The Mechanical Behavior of a Screwless Morse Taper Implant–Abutment Connection: An In Vitro Study
Abstract
:1. Introduction
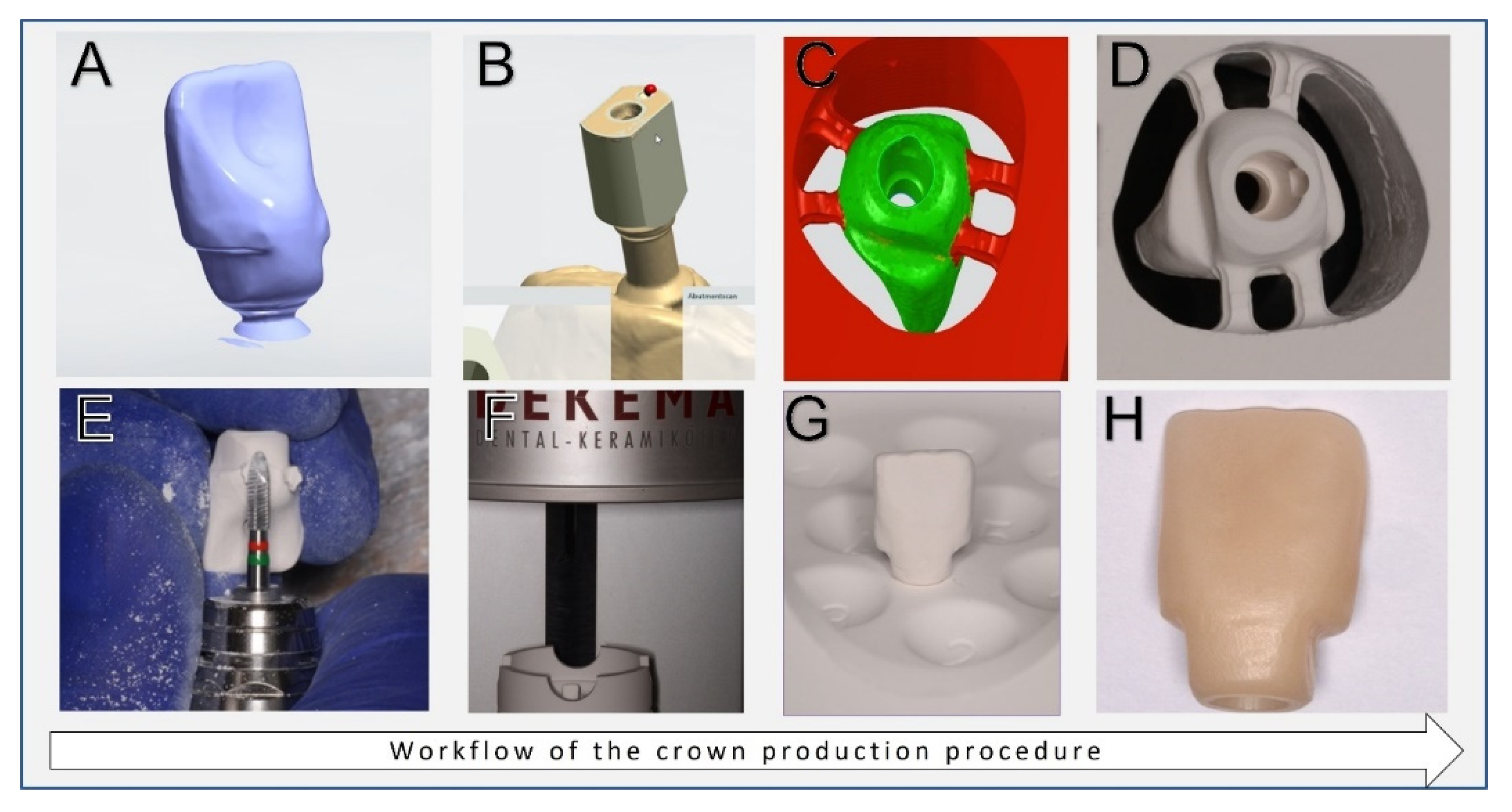
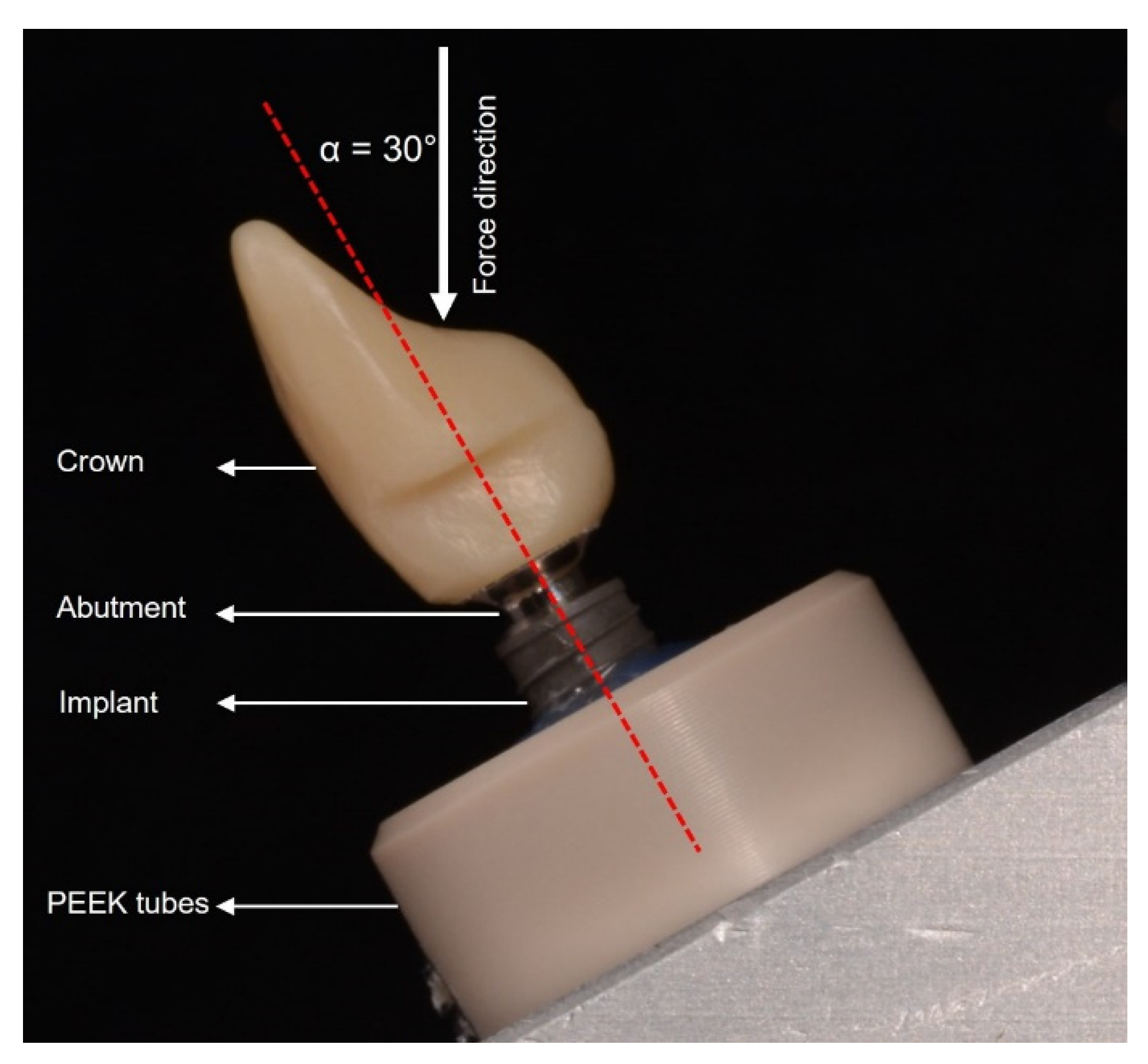
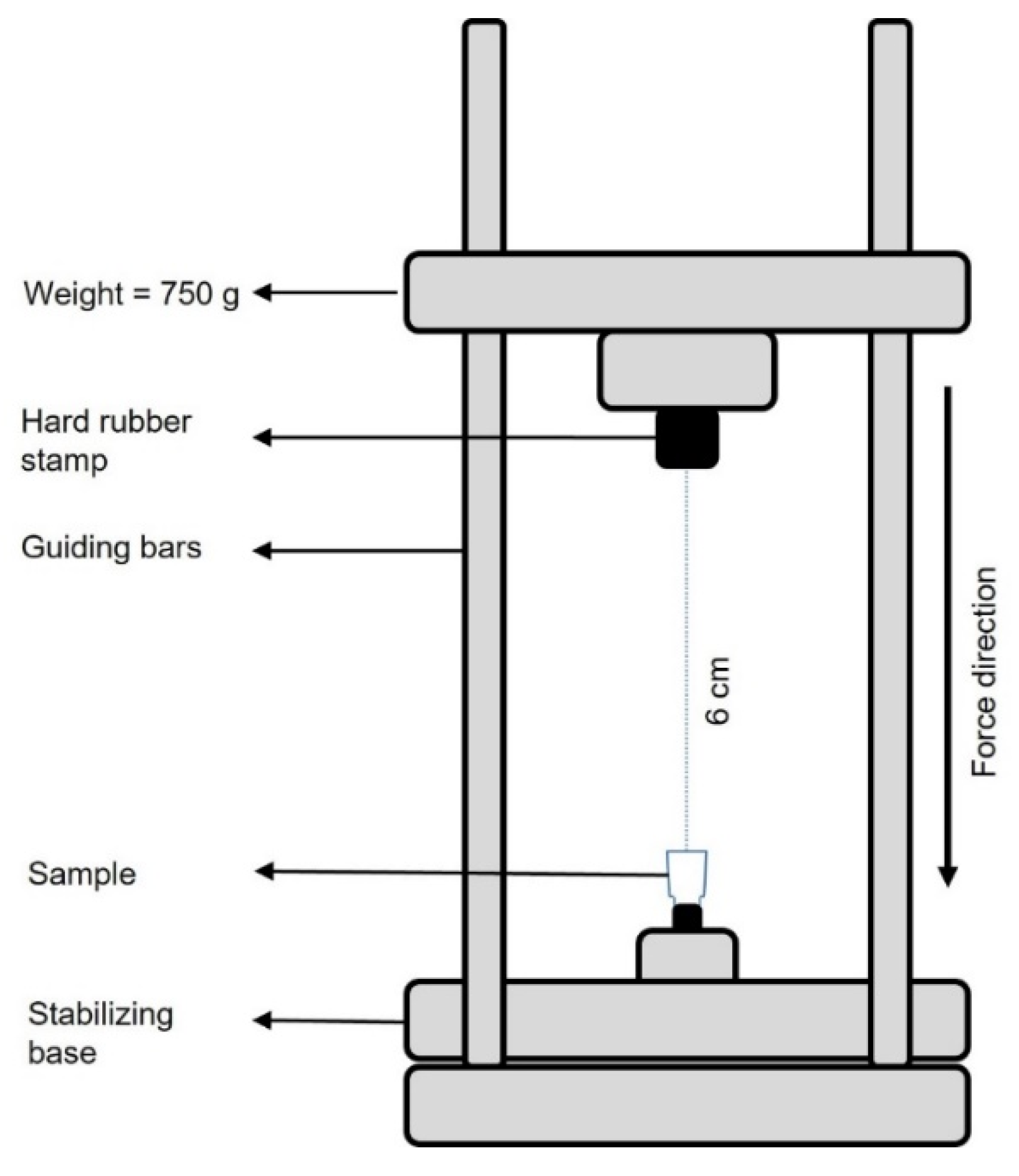
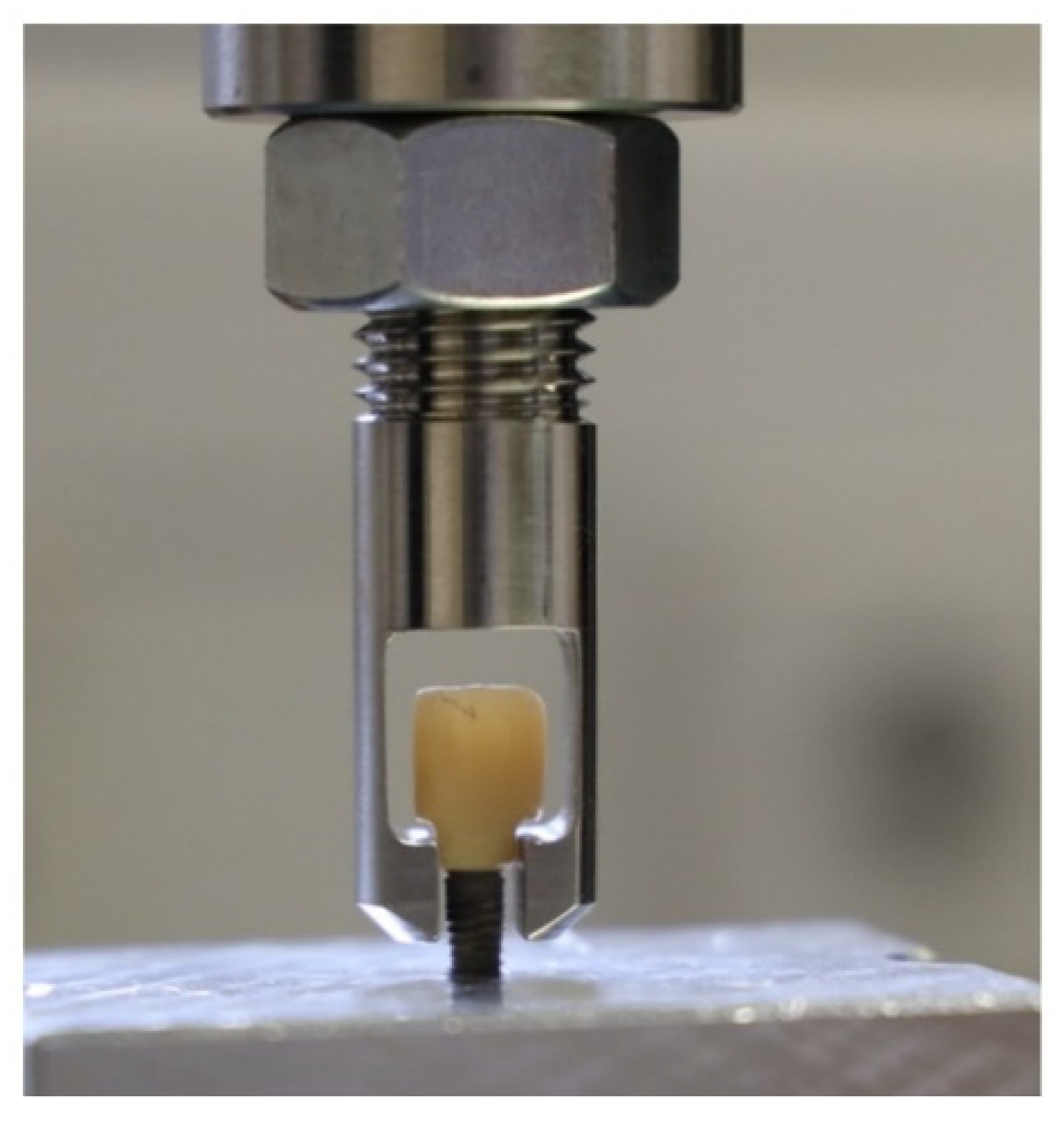
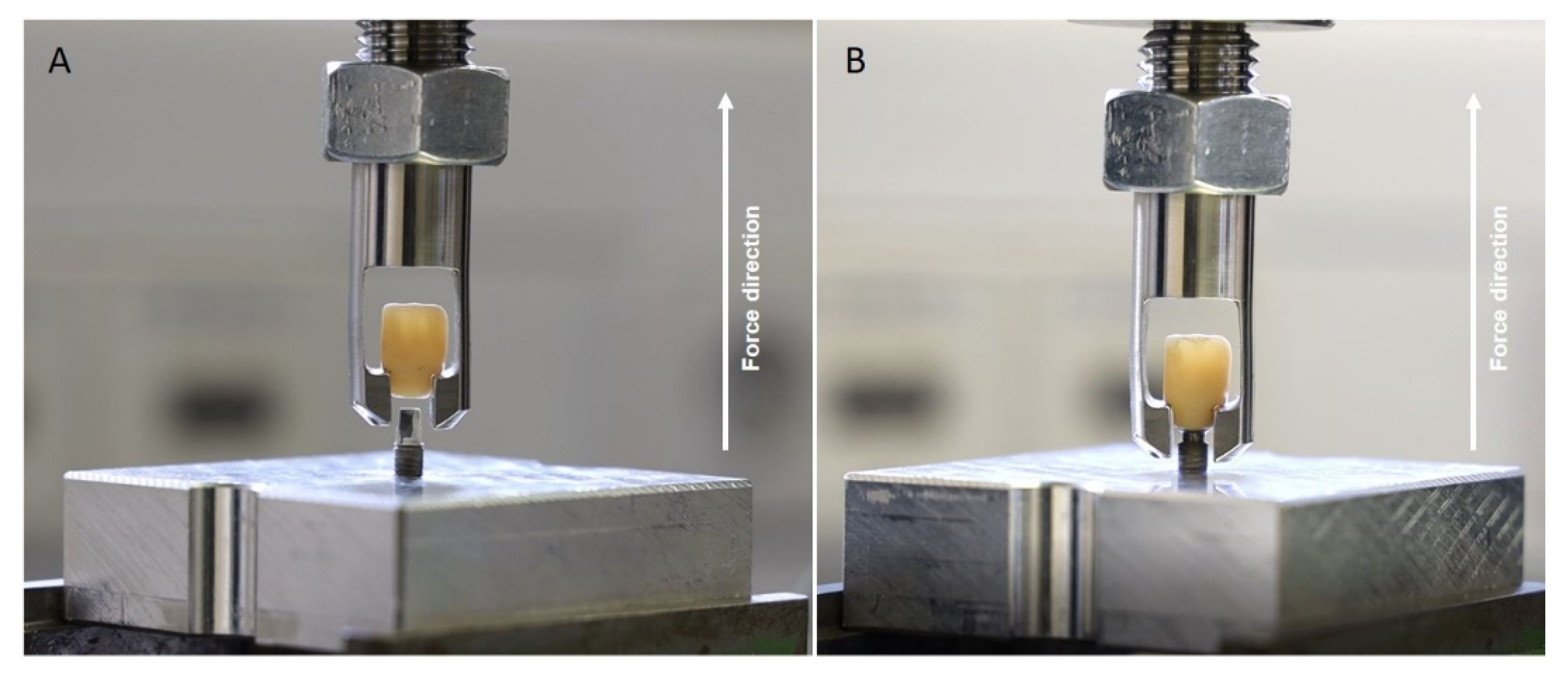
2. Materials and Methods
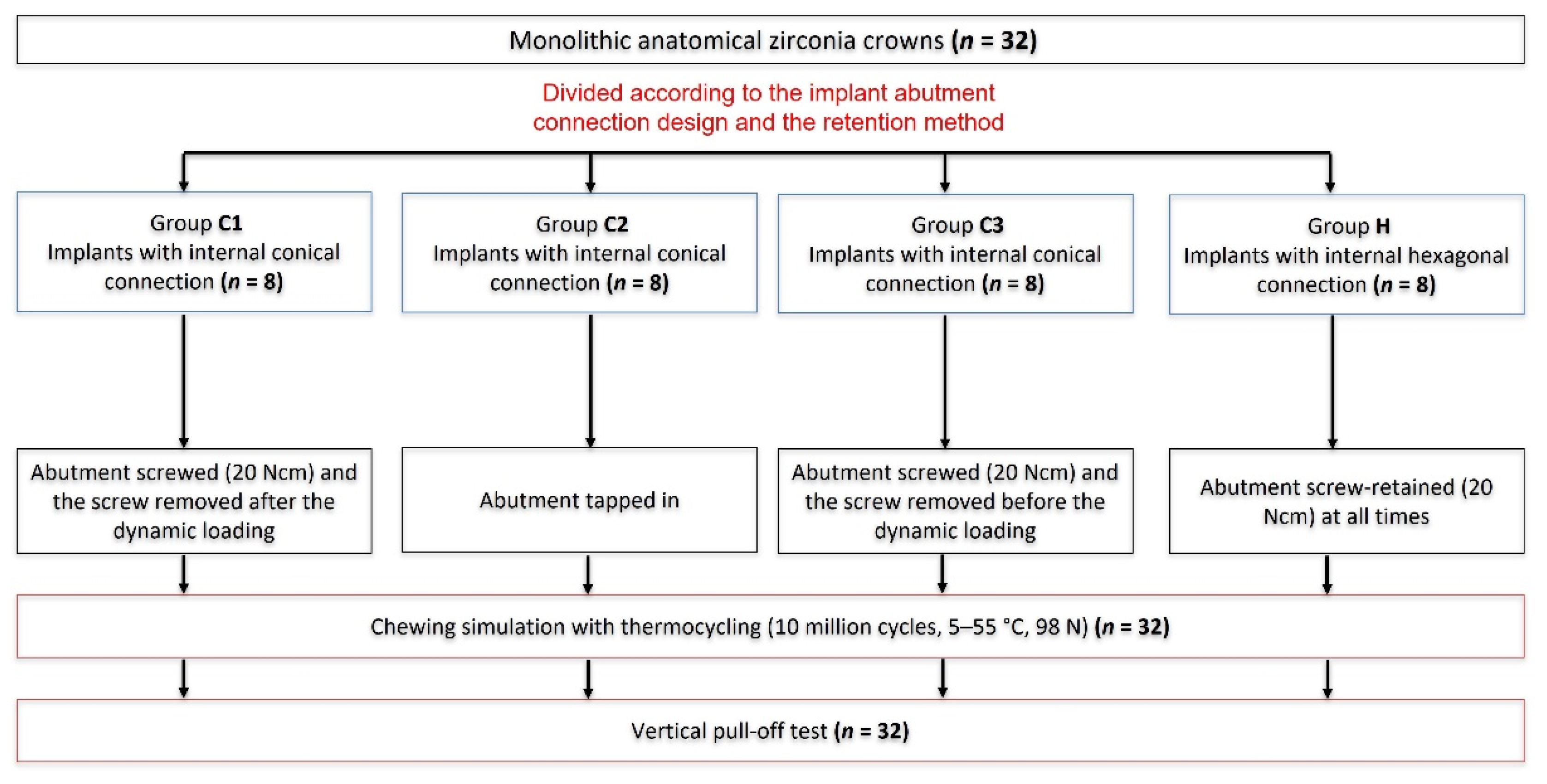
2.1. Outline of the Study
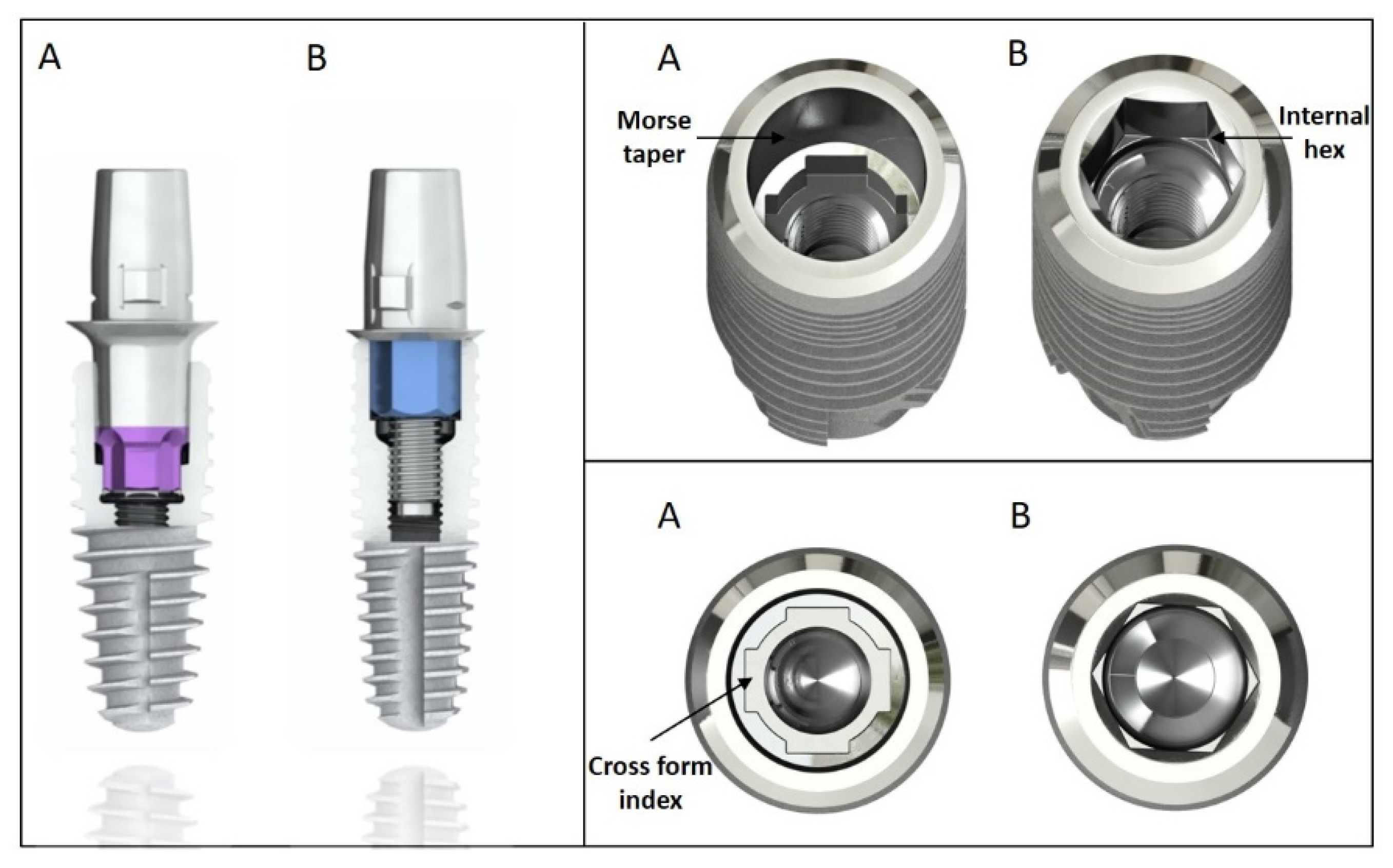
- Groups C1–C3: Morse taper internal conical connection (SICvantage tapered, SIC Invent AG, Basel, Switzerland). A cone angle of 2.8° and a cone length of 3 mm; indexed with four grooves in a cross form (Figure 2A).
- Group H: Internal hexagonal connection (SIC tapered, SIC Invent AG) characterized with parallel-walled orientation surfaces (Figure 2B).
2.2. Statistical Analysis
3. Results
3.1. Results from the Dynamic Loading (Chewing Simulation)
3.2. Quasi-Static Pull-Off Retention Stability Test Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Mazza, L.C.; Lemos, C.A.A.; Pesqueira, A.A.; Pellizzer, E.P. Survival and Complications of Monolithic Ceramic for Tooth-Supported Fixed Dental Prostheses: A Systematic Review and Meta-Analysis. J. Prosthet. Dent. 2021; in press. [Google Scholar] [CrossRef] [PubMed]
- AlTarawneh, S.; Thalji, G.; Cooper, L. Full-Arch Implant-Supported Monolithic Zirconia Fixed Dental Prostheses: An Updated Systematic Review. Int. J. Oral Implantol. 2021, 14, 13–22. [Google Scholar]
- Shi, J.; Lai, Y.; Qian, S.; Qiao, S.; Tonetti, M.S.; Lai, H. Clinical, Radiographic and Economic Evaluation of Short-6-mm Implants and Longer Implants Combined with Osteotome Sinus Floor Elevation in Moderately Atrophic Maxillae: A 3-year Randomized Clinical Trial. J. Clin. Periodontol. 2021, 48, 695–704. [Google Scholar] [CrossRef] [PubMed]
