Applying the WHO ICF Framework to the Outcome Measures Used in the Evaluation of Long-Term Clinical Outcomes in Coronavirus Outbreaks
Abstract
:1. Introduction
2. Methods
2.1. Stage 1. Identification of Long-Term Follow-Up Studies in Survivors of Previous Coronavirus Outbreaks
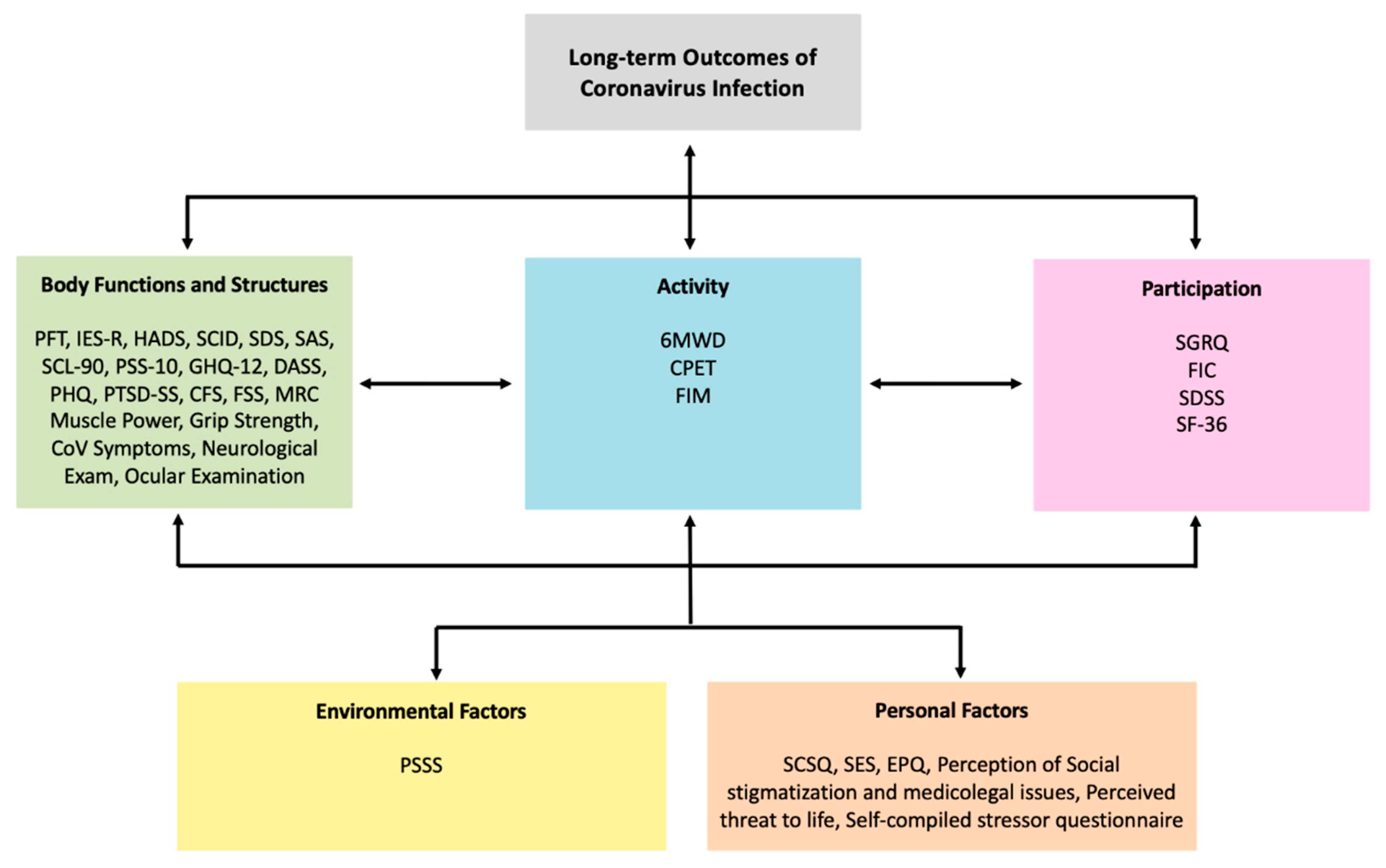
2.2. Stage 2. Classification of Outcome Measures According to the Five Main ICF Components
- Body structure and body function: refers to anatomical structure or physiological function such as those required for cognition, cardiovascular function, motor functions, pain or emotion.
