambelan, M. Creatine Fails to Augment the Benefits from Resistance Training in Patients with HIV Infection: A Randomized, Double-Blind, Placebo-Controlled Study. PLoS ONE 2009, 4, e4605. [Google Scholar] [CrossRef] [PubMed]
- Pullen, S.D.; Chigbo, N.N.; Nwigwe, E.C.; Chukwuka, C.J.; Amah, C.C.; Idu, S.C. Physiotherapy intervention as a complementary treatment for people living with HIV/AIDS. HIV/AIDS 2014, 6, 99. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Agin, D.; Gallagher, D.; Wang, J.; Heymsfield, S.B.; Pierson, R.N.; Kotler, D.P. Effects of whey protein and resistance exercise on body cell mass, muscle strength, and quality of life in women with HIV. AIDS 2001, 15, 2431–2440. [Google Scholar] [CrossRef] [PubMed]
- Hand, G.A.; Phillips, K.D.; Dudgeon, W.D.; Lyerly, G.W.; Durstine, J.L.; Burgess, S.E. Moderate intensity exercise training reverses functional aerobic impairment in HIV-infected individuals. AIDS Care 2008, 20, 1066–1074. [Google Scholar] [CrossRef] [PubMed]
- Bopp, C.M.; Phillips, K.D.; Fulk, L.J.; Dudgeon, W.D.; Sowell, R.; Hand, G.A. Physical activity and immunity in HIV-infected individuals. AIDS Care 2004, 16, 387–393. [Google Scholar] [CrossRef] [PubMed]
- Engelson, E.S.; Agin, D.; Kenya, S.; Werber-Zion, G.; Luty, B.; Albu, J.B.; Kotler, D.P. Body composition and metabolic effects of a diet and exercise weight loss regimen on obese, HIV-infected women. Metabolism 2006, 55, 1327–1336. [Google Scholar] [CrossRef] [PubMed]
- Mangili, A.; Murman, D.H.; Zampini, A.M.; Wanke, C.A.; Mayer, K.H. Nutrition and HIV Infection: Review of Weight Loss and Wasting in the Era of Highly Active Antiretroviral Therapy from the Nutrition for Healthy Living Cohort. Clin. Infect. Dis. 2006, 42, 836–842. [Google Scholar] [CrossRef]
- Grinspoon, S.; Mulligan, K. Weight Loss and Wasting in Patients Infected with Human Immunodeficiency Virus. Clin. Infect. Dis. 2003, 36, S69–S78. [Google Scholar] [CrossRef] [PubMed]

| Variable | Placebo/PRT (n = 17) | Whey/PRT (n = 13) | Control (n = 10) |
|---|---|---|---|
| Females | 14 | 11 | 5 |
| Males | 3 | 2 | 5 |
| Age (years) | 41.0 ± 8.1 | 40.8 ± 7.9 | 40.9 ± 7.0 |
| Weight (kg) | 73.7 ± 17.4 | 87.6 ± 14.9 | 72.9 ± 12.8 |
| BMI (kg/m2) CD4+ (cells/mm3) | 28.7 ± 6.9 445.82 ± 200.19 | 34.2 ± 6.3 396.92 ± 173.99 | 27.8 ± 7.0 383.80 ± 151.27 |
| Strength Exercise (kg) | T1 | T2 | T3 | |||
|---|---|---|---|---|---|---|