- Salvi, G.E.; Moëne, R.; Wallkamm, B.; Hicklin, S.P.; Bischof, M.; Nedir, R.; Mombelli, A.; Sculean, A. Clinical and Radiographic Changes at Tissue Level Implants with Either a Machined or a Modified Transmucosal Neck Surface: A 3-year Multicentre Randomized Controlled Proof-of-concept Study. J. Clin. Periodontol. 2020, 47, 500–508. [Google Scholar] [CrossRef]
- Saadoun, A.P.; Le Gall, M.G.; Touati, B. Current Trends in Implantology: Part II–Treatment Planning, Aesthetic Considerations, and Tissue Regeneration. Pract. Proced. Aesthet. Dent. 2004, 16, 707–714. [Google Scholar]
- Tischler, M. Dental Implants in the Esthetic Zone. Considerations for Form and Function. N. Y. State Dent. J. 2004, 70, 22–26. [Google Scholar]
- Ernst, C.-P.; Canbek, K.; Euler, T.; Willershausen, B. In Vivo Validation of the Historical in Vitro Thermocycling Temperature Range for Dental Materials Testing. Clin. Oral Investig. 2004, 8, 130–138. [Google Scholar] [CrossRef]
- Pjetursson, B.E.; Zarauz, C.; Strasding, M.; Sailer, I.; Zwahlen, M.; Zembic, A. A Systematic Review of the Influence of the Implant-Abutment Connection on the Clinical Outcomes of Ceramic and Metal Implant Abutments Supporting Fixed Implant Reconstructions. Clin. Oral Implant. Res. 2018, 29, 160–183. [Google Scholar] [CrossRef] [Green Version]
- Sailer, I.; Philipp, A.; Zembic, A.; Pjetursson, B.E.; Hämmerle, C.H.F.; Zwahlen, M. A Systematic Review of the Performance of Ceramic and Metal Implant Abutments Supporting Fixed Implant Reconstructions. Clin. Oral Implant. Res. 2009, 20, 4–31. [Google Scholar] [CrossRef] [Green Version]
- Vetromilla, B.M.; Brondani, L.P.; Pereira-Cenci, T.; Bergoli, C.D. Influence of Different Implant-Abutment Connection Designs on the Mechanical and Biological Behavior of Single-Tooth Implants in the Maxillary Esthetic Zone: A Systematic Review. J. Prosthet. Dent. 2019, 121, 398–403. [Google Scholar] [CrossRef]