- Activities: refers to the execution of tasks at an individual level.
- Participation: refers to the individual’s involvement in everyday life situations.
- Environmental factors: refer to physical, social and attitudinal factors in the person’s life and society which hinder or facilitate the functioning of the individual.
- Personal factors: refers to characteristics that are unique to each individual such as age, gender, ethnicity, personality, resilience or experiences.
3. Results
3.1. Stage 1. Study Selection
3.2. Stage 2. ICF Outcome Measures
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization. Coronavirus Disease (COVID-19) Pandemic. 2020. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 31 May 2020).
- Murray, A.; Gerada, C.; Morris, J. We Need a Nightingale Model for Rehab after COVID-19. Health Serv. J. 2020. Available online: https://www.hsj.co.uk/commissioning/we-need-a-nightingale-model-for-rehab-after-covid-19-/7027335.article (accessed on 13 May 2020).
- Carda, S.; Invernizzi, M.; Bavikatte, G.; Bensmaïl, D.; Bianchi, F.; Deltombe, T.; Draulans, N.; Esquenazi, A.; Francisco, G.E.; Gross, R.; et al. The role of physical and rehabilitation medicine in the COVID-19 pandemic: The clinician’s view. Ann. Phys. Rehabil. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Cohen Silver, R.; Everall, I.; et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 2020. [Google Scholar] [CrossRef]
- Ahmed, H.; Patel, K.; Greenwood, D.; Halpin, S.; Lewthwaite, P.; Salawu, A.; Eyre, L.; Breen, A.; O’Connor, R.; Jones, A.; et al. Long-term clinical outcomes in survivors of severe acute respiratory syndrome and Middle East respiratory syndrome coronavirus outbreaks after hospitalisation or ICU admission: A systematic review and meta-analysis. J. Rehabil. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Chan, K.S.; Zheng, J.P.; Mok, Y.W.; Li, Y.M.; Liu, Y.N.; Chu, C.M.; Ip, M.S. SARS: Prognosis, outcome and sequelae. Respirology 2003, 8, S36–S40. [Google Scholar] [CrossRef] [PubMed]
- Carfì, A.; Bernabei, R.; Landi, F. Persistent Symptoms in Patients After Acute COVID-19. JAMA 2020. [Google Scholar] [CrossRef]
- Halpin, S.J.; McIvor, C.; Whyatt, G.; Adams, A.; Harvey, O.; McLean, L.; Walshaw, C.; Kemp, S.; Corrado, J.; Singh, R.; et al. Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: A cross-sectional evaluation. J. Med. Virol. 2020. [Google Scholar] [CrossRef]
- Hui, D.S.; Wong, K.T.; Ko, F.W.; Tam, L.S.; Chan, D.P.; Woo, J.; Sung, J.J.Y. The 1-year impact of severe acute respiratory syndrome on pulmonary function, exercise capacity, and quality of life in a cohort of survivors. Chest 2005, 128, 2247–2261. [Google Scholar] [CrossRef] [Green Version]
- Chen, J.H.; Ma, D.Q.; He, W.; Jin, E.H.; Zhang, J.; Zhong, Z.H. Follow-up study of chest CT manifestations of patients with severe acute respiratory syndrome. Chin. J. Radiol. 2006, 40, 1161–1165. [Google Scholar]
- Tansey, C.M.; Louie, M.; Loeb, M.; Gold, W.L.; Muller, M.P.; De Jager, J.A.; Cameron, J.I.; Tomlinson, G.; Mazzulli, T.; Walmsley, S.L.; et al. One-year outcomes and health care utilization in survivors of severe acute respiratory syndrome. Arch. Intern. Med. 2007, 167, 1312–1320. [Google Scholar] [CrossRef] [Green Version]
- Park, W.B.; Jun, K.I.; Kim, G.; Choi, J.-P.; Rhee, J.-Y.; Cheon, S.; Lee, C.H.; Park, J.-S.; Kim, Y.; Joh, J.-S.; et al. Correlation between Pneumonia Severity and Pulmonary Complications in Middle East Respiratory Syndrome. J. Korean Med. Sci. 2018, 33, e169. [Google Scholar] [CrossRef]