| Whey/PRT (n = 13) | Placebo/PRT (n = 17) | Whey/PRT (n = 13) | Placebo/PRT (n = 17) | Whey/PRT (n = 12) | Placebo/PRT (n = 15) | |
| Bench Press | 34.80 ± 16.84 (27.15–42.45) | 30.32 ± 10.41 (23.63–37.00) | 42.50 ± 19.36 (34.85–50.15) | 39.41 ± 10.55 (32.72–46.10) | 46.04 ± 16.36 (38.08–54.00) | 39.33 ± 9.23 (32.21–46.45) |
| Squat | 43.88 ± 18.64 (30.04–57.73) | 40.03 ± 17.17 (27.93–52.13) | 71.46 ± 27.12 (57.62–85.30) | 77.82 ± 30.34 (65.72–89.93) | 72.08 ± 28.16 (57.68–86.49) | 78.00 ± 26.44 (65.12–90.88) |
| Deadlift | 50.50 ± 17.33 (38.71–62.29) | 45.88 ± 18.98 (35.57–56.19) | 68.46 ± 26.64 (56.67–80.25) | 71.72 ± 21.74 (61.41–82.03) | 68.33 ± 21.25 (56.06–80.61) | 66.90 ± 21.67 (55.92–77.88) |
| Bicep curl | 24.19 ± 7.65 (19.85–28.53) | 23.71 ± 6.75 (19.91–27.50) | 28.92 ± 9.01 (24.58–33.26) | 28.56 ± 8.17 (24.76–32.35) | 29.38 ± 9.18 (24.86–33.89) | 27.63 ± 6.60 (23.59–31.67) |
| Shoulder Press | 27.31 ± 8.85 (22.37–32.25) | 24.59 ± 783 (20.27–28.91) | 32.19 ± 10.34 (27.25–37.13) | 32.12 ± 9.84 (27.80–36.44) | 32.71 ± 9.01 (27.57–37.85) | 30.73 ± 7.64 (26.14–35.33) |
| Grip Strength (R) | 32.69 ± 12.45 (26.78–38.60) | 34.44 ± 11.33 (29.27–39.61) | 36.08 ± 9.47 (30.17–41.99) | 36.53 ± 12.21 (31.36–41.70) | 33.58 ± 8.50 (27.43–39.74) | 32.07 ± 8.96 (26.56–37.57) |
| Grip Strength (L) | 31.73 ± 12.58 (26.64–36.82) | 31.00 ± 8.76 (26.55–35.45) | 34.62 ± 9.01 (29.53–39.70) | 33.53 ± 9.15 (29.08–37.98) | 28.75 ± 6.86 (23.46–34.04) | 28.13 ± 8.11 (23.40–32.87) |
| Placebo/PRT | Whey/PRT | Control | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Strength Exercises (kg) | T1 | T2 | Cohen’s d | 95% CI | ES | T1 | T2 | Cohen’s d | 95% CI | ES | T1 | T2 | Cohen’s d | 95% CI | ES |
| Bench Press | 30.32 ± 10.41 | 39.41 ± 10.55 | 0.9 | −0.2, 1.6 | Medium | 34.80 ± 16.84 | 42.50 ± 19.36 | 0.4 | −0.4, 1.2 | Small | 42.85 ± 19.34 | 45.71 ± 18.86 | 0.1 | −0.7, 1.0 | Trivial |
| Squat | 40.03 ± 17.17 | 77.82 ± 30.34 | 1.5 | 0.8, 2.3 | Large | 43.88 ± 18.64 | 71.46 ± 27.12 | 1.2 | 0.4, 2 | Large | 65.00 ± 22.36 | 76.20 ± 23.04 | 0.5 | −0.4, 1.4 | Small |
| Deadlift | 45.88 ± 18.98 | 71.72 ± 21.74 | 1.3 | 0.5, 2 | Large | 50.50 ± 17.33 | 68.46 ± 26.64 | 0.8 | 0.0, 1.6 | Medium | 68.50 ± 24.04 | 77.50 ± 23.12 | 0.4 | −0.5, 1.3 | Small |
| Bicep Curl | 23.71 ± 6.75 | 28.56 ± 8.17 | 0.6 | −0.0, 1.3 | Medium | 24.19 ± 7.65 | 28.92 ± 9.01 | 0.6 | −0.2, 1.4 | Medium | 31.50 ± 9.85 | 31.20 ± 8.62 | −0.03 | −0.9, 0.8 | Trivial |