- Abrahamsson, I.; Berglundh, T.; Glantz, P.-O.; Lindhe, J. The Mucosal Attachment at Different Abutments. An Experimental Study in Dogs. J. Clin. Periodontol. 1998, 25, 721–727. [Google Scholar] [CrossRef] [PubMed]
- Lindhe, J.; Meyle, J.; on behalf of Group D of the European Workshop on Periodontology. Peri-Implant Diseases: Consensus Report of the Sixth European Workshop on Periodontology. J. Clin. Periodontol. 2008, 35, 282–285. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oskarsson, M.; Otsuki, M.; Welander, M.; Abrahamsson, I. Peri-Implant Tissue Healing at Implants with Different Designs and Placement Protocols: An Experimental Study in Dogs. Clin. Oral Implant. Res. 2018, 29, 873–880. [Google Scholar] [CrossRef] [PubMed]
- Stiesch, M.; Pott, P.-C.; Eisenburger, M. Implantat-Abutment-Verbund. Zahnmedizin up2date 2011, 5, 445–464. [Google Scholar] [CrossRef]
- Schmitt, C.M.; Nogueira-Filho, G.; Tenenbaum, H.C.; Lai, J.Y.; Brito, C.; Döring, H.; Nonhoff, J. Performance of Conical Abutment (Morse Taper) Connection Implants: A Systematic Review: Performance of Conical Implant-Abutment Connection Systems. J. Biomed. Mater. Res. 2014, 102, 552–574. [Google Scholar] [CrossRef]
- Bagegni, A.; Spies, B.C.; Kern, M.; Hazard, D.; Kohal, R. The Influence of Prosthetic Crown Height and Implant-Abutment Connection Design Selection on the Long-Term Implant-Abutment Stability: A Laboratory Study. J. Mech. Behav. Biomed. Mater. 2021, 113, 104095. [Google Scholar] [CrossRef]
- Merz, B.R.; Hunenbart, S.; Belser, U.C. Mechanics of the Implant-Abutment Connection: An 8-Degree Taper Compared to a Butt Joint Connection. Int. J. Oral Maxillofac. Implant. 2000, 15, 519–526. [Google Scholar]