- Tsai, L.K.; Hsieh, S.T.; Chao, C.C.; Chen, Y.C.; Lin, Y.H.; Chang, S.C.; Chang, Y.C. Neuromuscular disorders in severe acute respiratory syndrome. Arch. Neurol. 2004, 61, 1669–1673. [Google Scholar] [CrossRef] [PubMed]
- Sivan, M.; Sell, B.; Sell, P. A comparison of functional assessment instruments and work status in chronic back pain. Eur. J. Phys. Rehabil. Med. 2009, 45, 31–36. [Google Scholar]
- Müller, U.; Roeder, C.; Dubs, L.; Duetz, M.S.; Greenough, C.G. Condition-specific outcome measures for low back pain. Eur. Spine J. 2004, 13, 314–324. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stucki, G.; Ewert, T.; Cieza, A. Value and application of the ICF in rehabilitation medicine. Disabil. Rehabil. 2003, 25, 628–634. [Google Scholar] [CrossRef]
- World Health Organization. World Health Organization International Classification of Functioning, Disability and Health; World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Peng, M.; Cai, B.; Liu, T.; Ma, Y.; Xu, W.; Cao, B.; Shi, J.; Han, J.; Zhang, W. Assessment of pulmonary function in SARS patients during the convalescent period. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2003, 25, 529–532. [Google Scholar] [PubMed]
- Sivan, M.; O’Connor, R.J.; Makower, S.; Levesley, M.; Bhakta, B. Systematic review of outcome measures used in the evaluation of robot-assisted upper limb exercise in stroke. J. Rehabil. Med. 2011, 43, 181–189. [Google Scholar] [CrossRef] [Green Version]
- Bilbao, A.; Kennedy, C.; Chatterji, S.; Üstün, B.; Vásquez Barquero, J.L.; Barth, J.T. The ICF: Applications of the WHO model of functioning, disability and health to brain injury rehabilitation. NeuroRehabilitation 2003, 18, 239–250. [Google Scholar] [CrossRef] [Green Version]
- Peeri, N.C.; Shrestha, N.; Rahman, M.S.; Zaki, R.; Tan, Z.; Bibi, S.; Baghbanzadeh, M.; Aghamohammadi, N.; Zhang, W.; Haque, U. The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: What lessons have we learned? Int. J. Epidemiol. 2020, 49, 717–726. [Google Scholar] [CrossRef] [Green Version]
- Cieza, A.; Geyh, S.; Chatterji, S.; Kostanjsek, N.; Üstün, B.; Stucki, G. ICF linking rules: An update based on lessons learned. J. Rehabil. Med. 2005, 37, 212–218. [Google Scholar] [CrossRef] [Green Version]
- Mak, I.W.C.; Chu, C.M.; Pan, P.C.; Yiu, M.G.C.; Chan, V.L. Long-term psychiatric morbidities among SARS survivors. Gen. Hosp. Psychiatry 2009, 31, 318–326. [Google Scholar] [CrossRef]
- Lam, M.; Wing, Y.; Yu, M.; Leung, C.; Ma, R.; Kong, A.; So, W.; Fong, S.; Lam, S. Mental morbidities and chronic fatigue in severe acute respiratory syndrome survivors: Long-term follow-up. Arch. Intern. Med. 2009, 169, 2142–2147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, K.K.; Chan, S.K.; Ma, T.M. Posttraumatic stress, anxiety, and depression in survivors of severe acute respiratory syndrome (SARS). J. Trauma. Stress 2005, 18, 39–42. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.M.; Wong, J.G.W.S.; McAlonan, G.M.; Cheung, V.; Cheung, C.; Sham, P.C.; Chu, C.-M.; Wong, P.-C.; Tsang, K.W.T.; Chua, S.E. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can. J. Psychiatry. 2007, 52, 233–240. [Google Scholar] [CrossRef] [Green Version]