| Shoulder Press | 24.59 ± 7.83 | 32.12 ± 9.84 | 0.3 | −0.4, 1 | Small | 27.31 ± 8.95 | 32.19 ± 10.34 | 0.5 | −0.3, 1.3 | Small | 29.85 ± 9.37 | 31.86 ± 7.87 | 0.2 | −0.6, 1.1 | Small |
| Grip Strength (R) | 34.44 ± 11.33 | 36.53 ± 32.07 | 0.1 | −0.6, 0.8 | Trivial | 32.69 ± 12.45 | 36.08 ± 9.47 | 0.3 | −0.5, 1.1 | Small | 39.70 ± 16.91 | 37.00 ± 9.52 | −0.2 | −1.1, 0.7 | Small |
| Grip Strength (L) | 31.00 ± 8.76 | 33.53 ± 9.15 | 0.3 | −0.4, 1 | Small | 31.73 ± 12.58 | 34.62 ± 9.01 | 0.3 | −0.5, 1 | Small | 38.00 + 16.60 | 36.10 ± 9.40 | −0.1 | −1.0, 0.7 | Trivial |
| Placebo/PRT | Whey/PRT | Control | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Strength Exercises (kg) | T1 | T3 | Cohen’s d | 95% CI | ES | T1 | T3 | Cohen’s d | 95% CI | ES | T1 | T3 | Cohen’s d | 95% CI | ES |
| Bench Press | 30.32 ± 10.41 | 39.33 ± 9.23 | 0.9 | 0.1, 1.6 | Medium | 34.80 ± 16.84 | 46.04 ± 16.36 | 0.7 | −0.1, 1.5 | Medium | 42.85 ± 19.34 | 45.00 ± 17.68 | 0.1 | −0.8, 1.0 | Trivial |
| Squat | 40.03 ± 17.17 | 78.00 ± 26.44 | 1.7 | 0.9, 2.5 | Large | 43.88 ± 18.64 | 72.08 ± 28.16 | 1.2 | 0.3, 2.0 | Large | 65.00 ± 22.36 | 78.33 ± 24.87 | 0.6 | −0.4, 1.5 | Medium |
| Deadlift | 45.88 ± 18.98 | 66.90 ± 21.67 | 1.0 | 0.3, 1.8 | Medium | 50.50 ± 17.33 | 68.33 ± 21.25 | 0.9 | 0.1, 1.7 | Medium | 68.50 ± 24.04 | 83.33 ± 26.46 | 0.6 | −0.3, 1.5 | Medium |
| Bicep Curl | 23.71 ± 6.75 | 27.63 ± 6.60 | 0.6 | −0.1, 1.3 | Medium | 24.19 ± 7.65 | 29.38 ± 9.18 | 0.6 | −0.2, 1.4 | Medium | 31.50 ± 9.85 | 31.11 ± 9.61 | −0.0 | −0.9, 0.9 | Trivial |
| Shoulder Press | 24.59 ± 7.83 | 30.73 ± 7.64 | 0.8 | 0.1, 1.5 | Medium | 27.31 ± 8.95 | 32.71 ± 9.01 | 0.6 | −0.2, 1.4 | Medium | 29.85 ± 9.37 | 31.00 ± 6.46 | 0.1 | −0.8, 1.0 | Trivial |
| Grip Strength (R) | 34.44 ± 11.33 | 32.07 ± 8.96 | −0.2 | −0.9, 0.5 | Small | 32.69 ± 12.45 | 33.58 ± 8.50 | 0.1 | −0.7, 0.9 | Trivial | 39.70 ± 16.91 | 35.22 ± 10.24 | −0.3 | −1.2, 0.6 | Small |
| Grip Strength (L) | 31.00 ± 8.76 | 28.13 ± 8.11 | −0.3 | −1.0, 0.4 | Small | 31.73 ± 12.58 | 28.75 ± 6.86 | −0.3 | −1.1, 0.5 | Small | 38.00 ± 16.60 | 32.67 ± 10.68 | −0.4 | −1.3 | Small |
| Placebo/PRT | Whey/PRT | Control | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Strength Exercises (kg) | T2 | T3 | Cohen’s d | 95% CI | ES | T2 | T3 | Cohen’s d | 95% CI | ES | T2 | T3 | Cohen’s d | 95% CI | ES |
| Bench Press | 39.41 ± 10.55 | 39.33 ± 9.23 | −0.0 | −0.7, 0.7 | Trivial | 42.50 ± 19.36 | 46.04 ± 16.36 | 0.2 | −0.6, 1.0 | Small | 45.71 ± 18.86 | 45.00 ± 17.68 | −0.0 | −0.9, 0.9 | Trivial |