- Khraisat, A.; Stegaroiu, R.; Nomura, S.; Miyakawa, O. Fatigue Resistance of Two Implant/Abutment Joint Designs. J. Prosthet. Dent. 2002, 88, 604–610. [Google Scholar] [CrossRef]
- Beuer, F.; Beuer, S.; Schaller, P.; Schweiger, J.; Stimmelmayr, M. Cementation vs. Screw-Retention: A Rather Practical Decision! Implantologie 2015, 23, 131–137. [Google Scholar]
- Wittneben, J.; Joda, T.; Weber, H.; Brägger, U. Screw Retained vs. Cement Retained Implant-Supported Fixed Dental Prosthesis. Periodontology 2000 2017, 73, 141–151. [Google Scholar] [CrossRef]
- Schwarz, F.; Derks, J.; Monje, A.; Wang, H.L. Peri-implantitis. J Periodontol. 2018, 45 (Suppl. 1), S267–S290. [Google Scholar] [CrossRef] [PubMed]
- Jung, E.R.; Zembic, A.; Pjetursson, B.E.; Zwahlen, M.; Thoma, S.D. Systematic Review of the Survival Rate and the Incidence of Biological, Technical, and Aesthetic Complications of Single Crowns on Implants Reported in Longitudinal Studies with a Mean Follow-up of 5 Years. Clin. Oral Implant. Res. 2012, 23, 2–21. [Google Scholar] [CrossRef] [PubMed]
- Nissan, J.; Ghelfan, O.; Gross, O.; Priel, I.; Gross, M.; Chaushu, G. The Effect of Crown/Implant Ratio and Crown Height Space on Stress Distribution in Unsplinted Implant Supporting Restorations. J. Oral Maxillofac. Surg. 2011, 69, 1934–1939. [Google Scholar] [CrossRef] [PubMed]
- Nissan, J.; Gross, O.; Ghelfan, O.; Priel, I.; Gross, M.; Chaushu, G. The Effect of Splinting Implant-Supported Restorations on Stress Distribution of Different Crown-Implant Ratios and Crown Height Spaces. J. Oral Maxillofac. Surg. 2011, 69, 2990–2994. [Google Scholar] [CrossRef] [PubMed]
- Mangano, F.; Macchi, A.; Caprioglio, A.; Sammons, R.L.; Piattelli, A.; Mangano, C. Survival and Complication Rates of Fixed Restorations Supported by Locking-Taper Implants: A Prospective Study with 1 to 10 Years of Follow-Up: Survival and Complications of Fixed Restorations. J. Prosthodont. 2014, 23, 434–444. [Google Scholar] [CrossRef]