- Lee, S.H.; Shin, H.S.; Park, H.Y.; Kim, J.L.; Lee, J.J.; Lee, H.; Won, S.D.; Han, W. Depression as a mediator of chronic fatigue and post-traumatic stress symptoms in middle east respiratory syndrome survivors. Psychiatry Investig. 2019, 16, 59–64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, K.; Xu, Y.; Liu, Z.; Yang, H.; Song, L.; Xue, Y.; Lu, L.; Peng, C.; ZQ, C.; Wu, H.; et al. Controlled study of posttraumatic stress disorder among patients with severe acute respiratory syndrome and first-line hospital staffs as well as public in prevalent areas. Chin. J. Clin. Rehabil. 2005, 9, 94–96. [Google Scholar]
- Hong, X.; Currier, G.W.; Zhao, X.; Jiang, Y.; Zhou, W.; Wei, J. Posttraumatic stress disorder in convalescent severe acute respiratory syndrome patients: A 4-year follow-up study. Gen. Hosp. Psychiatry 2009, 31, 546–554. [Google Scholar] [CrossRef]
- Liu, K.; Zhang, W.; Yang, Y.; Zhang, J.; Li, Y.; Chen, Y. Respiratory rehabilitation in elderly patients with COVID-19: A randomized controlled study. Complement. Ther. Clin. Pract. 2020, 39, 101166. [Google Scholar] [CrossRef]
- Lam, S.P.; Tsui, E.; Chan, K.S.; Lam, C.L.; So, H.P. The validity and reliability of the functional impairment checklist (FIC) in the evaluation of functional consequences of severe acute respiratory distress syndrome (SARS). Qual. Life Res. 2006, 15, 217–231. [Google Scholar] [CrossRef]
- Xie, L.; Liu, Y.; Fan, B.; Xiao, Y.; Tian, Q.; Chen, L.; Zhao, H.; Chen, W. Dynamic changes of serum SARS-Coronavirus IgG, pulmonary function and radiography in patients recovering from SARS after hospital discharge. Respir. Res. 2005, 6, 5. [Google Scholar] [CrossRef]
- He, Z.Y. A follow-up study of the lung function and the chest CT changes in medical staff with severe acute respiratory syndrome in Beijing. Chinese J. Tuberc. Respir. Dis. 2005, 28, 10–12. [Google Scholar]
- Ong, K.; Ng, A.; Lee, L.; Kaw, G.; Kwek, S.; Leow, M.; Earnest, A. Pulmonary function and exercise capacity in survivors of severe acute respiratory syndrome. Eur. Respir. J. 2004, 24, 436–442. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ng, C.K.; Chan, J.W.M.; Kwan, T.L.; To, T.S.; Chan, Y.H.; Ng, F.Y.Y.; Mok, T.Y.W. Six month radiological and physiological outcomes in severe acute respiratory syndrome (SARS) survivors. Thorax 2004, 59, 889–891. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zheng, Z.; Chen, R.; Wu, H.; Liu, X.; He, W.; Xu, Y.; Chen, S.; Li, Y.; Zheng, J.; Zhong, N. Changes in pulmonary function in severe acute respiratory syndrome patients during convalescent period. Chin. Crit. Care Med. 2005, 17, 329–331. [Google Scholar] [CrossRef]
- Hsu, H.; Tzao, C.; Wu, C.; Chang, W.; Tsai, C.; Tung, H.; Chen, C. Correlation of high-resolution CT, symptoms, and pulmonary function in patients during recovery from severe acute respiratory syndrome. Chest 2004, 126, 149–158. [Google Scholar] [CrossRef] [Green Version]
- Gao, H.; Hui, W.; Lan, X. A follow-up study of post-traumatic stress disorder of SARS patients after discharge. Chin. J. Rehabil. Med. 2006, 21, 3–5. [Google Scholar]
- Zheng-yu, J.; Hui, Y.; Wei-hong, Z.; Yun, W.; Ji-Xiang, L.; Wen-bin, M.; Min, P.; Yi, M.; Bai-qiang, C.; Zhong, W.; et al. Thoracic high resolution CT findings of 100 SARS patients in convalescent period. Acta Acad. Med. Sin. 2003, 25, 512–515. [Google Scholar]
- Han, Y.; Geng, H.; Feng, W.; Tang, X.; Ou, A.; Lao, Y.; Xu, Y.; Lin, H.; Liu, H.; Li, Y.; et al. A follow-up study of 69 discharged SARS patients. J. Tradit. Chinese Med. 2003, 23, 214–217. [Google Scholar]