| Squat | 77.82 ± 30.34 | 78.00 ± 26.44 | 0.0 | −0.7, 0.7 | Trivial | 71.46 ± 27.12 | 72.08 ± 28.16 | 0.0 | −0.8, 0.8 | Trivial | 76.20 ± 23.04 | 78.33 ± 24.87 | 0.1 | −0.8, 1.0 | Trivial |
| Deadlift | 71.72 ± 21.74 | 66.90 ± 21.67 | −0.2 | −0.9, 0.5 | Small | 68.46 ± 26.64 | 68.33 ± 21.25 | −0.0 | −0.8, 0.8 | Trivial | 77.50 ± 23.12 | 83.33 ± 26.46 | 0.2 | −0.7, 1.1 | Small |
| Bicep Curl | 28.56 ± 8.17 | 27.63 ± 6.60 | −0.1 | −0.8, 0.6 | Trivial | 28.92 ± 9.01 | 29.38 ± 9.18 | 0.1 | −0.7, 0.8 | Trivial | 31.20 ± 8.62 | 31.11 ± 9.61 | −0.0 | −1.0, 0.9 | Trivial |
| Shoulder Press | 32.12 ± 9.84 | 30.73 ± 7.64 | −0.2 | −0.9, 0.5 | Small | 32.19 ± 10.34 | 32.71 ± 9.01 | 0.1 | −0.7, 0.8 | Trivial | 31.86 ± 7.87 | 31.00 ± 6.46 | −0.1 | −1.0, 0.8 | Trivial |
| Grip Strength (R) | 36.53 ± 12.21 | 32.07 ± 8.96 | −0.4 | −1.1, 0.3 | Small | 36.08 ± 9.47 | 33.58 ± 8.50 | −0.3 | −1.1, 0.5 | Small | 37.00 ± 9.52 | 35.22 ± 10.24 | −0.2 | −1.1, 0.7 | Small |
| Grip Strength (L) | 33.53 ± 9.15 | 28.13 ± 8.11 | −0.6 | −1.3, 0.1 | Medium | 34.62 ± 9.01 | 28.75 ± 6.86 | −0.7 | −1.5, 0.1 | Medium | 36.10 ± 9.40 | 32.67 ± 10.68 | −0.3 | −1.2, 0.6 | Small |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sookan, T.; Motala, A.; Ormsbee, M.; Antonio, J.; Magula, N.; Lalloo, U.; McKune, A. Improvement in Muscular Strength in HIV-Infected Individuals Receiving Antiretroviral Therapy. J. Funct. Morphol. Kinesiol. 2019, 4, 66. https://doi.org/10.3390/jfmk4030066
Sookan T, Motala A, Ormsbee M, Antonio J, Magula N, Lalloo U, McKune A. Improvement in Muscular Strength in HIV-Infected Individuals Receiving Antiretroviral Therapy. Journal of Functional Morphology and Kinesiology. 2019; 4(3):66. https://doi.org/10.3390/jfmk4030066
Chicago/Turabian StyleSookan, Takshita, Ayesha Motala, Michael Ormsbee, Jose Antonio, Nombulelo Magula, Umesh Lalloo, and Andrew McKune. 2019. "Improvement in Muscular Strength in HIV-Infected Individuals Receiving Antiretroviral Therapy" Journal of Functional Morphology and Kinesiology 4, no. 3: 66. https://doi.org/10.3390/jfmk4030066
APA StyleSookan, T., Motala, A., Ormsbee, M., Antonio, J., Magula, N., Lalloo, U., & McKune, A. (2019). Improvement in Muscular Strength in HIV-Infected Individuals Receiving Antiretroviral Therapy. Journal of Functional Morphology and Kinesiology, 4(3), 66. https://doi.org/10.3390/jfmk4030066