- Urdaneta, R.A.; Rodriguez, S.; McNeil, D.C.; Weed, M.; Chuang, S.-K. The Effect of Increased Crown-to-Implant Ratio on Single-Tooth Locking-Taper Implants. Int. J. Oral Maxillofac. Implant. 2010, 25, 729–743. [Google Scholar]
- Ahn, S.G.; Sorensen, J. Comparison of Mechanical Properties of Various Post and Core Materials. J. Korean Acad. Prosthodont. 2003, 41, 288–299. [Google Scholar]
- Zielak, J.C.; Rorbacker, M.; Gomes, R.; Yamashita, C.; Gonzaga, C.C.; Giovanni, A.F. In Vitro Evaluation of the Removal Force of Abutments in Frictional Dental Implants. J. Oral Implantol. 2011, 37, 519–523. [Google Scholar] [CrossRef]
- Kern, M.; Strub, J.R.; Lu, X.-Y. Wear of Composite Resin Veneering Materials in a Dual-Axis Chewing Simulator. J. Oral Rehabil. 1999, 26, 372–378. [Google Scholar] [CrossRef]
- Steiner, M.; Mitsias, M.E.; Ludwig, K.; Kern, M. In Vitro Evaluation of a Mechanical Testing Chewing Simulator. Dent. Mater. J. 2009, 25, 494–499. [Google Scholar] [CrossRef]
- Müller, L.; Rauch, A.; Reissmann, D.R.; Schierz, O. Impact of Cement Type and Abutment Height on Pull-off Force of Zirconia Reinforced Lithium Silicate Crowns on Titanium Implant Stock Abutments: An in Vitro Study. BMC Oral Health 2021, 21, 592. [Google Scholar] [CrossRef] [PubMed]
- Ugurel, C.S.; Steiner, M.; Isik-Ozkol, G.; Kutay, O.; Kern, M. Mechanical Resistance of Screwless Morse Taper and Screw-Retained Implant-Abutment Connections. Clin. Oral Implant. Res. 2015, 26, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Schwartz-Arad, D.; Samet, N.; Samet, N. Single Tooth Replacement of Missing Molars: A Retrospective Study of 78 Implants. J. Periodontol. 1999, 70, 449–454. [Google Scholar] [CrossRef] [PubMed]