- Liu, Y.; Ye, Y.; Zhang, P.; Chen, J.; Ye, H.; He, Y.; Li, N. Changes in pulmonary function in SARS patients during the three-year convalescent period. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue 2007, 19, 536–538. [Google Scholar]
- Ong, K.; Ng, A.; Lee, L.; Kaw, G.; Kwek, S.; Leow, M.; Earnest, A. 1-year pulmonary function and health status in survivors of severe acute respiratory syndrome. Chest 2005, 128, 1393–1400. [Google Scholar] [CrossRef] [Green Version]
- Zhang, P.; Li, J.; Liu, H.; Han, N.; Ju, J.; Kou, Y.; Chen, L.; Jiang, M.; Pan, F.; Zheng, Y.; et al. Long-term consequences in lung and bone associated with hospital-acquired severe acute respiratory syndrome: A 15-year follow-up from a prospective cohort study. Lancet 2020, 8, S11. [Google Scholar] [CrossRef] [Green Version]
- Wong, K.; Antonio, G.E.; Hui, D.S.C.; Ho, C.; Chan, P.; Ng, W.; Shing, K.; Wu, A.; Lee, N.; Yap, F.; et al. Severe Acute Respiratory Syndrome Thin-Section Computed Tomography Features, Temporal Changes, and Clinicoradiologic Correlation During the Convalescent Period. Lung 2004, 28, 790–795. [Google Scholar]
- Li, T.S.; Gomersall, C.D.; Joynt, G.M.; Chan, D.P.S.S.; Leung, P.; Hui, D.S.C.C. Long-term outcome of acute respiratory distress syndrome caused by severe acute respiratory syndrome (SARS): An observational study. Crit. Care Resusc. 2006, 8, 302–308. [Google Scholar]
- Chiang, C.H.; Shih, J.F.; Su, W.J.; Perng, R.P. Eight-month prospective study of 14 patients with hospital-acquired severe acute respiratory syndrome. Mayo Clin. Proc. 2004, 79, 1372–1379. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yin, C.; Wang, C.; Wen, Y.; Jiang, L.; Lu, Q.; Li, J.; Wang, J.; HE, Z. Prospective 2-year clinical study of patients with positive IgG-antibodies after recovering from severe acute respiratory syndrome. Chin. Crit. Care Med. 2005, 17, 740–742. [Google Scholar]
- Wu, X.; Dong, D.; Ma, D. Thin-section computed tomography manifestations during convalescence and long- term follow-up of patients with severe acute respiratory syndrome (SARS). Med. Sci. Monit. 2016, 22, 2793–2799. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Avendano, M.; Derkach, P.; Swan, S. Clinical course and management of SARS in health care workers in Toronto: A case series. CMAJ 2003, 168, 1649–1660. [Google Scholar] [PubMed]
- Isakbaeva, E.; Khetsuriani, N.; Beard, R.; Peck, S.; Erdman, D.; Monroe, S.; Tong, S.; Ksiazek, T.; Lowther, S.; Pandya-Smith, I.; et al. SARS-associated Coronavirus Traansmission, United States. Emerg. Infect. Dis. 2004, 10, 225–231. [Google Scholar] [CrossRef]
- Klopfenstein, T.; Kadiane-Oussou, N.; Toko, L.; Royer, P.; Lepiller, Q.; Gendrin, V.; Zayet, S. Features of anosmia in COVID-19. Médecine Mal. Infect. 2020, 50, 436–439. [Google Scholar] [CrossRef]
- Hopkins, C.; Surda, P.; Whitehead, E.; Kumar, B.N. Early recovery following new onset anosmia during the COVID-19 outbreak—An observational cohort study. J. Otolaryngol.-Head Neck Surgery 2020, 49, 1–6. [Google Scholar] [CrossRef]
- Yuen, K.S.C.; Chan, W.M.; Fan, D.S.P.; Chong, K.K.L.; Sung, J.J.Y.; Lam, D.S.C. Ocular screening in severe acute respiratory syndrome. Am. J. Ophthalmol. 2004, 137, 773–774. [Google Scholar] [CrossRef]
- Functioning and Disability Reference Group The ICF: An Overview. World Health Organ. 2010. Available online: https://www.cdc.gov/nchs/data/icd/icfoverview_finalforwho10sept.pdf (accessed on 3 September 2020).