- Theoharidou, A.; Petridis, H.P.; Tzannas, K.; Garefis, P. Abutment Screw Loosening in Single-Implant Restorations: A Systematic Review. Int. J. Oral Maxillofac. Implant. 2008, 23, 681–690. [Google Scholar]
- Mericske-Stern, R.; Grütter, L.; Rösch, R.; Mericske, E. Clinical Evaluation and Prosthetic Complications of Single Tooth Replacements by Non-Submerged Implants: Single Tooth Replacements by Non-Submerged Implants. Clin. Oral Implant. Res. 2001, 12, 309–318. [Google Scholar] [CrossRef]
- Jung, R.E.; Pjetursson, B.E.; Glauser, R.; Zembic, A.; Zwahlen, M.; Lang, N.P. A Systematic Review of the 5-Year Survival and Complication Rates of Implant-Supported Single Crowns. Clin. Oral Implant. Res. 2008, 19, 119–130. [Google Scholar] [CrossRef]
- Goodacre, C.J.; Kan, J.Y.K.; Rungcharassaeng, K. Clinical Complications of Osseointegrated Implants. J. Prosthet. Dent. 1999, 81, 537–552. [Google Scholar] [CrossRef]
- Gupta, S.; Gupta, H.; Tandan, A. Technical Complications of Implant-Causes and Management: A Comprehensive Review. Natl. J. Maxillofac. Surg. 2015, 6, 3–8. [Google Scholar] [CrossRef]
- Hsu, P.-F.; Yao, K.-T.; Kao, H.-C.; Hsu, M.-L. Effects of Axial Loading on the Pull-out Force of Conical Connection Abutments in Ankylos Implant. Int. J. Oral Maxillofac. Implant. 2018, 33, 788–794. [Google Scholar] [CrossRef]
- Ricciardi Coppedê, A.; da Glória Chiarello de Mattos, M.; Rodrigues, R.C.S.; Ribeiro, R.F. Effect of Repeated Torque/Mechanical Loading Cycles on Two Different Abutment Types in Implants with Internal Tapered Connections: An in Vitro Study. Clin. Oral Implant. Res. 2009, 20, 624–632. [Google Scholar] [CrossRef]
- Pintinha, M.; Camarini, E.T.; Sábio, S.; Pereira, J.R. Effect of Mechanical Loading on the Removal Torque of Different Types of Tapered Connection Abutments for Dental Implants. J. Prosthet. Dent. 2013, 110, 383–388. [Google Scholar] [CrossRef] [PubMed]