- Xie, L.; Liu, Y.; Xiao, Y.; Tian, Q.; Fan, B.; Zhao, H.; Chen, W. Follow-up study on pulmonary function and lung radiographic changes in rehabilitating severe acute respiratory syndrome patients after discharge. Chest 2005, 127, 2119–2124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hui, D.; Wong, K.; Antonio, G.; Tong, M.; Chan, D.; Sung, J. Long-term sequelae of SARS: Physical, neuropsychiatric, and quality-of-life. Hong Kong Med. J. 2009, 15, 21–23. [Google Scholar] [PubMed]
- Xu, X.; Zhang, L.; Chen, L.; Wei, F. Does COVID-2019 have an Impact on the Purchase Intention of Commercial Long-Term Care Insurance among the Elderly in China? Healthcare 2020, 8, 126. [Google Scholar] [CrossRef] [PubMed]
- Ehrich, J.; Mornane, A.; Powern, T. Psychometric Validation of the 10-item Connor-Davidson Resilience Scale. J. Appl. Meas. 2017, 18, 122–136. [Google Scholar]
- Kang, Y.K.; Guo, W.J.; Xu, H.; Chen, Y.H.; Li, X.J.; Tan, Z.P.; Li, N.; Gesang, Z.R.; Wang, Y.M.; Liu, C.B.; et al. The 6-item Kessler psychological distress scale to survey serious mental illness among Chinese undergraduates: Psychometric properties and prevalence estimate. Compr. Psychiatry 2015, 63, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Heinemann, A.W.; Miskovic, A.; Semik, P.; Wong, A.; Dashner, J.; Baum, C.; Magasi, S.; Hammel, J.; Tulsky, D.S.; Garcia, S.F.; et al. Measuring Environmental Factors: Unique and Overlapping International Classification of Functioning, Disability and Health Coverage of 5 Instruments Archives of Physical Medicine and Rehabilitation. Arch. Phys. Med. Rehabil. 2016, 97, 2113–2135. [Google Scholar] [CrossRef]

| Abbreviation | Outcome Measure |
|---|---|
| PFT | Pulmonary Function Test |
| IES-R | Impact of Event Scale–Revised |
| HADS | Hospital Anxiety and Depression Scale |
| SCID | Structures Clinical Interview for DSM Disorders |
| SDS | Self-rating Depression Scale |
| SAS | Self-rating Anxiety Scale |
| SCL-90 | Symptom Checklist 90 |
| PSS-10 | Perceived Stress Scale |
| GHQ-12 | General Health Questionnaire 12 |
| DASS | Depression Anxiety Stress Scale |
| PHQ | Patient Health Questionnaire 9 |
| PTSD-SS | PTSD Self-rating Scale |
| CFS | Chalder Fatigue Scale |
| FSS | Fatigue Severity Scale |
| MRC Muscle Power | Medical Research Council Muscle Power |
| NMS Exam | Neuromuscular Examination |
| 6MWD | 6-Minute Walking Distance |
| CPET | Cardiopulmonary Exercise Testing |
| FIM | Functional Independence Measure |
| SGRQ | St George’s Respiratory Questionnaire |
| FIC | Functional Impairment Checklist |
| SDSS | Social Disability Screening Schedule |
| SF-36 | Short-Form 36 |
| PSSS | Perceived Social Support Scale |
| SCSQ | Simple Coping Style Questionnaire |
| SES | Self-Esteem Scale |
| EPQ | Eysenck Personality Questionnaire |
| Studies | Outcome Measures Used in Follow-Up Studies of Coronavirus Survivors | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PFT | IES-R | HADS | SCID | SDS | SAS | SCL-90 | PSS-10 | GHQ-12 | DASS | PHQ-9 | PTSD-SS | CFS | FSS | MRC Power | Grip Strength | Symptoms | NMS Exam | Ocular Exam | 6MWD | CPET | FIM | SF-36 | SGRQ | FIC | SDSS | PSSS | SCSQ | SES | EPQ | Others | |
| Mak et al. (2009) [23] | + | + | + | + | |||||||||||||||||||||||||||
| Lam et al. (2009) [24] | + | + | + | + | Perception of social stigmatization and medicolegal issues | ||||||||||||||||||||||||||
| Wu et al. (2005) [25] | + | + | 5-point scale measuring perceived threat to life | ||||||||||||||||||||||||||||
| Lee et al. (2007) [26] | + | + | + | + | |||||||||||||||||||||||||||
| Lee et al. (2019) [27] | + | + | + | ||||||||||||||||||||||||||||
| Zhang et al. (2005) [28] | + | + | + | + | + | Self-compiled stressor questionnaire | |||||||||||||||||||||||||
| Hong et al. (2009) [29] | + | + | + | + | + | + | |||||||||||||||||||||||||
| Liu et al. (2020) [30] | + | + | + | + | + | + | |||||||||||||||||||||||||
| Lam et al. (2006) [31] | + | + | + | + | + | ||||||||||||||||||||||||||
| Peng et al. (2003) [18] | + | ||||||||||||||||||||||||||||||
| Xie et al. (2005) [32] | + | ||||||||||||||||||||||||||||||
| HE et al. (2005) [33] | + | ||||||||||||||||||||||||||||||
| Ong et al. (2004) [34] | + | + | |||||||||||||||||||||||||||||
| Ng et al. (2005) [35] | + | ||||||||||||||||||||||||||||||
| Zheng et al. (2005) [36] | + | ||||||||||||||||||||||||||||||
| Hsu et al. (2004) [37] | + | + | |||||||||||||||||||||||||||||
| Gao et al. (2006) [38] | + | ||||||||||||||||||||||||||||||
| Zheng-Yu et al. (2003) [39] | + | ||||||||||||||||||||||||||||||
| Yun et al. (2003) [40] | + | ||||||||||||||||||||||||||||||
| Liu et al. (2007) [41] | + | ||||||||||||||||||||||||||||||
| Ong et al. (2005) [42] | + | + | |||||||||||||||||||||||||||||
| Zhang et al. (2020) [43] | + | ||||||||||||||||||||||||||||||
| Tsai et al. (2004) [13] | + | + | |||||||||||||||||||||||||||||
| Chen et al. (2006) [10] | + | ||||||||||||||||||||||||||||||
| Hui et al. (2005) [9] | + | + | + | ||||||||||||||||||||||||||||
| Wong et al. (2004) [44] | + | ||||||||||||||||||||||||||||||
| Li et al. (2006) [45] | + | + | + | ||||||||||||||||||||||||||||
| Park et al. (2018) [12] | + | + | |||||||||||||||||||||||||||||
| Chiang et al. (2004) [46] | + | ||||||||||||||||||||||||||||||
| Yin et al. (2005) [47] | + | ||||||||||||||||||||||||||||||
| Wu et al. (2016) [48] | + | ||||||||||||||||||||||||||||||
| Tansey et al. (2007) [11] | + | + | + | + | |||||||||||||||||||||||||||
| Avendano et al. (2003) [49] | + | ||||||||||||||||||||||||||||||
| Isakbaeva et al. (2004) [50] | + | ||||||||||||||||||||||||||||||
| Klopfenstein et al. (2020) [51] | + | ||||||||||||||||||||||||||||||
| Hopkins et al. (2020) [52] | + | ||||||||||||||||||||||||||||||
| Yuen et al. (2004) [53] | + | ||||||||||||||||||||||||||||||
| ICF Code | Assessment | Body Functions and Structure | Activity | Participation | Environment | Personal Factors * | |||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PFT | IES-R | HADS | SCID | SDS | SAS | SCL-90 | PSS-10 | GHQ-12 | DASS | PHQ-9 | PTSD-SS | CFS | FSS | MRC Power | Grip Strength | Symptoms | Neuro Exam | Ocular Exam | 6MWD | CPET | FIM | SGRQ | FIC | SDSS | SF-36 | PSSS | SCSQ, SES, EPQ, Social Support, Threat to Life | ||||||
| b1263 | Psychic stability | + | |||||||||||||||||||||||||||||||
| b1266 | Confidence | + | |||||||||||||||||||||||||||||||
| b130 | Energy and drive functions | + | + | + | + | ||||||||||||||||||||||||||||
| b1302 | Appetite | + | |||||||||||||||||||||||||||||||
| b134 | Sleep function | + | + | + | + | ||||||||||||||||||||||||||||
| b144 | Memory function | ||||||||||||||||||||||||||||||||
| b152 | Stress | + | + | + | |||||||||||||||||||||||||||||
| b152 | Anxiety | + | + | + | + | + | + | ||||||||||||||||||||||||||
| b152 | Depression | + | + | + | + | + | + | + | + | ||||||||||||||||||||||||
| b152 | Panic | + | |||||||||||||||||||||||||||||||
| b152 | Fear | + | + | ||||||||||||||||||||||||||||||
| b152 | Concentrate | + | + | + | + | ||||||||||||||||||||||||||||
| b1522 | Anger | + | |||||||||||||||||||||||||||||||