- Bagegni, A.; Zabler, S.; Nelson, K.; Rack, A.; Spies, B.C.; Vach, K.; Kohal, R. Synchrotron-Based Micro Computed Tomography Investigation of the Implant-Abutment Fatigue-Induced Microgap Changes. J. Mech. Behav. Biomed. Mater. 2021, 116, 104330. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.-S.; Han, J.-S.; Lim, Y.-J. Settling of Abutments into Implants and Changes in Removal Torque in Five Different Implant-Abutment Connections. Part 1: Cyclic Loading. Int. J. Oral Maxillofac. Implant. 2014, 29, 1079–1084. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kofron, M.D.; Carstens, M.; Fu, C.; Wen, H.B. In Vitro Assessment of Connection Strength and Stability of Internal Implant-Abutment Connections. Clin. Biomech. 2019, 65, 92–99. [Google Scholar] [CrossRef] [Green Version]
- D’Addazio, G.; Sinjari, B.; Arcuri, L.; Femminella, B.; Murmura, G.; Santilli, M.; Caputi, S. Mechanical Pull-Out Test of a New Hybrid Fixture-Abutment Connection: An In Vitro Study. Materials 2021, 14, 1555. [Google Scholar] [CrossRef]
- Morresi, A.L.; D’Amario, M.; Capogreco, M.; Gatto, R.; Marzo, G.; D’Arcangelo, C.; Monaco, A. Thermal Cycling for Restorative Materials: Does a Standardized Protocol Exist in Laboratory Testing? A Literature Review. J. Mech. Behav. Biomed. Mater. 2014, 29, 295–308. [Google Scholar] [CrossRef]
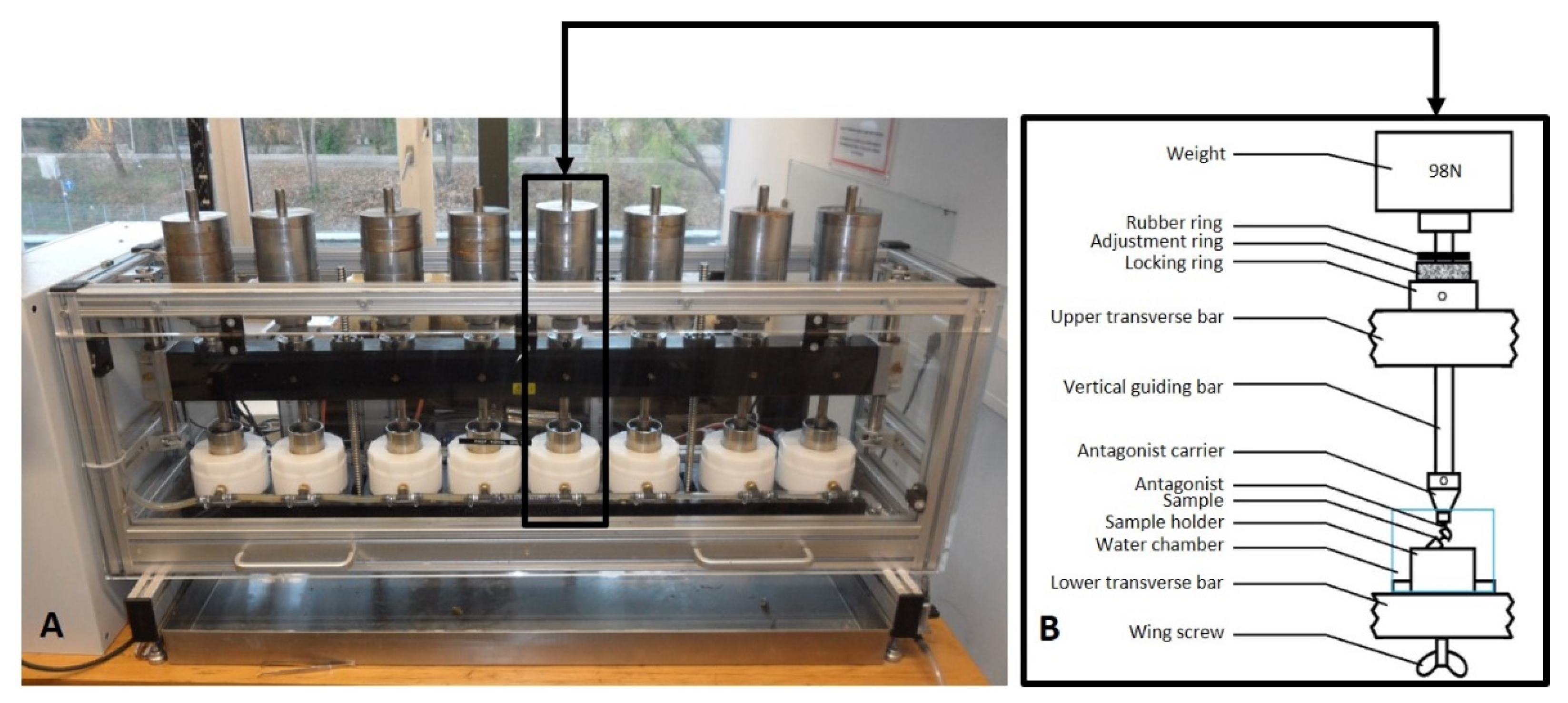

| Specifications of the Chewing Simulator | |
|---|---|
| Total Number of cycles | 10 Million |
| Movement | Vertical: 1.5 mm; horizontal: 0.5 mm |
| Speed and frequency | Descending: 60 mm/s; rising: 60 mm/s; forward: 55 mm/s; backward: 55 mm/s; frequency: 1.9 Hz |
| Weight | 10 kg (98 N) |
| Thermocycling | Cold: 5 °C; hot: 55 °C |