| b1603 | Control of Thoughts | + | |||||||||||||||||||||||||||||||
| b210 | Seeing function | + | |||||||||||||||||||||||||||||||
| b255 | Smell function | + | |||||||||||||||||||||||||||||||
| b265 | Touch sensation | + | |||||||||||||||||||||||||||||||
| b280 | Sensation of Pain | + | |||||||||||||||||||||||||||||||
| b440 | Respiratory functions | + | |||||||||||||||||||||||||||||||
| b455 | Exercise tolerance functions | + | + | + | + | ||||||||||||||||||||||||||||
| b4552 | Fatiguability | + | + | + | |||||||||||||||||||||||||||||
| b460 | Sensation of respiratory system | + | + | ||||||||||||||||||||||||||||||
| b730 | Muscle power functions | + | + | + | |||||||||||||||||||||||||||||
| s220 | Structure of eyeball | + | |||||||||||||||||||||||||||||||
| d175 | Solving Problems | + | + | + | |||||||||||||||||||||||||||||
| d177 | Making decisions | + | + | ||||||||||||||||||||||||||||||
| d310 | Communication with – receiving – spoken language | + | |||||||||||||||||||||||||||||||
| d330 | Speaking | ||||||||||||||||||||||||||||||||
| d450 | Walking | + | + | + | + | ||||||||||||||||||||||||||||
| d460 | Moving around in different locations | + | + | ||||||||||||||||||||||||||||||
| d510 | Washing oneself | + | + | + | + | + | |||||||||||||||||||||||||||
| d520 | Caring for body parts | + | + | + | |||||||||||||||||||||||||||||
| d530 | Toileting | + | + | ||||||||||||||||||||||||||||||
| d540 | Dressing | + | + | + | |||||||||||||||||||||||||||||
| d640 | Doing housework | + | + | + | + | ||||||||||||||||||||||||||||
| d710 | Basic interpersonal interaction | + | + | + | |||||||||||||||||||||||||||||
| d640 | Formal Relationship | + | |||||||||||||||||||||||||||||||
| d760 | Family Relationship | + | + | ||||||||||||||||||||||||||||||
| d770 | Intimate Relationship | + | + | ||||||||||||||||||||||||||||||
| d845 | Work and employment | + | + | ||||||||||||||||||||||||||||||
| d920 | Recreation and Leisure | + | + | + | + | ||||||||||||||||||||||||||||
| e310 | Immediate family | + | |||||||||||||||||||||||||||||||
| e320 | Friends | + | |||||||||||||||||||||||||||||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Patel, K.; Straudi, S.; Yee Sien, N.; Fayed, N.; Melvin, J.L.; Sivan, M. Applying the WHO ICF Framework to the Outcome Measures Used in the Evaluation of Long-Term Clinical Outcomes in Coronavirus Outbreaks. Int. J. Environ. Res. Public Health 2020, 17, 6476. https://doi.org/10.3390/ijerph17186476
Patel K, Straudi S, Yee Sien N, Fayed N, Melvin JL, Sivan M. Applying the WHO ICF Framework to the Outcome Measures Used in the Evaluation of Long-Term Clinical Outcomes in Coronavirus Outbreaks. International Journal of Environmental Research and Public Health. 2020; 17(18):6476. https://doi.org/10.3390/ijerph17186476
Chicago/Turabian StylePatel, Kajal, Sofia Straudi, Ng Yee Sien, Nora Fayed, John L. Melvin, and Manoj Sivan. 2020. "Applying the WHO ICF Framework to the Outcome Measures Used in the Evaluation of Long-Term Clinical Outcomes in Coronavirus Outbreaks" International Journal of Environmental Research and Public Health 17, no. 18: 6476. https://doi.org/10.3390/ijerph17186476
APA StylePatel, K., Straudi, S., Yee Sien, N., Fayed, N., Melvin, J. L., & Sivan, M. (2020). Applying the WHO ICF Framework to the Outcome Measures Used in the Evaluation of Long-Term Clinical Outcomes in Coronavirus Outbreaks. International Journal of Environmental Research and Public Health, 17(18), 6476. https://doi.org/10.3390/ijerph17186476