| IAC Design | Hexagonal IAC | Conical IAC | ||
|---|---|---|---|---|
| Group | H | C1 | C2 | C3 |
| Prevalence of implant fractures | 0 | 0 | 0 | 0 |
| Prevalence of abutment fractures | 0 | 0 | 0 | 0 |
| Prevalence of crack/deformation events | 0 | 0 | 0 | 0 |
| Prevalence of screw loosening events | 0 | 8 | 0 | 0 |
| Prevalence of crown–abutment decementations | 0 | 1 | 2 | 1 |
| Implant survival rates | 100% | 100% | ||
| Abutment survival rates | 100% | 100% | ||
| Overall survival rate | 100% | |||
| Group | No. | Max (N) | Min (N) | Mean (N) | SD (N) | No. of Crown–Abutment Decementations | No. of Abutment–Implant Detachments |
|---|---|---|---|---|---|---|---|
| C1 | 8 | 321 | 136 | 224.4 | 61.9 | 1 | 7 |
| C2 | 7 | 245 | 136 | 171.6 | 37.7 | 0 | 7 |
| C3 | 8 | 318 | 72.7 | 247.0 | 77.4 | 1 | 7 |
| H | 8 | 1270 | 121 | 769.6 | 413.5 | 8 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bagegni, A.; Weihrauch, V.; Vach, K.; Kohal, R. The Mechanical Behavior of a Screwless Morse Taper Implant–Abutment Connection: An In Vitro Study. Materials 2022, 15, 3381. https://doi.org/10.3390/ma15093381
Bagegni A, Weihrauch V, Vach K, Kohal R. The Mechanical Behavior of a Screwless Morse Taper Implant–Abutment Connection: An In Vitro Study. Materials. 2022; 15(9):3381. https://doi.org/10.3390/ma15093381
Chicago/Turabian StyleBagegni, Aimen, Vincent Weihrauch, Kirstin Vach, and Ralf Kohal. 2022. "The Mechanical Behavior of a Screwless Morse Taper Implant–Abutment Connection: An In Vitro Study" Materials 15, no. 9: 3381. https://doi.org/10.3390/ma15093381
APA StyleBagegni, A., Weihrauch, V., Vach, K., & Kohal, R. (2022). The Mechanical Behavior of a Screwless Morse Taper Implant–Abutment Connection: An In Vitro Study. Materials, 15(9), 3381. https://doi.org/10.3390/ma15093381








